An Integrated CT and MRI Imaging Model to Differentiate between Adrenal Adenomas and Pheochromocytomas
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
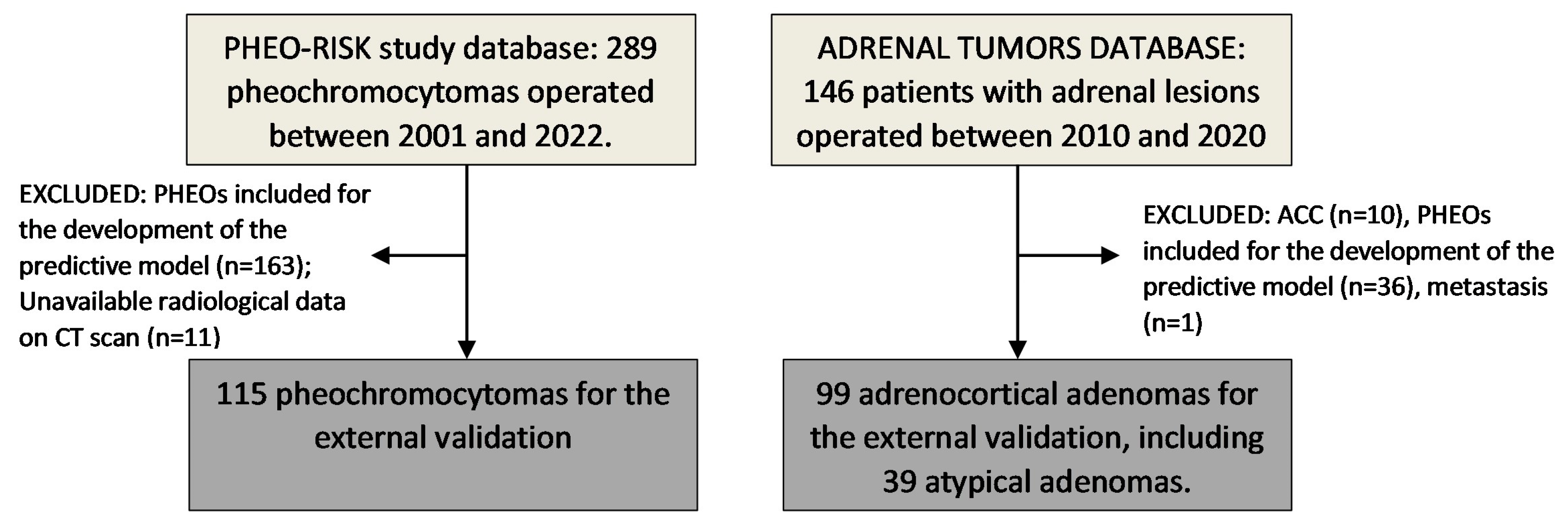
2.1. Study Population for the External Validation
2.2. Clinical, Hormonal, and Radiological Data
2.3. Statistical Analysis
3. Results
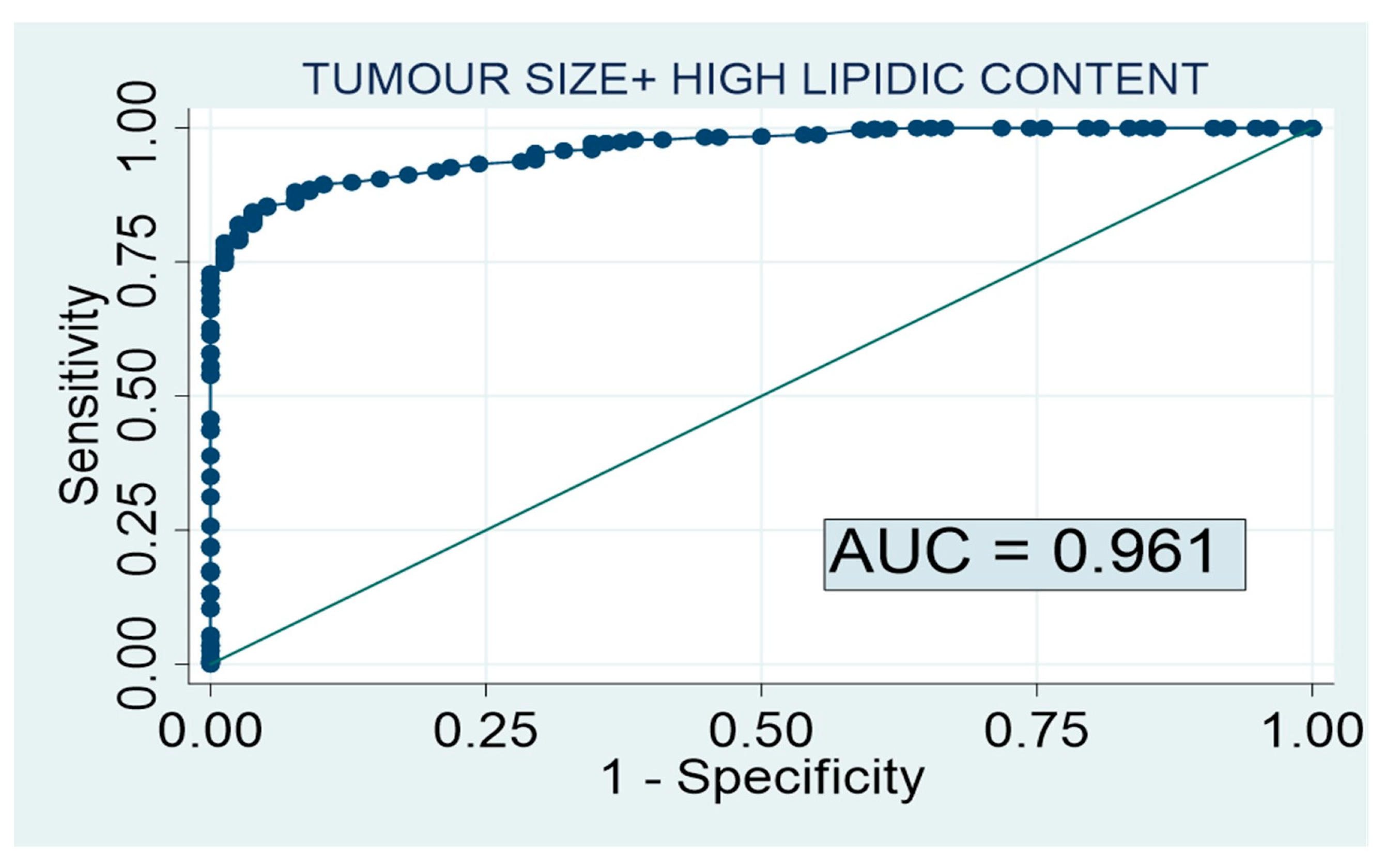
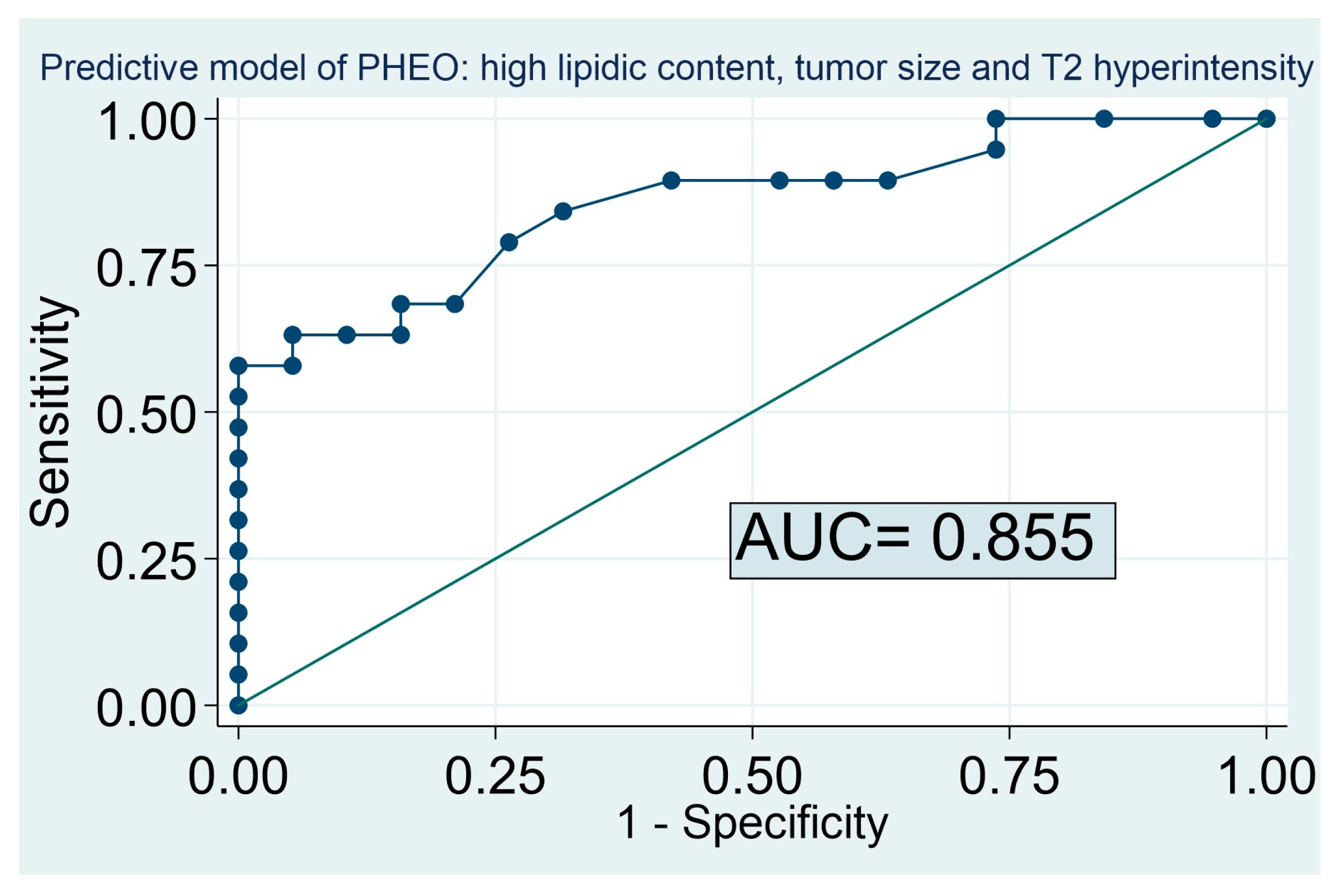
3.1. Predictive Model of PHEO
3.2. Baseline Characteristics of the Patients Included for the External Validation
3.3. External Validation of Our Previous Predictive Model and New Proposed Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Voltan, G.; Boscaro, M.; Armanini, D.; Scaroni, C.; Ceccato, F. A multidisciplinary approach to the management of adrenal incidentaloma. Expert Rev. Endocrinol. Metab. 2021, 16, 201–212. [Google Scholar] [CrossRef]
- Araujo-Castro, M.; Guevara, M.I.; Gutiérrez, M.C.; Ramírez, P.P.; Gimeno, P.G.; Hanzu, F.A.; Oliveira, C.L. Practical guide on the initial evaluation, follow-up, and treatment of adrenal incidentalomas Adrenal Diseases Group of the Spanish Society of Endocrinology and Nutrition. Endocrinol. Diabetes Y Nutr. 2020, 67, 408–419. [Google Scholar] [CrossRef]
- Fassnacht, M.; Arlt, W.; Bancos, I.; Dralle, H.; Newell-Price, J.; Sahdev, A.; Tabarin, A.; Terzolo, M.; Tsagarakis, S.; Dekkers, O.M. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2016, 175, G1–G34. [Google Scholar] [CrossRef]
- Araujo-Castro, M.; Núñez, M.A.S.; Marazuela, M. Autonomous cortisol secretion in adrenal incidentalomas. Endocrine 2019, 64, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Paschou, S.A.; Vryonidou, A.; Goulis, D.G. Adrenal incidentalomas: A guide to assessment, treatment and follow-up. Maturitas 2016, 92, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Bokuda, K.; Yatabe, M.; Seki, Y.; Ichihara, A. Clinical factors affecting spot urine fractionated metanephrines in patients suspected pheochromocytoma/paraganglioma. Hypertens. Res. 2020, 43, 543–549. [Google Scholar] [CrossRef]
