Hypofractionation in Glioblastoma: An Overview of Palliative, Definitive, and Exploratory Uses
Abstract
:Simple Summary
Abstract
1. Introduction
2. Pre-Operative Hypofractionation in Newly Diagnosed Glioblastoma
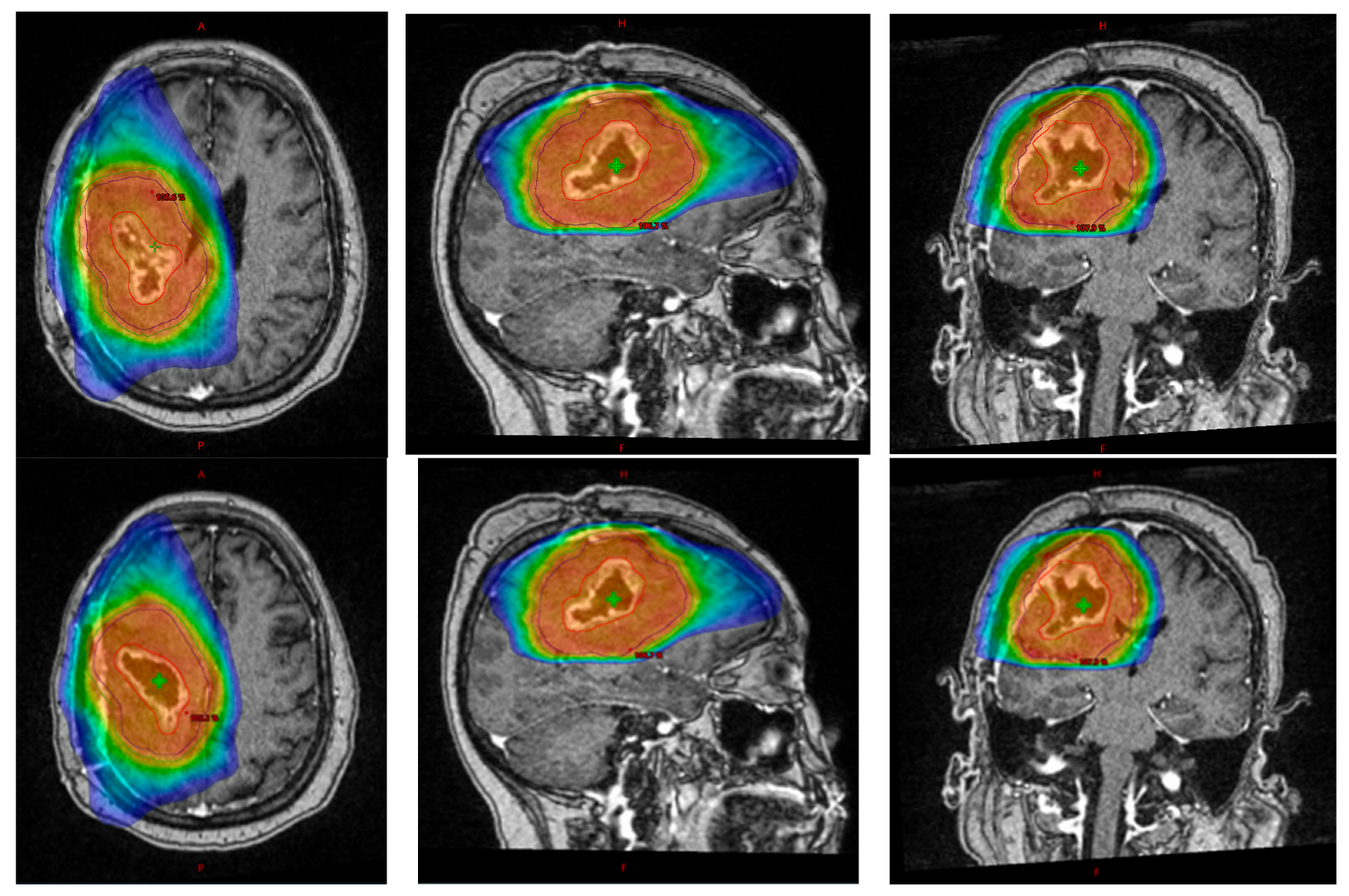
3. Post-Operative Hypofractionation in Newly Diagnosed Glioblastoma
3.1. Pre-Temozolomide Era
3.2. Post-Temozolomide Era
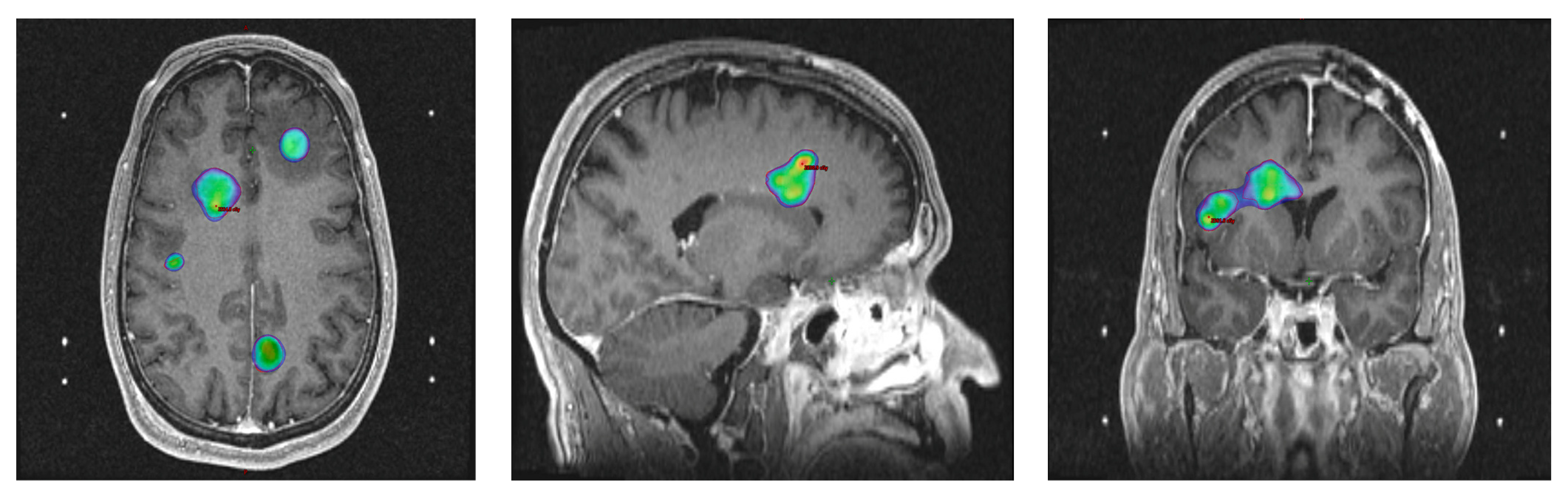
4. Hypofractionation for Recurrent Glioblastoma
5. Institutional Practices
6. Future Directions
6.1. FLASH-RT
6.2. Radiomics
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A summary. Neuro-Oncol. 2021, 23, 1231–1251. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, Q.T.; Cioffi, G.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2014–2018. Neuro-Oncol. 2021, 23 (Suppl. 2), 1–105. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients with Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316, Erratum in JAMA 2018, 319, 1824. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Carrillo, M.; Tovar-Martín, I.; Zurita-Herrera, M.; Del Moral-Ávila, R.; Guerrero-Tejada, R.; Saura-Rojas, E.; Osorio-Ceballos, J.L.; Arrebola-Moreno, J.P.; Expósito-Hernández, J. Salvage radiosurgery for selected patients with recurrent malignant gliomas. Biomed. Res. Int. 2014, 2014, 657953. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, F.H.; Pruitt, A. Assumptions in the radiotherapy of glioblastoma. Neurology 1980, 30, 907–911. [Google Scholar] [CrossRef] [PubMed]
- Wallner, K.E.; Galicich, J.H.; Krol, G.; Arbit, E.; Malkin, M.G. Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int. J. Radiat. Oncol. Biol. Phys. 1989, 16, 1405–1409. [Google Scholar] [CrossRef]
