Does the Argentine Tango Sustainably Improve Cancer-Associated Fatigue and Quality of Life in Breast Cancer Survivors?
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
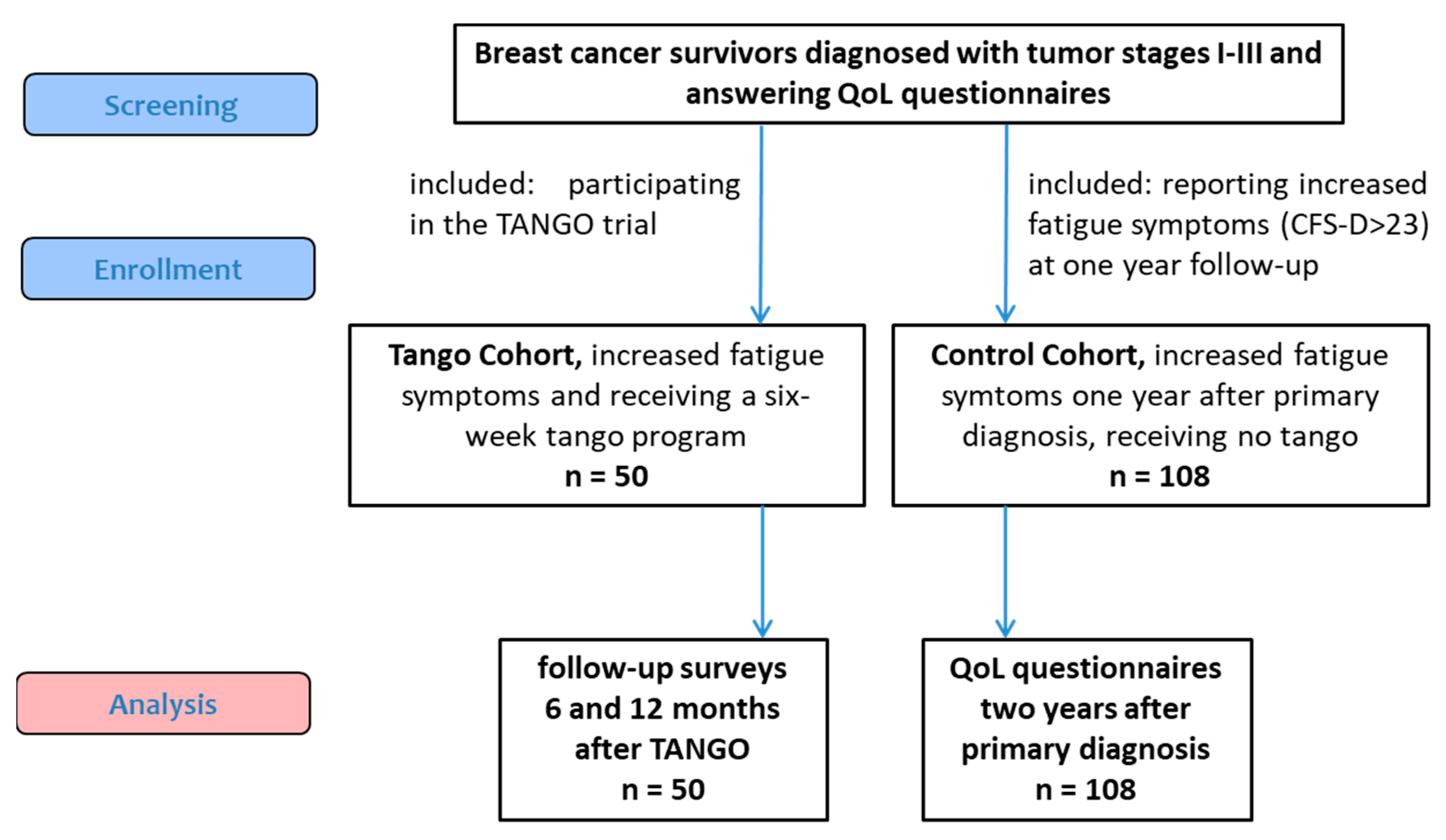
2.1. Participants, Study Design, and Procedure
2.2. Outcome Measures
2.3. Statistical Analysis
3. Results
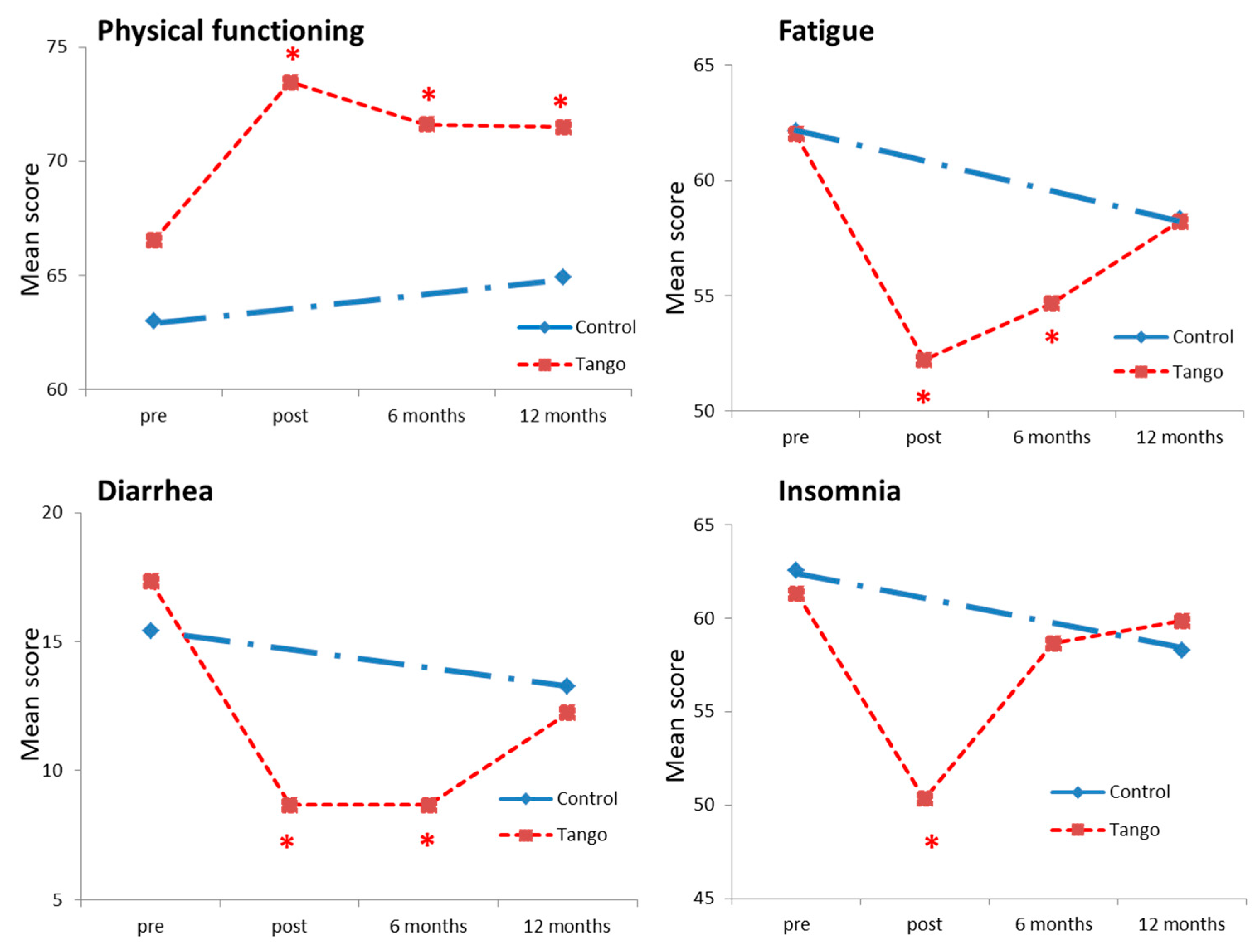
3.1. Comparison of QoL Outcomes in the Tango and the Control Cohort
3.2. Follow-Up Evaluation of the Tango Cohort
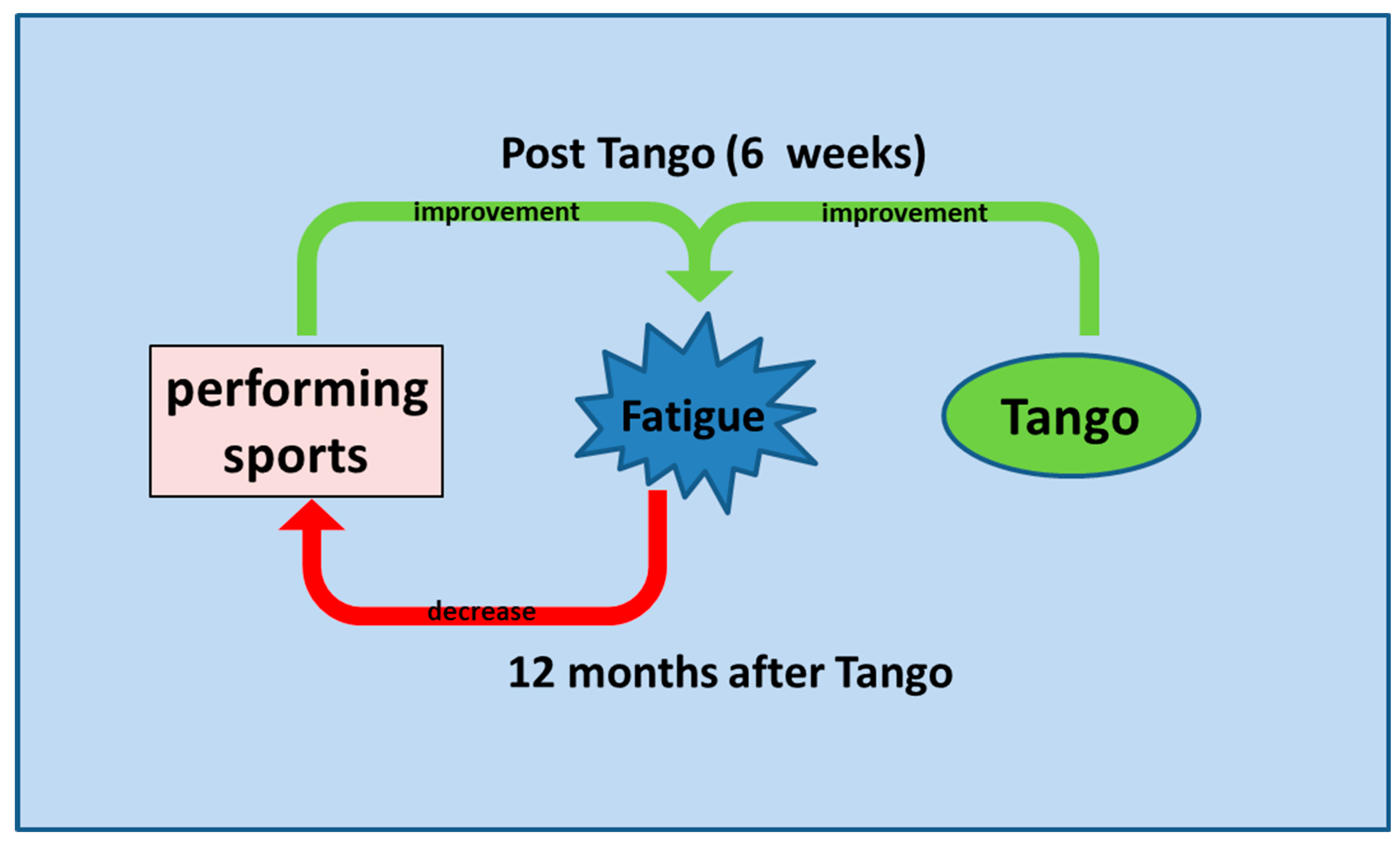
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Fabi, A.; Falcicchio, C.; Giannarelli, D.; Maggi, G.; Cognetti, F.; Pugliese, P. The course of cancer related fatigue up to ten years in early breast cancer patients: What impact in clinical practice? Breast 2017, 34, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Abrahams, H.J.G.; Gielissen, M.F.M.; Schmits, I.C.; Verhagen, C.; Rovers, M.M.; Knoop, H. Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: A meta-analysis involving 12 327 breast cancer survivors. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2016, 27, 965–974. [Google Scholar] [CrossRef]
- Bower, J.E. Cancer-related fatigue--mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609. [Google Scholar] [CrossRef] [PubMed]
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. Cancer-related fatigue: Esmo clinical practice guidelines for diagnosis and treatment. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Network NCC (2022) NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue (Version 1.2022). Available online: https://allofmeiowa.org/wp-content/uploads/2022/04/NCCN-Guidelines-1.2022-CA-related-fatigue.pdf (accessed on 3 January 2022).