- Kopetschke, R.; Slisko, M.; Kilisli, A.; Tuschy, U.; Wallaschofski, H.; Fassnacht, M.; Ventz, M.; Beuschlein, F.; Reincke, M.; Reisch, N.; et al. Frequent incidental discovery of phaeochromocytoma: Data from a German cohort of 201 phaeochromocytoma. Eur. J. Endocrinol. 2009, 161, 355–361. [Google Scholar] [CrossRef]
- Northcutt, B.G.; Raman, S.P.; Long, C.; Oshmyansky, A.R.; Siegelman, S.S.; Fishman, E.K.; Johnson, P.T. MDCT of Adrenal Masses: Can Dual-Phase Enhancement Patterns Be Used to Differentiate Adenoma and Pheochromocytoma? Am. J. Roentgenol. 2013, 201, 834–839. [Google Scholar] [CrossRef] [PubMed]
- Northcutt, B.G.; Trakhtenbroit, M.A.; Gomez, E.N.; Fishman, E.; Johnson, P.T. Adrenal Adenoma and Pheochromocytoma. J. Comput. Assist. Tomogr. 2016, 40, 194–200. [Google Scholar] [CrossRef]
- Mohammed, M.F.; Elbanna, K.Y.; Ferguson, D.; Harris, A.; Khosa, F. Pheochromocytomas Versus Adenoma: Role of Venous Phase CT Enhancement. Am. J. Roentgenol. 2018, 210, 1073–1078. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Oh, Y.L.; Park, S.Y. Distinguishing pheochromocytoma from adrenal adenoma by using modified computed tomography criteria. Abdom. Imaging 2020, 46, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Ojeda, C.M.; Dos Santos, V.G.; Lorca, J.; Ruz-Caracuel, I.; Pian, H.; Dehesa, A.S.; Revilla, F.J.B.; Araujo-Castro, M. Tumour size in adrenal tumours: Its importance in the indication of adrenalectomy and in surgical outcomes—A single-centre experience. J. Endocrinol. Investig. 2022, 45, 1999–2006. [Google Scholar] [CrossRef] [PubMed]