- Cuddapah, V.A.; Robel, S.; Watkins, S.; Sontheimer, H. A neurocentric perspective on glioma invasion. Nat. Rev. Neurosci. 2014, 15, 455–465. [Google Scholar] [CrossRef]
- Hingorani, M.; Colley, W.P.; Dixit, S.; Beavis, A.M. Hypofractionated radiotherapy for glioblastoma: Strategy for poor-risk patients or hope for the future? Br. J. Radiol. 2012, 85, e770–e781. [Google Scholar] [CrossRef]
- Guo, L.; Li, X.; Chen, Y.; Liu, R.; Ren, C.; Du, S. The efficacy of hypofractionated radiotherapy (HFRT) with concurrent and adjuvant temozolomide in newly diagnosed glioblastoma: A meta-analysis. Cancer Radiother. 2021, 25, 182–190. [Google Scholar] [CrossRef]
- Sulman, E.P.; Ismaila, N.; Armstrong, T.S.; Tsien, C.; Batchelor, T.T.; Cloughesy, T.; Galanis, E.; Gilbert, M.; Gondi, V.; Lovely, M.; et al. Radiation Therapy for Glioblastoma: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Society for Radiation Oncology Guideline. J. Clin. Oncol. 2017, 35, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, R.S.; Patel, K.R.; Press, R.H.; Soltys, S.G.; Brown, P.D.; Mehta, M.P.; Asher, A.L.; Burri, S.H. Preoperative Vs Postoperative Radiosurgery For Resected Brain Metastases: A Review. Neurosurgery 2019, 84, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.R.; Burri, S.H.; Boselli, D.; Symanowski, J.T.; Asher, A.L.; Sumrall, A.; Fraser, R.W.; Press, R.H.; Zhong, J.; Cassidy, R.J.; et al. Comparing pre-operative stereotactic radiosurgery (SRS) to post-operative whole brain radiation therapy (WBRT) for resectable brain metastases: A multi-institutional analysis. J. Neurooncol. 