DICER1 Syndrome: A Multicenter Surgical Experience and Systematic Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
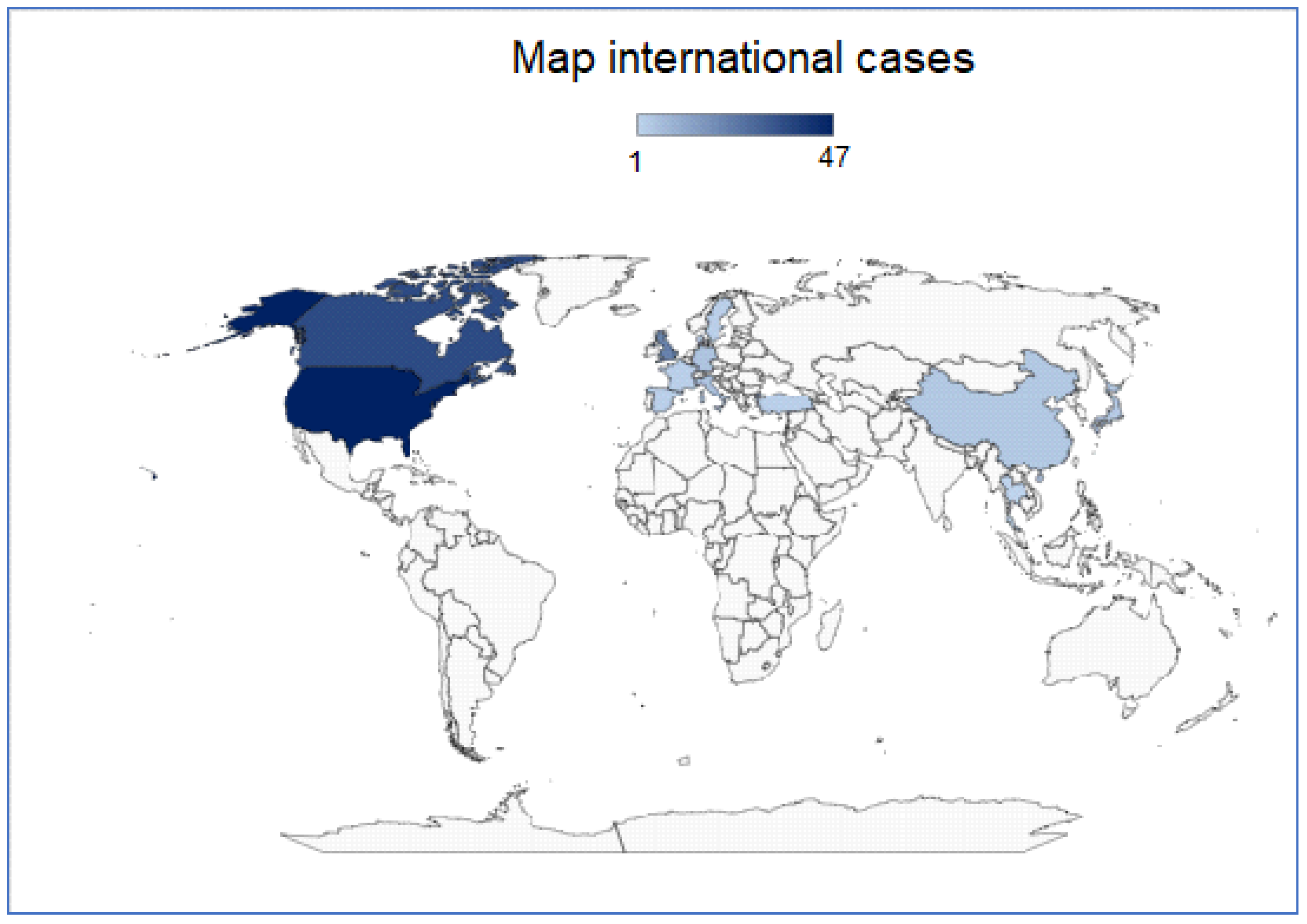
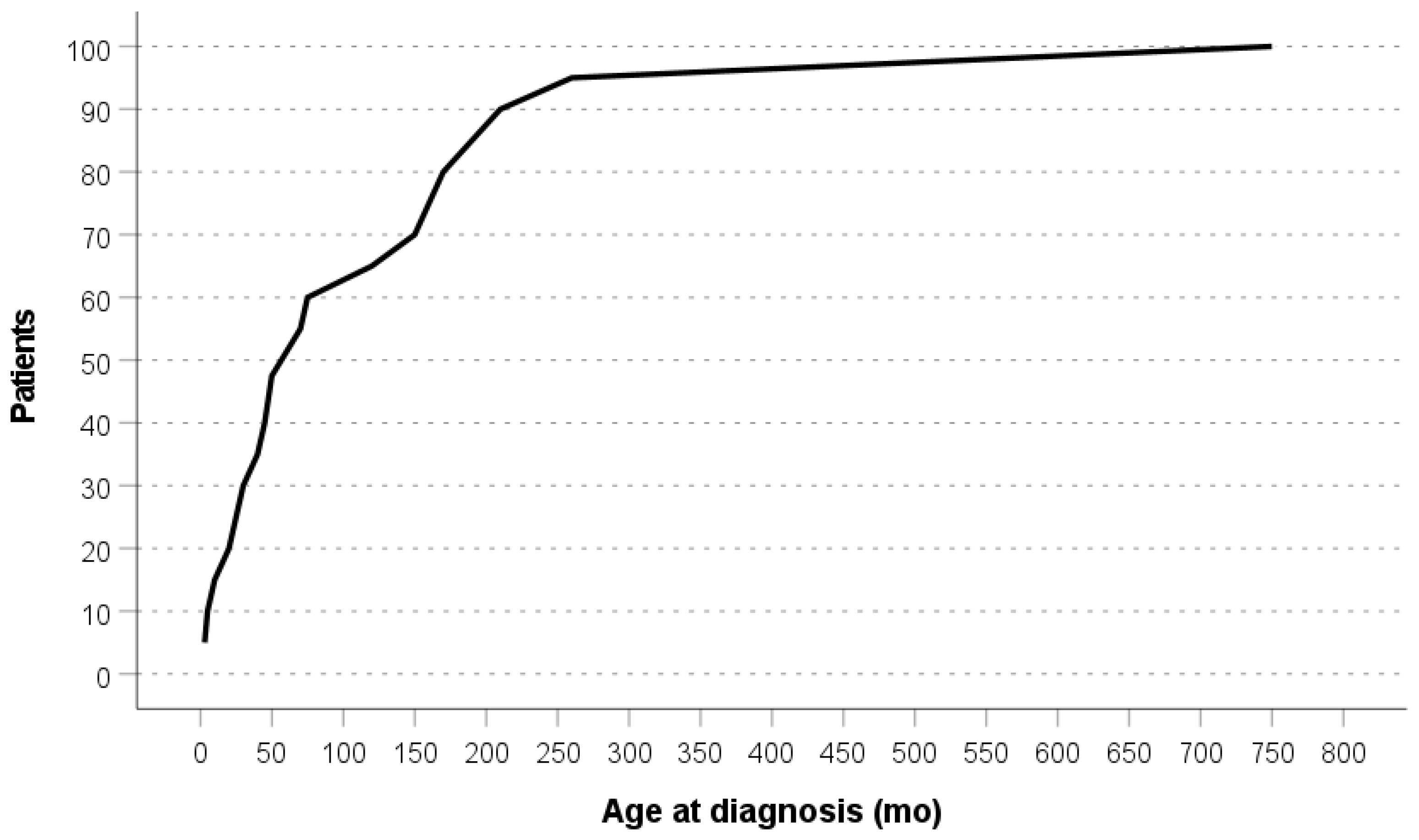
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Robertson, J.C.; Jorcyk, C.L.; Oxford, J.T. DICER1 Syndrome: DICER1 Mutations in Rare Cancers. Cancers 2018, 10, 143. [Google Scholar] [CrossRef]
- Hořínová, V.; Drábová, K.; Nosková, H.; Bajčiová, V.; Šoukalová, J.; Černá, L.; Hůrková, V.; Slabý, O.; Štěrba, J. DICER1 Syndrome. Syndrom DICER1. Klin. Onkol. 2019, 32, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Field, A.; Schultz, K.A.P.; Hill, D.A.; Stewart, D.R. The prevalence of DICER1 pathogenic variation in population databases. Int. J. Cancer 2017, 141, 2030–2036. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Schultz, K.A.P.; Hill, D.A.; Stewart, D.R. The prevalence of germline DICER1 pathogenic variation in cancer populations. Mol. Genet. Genom. Med. 2019, 7, e555. [Google Scholar] [CrossRef] [PubMed]
- González, I.A.; Stewart, D.R.; Schultz, K.A.P.; Field, A.P.; Hill, D.A.; Dehner, L.P. DICER1 tumor predisposition syndrome: An evolving story initiated with the pleuropulmonary blastoma. Mod. Pathol. 2022, 35, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Brenneman, M.; Field, A.; Yang, J.; Williams, G.; Doros, L.; Rossi, C.; Schultz, K.A.; Rosenberg, A.; Ivanovich, J.; Turner, J.; et al. Temporal order of RNase IIIb and loss-of-function mutations during development determines phenotype in pleuropulmonary blastoma/DICER1 syndrome: A unique variant of the two-hit tumor suppression model. F1000Res 2018, 4, 214. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, X.H.; Wang, C.X.; Liu, B.; Fan, X.S.; Wen, J.J.; Shi, Q.L.; Zhou, X.J. Dysregulation of microRNA biosynthesis enzyme Dicer plays an important role in gastric cancer progression. Int. J. Clin. Exp. Pathol. 2014, 7, 1702–1707. [Google Scholar]
- Song, M.S.; Rossi, J.J. Molecular mechanisms of Dicer: Endonuclease and enzymatic activity. Biochem. J. 2017, 474, 1603–1618. [Google Scholar] [CrossRef] [PubMed]
- Thunders, M.; Delahunt, B. Gene of the month: DICER1: Ruler and controller. J. Clin. Pathol. 2021, 74, 69–72. [Google Scholar] [CrossRef]
- Zhang, L.; Huang, J.; Yang, N.; Greshock, J.; Megraw, M.S.; Giannakakis, A.; Liang, S.; Naylor, T.L.; Barchetti, A.; Ward, M.R.; et al. MicroRNAs exhibit high frequency genomic alterations in human cancer. Proc. Natl. Acad. Sci. USA 2006, 103, 9136–9141. [Google Scholar] [CrossRef]
- de Kock, L.; Sabbaghian, N.; Soglio, D.B.; Guillerman, R.P.; Park, B.K.; Chami, R.; Deal, C.L.; Priest, J.R.; Foulkes, W.D. Exploring the association Between DICER1 mutations and differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 2014, 99, E1072–E1077. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.R.; Best, A.F.; Williams, G.M.; Harney, L.A.; Carr, A.G.; Harris, A.K.; Kratz, C.P.; Dehner, L.P.; Messinger, Y.H.; Rosenberg, P.S. Neoplasm Risk Among Individuals With a Pathogenic Germline Variant in DICER1. J. Clin. Endocrinol. Metab. 2019, 37, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Ali Syeda, Z.; Langden, S.S.S.; Munkhzul, C.; Lee, M.; Song, S.J. Regulatory Mechanism of MicroRNA Expression in Cancer. Int. J. Mol. Sci. 2020, 21, 1723. [Google Scholar] [CrossRef] [PubMed]