- Araujo-Castro, M.; Centeno, R.G.; Lázaro, C.R.; Ramírez, P.P.; Gimeno, P.G.; Rojas-Marcos, P.M.; Fernández-Ladreda, M.T.; Hualpa, J.C.P.; Núñez, M.S.; López-García, M.-C.; et al. Predictive model of pheochromocytoma based on the imaging features of the adrenal tumours. Sci. Rep. 2022, 12, 2671. [Google Scholar] [CrossRef]
- Barat, M.; Cottereau, A.-S.; Gaujoux, S.; Tenenbaum, F.; Sibony, M.; Bertherat, J.; Libé, R.; Gaillard, M.; Jouinot, A.; Assié, G.; et al. Adrenal Mass Characterization in the Era of Quantitative Imaging: State of the Art. Cancers 2022, 14, 569. [Google Scholar] [CrossRef]
- Song, J.H.; Chaudhry, F.S.; Mayo-Smith, W.W. The Incidental Adrenal Mass on CT: Prevalence of Adrenal Disease in 1,049 Consecutive Adrenal Masses in Patients with No Known Malignancy. Am. J. Roentgenol. 2008, 190, 1163–1168. [Google Scholar] [CrossRef]
- Gargan, M.L.; Lee, E.; O’Sullivan, M.; Egan, M.; Gibney, J.; Crowther, S.; Conlon, K.; Feeney, J. Imaging features of atypical adrenocortical adenomas: A radiological-pathological correlation. Br. J. Radiol. 2022, 95, 20210642. [Google Scholar] [CrossRef] [PubMed]
- Niu, Z.; Wang, J.; Yang, Y.; He, J.; Wang, S.; Xie, Z.; Shao, M.; Zhu, F. Risk prediction model establishment with tri-phasic CT image features for differential diagnosis of adrenal pheochromocytomas and lipid-poor adenomas: Grouping method. Front. Endocrinol. 2022, 13, 925577. [Google Scholar] [CrossRef]
- Goroshi, M.; Jadhav, S.S.; Sarathi, V.; Lila, A.R.; Patil, V.A.; Shah, R.; Hira, P.; Sharma, R.; Goroshi, S.; Fernandes, G.; et al. Radiological differentiation of phaeochromocytoma from other malignant adrenal masses: Importance of wash-in characteristics on multiphase CECT. Endocr. Connect. 2019, 8, 898–905. [Google Scholar] [CrossRef]