2017, 131, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Faruqi, S.; Nordal, R.; Starreveld, Y.; Kelly, J.; Bowden, G.; Amanie, J.; Fairchild, A.; Lim, G.; Loewen, S.; et al. A phase III, multicenter, randomized controlled trial of preoperative versus postoperative stereotactic radiosurgery for patients with surgically resectable brain metastases. BMC Cancer 2022, 22, 1368. [Google Scholar] [CrossRef] [PubMed]
- Newcomb, E.W.; Demaria, S.; Lukyanov, Y.; Shao, Y.; Schnee, T.; Kawashima, N.; Lan, L.; Dewyngaert, J.K.; Zagzag, D.; McBride, W.H.; et al. The combination of ionizing radiation and peripheral vaccination produces long-term survival of mice bearing established invasive GL261 gliomas. Clin. Cancer Res. 2006, 12, 4730–4737. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; See, A.P.; Phallen, J.; Jackson, C.M.; Belcaid, Z.; Ruzevick, J.; Durham, N.; Meyer, C.; Harris, T.J.; Albesiano, E.; et al. Anti-PD-1 blockade and stereotactic radiation produce long-term survival in mice with intracranial gliomas. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 343–349. [Google Scholar] [CrossRef]
- NCCN Clinical Practice Guidelines in Oncology Version 1.2023. Central Nervous System Cancers. Available online: https://nccn.org (accessed on 13 September 2023).
- Waqar, M.; Roncaroli, F.; Djoukhadar, I.; Akkari, L.; O’Leary, C.; Hewitt, L.; Forte, G.; Jackson, R.; Hessen, E.; Withington, L.; et al. Study protocol: PreOperative Brain Irradiation in Glioblastoma (POBIG)—A phase I trial. Clin. Transl. Radiat. Oncol. 2023, 39, 100585. [Google Scholar] [CrossRef]
- Preoperative Radiosurgery for the Treatment of High Grade Glioma. The NeoGlioma Study. NCT05030298. Available online: https://clinicaltrials.gov (accessed on 15 September 2023).