- Bardón-Cancho, E.J.; Haro-Díaz, A.; Alonso-García-de la Rosa, F.J.; Huerta-Aragonés, J.; García-Morín, M.; González-Martínez, F.; Garrido-Colino, C. DICER1 mutation and tumors associated with a familial tumor predisposition syndrome: Practical considerations. Fam. Cancer 2017, 16, 291–294. [Google Scholar] [CrossRef]
- Wu, M.K.; Cotter, M.B.; Pears, J.; McDermott, M.B.; Fabian, M.R.; Foulkes, W.D.; O’Sullivan, M.J. Tumor progression in DICER1-mutated cystic nephroma-witnessing the genesis of anaplastic sarcoma of the kidney. Hum. Pathol. 2016, 53, 114–120. [Google Scholar] [CrossRef]
- de Kock, L.; Sabbaghian, N.; Plourde, F.; Srivastava, A.; Weber, E.; Bouron-Dal Soglio, D.; Hamel, N.; Choi, J.H.; Park, S.H.; Deal, C.L. Pituitary blastoma: A pathognomonic feature of germ-line DICER1 mutations. Acta Neuropathol. 2014, 128, 111–122. [Google Scholar] [CrossRef]
- Venger, K.; Elbracht, M.; Carlens, J.; Deutz, P.; Zeppernick, F.; Lassay, L.; Kratz, C.; Zenker, M.; Kim, J.; Stewart, D.R.; et al. Unusual phenotypes in patients with a pathogenic germline variant in DICER1. Fam. Cancer 2021. [Google Scholar] [CrossRef]
- Kaspar, C.; Reis, H.; Stehling, F.; Dirksen, U.; Hadaschik, B.A.; Rehme, C. Zystisches Nephrom bei einem 15 Monate alten Patienten mit DICER1-Mutation [Cystic nephroma in a 15-month-old boy with DICER1 mutation]. Der Urologe. Ausg. A. 2021, 60, 776–779. [Google Scholar] [CrossRef]
- Pontén, E.; Frisk, S.; Taylan, F.; Vaz, R.; Wessman, S.; de Kock, L.; Pal, N.; Foulkes, W.D.; Lagerstedt-Robinson, K.; Nordgren, A. A complex DICER1 syndrome phenotype associated with a germline pathogenic variant affecting the RNase IIIa domain of DICER1. J. Med. Genet. 2022, 59, 141–146. [Google Scholar] [CrossRef]
- Hammad, R.; Lo, W.; Chen, H.; Shroff, M.; Malkin, D.; Villani, A.; Denburg, A. Congenital midline spinal hamartoma in an infant with DICER1 syndrome: A case report. Front. Oncol. 2022, 12, 963768. [Google Scholar] [CrossRef]
- Hill, D.A.; Ivanovich, J.; Priest, J.R.; Gurnett, C.A.; Dehner, L.P.; Desruisseau, D.; Jarzembowski, J.A.; Wikenheiser-Brokamp, K.A.; Suarez, B.K.; Whelan, A.J. DICER1 mutations in familial pleuropulmonary blastoma. Science 2009, 325, 965. [Google Scholar] [CrossRef] [PubMed]
- McCluggage, W.G.; Apellaniz-Ruiz, M.; Chong, A.L.; Hanley, K.Z.; Velázquez Vega, J.E.; McVeigh, T.P.; Foulkes, W.D. Embryonal Rhabdomyosarcoma of the Ovary and Fallopian Tube: Rare Neoplasms Associated with Germline and Somatic DICER1 Mutations. Am. J. Surg. Pathol. 2020, 44, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Darbinyan, A.; Morotti, R.; Cai, G.; Prasad, M.L.; Christison-Lagay, E.; Dinauer, C.; Adeniran, A.J. Cytomorphologic features of thyroid disease in patients with DICER1 mutations: A report of cytology-histopathology correlation in 7 patients. Cancer Cytopathol. 2020, 128, 746–756. [Google Scholar] [CrossRef] [PubMed]
- Bailey, K.M.; Jacobs, M.F.; Anderson, B.; Rabah, R.; Wu, Y.M.; Else, T.; Mody, R.J. DICER1 Mutations in the Era of Expanding Integrative Clinical Sequencing in Pediatric Oncology. JCO Precis. Oncol. 2019, 3, PO.18.00172. [Google Scholar] [CrossRef]
- Stewart, D.R.; Messinger, Y.; Williams, G.M.; Yang, J.; Field, A.; Schultz, K.A.; Harney, L.A.; Doros, L.A.; Dehner, L.P.; Hill, D.A. Nasal chondromesenchymal hamartomas arise secondary to germline and somatic mutations of DICER1 in the pleuropulmonary blastoma tumor predisposition disorder. Hum. Genet. 2014, 133, 1443–1450. [Google Scholar] [CrossRef]