- An, Y.-Y.; Yang, G.-Z.; Lin, B.; Zhang, N.; Hou, H.-T.; Zhu, F.-M.; Tian, F.-J.; Wang, J. Differentiation of lipid-poor adenoma from pheochromocytoma on biphasic contrast-enhanced CT. Abdom. Imaging 2021, 46, 4353–4361. [Google Scholar] [CrossRef] [PubMed]
- Blake, M.A.; Kalra, M.K.; Maher, M.M.; Sahani, D.V.; Sweeney, A.T.; Mueller, P.R.; Hahn, P.F.; Boland, G.W. Pheochromocytoma: An Imaging Chameleon. RadioGraphics 2004, 24, S87–S99. [Google Scholar] [CrossRef]
- Varghese, J.; Hahn, P.; Papanicolaou, N.; Mayo-Smith, W.; Gaa, J.; Lee, M. MR differentiation of phaeochromocytoma from other adrenal lesions based on qualitative analysis of T2 relaxation times. Clin. Radiol. 1997, 52, 603–606. [Google Scholar] [CrossRef]
- Schieda, N.; Alrashed, A.; Flood, T.A.; Samji, K.; Shabana, W.; McInnes, M.D.F. Comparison of Quantitative MRI and CT Washout Analysis for Differentiation of Adrenal Pheochromocytoma From Adrenal Adenoma. Am. J. Roentgenol. 2016, 206, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Adam, S.Z.; Nikolaidis, P.; Horowitz, J.; Gabriel, H.; Hammond, N.A.; Patel, T.; Yaghmai, V.; Miller, F.H. Chemical Shift MR Imaging of the Adrenal Gland: Principles, Pitfalls, and Applications. RadioGraphics 2016, 36, 414–432. [Google Scholar] [CrossRef]
- Liu, J.; Xue, K.; Li, S.; Zhang, Y.; Cheng, J. Combined Diagnosis of Whole-Lesion Histogram Analysis of T1- and T2-Weighted Imaging for Differentiating Adrenal Adenoma and Pheochromocytoma: A Support Vector Machine-Based Study. Can. Assoc. Radiol. J. 2020, 72, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Yi, X.; Guan, X.; Chen, C.; Zhang, Y.; Zhang, Z.; Li, M.; Liu, P.; Yu, A.; Long, X.; Liu, L.; et al. Adrenal incidentaloma: Machine learning-based quantitative texture analysis of unenhanced CT can effectively differentiate sPHEO from lipid-poor adrenal adenoma. J. Cancer 2018, 9, 3577–3582. [Google Scholar] [CrossRef]