- Kongkham, P.N.; Knifed, E.; Tamber, M.S.; Bernstein, M. Complications in 622 cases of frame-based stereotactic biopsy, a decreasing procedure. Can. J. Neurol. Sci. 2008, 35, 79–84. [Google Scholar] [CrossRef]
- Bleehen, N.M.; Stenning, S.P. A Medical Research Council trial of two radiotherapy doses in the treatment of grades 3 and 4 astrocytoma. Br. J. Cancer 1991, 64, 769–774. [Google Scholar] [CrossRef]
- Souhami, L.; Seiferheld, W.; Brachman, D.; Podgorsak, E.B.; Werner-Wasik, M.; Lustig, R.; Schultz, C.J.; Sause, W.; Okunieff, P.; Buckner, J.; et al. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: Report of Radiation Therapy Oncology Group 93-05 protocol. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 853–860. [Google Scholar] [CrossRef]
- Schaff, L.R.; Mellinghoff, I.K. Glioblastoma and Other Primary Brain Malignancies in Adults: A Review. JAMA 2023, 329, 574–587. [Google Scholar] [CrossRef] [PubMed]
- Roa, W.; Brasher, P.M.; Bauman, G.; Anthes, M.; Bruera, E.; Chan, A.; Fisher, B.; Fulton, D.; Gulavita, S.; Hao, C.; et al. Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: A prospective randomized clinical trial. J. Clin. Oncol. 2004, 22, 1583–1588. [Google Scholar] [CrossRef] [PubMed]
- Roa, W.; Kepka, L.; Kumar, N.; Sinaika, V.; Matiello, J.; Lomidze, D.; Hentati, D.; Guedes de Castro, D.; Dyttus-Cebulok, K.; Drodge, S.; et al. International Atomic Energy Agency Randomized Phase III Study of Radiation Therapy in Elderly and/or Frail Patients with Newly Diagnosed Glioblastoma Multiforme. J. Clin. Oncol. 2015, 33, 4145–4150. [Google Scholar] [CrossRef] [PubMed]
- Malmström, A.; Grønberg, B.H.; Marosi, C.; Stupp, R.; Frappaz, D.; Schultz, H.; Abacioglu, U.; Tavelin, B.; Lhermitte, B.; Hegi, M.E.; et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: The Nordic randomized, phase 3 trial. Lancet Oncol. 2012, 13, 916–926. [Google Scholar] [CrossRef]
- Perry, J.R.; Laperriere, N.; O’Callaghan, C.J.; Brandes, A.A.; Menten, J.; Phillips, C.; Fay, M.; Nishikawa, R.; Cairncross, J.G.; Roa, W.; et al. Short-Course Radiation plus Temozolomide in Elderly Patients with Glioblastoma. N. Engl. J. Med. 2017, 376, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Omuro, A.; Beal, K.; Gutin, P.; Karimi, S.; Correa, D.D.; Kaley, T.J.; DeAngelis, L.M.; Chan, T.A.; Gavrilovic, I.T.; Nolan, C.; et al. Phase II study of bevacizumab, temozolomide, and hypofractionated stereotactic radiotherapy for newly diagnosed glioblastoma. Clin. Cancer Res. 2014, 20, 5023–5031. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, M.G.; Azoulay, M.; Chang, S.D.; Gibbs, I.C.; Hancock, S.L.; Pollom, E.L.; Adler, J.R.; Harraher, C.; Li, G.; Gephart, M.H.; et al. Patterns of Progression in Patients with Newly Diagnosed Glioblastoma Treated with 5-mm Margins in a Phase ½ Trial of 5-Fraction Stereotactic Radiosurgery with Concurrent and Adjuvant Temozolomide. Pract. Radiat. Oncol. 2023, 13, e239–e245. [Google Scholar] [CrossRef]
