Modern Techniques in Re-Irradiation for Locally Recurrent Rectal Cancer: A Systematic Review
Abstract
:Simple Summary
Abstract
1. Introduction
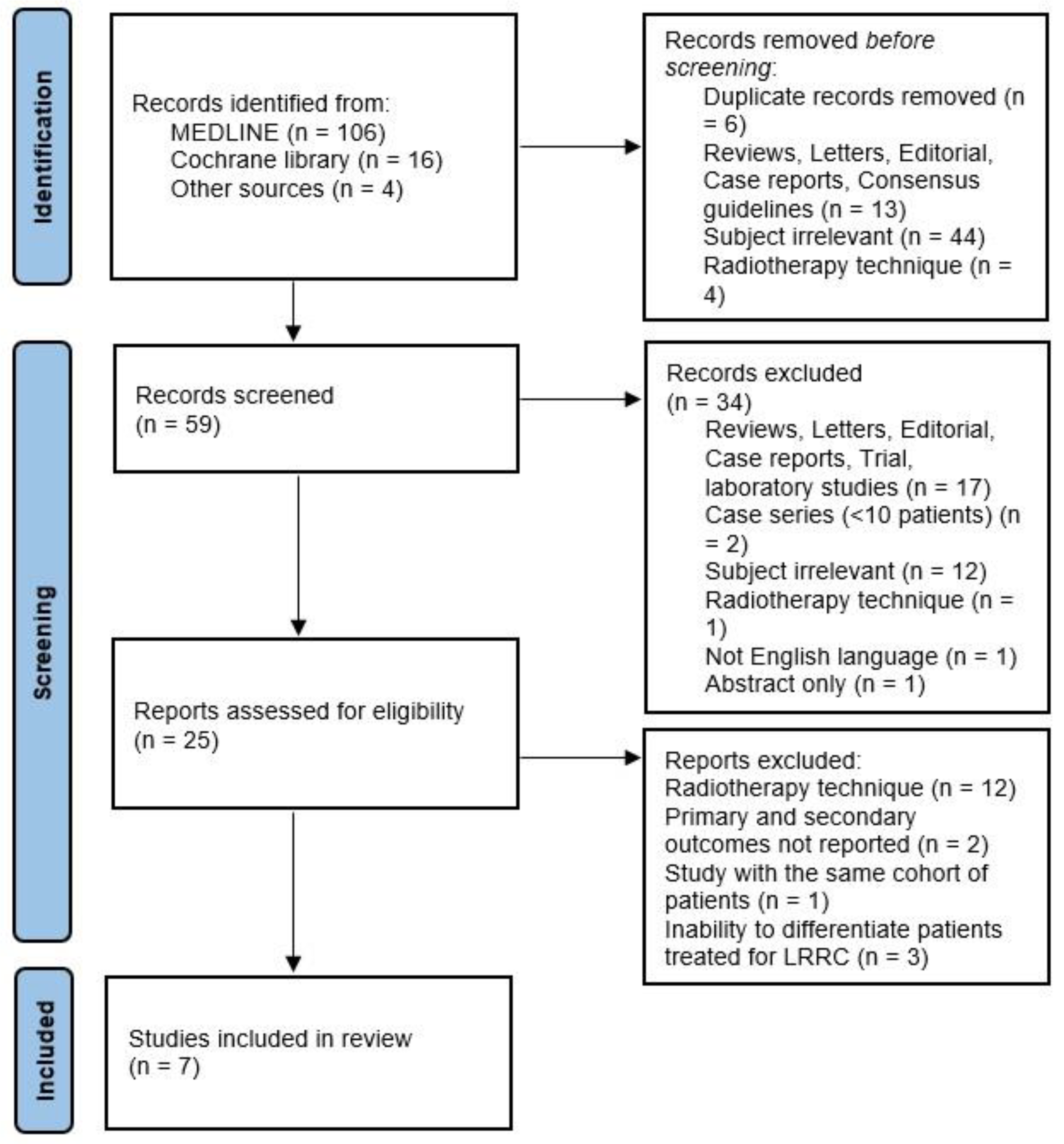
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.; Xu, P. Global Colorectal Cancer Burden in 2020 and Projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef]
- Das, P.; Skibber, J.M.; Rodriguez-Bigas, M.A.; Feig, B.W.; Chang, G.J.; Hoff, P.M.; Eng, C.; Wolff, R.A.; Janjan, N.A.; Delclos, M.E.; et al. Clinical and Pathologic Predictors of Locoregional Recurrence, Distant Metastasis, and Overall Survival in Patients Treated with Chemoradiation and Mesorectal Excision for Rectal Cancer. Am. J. Clin. Oncol. 2006, 29, 219–224. [Google Scholar] [CrossRef]
- Ngan, S.Y.; Burmeister, B.; Fisher, R.J.; Solomon, M.; Goldstein, D.; Joseph, D.; Ackland, S.P.; Schache, D.; McClure, B.; McLachlan, S.-A.; et al. Randomized Trial of Short-Course Radiotherapy versus Long-Course Chemoradiation Comparing Rates of Local Recurrence in Patients with T3 Rectal Cancer: Trans-Tasman Radiation Oncology Group Trial 01.04. J. Clin. Oncol. 2012, 30, 3827–3833. [Google Scholar] [CrossRef]
- Yu, T.-K.; Bhosale, P.R.; Crane, C.H.; Iyer, R.B.; Skibber, J.M.; Rodriguez-Bigas, M.A.; Feig, B.W.; Chang, G.J.; Eng, C.; Wolff, R.A.; et al. Patterns of Locoregional Recurrence After Surgery and Radiotherapy or Chemoradiation for Rectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 1175–1180. [Google Scholar] [CrossRef] [PubMed]
- Bhangu, A.; Ali, S.M.; Darzi, A.; Brown, G.; Tekkis, P. Meta-Analysis of Survival Based on Resection Margin Status Following Surgery for Recurrent Rectal Cancer. Color. Dis. 2012, 14, 1457–1466. [Google Scholar] [CrossRef]
- Alberda, W.J.; Verhoef, C.; Schipper, M.E.I.; Nuyttens, J.J.; Rothbarth, J.; de Wilt, J.H.W.; Burger, J.W.A. The Importance of a Minimal Tumor-Free Resection Margin in Locally Recurrent Rectal Cancer. Dis. Colon. Rectum 2015, 58, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Kusters, M.; Dresen, R.C.; Martijn, H.; Nieuwenhuijzen, G.A.; van de Velde, C.J.H.; van den Berg, H.A.; Beets-Tan, R.G.H.; Rutten, H.J.T. Radicality of Resection and Survival after Multimodality Treatment Is Influenced by Subsite of Locally Recurrent Rectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 1444–1449. [Google Scholar] [CrossRef]