- Zhang, G.-M.; Shi, B.; Sun, H.; Jin, Z.-Y.; Xue, H.-D. Differentiating pheochromocytoma from lipid-poor adrenocortical adenoma by CT texture analysis: Feasibility study. Abdom. Imaging 2017, 42, 2305–2313. [Google Scholar] [CrossRef]
- Tu, W.; Abreu-Gomez, J.; Udare, A.; Alrashed, A.; Schieda, N. Utility of T2-weighted MRI to Differentiate Adrenal Metastases from Lipid-Poor Adrenal Adenomas. Radiol. Imaging Cancer 2020, 2, e200011. [Google Scholar] [CrossRef]
- Gerson, R.; Tu, W.; Abreu-Gomez, J.; Udare, A.; McPhedran, R.; Ramsay, T.; Schieda, N. Evaluation of the T2-weighted (T2W) adrenal MRI calculator to differentiate adrenal pheochromocytoma from lipid-poor adrenal adenoma. Eur. Radiol. 2022, 32, 8247–8255. [Google Scholar] [CrossRef] [PubMed]
- Romeo, V.; Maurea, S.; Cuocolo, R.; Petretta, M.; Mainenti, P.P.; Verde, F.; Coppola, M.; Dell’Aversana, S.; Brunetti, A. Characterization of Adrenal Lesions on Unenhanced MRI Using Texture Analysis: A Machine-Learning Approach. J. Magn. Reson. Imaging 2018, 48, 198–204. [Google Scholar] [CrossRef]
- Stanzione, A.; Cuocolo, R.; Verde, F.; Galatola, R.; Romeo, V.; Mainenti, P.P.; Aprea, G.; Guadagno, E.; Caro, M.D.B.D.; Maurea, S. Handcrafted MRI radiomics and machine learning: Classification of indeterminate solid adrenal lesions. Magn. Reson. Imaging 2021, 79, 52–58. [Google Scholar] [CrossRef]
| PHEO (n = 115) | ADENOMA (n = 99) | p Value | |
|---|---|---|---|
| Clinical and Hormonal Data | |||
| Age (years) | 49.7 ± 18.06 | 55.9 ± 11.20 | 0.004 |
| Female sex | 47.0% (n = 54) | 39.4% (n = 39) | 0.266 |
| Hypertension | 50.4% (n = 58) | 63.6% (n = 63) | 0.052 |
| Type 2 diabetes | 25.2% (n = 29) | 30.3% (n = 30) | 0.406 |
| Dyslipidemia | 29.6% (n = 32) | 28.3% (n = 28) | 0.831 |