- Guan, Y.; Pan, M.; Yang, J.; Lu, Q.; Han, L.; Liu, Y.; Li, J.; Zhu, H.; Gong, X.; Mei, G.; et al. A phase II open label, single arm study of hypofractionated stereotactic radiotherapy with chemoradiotherapy using intensity-modulated radiotherapy for newly diagnosed glioblastoma after surgery: The HSCK-010 trial protocol. BMC Cancer 2022, 22, 827. [Google Scholar] [CrossRef]
- Kazmi, F.; Soon, Y.Y.; Leong, Y.H.; Koh, W.Y.; Vellayappan, B. Re-irradiation for recurrent glioblastoma (GBM): A systematic review and meta-analysis. J. Neurooncol. 2019, 142, 79–90. [Google Scholar] [CrossRef]
- Tsien, C.I.; Pugh, S.L.; Dicker, A.P.; Raizer, J.J.; Matuszak, M.M.; Lallana, E.C.; Huang, J.; Algan, O.; Deb, N.; Portelance, L.; et al. NRG Oncology/RTOG1205: A Randomized Phase II Trial of Concurrent Bevacizumab and Reirradiation Versus Bevacizumab Alone as Treatment for Recurrent Glioblastoma. J. Clin. Oncol. 2023, 41, 1285–1295. [Google Scholar] [CrossRef]
- Bagley, S.; Shabason, J.; Mathew, D.; Kothari, S.; Oldridge, D.; Desai, A.; Lustig, R.; Kurtz, G.; Alonso-Basanta, M.; Chen, K.; et al. CTIM-35. A phase II study of GITR agonist incagn01876 and pd-1 inhibitor retifanlimab in combination with stereotactic radiotherapy in patients with recurrent glioblastoma. Neuro-Oncol. 2022, 24 (Suppl. 7), 69. [Google Scholar] [CrossRef]
- Chan, S.; Belmar, N.; Ho, S.; Rogers, B.; Stickler, M.; Graham, M.; Lee, E.; Tran, N.; Zhang, D.; Gupta, P.; et al. An anti-PD-1-GITR-L bispecific agonist induces GITR clustering-mediated T cell activation for cancer immunotherapy. Nat. Cancer 2022, 3, 337–354. [Google Scholar] [CrossRef] [PubMed]
- Montay-Gruel, P.; Acharya, M.M.; Gonçalves Jorge, P.; Petit, B.; Petridis, I.G.; Fuchs, P.; Leavitt, R.; Petersson, K.; Gondré, M.; Ollivier, J.; et al. Hypofractionated FLASH-RT as an Effective Treatment against Glioblastoma that Reduces Neurocognitive Side Effects in Mice. Clin. Cancer Res. 2021, 27, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Mascia, A.E.; Daugherty, E.C.; Zhang, Y.; Lee, E.; Xiao, Z.; Sertorio, M.; Woo, J.; Backus, L.R.; McDonald, J.M.; McCann, C.; et al. Proton FLASH Radiotherapy for the Treatment of Symptomatic Bone Metastases: The FAST-01 Nonrandomized Trial. JAMA Oncol. 2023, 9, 62–69, Erratum in JAMA Oncol. 2023, 9, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Favaudon, V.; Caplier, L.; Monceau, V.; Pouzoulet, F.; Sayarath, M.; Fouillade, C.; Poupon, M.-F.; Brito, I.; Hupé, P.; Bourhis, J.; et al. Ultrahigh dose-rate FLASH irradiation increases the differential response between normal and tumor tissue in mice. Sci. Transl. Med. 2014, 6, 245ra93. [Google Scholar] [CrossRef] [PubMed]