- Azzollini, J.; Ferrari, A.; Stracuzzi, A.; Chiaravalli, S.; Terenziani, M.; Spreafico, F.; Grasso, M.; Collini, P.; Pensotti, V.; Massimino, M.; et al. Clinical heterogeneity and reduced penetrance in DICER1 syndrome: A report of three families. Tumori 2021, 107, NP144–NP148. [Google Scholar] [CrossRef]
- Slade, I.; Bacchelli, C.; Davies, H.; Murray, A.; Abbaszadeh, F.; Hanks, S.; Barfoot, R.; Burke, A.; Chisholm, J.; Hewitt, M.; et al. DICER1 syndrome: Clarifying the diagnosis, clinical features and management implications of a pleiotropic tumour predisposition syndrome. J. Med. Genet. 2011, 48, 273–278. [Google Scholar] [CrossRef]
- Rio Frio, T.; Bahubeshi, A.; Kanellopoulou, C.; Hamel, N.; Niedziela, M.; Sabbaghian, N.; Pouchet, C.; Gilbert, L.; O’Brien, P.K.; Serfas, K.; et al. DICER1 mutations in familial multinodular goiter with and without ovarian Sertoli-Leydig cell tumors. JAMA 2011, 305, 68–77. [Google Scholar] [CrossRef]
- Haley, M.; Bindal, P.; McAuliffe, A.; Vredenburgh, J. A family with Sertoli-Leydig cell tumour, multinodular goiter, and DICER1 mutation. Curr. Oncol. 2019, 26, 183–185. [Google Scholar] [CrossRef]
- Warren, M.; Hiemenz, M.C.; Schmidt, R.; Shows, J.; Cotter, J.; Toll, S.; Parham, D.M.; Biegel, J.A.; Mascarenhas, L.; Shah, R. Expanding the spectrum of dicer1-associated sarcomas. Mod. Pathol. 2020, 33, 164–174. [Google Scholar] [CrossRef]
- Miyama, Y.; Makise, N.; Miyakawa, J.; Kume, H.; Fukayama, M.; Ushiku, T. An autopsy case of prostatic rhabdomyosarcoma with DICER1 hotspot mutation. Pathol. Int. 2021, 71, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Foulkes, W.D.; Bahubeshi, A.; Hamel, N.; Pasini, B.; Asioli, S.; Baynam, G.; Choong, C.S.; Charles, A.; Frieder, R.P.; Dishop, M.K.; et al. Extending the phenotypes associated with DICER1 mutations. Hum. Mutat. 2011, 32, 1381–1384. [Google Scholar] [CrossRef] [PubMed]
- Bahubeshi, A.; Bal, N.; Rio Frio, T.; Hamel, N.; Pouchet, C.; Yilmaz, A.; Bouron-Dal Soglio, D.; Williams, G.M.; Tischkowitz, M.; Priest, J.R.; et al. Germline DICER1 mutations and familial cystic nephroma. J. Med. Genet. 2010, 47, 863–866. [Google Scholar] [CrossRef] [PubMed]
- Doros, L.; Yang, J.; Dehner, L.; Rossi, C.T.; Skiver, K.; Jarzembowski, J.A.; Messinger, Y.; Schultz, K.A.; Williams, G.; André, N.; et al. DICER1 mutations in embryonal rhabdomyosarcomas from children with and without familial PPB-tumor predisposition syndrome. Pediatr. Blood Cancer 2012, 59, 558–560. [Google Scholar] [CrossRef]
- Sabbaghian, N.; Hamel, N.; Srivastava, A.; Albrecht, S.; Priest, J.R.; Foulkes, W.D. Germline DICER1 mutation and associated loss of heterozygosity in a pineoblastoma. J. Med. Genet. 2012, 49, 417–419. [Google Scholar] [CrossRef]
- de Kock, L.; Plourde, F.; Carter, M.T.; Hamel, N.; Srivastava, A.; Meyn, M.S.; Arseneau, J.; Bouron-Dal Soglio, D.; Foulkes, W.D. Germ-line and somatic DICER1 mutations in a pleuropulmonary blastoma. Pediatr. Blood Cancer 2013, 60, 2091–2092. [Google Scholar] [CrossRef]
- Sabbaghian, N.; Srivastava, A.; Hamel, N.; Plourde, F.; Gajtko-Metera, M.; Niedziela, M.; Foulkes, W.D. Germ-line deletion in DICER1 revealed by a novel MLPA assay using synthetic oligonucleotides. Pediatr. Blood Cancer 2014, 22, 564–567. [Google Scholar] [CrossRef]
- Darrat, I.; Bedoyan, J.K.; Chen, M.; Schuette, J.L.; Lesperance, M.M. Novel DICER1 mutation as cause of multinodular goiter in children. Head Neck 2013, 35, E369–E371. [Google Scholar] [CrossRef]