- Lee, D.J.-K.; Sagar, P.M.; Sadadcharam, G.; Tan, K.-Y. Advances in Surgical Management for Locally Recurrent Rectal Cancer: How Far Have We Come? World J. Gastroenterol. 2017, 23, 4170. [Google Scholar] [CrossRef]
- Bouchard, P.; Efron, J. Management of Recurrent Rectal Cancer. Ann. Surg. Oncol. 2010, 17, 1343–1356. [Google Scholar] [CrossRef]
- Glimelius, B. Recurrent Rectal Cancer. The Pre-Irradiated Primary Tumour: Can More Radiotherapy Be Given? Color. Dis. 2003, 5, 501–503. [Google Scholar] [CrossRef]
- PelvEx Collaborative; Voogt, E.L.K.; Nordkamp, S.; Aalbers, A.G.J.; Buffart, T.; Creemers, G.J.; Marijnen, C.A.M.; Verhoef, C.; Havenga, K.; Holman, F.A.; et al. Induction Chemotherapy Followed by Chemoradiotherapy versus Chemoradiotherapy Alone as Neoadjuvant Treatment for Locally Recurrent Rectal Cancer: Study Protocol of a Multicentre, Open-Label, Parallel-Arms, Randomized Controlled Study (PelvEx II). BJS Open 2021, 5, zrab029. [Google Scholar] [CrossRef]
- Mantello, G.; Galofaro, E.; Caravatta, L.; Di Carlo, C.; Montrone, S.; Arpa, D.; Chiloiro, G.; De Paoli, A.; Donato, V.; Gambacorta, M.A.; et al. Pattern of Care for Re-Irradiation in Locally Recurrent Rectal Cancer: A National Survey on Behalf of the AIRO Gastrointestinal Tumors Study Group. Radiol. Med. 2023, 128, 869–876. [Google Scholar] [CrossRef]
- Das, S.; Patro, K.C.; Mukherji, A. Recovery and Tolerance of the Organs at Risk during Re-Irradiation. J. Curr. Oncol. 2018, 1, 23. [Google Scholar] [CrossRef]
- Abusaris, H.; Hoogeman, M.; Nuyttens, J.J. Re-Irradiation: Outcome, Cumulative Dose and Toxicity in Patients Retreated with Stereotactic Radiotherapy in the Abdominal or Pelvic Region. Technol. Cancer Res. Treat. 2012, 11, 591–597. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Tsai, C.J.; Jensen, G.; Eng, C.; Kopetz, S.; Overman, M.J.; Skibber, J.M.; Rodriguez-Bigas, M.; Chang, G.J.; You, Y.-Q.N.; et al. Hyperfractionated Accelerated Reirradiation for Rectal Cancer: An Analysis of Outcomes and Toxicity. Radiother. Oncol. 2017, 122, 146–151. [Google Scholar] [CrossRef]