- Konradsson, E.; Liljedahl, E.; Gustafsson, E.; Adrian, G.; Beyer, S.; Ilaahi, S.E.; Petersson, K.; Ceberg, C.; Nittby Redebrandt, H. Comparable Long-Term Tumor Control for Hypofractionated FLASH Versus Conventional Radiation Therapy in an Immunocompetent Rat Glioma Model. Adv. Radiat. Oncol. 2022, 7, 101011. [Google Scholar] [CrossRef]
- Aerts, H.J. The Potential of Radiomic-Based Phenotyping in Precision Medicine: A Review. JAMA Oncol. 2016, 2, 1636–1642. [Google Scholar] [CrossRef]
- Randall, J.; Teo, P.T.; Lou, B.; Shah, J.; Patel, J.; Kamen, A.; Abazeed, M.E. Image-Based Deep Neural Network for Individualizing Radiotherapy Dose Is Transportable Across Health Systems. JCO Clin. Cancer Inf. 2023, 7, e2200100. [Google Scholar] [CrossRef]
- Li, Z.C.; Bai, H.; Sun, Q.; Zhao, Y.; Lv, Y.; Zhou, J.; Liang, C.; Chen, Y.; Liang, D.; Zheng, H. Multiregional radiomics profiling from multiparametric MRI: Identifying an imaging predictor of IDH1 mutation status in glioblastoma. Cancer Med. 2018, 7, 5999–6009. [Google Scholar] [CrossRef]
- Akbari, H.; Macyszyn, L.; Da, X.; Bilello, M.; Wolf, R.L.; Martinez-Lage, M.; Biros, G.; Alonso-Basanta, M.; O’Rourke, D.M.; Davatzikos, C. Imaging Surrogates of Infiltration Obtained Via Multiparametric Imaging Pattern Analysis Predict Subsequent Location of Recurrence of Glioblastoma. Neurosurgery 2016, 78, 572–580. [Google Scholar] [CrossRef]
- Personalized Treatment of Glioblastoma via Image-Guided Predictive Modeling of Recurrence: A Single-Arm, Single Institutional Pilot Prospective Study of Dose-Escalated Radiation Therapy. NCT03477513. Available online: https://clinicaltrials.gov (accessed on 22 September 2023).
| Study | Phase | Key Inclusion/Exclusion Criteria | Arms | Target Accrual | Key Endpoints |
|---|---|---|---|---|---|
| POBIG [18] | I | Age ≥ 18, ECOG PS 0–1, radiographically diagnosed GBM, surgical candidate, safe for pre-operative SRS, tumor allows for hot and cold spot delineation | 1 arm: Pre-operative SRS (6–14 Gy × 1 fx) → surgery → adjuvant RT (15 or 30 fractions) with concurrent + adjuvant TMZ | 18 patients | Prim: maximum tolerated dose and maximum tolerated SRS volume Sec: rate of surgical and SRS complications, PFS, OS, steroid dose after pre-operative SRS, concordance between MRI diagnosis and histological diagnosis |
| NeoGLIOMA [19] | I/IIA | Age ≥ 18, ECOG PS 0–2, clinical and radiographic evidence of HGG, surgical candidate, no prior cranial RT, safe for pre-operative SRS | 1. Pre-operative SRS (1 fx), surgery, 30 fraction CFRT, TMZ, ±TTF 2. Surgery, 30 fraction CFRT, TMZ, ±TTF | 40 patients | Prim: Rate of acute grade 3+ adverse events Sec: acute clinical toxicity, radiographic tumor control, rate of pseudoprogression, OS |
| Study | Inclusion Criteria | Randomization | Number of Patients | Key Outcomes (Arm 1 vs. Arm 2 ±vs. Arm 3) |
|---|---|---|---|---|
| Pre-Temozolomide Era | ||||
| UK MRC, 1991 [21] | Age ≥ 18, and ≤70, grade III/IV supratentorial astrocytoma (including GBM) | 1: 45 Gy/20 fx, post-operative 2: 60 Gy/30 fx, post-operative | Arm 1: 156 Arm 2: 318 Total: 474 | Median OS: 9 vs. 12 mo (p = 0.007) |