- Rath, S.R.; Bartley, A.; Charles, A.; Powers, N.; Baynam, G.; Jones, T.; Priest, J.R.; Foulkes, W.D.; Choong, C.S. Multinodular Goiter in children: An important pointer to a germline DICER1 mutation. J. Clin. Endocrinol. Metab. 2014, 99, 1947–1948. [Google Scholar] [CrossRef]
- Rossing, M.; Gerdes, A.M.; Juul, A.; Rechnitzer, C.; Rudnicki, M.; Nielsen, F.C.; Vo Hansen, T. A novel DICER1 mutation identified in a female with ovarian Sertoli-Leydig cell tumor and multinodular goiter: A case report. J. Med. Case Rep. 2014, 8, 112. [Google Scholar] [CrossRef]
- Sahakitrungruang, T.; Srichomthong, C.; Pornkunwilai, S.; Amornfa, J.; Shuangshoti, S.; Kulawonganunchai, S.; Suphapeetiporn, K.; Shotelersuk, V. Germline and somatic DICER1 mutations in a pituitary blastoma causing infantile-onset Cushing’s disease. J. Clin. Endocrinol. Metab. 2014, 99, E1487–E1492. [Google Scholar] [CrossRef] [PubMed]
- Palculict, T.B.; Ruteshouser, E.C.; Fan, Y.; Wang, W.; Strong, L.; Huff, V. Identification of germline DICER1 mutations and loss of heterozygosity in familial Wilms tumour. J. Med. Genet. 2016, 53, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Oost, E.E.; Charles, A.; Choong, C.S.; Leung, Y.C.; Salfinger, S.; Sonnendecker, H.; Tan, J.; Townshend, S.; Witkowski, L.; Foulkes, W.D.; et al. Ovarian Sex Cord-Stromal Tumors in Patients with probable or confirmed germline DICER1 mutations. Int. J. Gynecol. Pathol. 2015, 34, 266–274. [Google Scholar] [CrossRef] [PubMed]
- de Kock, L.; Druker, H.; Weber, E.; Hamel, N.; Traubici, J.; Malkin, D.; Arseneau, J.; Stewart, C.J.; Bouron-Dal Soglio, D.; Priest, J.R.; et al. Ovarian embryonal rhabdomyosarcoma is a rare manifestation of the DICER1 syndrome. Hum. Pathol. 2015, 46, 917–922. [Google Scholar] [CrossRef]
- Schultz, K.A.; Harris, A.; Messinger, Y.; Sencer, S.; Baldinger, S.; Dehner, L.P.; Hill, D.A. Ovarian tumors related to intronic mutations in DICER1: A report from the international ovarian and testicular stromal tumor registry. Fam. Cancer 2016, 15, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Kuhlen, M.; Hönscheid, A.; Schemme, J.; Merz, H.; Mauz-Körholz, C.; Borkhardt, A.; Troeger, A. Hodgkin lymphoma as a novel presentation of familial DICER1 syndrome. Eur. J. Pediatr. 2016, 175, 593–597. [Google Scholar] [CrossRef]
- Canfarotta, M.; Riba-Wolman, R.; Orsey, A.D.; Balarezo, F.; Finck, C. DICER1 syndrome and thyroid disease. J. Pediatr. Surg. Case Rep. 2016, 11, 31–34. [Google Scholar] [CrossRef]
- de Kock, L.; Bah, I.; Wu, Y.; Xie, M.; Priest, J.R.; Foulkes, W.D. Germline and Somatic DICER1 Mutations in a Well-Differentiated Fetal Adenocarcinoma of the Lung. J. Thorac. Oncol. 2016, 11, e31–e33. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, D.; Li, Y.; Bian, L.; Ma, T.; Xie, M. DICER1 mutations in a patient with an ovarian Sertoli-Leydig tumor, well-differentiated fetal adenocarcinoma of the lung, and familial multinodular goiter. Eur. J. Med. Genet. 2014, 57, 621–625. [Google Scholar] [CrossRef]
- Wu, M.K.; de Kock, L.; Conwell, L.S.; Stewart, C.J.; King, B.R.; Choong, C.S.; Hussain, K.; Sabbaghian, N.; MacRae, I.J.; Fabian, M.R.; et al. Functional characterization of multiple DICER1 mutations in an adolescent. Endocr. Relat. Cancer 2016, 23, L1–L5. [Google Scholar] [CrossRef]