- Greenlee, H.; DuPont-Reyes, M.J.; Balneaves, L.G.; Carlson, L.E.; Cohen, M.R.; Deng, G.; Johnson, J.A.; Mumber, M.; Seely, D.; Zick, S.M.; et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: A Cancer J. Clin. 2017, 67, 194–232. [Google Scholar] [CrossRef]
- Mokhatri-Hesari, P.; Montazeri, A. Health-related quality of life in breast cancer patients: Review of reviews from 2008 to 2018. Health Qual. Life Outcomes 2020, 18, 338. [Google Scholar] [CrossRef]
- Medeiros Torres, D.; Jorge Koifman, R.; da Silva Santos, S. Impact on fatigue of different types of physical exercise during adjuvant chemotherapy and radiotherapy in breast cancer: Systematic review and meta-analysis. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2022, 30, 4651–4662. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise guidelines for cancer survivors: Consensus statement from international multidisciplinary roundtable. Med. Sci. Sport. Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Frikkel, J.; Götte, M.; Beckmann, M.; Kasper, S.; Hense, J.; Teufel, M.; Schuler, M.; Tewes, M. Fatigue, barriers to physical activity and predictors for motivation to exercise in advanced cancer patients. BMC Palliat. Care 2020, 19, 43. [Google Scholar] [CrossRef]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016, CD006911. [Google Scholar] [CrossRef] [PubMed]
- Hohmann, L.; Bradt, J.; Stegemann, T.; Koelsch, S. Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLoS ONE 2017, 12, e0187363. [Google Scholar] [CrossRef]
- Sturm, I.; Baak, J.; Storek, B.; Traore, A.; Thuss-Patience, P. Effect of dance on cancer-related fatigue and quality of life. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2014, 22, 2241–2249. [Google Scholar] [CrossRef] [PubMed]
- Boing, L.; Fretta, T.d.B.; Lynch, B.M.; Dias, M.; Rosa, L.M.d.; Baptista, F.; Bergmann, A.; Fausto, D.Y.; Bocchi Martins, J.B.; Guimarães, A.C.d.A. Mat pilates and belly dance: Effects on patient-reported outcomes among breast cancer survivors receiving hormone therapy and adherence to exercise. Complement. Ther. Clin. Pract. 2023, 50, 101683. [Google Scholar] [CrossRef] [PubMed]
- da Silva Cruz, E.I.; Cruz, A.H.d.S.; Ventura, J.A.; Marques, R.A.S.; Santos, R.d.S.; Reis, A.A.d.S. The impact of dance as a non-pharmacological adjuvant therapy cancer survivors: A clinical trial. Res. Soc. Dev. 2022, 11, e14411729714. [Google Scholar] [CrossRef]
- Lotzke, D.; Ostermann, T.; Bussing, A. Argentine tango in parkinson disease—A systematic review and meta-analysis. BMC Neurol. 2015, 15, 226. [Google Scholar] [CrossRef]
- Worthen-Chaudhari, L.; Lamantia, M.T.; Monfort, S.M.; Mysiw, W.; Chaudhari, A.M.W.; Lustberg, M.B. Partnered, adapted argentine tango dance for cancer survivors: A feasibility study and pilot study of efficacy. Clin. Biomech. 2019, 70, 257–264. [Google Scholar] [CrossRef]
- Schad, F.; Rieser, T.; Becker, S.; Groß, J.; Matthes, H.; Oei, S.L.; Thronicke, A. Efficacy of tango argentino for cancer-associated fatigue and quality of life in breast cancer survivors: A randomized controlled trial. Cancers 2023, 15, 2920. [Google Scholar] [CrossRef]