- Guren, M.G.; Undseth, C.; Rekstad, B.L.; Brændengen, M.; Dueland, S.; Spindler, K.-L.G.; Glynne-Jones, R.; Tveit, K.M. Reirradiation of Locally Recurrent Rectal Cancer: A Systematic Review. Radiother. Oncol. 2014, 113, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, C.Y.; Koom, W.S.; Rim, C.H. Practical Effectiveness of Re-Irradiation with or without Surgery for Locoregional Recurrence of Rectal Cancer: A Meta-Analysis and Systematic Review. Radiother. Oncol. 2019, 140, 10–19. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.Y.; Takiyama, H.; Kang, J.H.; Chang, J.S.; Min, B.S.; Tsuji, H.; Yamada, S.; Koom, W.S. Comparison of Clinical Outcomes between Carbon Ion Radiotherapy and X-Ray Radiotherapy for Reirradiation in Locoregional Recurrence of Rectal Cancer. Sci. Rep. 2022, 12, 1845. [Google Scholar] [CrossRef]
- Yamada, S.; Takiyama, H.; Isozaki, Y.; Shinoto, M.; Ebner, D.K.; Koto, M.; Tsuji, H.; Miyauchi, H.; Sekimoto, M.; Ueno, H.; et al. Carbon Ion Radiotherapy for Locally Recurrent Rectal Cancer of Patients with Prior Pelvic Irradiation. Ann. Surg. Oncol. 2022, 29, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Barcellini, A.; Vitolo, V.; Cobianchi, L.; Peloso, A.; Vanoli, A.; Mirandola, A.; Facoetti, A.; Fiore, M.R.; Iannalfi, A.; Vischioni, B.; et al. Re-Irradiation With Carbon Ion Radiotherapy for Pelvic Rectal Cancer Recurrences in Patients Previously Irradiated to the Pelvis. In Vivo 2020, 34, 1547–1553. [Google Scholar] [CrossRef]
- Habermehl, D.; Wagner, M.; Ellerbrock, M.; Büchler, M.W.; Jäkel, O.; Debus, J.; Combs, S.E. Reirradiation Using Carbon Ions in Patients with Locally Recurrent Rectal Cancer at HIT: First Results. Ann. Surg. Oncol. 2015, 22, 2068–2074. [Google Scholar] [CrossRef] [PubMed]
- Cai, G.; Zhu, J.; Hu, W.; Zhang, Z. Accelerated Hyperfractionated Intensity-Modulated Radiotherapy for Recurrent/Unresectable Rectal Cancer in Patients with Previous Pelvic Irradiation: Results of a Phase II Study. Radiat. Oncol. 2014, 9, 278. [Google Scholar] [CrossRef] [PubMed]
- Dagoglu, N.; Mahadevan, A.; Nedea, E.; Poylin, V.; Nagle, D. Stereotactic Body Radiotherapy (SBRT) Reirradiation for Pelvic Recurrence from Colorectal Cancer: SBRT for Recurrent Colorectal Cancer. J. Surg. Oncol. 2015, 111, 478–482. [Google Scholar] [CrossRef]