- Wu, M.K.; Goudie, C.; Druker, H.; Thorner, P.; Traubici, J.; Grant, R.; Albrecht, S.; Weber, E.; Charles, A.; Priest, J.R.; et al. Evolution of Renal Cysts to Anaplastic Sarcoma of Kidney in a Child with DICER1 Syndrome. Pediatr. Blood Cancer 2016, 63, 1272–1275. [Google Scholar] [CrossRef] [PubMed]
- Fremerey, J.; Balzer, S.; Brozou, T.; Schaper, J.; Borkhardt, A.; Kuhlen, M. Embryonal rhabdomyosarcoma in a patient with a heterozygous frameshift variant in the DICER1 gene and additional manifestations of the DICER1 syndrome. Fam. Cancer 2017, 16, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Caruso, S.; Calderaro, J.; Letouzé, E.; Nault, J.C.; Couchy, G.; Boulai, A.; Luciani, A.; Zafrani, E.S.; Bioulac-Sage, P.; Seror, O.; et al. Germline and somatic DICER1 mutations in familial and sporadic liver tumors. J. Hepatol. 2017, 66, 734–742. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Martínez, L.; Villegas, J.A.; Santamaría, Í.; Pitiot, A.S.; Alvarado, M.G.; Fernández, S.; Torres, H.; Paredes, Á.; Blay, P.; Balbín, M. Identification of somatic and germ-line DICER1 mutations in pleuropulmonary blastoma, cystic nephroma and rhabdomyosarcoma tumors within a DICER1 syndrome pedigree. BMC Cancer 2017, 17, 146. [Google Scholar] [CrossRef]
- Saskin, A.; de Kock, L.; Sabbaghian, N.; Apellaniz-Ruiz, M.; Bozkurt, C.; Bouron-Dal Soglio, D.; Foulkes, W.D. A case of neuroblastoma in DICER1 syndrome: Chance finding or noncanonical causation? Pediatr. Blood Cancer 2018, 65, e26715. [Google Scholar] [CrossRef]
- Yoshida, M.; Hamanoue, S.; Seki, M.; Tanaka, M.; Yoshida, K.; Goto, H.; Ogawa, S.; Takita, J.; Tanaka, Y. Metachronous anaplastic sarcoma of the kidney and thyroid follicular carcinoma as manifestations of DICER1 abnormalities. Hum. Pathol. 2017, 61, 205–209. [Google Scholar] [CrossRef]
- Apellaniz-Ruiz, M.; Segni, M.; Kettwig, M.; Glüer, S.; Pelletier, D.; Nguyen, V.H.; Wagener, R.; López, C.; Muchantef, K.; Bouron-Dal Soglio, D.; et al. Mesenchymal Hamartoma of the Liver and DICER1 Syndrome. N. Engl. J. Med. 2019, 380, 1834–1842. [Google Scholar] [CrossRef]
- Dural, O.; Kebudi, R.; Yavuz, E.; Yilmaz, I.; Buyukkapu Bay, S.; Schultz, K.A.P.; Hill, D.A. DICER1-Related Embryonal Rhabdomyosarcoma of the Uterine Corpus in a Prepubertal Girl. J. Pediatr. Adolesc. Gynecol. 2020, 33, 173–176. [Google Scholar] [CrossRef]
- Herriges, J.C.; Brown, S.; Longhurst, M.; Ozmore, J.; Moeschler, J.B.; Janze, A.; Meck, J.; South, S.T.; Andersen, E.F. Identification of two 14q32 deletions involving DICER1 associated with the development of DICER1-related tumors. Eur. J. Med. Genet. 2019, 62, 9–14. [Google Scholar] [CrossRef]
- Nagasaki, K.; Shibata, N.; Nyuzuki, H.; Sasaki, S.; Ogawa, Y.; Soda, S.; Kogai, T.; Hishinuma, A. A Japanese Family with DICER1 Syndrome Found in Childhood-Onset Multinodular Goitre. Horm. Res. Paediatr. 2020, 93, 477–482. [Google Scholar] [CrossRef]
- Tutor, J.D.; Miller, S.F.; Al Zubeidi, H.; Sheyn, A.; Zhang, J.; Williams, R.; McGee, R.B. Lung cyst and multinodular thyroid goiter: Keys to DICER1 syndrome diagnosis in a 16-year-old female. Clin. Case Rep. 2020, 8, 2373–2376. [Google Scholar] [CrossRef] [PubMed]
- Apellaniz-Ruiz, M.; Cullinan, N.; Grant, R.; Marrano, P.; Priest, J.R.; Thorner, P.S.; Goudie, C.; Foulkes, W.D. DICER1 screening in 15 paediatric paratesticular sarcomas unveils an unusual DICER1-associated sarcoma. J. Pathol. Clin. Res. 2020, 6, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ye, H.; Jin, Y.; Zhong, P.; Duan, H. Somatic DICER1 Mutations in a Pubertal Girl with Cervical Embryonal Rhabdomyosarcoma and Papillary Thyroid Adenoma. J. Pediatr. Adolesc. Gynecol. 2020, 33, 742–744. [Google Scholar] [CrossRef] [PubMed]