| Cardiovascular events | 10.4% (n = 12) | 3.3% (n = 3) | 0.034 |
| Cerebrovascular events | 5.4% (n = 6) | 3.1% (n = 3) | 0.404 |
| Obesity | 19.1% (n = 22) | 8.1% (n = 8) | 0.020 |
| Systolic blood pressure (mmHg) | 137.7 ± 22.20 | 137.9 ± 11.91 | 0.952 |
| Diastolic blood pressure (mmHg) | 81.2 ± 14.65 | 79.8 ± 10.09 | 0.425 |
| Body mass index (kg/m2) | 26.4 ± 4.87 | 26.4 ± 3.17 | 0.973 |
| Urinary metanephrine (mcg/24 h) | 2521.4 ± 5405.26 | 339.2 ± 133.11 | <0.001 |
| Unenhanced CT scan | |||
| Tumor size (mm) | 52.0 ± 31.80 | 37.0 ± 19.47 | <0.001 |
| Tumor size > 40 mm | 61.7% (n = 66/107) | 47.5% (n = 47/99) | 0.041 |
| Hounsfield Units (n = 86) | 45.3 ± 27.3 | 29.9 ± 31.89 | 0.035 |
| Hounsfield Units >10 (n = 86) | 97.1% (n = 34/35) | 65.0% (n = 39/60) | <0.001 |
| Bilaterality | 5.1% (n = 5/99) | 6.1% (n = 6/99) | 0.756 |
| Necrosis | 20.2% (n = 18/89) | 2.2% (n = 2/90) | <0.001 |
| Calcifications | 6.6% (n = 5/76) | 16.7% (n = 15/90) | 0.047 |
| High lipid content | 1.3% (n = 1/75) | 26.7% (n = 24/90) | <0.001 |
| MRI evaluation | |||
| Loss of signal in the “out of phase” sequence | 7.1% (n = 2/28) | 72.7% (n = 24/33) | <0.001 |
| Hyperintensity in T2 sequence | 64.9% (n = 24/37) | 15.2% (n = 5/33) | <0.001 |
| Tumour Size | <10 mm | 10–20 mm | 21–30 mm | 31–40 mm | 41–50 mm | >50 mm | |
|---|---|---|---|---|---|---|---|
| Lipid Content | |||||||
| High | 1.1% | 1.6% | 2.4% | 3.5% | 5.1% | 7.3% | |
| Low | 23.1% | 30.7% | 39.7% | 49.4% | 59.1% | 68.2% | |
| HYPERINTENSITY IN T2 MRI SEQUENCE | |||||||
| Tumour Size | <10 mm | 10–20 mm | 21–30 mm | 31–40 mm | 41–50 mm | >50 mm | |
| Lipid Content | |||||||
| Low | 37.2% | 72.4% | 92.1% | 98.1% | 99.6% | 99.9% | |
| ABSCENSE OF HYPERINTENSITY IN T2 MRI SEQUENCE | |||||||
| Tumour Size | <10 mm | 10–20 mm | 21–30 mm | 31–40 mm | 41–50 mm | >50 mm | |