- DeFoe, S.; Bernard, M.; Rwigema, J.-C.; Heron, D.; Ozhasoglu, C.; Burton, S. Stereotactic Body Radiotherapy for the Treatment of Presacral Recurrences from Rectal Cancers. J. Can. Res. Ther. 2011, 7, 408. [Google Scholar] [CrossRef]
- Venkatesulu, B.P.; Giridhar, P.; Malouf, T.D.; Trifletti, D.M.; Krishnan, S. A Systematic Review of the Role of Carbon Ion Radiation Therapy in Recurrent Rectal Cancer. Acta Oncol. 2020, 59, 1218–1223. [Google Scholar] [CrossRef]
- Liu, X.; Li, Z.; Yin, Y. Clinical Application of MR-Linac in Tumor Radiotherapy: A Systematic Review. Radiat. Oncol. 2023, 18, 52. [Google Scholar] [CrossRef]
- Rammohan, N.; Randall, J.W.; Yadav, P. History of Technological Advancements towards MR-Linac: The Future of Image-Guided Radiotherapy. J. Clin. Med. 2022, 11, 4730. [Google Scholar] [CrossRef] [PubMed]
- Chiloiro, G.; Boldrini, L.; Meldolesi, E.; Re, A.; Cellini, F.; Cusumano, D.; Corvari, B.; Mantini, G.; Balducci, M.; Valentini, V.; et al. MR-Guided Radiotherapy in Rectal Cancer: First Clinical Experience of an Innovative Technology. Clin. Transl. Radiat. Oncol. 2019, 18, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Calvo, F.A.; Sole, C.V.; Rutten, H.J.; Dries, W.J.; Lozano, M.A.; Cambeiro, M.; Poortmans, P.; González-Bayón, L. ESTRO/ACROP IORT Recommendations for Intraoperative Radiation Therapy in Locally Recurrent Rectal Cancer. Clin. Transl. Radiat. Oncol. 2020, 24, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Ott, O.J.; Gani, C.; Lindner, L.H.; Schmidt, M.; Lamprecht, U.; Abdel-Rahman, S.; Hinke, A.; Weissmann, T.; Hartmann, A.; Issels, R.D.; et al. Neoadjuvant Chemoradiation Combined with Regional Hyperthermia in Locally Advanced or Recurrent Rectal Cancer. Cancers 2021, 13, 1279. [Google Scholar] [CrossRef] [PubMed]
- Antonietta, G.M. Radiotherapy & Total Neoadjuvant Therapy for Recurrent Rectal Cancer in Previously Irradiated Patients, an Italian Association for Radiotherapy and Clinical Oncology (AIRO)-GI Platform: A Multi-Centre Prospective Observational Study; Clinicaltrials.gov: Bethesda, MD, USA, 2023.