- Chernock, R.D.; Rivera, B.; Borrelli, N.; Hill, D.A.; Fahiminiya, S.; Shah, T.; Chong, A.S.; Aqil, B.; Mehrad, M.; Giordano, T.J.; et al. Poorly differentiated thyroid carcinoma of childhood and adolescence: A distinct entity characterized by DICER1 mutations. Mod. Pathol. 2020, 33, 1264–1274. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, X.; Li, S.; Cai, S.; Yu, T.; Fu, L.; Zhang, N.; Peng, X.; Zeng, Q.; Ma, X. Outcome of two pairs of monozygotic twins with pleuropulmonary blastoma: Case report. Ital. J. Pediatr. 2020, 46, 148. [Google Scholar] [CrossRef]
- Chong, A.S.; Han, H.; Albrecht, S.; Weon, Y.C.; Park, S.K.; Foulkes, W.D. DICER1 syndrome in a young adult with pituitary blastoma. Acta Neuropathol. 2021, 142, 1071–1076. [Google Scholar] [CrossRef]
- See, S.C.; Wadhwani, N.R.; Yap, K.L.; Arva, N.C. Primary Biphasic Hepatic Sarcoma in DICER1 Syndrome. Pediatr. Dev. Pathol. 2021, 24, 484–488. [Google Scholar] [CrossRef]
- Juhlin, C.C.; Stenman, A.; Zedenius, J. Macrofollicular variant follicular thyroid tumors are DICER1 mutated and exhibit distinct histological features. Histopathology 2021, 79, 661–666. [Google Scholar] [CrossRef]
- Rossi, S.; Barresi, S.; Stracuzzi, A.; Lopez-Nunez, O.; Chiaravalli, S.; Ferrari, A.; Ciolfi, A.; Maria Milano, G.; Giovannoni, I.; Tartaglia, M.; et al. DICER1-associated malignancies mimicking germ cell neoplasms: Report of two cases and review of the literature. Pathol. Res. Pract. 2021, 225, 153553. [Google Scholar] [CrossRef]
- Ni, Y.; Zhou, X.; Wu, L.; Wu, P.; Liu, Y.; Li, Y.; Cai, L.; Fu, X.; Zhang, C. Ovarian Sertoli-Leydig Cell Tumor, Multinodular Goiter, Cystic Nephromas and DICER1 Mutations: Case Report and Literature Review. Pharmacogenom. Pers. Med. 2021, 14, 947–953. [Google Scholar] [CrossRef]
- Karnak, İ.; Ceylan, A.C.; Haliloğlu, M.; Özön, A.; Orhan, D.; Kutluk, T. Sertoli-leydig cell tumor, thyroid follicular carcinoma and rhabdomyosarcoma of the uterine cervix in a prepubertal girl with pathogenic germline variant in dicer1 gene. Turk. J. Pediatr. 2021, 63, 500. [Google Scholar] [CrossRef] [PubMed]
- Gupte, A.; Sood, S.; Kupsky, W.J.; Altinok, D.; Miller, S.; Roy, S.; Bhambhani, K. Pineal Parenchymal Tumor of Intermediate Differentiation and DICER1 Syndrome: A Case Report. J. Pediatr. Hematol. 2022, 45, e406–e409. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.B.; Hoefgen, H.R.; Vrecenak, J.D. Uterine Sarcoma Auto-Amputation in an Infant with DICER1 Syndrome. J. Pediatr. Adolesc. Gynecol. 2022, 35, 411–412. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.; Desrosiers, L.; Scollon, S.; Gruner, S.; Reuther, J.; Gandhi, I.; Patil, N.; Fuller, M.Y.; Dai, H.; Muzny, D.; et al. Distinct somatic DICER1 hotspot mutations in three metachronous ovarian Sertoli-Leydig cell tumors in a patient with DICER1 syndrome. Cancer Genet. 2022, 262, 53–56. [Google Scholar] [CrossRef]
- Lau, J.C.C.; McCluggage, W.G.; Yuen, L.Y.P.; Shing, M.M.K.; Chan, G.C.F.; Yam, F.S.D.; Leung, M.W.Y.; Ng, W.F.; Liu, A.P.Y. DICER1-Altered Extraovarian Moderately Differentiated Sertoli-Leydig Cell Tumor: Report of a Rare Case. Int. J. Gynecol. Pathol. 2022, 42, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, C.; Palit, V.; Bardapure, M.; Thomas, J.; Browning, A.J.; Gill, K.; Biyani, C.S. Adult multilocular cystic nephroma: Report of six cases with clinical, radio-pathologic correlation and review of literature. Urol. Ann. 2013, 5, 13. [Google Scholar] [CrossRef]