- Schad, F.; Axtner, J.; Happe, A.; Breitkreuz, T.; Paxino, C.; Gutsch, J.; Matthes, B.; Debus, M.; Kroz, M.; Spahn, G.; et al. Network oncology (no)—A clinical cancer register for health services research and the evaluation of integrative therapeutic interventions in anthroposophic medicine. Forsch. Komplement. 2013, 20, 353–360. [Google Scholar] [CrossRef]
- Oei, S.L.; Rieser, T.; Becker, S.; Groß, J.; Matthes, H.; Schad, F.; Thronicke, A. Tango: Effect of tango argentino on cancer-associated fatigue in breast cancer patients-study protocol for a randomized controlled trial. Trials 2021, 22, 866. [Google Scholar] [CrossRef]
- Schad, F.; Thronicke, A.; Merkle, A.; Steele, M.L.; Kroz, M.; Herbstreit, C.; Matthes, H. Implementation of an integrative oncological concept in the daily care of a german certified breast cancer center. Complement Med Res 2018, 25, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Kroz, M.; Zerm, R.; Reif, M.; HB, V.O.N.L.; Schad, F.; Bussing, A.; Bartsch, C.; Feder, G.; Girke, M. Validation of the german version of the cancer fatigue scale (cfs-d). Eur. J. Cancer Care 2008, 17, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; de Haes, J.C.; et al. The european organization for research and treatment of cancer qlq-c30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Millman, L.S.M.; Terhune, D.B.; Hunter, E.C.M.; Orgs, G. Towards a neurocognitive approach to dance movement therapy for mental health: A systematic review. Clin. Psychol. Psychother. 2021, 28, 24–38. [Google Scholar] [CrossRef] [PubMed]
- Olsson Möller, U.; Beck, I.; Rydén, L.; Malmström, M. A comprehensive approach to rehabilitation interventions following breast cancer treatment—A systematic review of systematic reviews. BMC Cancer 2019, 19, 472. [Google Scholar] [CrossRef] [PubMed]
- Goodill, S.W. Accumulating evidence for dance/movement therapy in cancer care. Front. Psychol. 2018, 9, 1778. [Google Scholar] [CrossRef]
- Monti, A.C.; Scalera, P. Tango: Music, dance and statistical thinking. In Research Papers in Statistical Inference for Time Series and Related Models: Essays in Honor of Masanobu Taniguchi; Liu, Y., Hirukawa, J., Kakizawa, Y., Eds.; Springer Nature Singapore: Singapore, 2023; pp. 369–380. [Google Scholar] [CrossRef]
- Sodergren, S.C.; Copson, E.; White, A.; Efficace, F.; Sprangers, M.; Fitzsimmons, D.; Bottomley, A.; Johnson, C.D. Systematic review of the side effects associated with anti-her2-targeted therapies used in the treatment of breast cancer, on behalf of the eortc quality of life group. Target. Oncol. 2016, 11, 277–292. [Google Scholar] [CrossRef]
- Moschen, A.R.; Sammy, Y.; Marjenberg, Z.; Heptinstall, A.B.; Pooley, N.; Marczewska, A.M. The underestimated and overlooked burden of diarrhea and constipation in cancer patients. Curr. Oncol. Rep. 2022, 24, 861–874. [Google Scholar] [CrossRef]