| Author | N° Patients | Country | Year | Study Design | Study Period | Patient Population | Re-RT Technique | Age, (Range) Years | Previous RT Dose (Range), Gy | Interval between RT (Range), mo | Re-RT Total Dose, Gy | Re-RT Fx. Dose, Gy | CTx. Rate (%) (Agent) | Surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chung SY | 35 | Japan-Korea | 2022 | R | 2005–2019 | LRRC | CIRT | 62 (37–76) | 50 (20–66) | NR | 70.4 Gy (RBE) 101.38 Gy in BED10 | 4.4 Gy [RBE] | Not administered | 0% |
| 31 | 29% 3D RT, 71% IMRT or Cyberknife | 60 (35–87) | 50.4 (45–60) | NR | 50 Gy (range 25–62.5 Gy) 60 Gy in BED10 | 68% * | 23% After, 13% Before re-RT | |||||||
| Yamada S | 77 | Japan | 2022 | R | 2005–2017 | LLRC | CIRT | 60 (37–76) | 50 (20–74) | 50 (13–157) | 70.4 Gy (RBE) | 4.4 Gy [RBE] | Not administered | 0% |
| Barcellini A | 14 | Italy | 2020 | R | LRRC | CIRT | 58.5 (34–78) | 45 (45–76) | 65 (14–139) | 60 Gy RBE (35–76.8) | 3 Gy RBE (3–4.8) | NR | 0% | |
| Habermehl D | 19 | Germany | 2014 | R | 2010–2013 | Unresectable LRRC | CIRT | 62 (14–76) | 50.4 (50.4–60.4) | 47.4 (17–110) | 36 to 51 Gy (RBE) | 3 Gy (RBE). | NR | NR |
| Cai G. | 22 | China | 2014 | Phase II | 2007–2012 | Unresectable LRRC | IMRT | 53 (40–68) | 48.6 (36–62) | 30 (18–93) | 39 | 1.3 BID | 81.8% (5-FU based) | 0% |
| Dagoglu N. | 18 | Turkey | 2015 | R | 2006–2012 | Pelvic RRC or CC | Cyberknife | 68 (32–93) | 50.4 (25–100.4) | 22 (15–336) | 25 (24–40) | 5 | Not administered | NR |
| DeFoe S.G. | 14 | USA | 2011 | R | 2003–2008 | Presacral RRC | Cyberknife | 65.5 (42–77) | 50.4 (20–81) | NR | 16 (12–36) | 12 | NR | NR |
| Author | ReRT Technique | Position | Fractionation | GTV | CTV | PTV | Recurred Tumor Size/Volume mm/cm3 (Range) | Site of Recurrence Number (%) | Dose Constraints |
|---|---|---|---|---|---|---|---|---|---|
| Chung S.Y. | CIRT | NR | Daily, 4 days a week | NR | GTV + 5 mm | NR | 25 (15-80) mm | Non-presacral, regional, nodal 17 (49%) Presacral 18 (51%) | Dose constraints of D2cc for the bowel and bladder were 44 Gy (RBE) and 50 Gy (RBE) in 16 fractions, respectively |
| 3D - IMRT or CyberKnife | NR | 25 Fx (range 3–33) | NR | NR | GTV of the recurred tumor plus a 0.5–3-cm margin | 30 (10-70) mm | Non-presacral, regional, nodal 22 (71%) Presacral 9 (29%) | NR | |
| Yamada S. | CIRT | NR | Daily, 4 days a week | Macroscopic tumor visible on CT, MRI, and PET imaging | GTV + 5 mm | CTV + 3-5 mm | 40 (14-110) mm | Presacral 29 (43.3%) Side wall 23 (34.3%) Perineal 15 (22.4%) | D2cc of the intestine and bladder were set at 50 Gy (RBE) and 60 Gy (RBE) in 16 fractions, and at 60 Gy (RBE) and 70 Gy (RBE) when combined with the dose distribution of the previous RT |
| Barcellini A. | CIRT | Prone | NR | Area of Contrast Enhancement on T1-Weighted MRI Images. | GTV + 5–10 mm | CTV + 3–10 mm | 154.63 (7.2–359.9) Volume cm3 | Presacral 10 (72%) Perineal 1 (7%) Perianal 1 (7%) Pre-Coccygeal 2 (14%) | NR |
| Habermehl D. | CIRT | Supine | NR | Macroscopic tumor visible in T1-weighted MRI | GTV + 5–10 mm | CTV 3–10 mm based on individual anatomical factors | 58 (12–112) mm | NR | NR |