- Li, Y.; Pawel, B.R.; Hill, D.A.; Epstein, J.I.; Argani, P. Pediatric Cystic Nephroma Is Morphologically, Immunohistochemically, and Genetically Distinct from Adult Cystic Nephroma. Am. J. Surg. Pathol. 2017, 41, 472–481. [Google Scholar] [CrossRef]
- Caroleo, A.M.; De Ioris, M.A.; Boccuto, L.; Alessi, I.; Del Baldo, G.; Cacchione, A.; Agolini, E.; Rinelli, M.; Serra, A.; Carai, A.; et al. DICER1 Syndrome and Cancer Predisposition: From a Rare Pediatric Tumor to Lifetime Risk. Front. Oncol. 2021, 10, 614541. [Google Scholar] [CrossRef]
- Priest, J.R.; McDermott, M.B.; Bhatia, S.; Watterson, J.; Manivel, J.C.; Dehner, L.P. Pleuropulmonary blastoma: A clinicopathologic study of 50 cases. Cancer 1997, 80, 147–161. [Google Scholar] [CrossRef]
- Juhlin, C.C. On the Chopping Block: Overview of DICER1 Mutations in Endocrine and Neuroendocrine Neoplasms. Surg. Pathol. Clin. 2023, 16, 107–118. [Google Scholar] [CrossRef]
- González, I.A.; Mallinger, P.; Watson, D.; Harris, A.K.; Messinger, Y.H.; Schultz, K.A.P.; Field, A.; Hill, D.A.; Dehner, L.P. Expression of p53 is significantly associated with recurrence-free survival and overall survival in pleuropulmonary blastoma (PPB): A report from the International Pleuropulmonary Blastoma/DICER1 Registry. Mod. Pathol. 2021, 34, 1104–1115. [Google Scholar] [CrossRef]
- Khan, N.E.; Bauer, A.J.; Schultz, K.A.P.; Doros, L.; Decastro, R.M.; Ling, A.; Lodish, M.B.; Harney, L.A.; Kase, R.G.; Carr, A.G.; et al. Quantification of Thyroid Cancer and Multinodular Goiter Risk in the DICER1 Syndrome: A Family-Based Cohort Study. J. Clin. Endocrinol. Metab. 2017, 102, 1614–1622. [Google Scholar] [CrossRef] [PubMed]
- Fineberg, S.K.; Kosik, K.S.; Davidson, B.L. MicroRNAs Potentiate Neural Development. Neuron 2009, 64, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.D.; Martinez-Agosto, J.A. Hotspot Mutations in DICER1 Causing GLOW Syndrome-Associated Macrocephaly via Modulation of Specific microRNA Populations Result in the Activation of PI3K/ATK/mTOR Signaling. Microrna 2020, 9, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.T.; Lee, K.; Chung, W.K.; Gordon, A.S.; Herman, G.E.; Klein, T.E.; Stewart, D.R.; Amendola, L.M.; Adelman, K.; Bale, S.J. ACMG SF v3.0 list for reporting of secondary findings in clinical exome and genome sequencing: A policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 2021, 23, 1381–1390. [Google Scholar] [CrossRef]
- Hill, D.A.; Jarzembowski, J.A.; Priest, J.R.; Williams, G.; Schoettler, P.; Dehner, L.P. Type I pleuropulmonary blastoma: Pathology and biology study of 51 cases from the international pleuropulmonary blastoma registry. Am. J. Surg. Pathol. 2008, 32, 282–295. [Google Scholar] [CrossRef]


| Sex | Age at First Surgery (mo) | Age at Diagnosis of DICER1 Syndrome (mo) | Clinical Manifestations | Genetic Variation | Familial | Outcome Status | |
|---|---|---|---|---|---|---|---|
| Case 1 | F | 36 | 48 | PPB, NG, TA | c.919_932 of CGTGCCGTATTGGT (p.Arg307Serfs*9) | Yes (Father, Brother) | Alive |
| Case 2 | M | 18 | 36 | GLOW Syndrome, CN | c.[2339delC]; [-] | No | Alive |
| Case 3 | M | 36 | 36 | ASK, MNG, DTC | c.574-1G>A | No | Alive |