- Verhaar, S.; Vissers, P.A.; Maas, H.; van de Poll-Franse, L.V.; van Erning, F.N.; Mols, F. Treatment-related differences in health related quality of life and disease specific symptoms among colon cancer survivors: Results from the population-based profiles registry. Eur. J. Cancer 2015, 51, 1263–1273. [Google Scholar] [CrossRef]
- Bossi, P.; Antonuzzo, A.; Cherny, N.I.; Rosengarten, O.; Pernot, S.; Trippa, F.; Schuler, U.; Snegovoy, A.; Jordan, K.; Ripamonti, C.I. Diarrhoea in adult cancer patients: Esmo clinical practice guidelines. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2018, 29, iv126–iv142. [Google Scholar] [CrossRef]
- Peterson, L.L.; Ligibel, J.A. Physical activity and breast cancer: An opportunity to improve outcomes. Curr. Oncol. Rep. 2018, 20, 50. [Google Scholar] [CrossRef] [PubMed]
- Van Dijck, S.; Nelissen, P.; Verbelen, H.; Tjalma, W.; Gebruers, N. The effects of physical self-management on quality of life in breast cancer patients: A systematic review. Breast 2016, 28, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Greenlee, H.; Bohlke, K.; Bao, T.; DeMichele, A.M.; Deng, G.E.; Fouladbakhsh, J.M.; Gil, B.; Hershman, D.L.; Mansfield, S.; et al. Integrative therapies during and after breast cancer treatment: Asco endorsement of the sio clinical practice guideline. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2018, 36, 2647–2655. [Google Scholar] [CrossRef] [PubMed]
- Beenhakker, L.; Witteveen, A.; Wijlens, K.A.E.; Siemerink, E.J.M.; van der Lee, M.L.; Bode, C.; Siesling, S.; Vollenbroek-Hutten, M.M.R. Patient preference attributes in ehealth interventions for cancer-related fatigue: A scoping review. Eur. J. Cancer Care 2022, 31, e13754. [Google Scholar] [CrossRef]
| Tango | Control | |
|---|---|---|
| Number of patients, n (%) | 50 (100) | 108 (100) |
| Age, years, mean (SD) | 61.3 (9.9) | 61.6 (11.7) |
| UICC stages, n (%) | ||
| I | 23 (46) | 51 (47) |
| II | 20 (40) | 48 (44) |
| III | 7 (14) | 9 (8) |
| Hormonal status, n (%) | ||
| Premenopausal | 2 (4) | 7 (6) |
| Postmenopausal | 48 (96) | 101 (94) |
| Interventions received, n (%) | ||
| Endocrine therapy | 34 (68) | 84 (78) |
| Chemotherapy | 24 (48) | 47 (44) |
| Immunotherapy | 6 (12) | 13 (12) |
| QoL questionnaires, mean (SD) | ||
| CFS-D total | 31.0 (9.3) | 32.2 (6.3) |
| EORTC QLQ C30 global health | 54.1 (16.9) | 54.6 (17.7) |
| Physical functioning | 66.5 (20.8) | 63.0 (20.5) |
| Role functioning | 54.0 (27.0) | 49.4 (27.7) |
| Emotional functioning | 42.1 (25.4) | 42.4 (23.3) |
| Fatigue | 62.0 (24.6) | 62.2 (19.9) |
| Insomnia | 61.3 (29.9) | 62.6 (33.6) |
| Diarrhea | 17.3 (29.2) | 15.4 (25.8) |
| Tango, at 6 Months n = 50 dmean (SD) p-Value | Tango, at 12 Months n = 49 dmean (SD) p-Value | Control n = 108 dmean (SD) p-Value | |
|---|---|---|---|
| EORTC QLQ C30 | |||
| Global health | 5.7 (18.4) 0.01 * | 0.2 (17.5) 0.94 | 3.1 (18.6) 0.09 |
| Physical functioning | 5.1 (13.6) 0.01 * | 4.8 (13.3) 0.015 * | 2.3 (15.7) 0.24 |
| Role functioning | 3.7 (23.2) 0.27 | 0.0 (27.6) 1.0 | 5.3 (30.8) 0.13 |
| Emotional functioning | 7.0 (20.0) 0.018 * | 1.4 (19.1) 0.67 | 6.7 (22.5) 0.003 * |
| Fatigue | −7.0 (17.9) 0.006 * | −3.7 (17.7) 0.15 | −3.8 (20.7) 0.062 |