| RTOG 9305, 2004 [22] | Age ≥ 18, supratentorial GBM with post-op diameter ≤ 40 mm, KPS ≥ 60 | 1: EBRT + BCNU 2: SRS + EBRT + BCNU | Arm 1: 97 Arm 2: 89 Total: 186 | Median OS: 13.6 vs. 13.5 mo (p = 0.5711) 3-year OS: 13% vs. 9% (NS) Pattern of failure: 92.5% with component of local failure overall (NS between arms) 3 mo deterioration in MMSE: 35% vs. 25% (p = 0.21) |
| Roa et al., 2004 [24] | Age ≥ 60 years, histologically confirmed GBM, KPS ≥ 50 | 1: 60 Gy/30 fx 2: 40 Gy/15 fx | Arm 1: 51 Arm 2: 49 Total: 100 | Median OS: 5.1 vs. 5.6 mo (p = 0.57) Percentage with increase in post-treatment corticosteroids: 49% vs. 23% (p = 0.02) |
| Post-Temozolomide Era | ||||
| Malmström et al., 2012 [26] | Age ≥ 60, WHO PS ≤ 2, newly diagnosed GBM | 1. TMZ alone 2. 60 Gy/30 fx 3. 34 Gy/10 fx | Arm 1: 93 Arm 2: 124 Arm 3: 125 Total: 342 | Median OS: 8.3 vs. 6.0 vs. 7.5 mo (NS for arm 1 vs. 3, p = 0.001 for arm 1 vs. 2) Median OS (age ≥ 70): 9.0 vs. 5.2 vs. 7.0 mo (p < 0.0001 for arm 1 vs. 2, p = 0.02 for arm 2 vs. 3) Median OS (MGMT-methylated vs. non-methylated in arm 1): 9.7 vs. 6.7 mo (p = 0.02) Median OS (MGMT-methylated vs. non-methylated in arm 3): NS |
| Roa et al., 2015 [25] | Age ≥ 50 and KPS 50–70% or age ≥ 65 and KPS 80–100%, GBM | 1. 25 Gy/5 fx 2. 40 Gy/15 fx | Arm 1: 48 Arm 2: 50 Total: 98 | Median OS: 7.9 vs. 6.4 mo (p = 0.988) Median PFS: 4.2 vs. 4.2 mo (p = 0.716) QOL at 4 and 8 weeks post-treatment: NS |
| Perry et al., 2017 [27] | Age ≥ 65, newly histologically confirmed GBM, ECOG PS 0–2, receiving stable or decreasing dose of steroids | 1: 40.05 Gy/15 fx 2: 40.05 Gy/15 fx + concurrent and adjuvant TMZ | Arm 1: 281 Arm 2: 281 Total: 562 | Median OS: 7.6 vs. 9.3 mo (p < 0.001) Median OS (MGMT-methylated): 7.7 vs. 13.5 mo (p < 0.001) Median PFS: 3.9 vs. 5.3 mo (p < 0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, C.; Mogilevsky, C.; Belal, Z.; Kurtz, G.; Alonso-Basanta, M. Hypofractionation in Glioblastoma: An Overview of Palliative, Definitive, and Exploratory Uses. Cancers 2023, 15, 5650. https://doi.org/10.3390/cancers15235650
Jiang C, Mogilevsky C, Belal Z, Kurtz G, Alonso-Basanta M. Hypofractionation in Glioblastoma: An Overview of Palliative, Definitive, and Exploratory Uses. Cancers. 2023; 15(23):5650. https://doi.org/10.3390/cancers15235650
Chicago/Turabian StyleJiang, Cecilia, Casey Mogilevsky, Zayne Belal, Goldie Kurtz, and Michelle Alonso-Basanta. 2023. "Hypofractionation in Glioblastoma: An Overview of Palliative, Definitive, and Exploratory Uses" Cancers 15, no. 23: 5650. https://doi.org/10.3390/cancers15235650
APA StyleJiang, C., Mogilevsky, C., Belal, Z., Kurtz, G., & Alonso-Basanta, M. (2023). Hypofractionation in Glioblastoma: An Overview of Palliative, Definitive, and Exploratory Uses. Cancers, 15(23), 5650. https://doi.org/10.3390/cancers15235650