| Cai G. | IMRT | Prone or supine | BID 5 days per week | Defined from CT, MRI, and/or PET/CT | NR | GTV + 2–3 cm | NR | Perirectal region 5 (20%) Presacral region 7 (28%) Internal iliac nodal region 7 (28%) Perineum 5 (20%) External iliac nodal region 1 (4%). | Small bowel: no more than 180 cc above 20 Gy, no more than 65 cc above 30 Gy, and maximum dose less than 40 Gy; Femoral heads: no more than40% volume above 25 Gy, no more than 25% volume above 30 Gy, and maximum dose less than 40 Gy; Bladder: no more than 40% volume above 25 Gy, no more than 15% volume above 30 Gy, and maximum dose less than 40 Gy |
| Dagoglu N. | Cyberknife | Supine | Daily | CT images | NR | NR | 90.1 cc (36.8–1029.4) volume cm3 | Presacral 5 (23.8%) Pelvic side wall 12 (57.1%) Central pelvis 2 (9.5%) Presacral + Pelvic side wall 1 (4.8%) Pubic area 1 (4.8%) | Protocol from institution |
| DeFoe S.G. | Cyberknife | Supine | 2–3 times per week or single dose | NR | Identical to GTV | GTV + 5 mm | 52.5 (19–110) volume cm3 | Presacral 100% | NR |
| Author | Re-RT Technique | Follow up (Range), Months | Progression-Free Survival (PFS) | Overall Survival (OS) | Local Control (LC) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (months) | 1-year PFS | 2-year PFS | 3-year PFS | 5-year PFS | Median (months) | 1-year OS | 2-year OS | 3-year OS | 5-year OS | Median (months) | 1-year LC | 2-year LC | 3-year LC | 5-year LC | |||
| Chung S.Y. | CIRT | 45.7 (7–148.4) | NR | NR | NR | NR | NR | Not achieved | 97% | 93% | 86.4% | 62% | NR | 94% | NR | 87% | 70% |
| 3D—IMRT or Cyberknife | 22.8 (7.2–148.4) | NR | NR | NR | NR | NR | 36.9 | 88.9% | 59% | 54.5% | 30% | NR | 89% | NR | 44% | 55% | |
| Yamada S. | CIRT | 45 (7–159) | 14 | 58% | 36% | 33% | 25% | 47 | 90% | 73% | 61% | 38% | NR | 85% | 75% | 69% | 62% |
| Barcellini A. | CIRT | 18 | m-PFS 14.4 (2–40) | 64.3% | 43% | NR | NR | NR | 100% | 76.2% | 76.2% | NR | 14.5 (2.4–49.5) | 78% | 52% | NR | NR |
| Habermehl D. | CIRT | 8 | NR | NR | NR | NR | NR | 9.1 | NR | NR | NR | NR | 20.6 * | 85% | NR | NR | NR |
| Cai G. | IMRT | 17 (2–59) | NR | 67% | 10.7% | NR | NR | 19 | 85.9% | 27.2% | NR | NR | 14 | NR | NR | NR | NR |
| Dagoglu N. | IMRT | 38 (6–36) | 38 | 80.2% | 68.7% | 61.1% | NR | 40 | 76.8% | 65.9% | 59.3% | NR | NR | 100% | 93.7% | 85.9% | NR |
| DeFoe S.G. | cyberknife | 16.5 (6–69) | NR | NR | NR | NR | NR | NR | 90% | 78.8% | NR | 60% | NR | 90.9% | 68.2% | 30% | NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantello, G.; Galofaro, E.; Bisello, S.; Chiloiro, G.; Romano, A.; Caravatta, L.; Gambacorta, M.A. Modern Techniques in Re-Irradiation for Locally Recurrent Rectal Cancer: A Systematic Review. Cancers 2023, 15, 4838. https://doi.org/10.3390/cancers15194838
Mantello G, Galofaro E, Bisello S, Chiloiro G, Romano A, Caravatta L, Gambacorta MA. Modern Techniques in Re-Irradiation for Locally Recurrent Rectal Cancer: A Systematic Review. Cancers. 2023; 15(19):4838. https://doi.org/10.3390/cancers15194838
Chicago/Turabian StyleMantello, Giovanna, Elena Galofaro, Silvia Bisello, Giuditta Chiloiro, Angela Romano, Luciana Caravatta, and Maria Antonietta Gambacorta. 2023. "Modern Techniques in Re-Irradiation for Locally Recurrent Rectal Cancer: A Systematic Review" Cancers 15, no. 19: 4838. https://doi.org/10.3390/cancers15194838
APA StyleMantello, G., Galofaro, E., Bisello, S., Chiloiro, G., Romano, A., Caravatta, L., & Gambacorta, M. A. (2023). Modern Techniques in Re-Irradiation for Locally Recurrent Rectal Cancer: A Systematic Review. Cancers, 15(19), 4838. https://doi.org/10.3390/cancers15194838