| Insomnia | −2.7 (26.7) 0.49 | −1.4 (22.6) 0.68 | −4.1 (29.9) 0.16 |
| Diarrhea | −8.7 (28.1) 0.036 * | −4.1 (23.0) 0.22 | −2.2 (28.1) 0.4 |
| At 6 Months, n = 50 n (%) | At 12 Months, n = 49 n (%) | |
|---|---|---|
| Did you engage in any sports activities? | ||
| No = 0 | 10 (20) | 12 (24) |
| occasionally = 1 | 3 (6) | 7 (14) |
| 1–2 weekly = 2 | 28 (56) | 19 (39) |
| >2 weekly = 3 | 9 (18) | 10 (20) |
| ND | 0 | 1 (2) |
| Did you like dancing in a group? Or did you prefer dancing alone with the instructor? | ||
| preferred in the group | 40 (80) | |
| no preference | 6 (12) | |
| single, with instructor preferred | 2 (4) | |
| ND | 2 (4) | |
| Would you like to take a regular guided dance class? | ||
| no | 4 (8) | |
| probably | 14 (28) | |
| yes | 32 (64) | |
| ND | 0 | |
| Have you danced tango at home? | Did you do any kind of dance exercises? | |
| No = 0 | 23 (46) | 18 (37) |
| occasionally = 1 | 26 (52) | 27 (55) |
| regularly = 2 | 1 (2) | 3 (6) |
| ND | 0 | 1 (2) |
| Are you interested in online offers? | Have you used online offerings for sports or dance practice? | |
| No = 0 | 18 (36) | 34 (69) |
| probably/occasionally = 1 | 15 (30) | 12 (24) |
| Yes/regularly = 2 | 15 (30) | 2 (4) |
| ND | 2 (4) | 1 (2) |
| CFS-D Fatigue | Any Sports Engagement? | Any Online Sports? | Any Dance Exercises? |
|---|---|---|---|
| total | −0.026 * | −0.008 | 0.0001 |
| physical | −0.023 * | −0.003 | 0.0005 |
| cognitive | −0.01 | −0.006 | 0.001 |
| affective | −0.034 ** | −0.01 * | −0.001 |
| EORTC QLQ C30 | Any Sports Engagement? | Any Online Sports? | Any Dance Exercises? |
| global health status | 0.027 ** | 0.007 | 0.002 |
| physical functioning | 0.018 + | −0.002 | 0.006 |
| role functioning | 0.011 * | −0.004 | −0.002 |
| pain | −0.014 ** | −0.001 | −0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oei, S.L.; Thronicke, A.; Groß, J.; Rieser, T.; Becker, S.; Grabowski, P.; Grieb, G.; Matthes, H.; Schad, F. Does the Argentine Tango Sustainably Improve Cancer-Associated Fatigue and Quality of Life in Breast Cancer Survivors? Cancers 2023, 15, 5678. https://doi.org/10.3390/cancers15235678
Oei SL, Thronicke A, Groß J, Rieser T, Becker S, Grabowski P, Grieb G, Matthes H, Schad F. Does the Argentine Tango Sustainably Improve Cancer-Associated Fatigue and Quality of Life in Breast Cancer Survivors? Cancers. 2023; 15(23):5678. https://doi.org/10.3390/cancers15235678
Chicago/Turabian StyleOei, Shiao Li, Anja Thronicke, Jessica Groß, Thomas Rieser, Sarah Becker, Patricia Grabowski, Gerrit Grieb, Harald Matthes, and Friedemann Schad. 2023. "Does the Argentine Tango Sustainably Improve Cancer-Associated Fatigue and Quality of Life in Breast Cancer Survivors?" Cancers 15, no. 23: 5678. https://doi.org/10.3390/cancers15235678
APA StyleOei, S. L., Thronicke, A., Groß, J., Rieser, T., Becker, S., Grabowski, P., Grieb, G., Matthes, H., & Schad, F. (2023). Does the Argentine Tango Sustainably Improve Cancer-Associated Fatigue and Quality of Life in Breast Cancer Survivors? Cancers, 15(23), 5678. https://doi.org/10.3390/cancers15235678