| Lipid Content | |||||||
| Low | 0.1% | 0.3% | 1.2% | 5.2% | 19.5% | 51.8% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araujo-Castro, M.; García Sanz, I.; Mínguez Ojeda, C.; Calatayud, M.; Hanzu, F.A.; Mora, M.; Vicente Delgado, A.; Carrera, C.B.; de Miguel Novoa, P.; del Carmen López García, M.; et al. An Integrated CT and MRI Imaging Model to Differentiate between Adrenal Adenomas and Pheochromocytomas. Cancers 2023, 15, 3736. https://doi.org/10.3390/cancers15143736
Araujo-Castro M, García Sanz I, Mínguez Ojeda C, Calatayud M, Hanzu FA, Mora M, Vicente Delgado A, Carrera CB, de Miguel Novoa P, del Carmen López García M, et al. An Integrated CT and MRI Imaging Model to Differentiate between Adrenal Adenomas and Pheochromocytomas. Cancers. 2023; 15(14):3736. https://doi.org/10.3390/cancers15143736
Chicago/Turabian StyleAraujo-Castro, Marta, Iñigo García Sanz, César Mínguez Ojeda, María Calatayud, Felicia A. Hanzu, Mireia Mora, Almudena Vicente Delgado, Concepción Blanco Carrera, Paz de Miguel Novoa, María del Carmen López García, and et al. 2023. "An Integrated CT and MRI Imaging Model to Differentiate between Adrenal Adenomas and Pheochromocytomas" Cancers 15, no. 14: 3736. https://doi.org/10.3390/cancers15143736
APA StyleAraujo-Castro, M., García Sanz, I., Mínguez Ojeda, C., Calatayud, M., Hanzu, F. A., Mora, M., Vicente Delgado, A., Carrera, C. B., de Miguel Novoa, P., del Carmen López García, M., Manjón-Miguélez, L., Rodríguez de Vera Gómez, P., del Castillo Tous, M., Barahona San Millán, R., Recansens, M., Fernández-Ladreda, M. T., Valdés, N., Gracia Gimeno, P., Robles Lazaro, C., ... Herrera-Martínez, A. (2023). An Integrated CT and MRI Imaging Model to Differentiate between Adrenal Adenomas and Pheochromocytomas. Cancers, 15(14), 3736. https://doi.org/10.3390/cancers15143736