| Case 4 | M | 11 | 12 | ERMS | c.1069G>A | No | Dead |
| Case 5 | F | 36 | 36 | CN, PPB | c.1376+G>T (rs886037670-CS118387) | Yes (Father, Brother) | Alive |
| Case 6 | F | 4 | 8 | PPB | c.5465A>T p.D1822V | Yes (Father) | Alive |
| Case 7 | M | 1.3 | 3 | CBME, CN, PPB | c.3288_3289insTTTC | No | Alive |
| Author | Year | Sex | Age at Diagnosis | Clinical Manifestations | Genetic Mutation | Familial | Outcome Status |
|---|---|---|---|---|---|---|---|
| Hill et al. [21] | 2009 | 3 F 7 M | 0.5 0.9 N/A N/A N/A N/A N/A N/A N/A N/A | PPB + cERMS | c.1910dupA c.2268_2271delTTTG c.1507G>T c.2245_2248dupTACC c.2247C>A c.1684_1685delAT c.2392dupA c.2830C>T c.3540C>A c.4748T>G | 3 No 7 Yes | 1 Dead 9 Alive |
| Slade et al. [27] | 2011 | 4 F 1 M 14 N/A | 1.5 0.8 4 3 7 0.9 4.2 3 4 1.8 1.3 1.5 3 17 12 6 8 13 32 | 11 PPB, CBME 2CN, 3 SLCT dx, sx, PB, OSCST dx, WT, MNG, MB/PNET infratentorial, seminoma | c.4403_4406delCTCT c.1716delT c.1196_1197dupAG c.3505delT c.1966C>T p.R656X c.2268_2271delTTTG c.3665delT c.2040+1 G>C c.3726C>A p.Y1242X c.5465A>T p.D1822V c.3583_3584delGA c.3288_3289insTTTC c.328_338dupGTGTCAGCTGT c.5122_5128delGGAGATG c.1966C>T_p.R656X c.3793delA c.2988N/A2_2988N/A1delAGinsCT c.1153delC c.4740G>T p.Q1580H | 11 No 6 Yes 2 N/A | 16 Alive 2 N/A 1 Dead |
| Rio Frio et al. [28] | 2011 | 4 F 1 M | 16 18 18 15 N/A | 5MNG, 3SLCT, 1PPB | c.876_879delAAAG C.2457C>G c.5018_5021delTCAA c.2516C>T c.2805N/A1G>T | 3 Yes 2 N/A | 4 Alive 1 Dead |
| Foulkes et al. [32] | 2011 | 5 F 2 M | 9 4 2 1.3 5 14 11 | SLCT, MNG | c.4050+1delG c.912_919dupAGACTGTC c.1306dupT c.1966C>T c.2117N/A1G>A c.3611_3616delACTACAinsT c.3907_3908delCT | 7 Yes | 4 Alive 3 N/A |
| Bahubeshi et al. [33] | 2012 | F | 2.1 | CN, PPB | c.4309_4312delGACT | N/A | N/A |
| Doros et al. [34] | 2012 | F M | 4 0.1 | PPB, cERMS, ERMS | c.4309_4312delGACT c.2247C>A | N/A | N/A |
| Sabbaghian et al. [35] | 2012 | M | <3 | PB | c.1128_1132delAGTAA | N/A | N/A |
| de Kock et al. [36] | 2013 | F | 3 | PPB | c.4555delG | N/A | N/A |
| Sabbaghian et al. [37] | 2013 | F | 6 | SLCT, MNG | c.3270N/A6_4051—1280delinsG | Yes | Alive |
| Darrat et al. [38] | 2013 | F | 12 | MNG | c.1525C>T | Yes | Alive |
| Stewart et al. [25] | 2014 | 4 F 4 M | 2.9 1.8 3.4 4.6 6 3.4 13 17 | 8PPB, 8NCMH, 3SLCT, DTC | c.2863delA; p.T955fs c.5437G>A; p.Glu1813Lys c.2040+1G>T c.4407_4410delTTCT; p.L1469fs c.1376+1G>T c.5394delA c.3726C>A; P.Y1242X P. Y749X | N/A | N/A |
| de Kock et al. [16] | 2014 | 5 F 4 M | 27 2.8 2.11 17 1.11 3 7 N/A 1.9 | 3PPB, NCMH, 2MNG, DTC, 6PitB | c.3019C>T; P.Q1007X c.2379T>G c.3505dupT c.2026C>T c.1284delGA c.2379T>G c.3277_3280delAACT c.4309_4312delGACT c.5125G>C | 1 No 8 N/A | 8 Alive 1 Dead |
| Rath et al. [39] | 2014 | M | 2.8 | CN, PPB, MNG | c.5221_5232delAACAACACCATC | Yes | Alive |
| Rossing et al. [40] | 2014 | F | 13 | MNG, SLCT | c.3647C>A; c.3649T | Yes | Alive |
| Sahakit Rungruang et al. [41] | 2014 | F | 1 | PitB | c.3046delA | N/A | N/A |
| Palculict et al. [42] | 2015 | F | 3.5 | WT | c.2399delG; p.R800fsX5 | Yes | Alive |
| Oost et al. [43] | 2015 | F | 16 | SLCT | c.1532_1533delAT | Yes | N/A |
| de Kock et al. [44] | 2015 | F | 6 | cERMS, CN, MNG | c.1196_1197dupAG | N/A | N/A |
| Schultz et al. [45] | 2016 | M | 5 | PPB, MNG, SLCT | c.5096N/A12 G>A + c.5126A>T; p.Asp1709Val | No | Alive |
| Kuhlen et al. [46] | 2016 | M | 11 | PPB, MNG | c.4616C>T | Yes | Alive |
| Canfarotta et al. [47] | 2016 | F | 7 | SLCT, MNG | c.325C>T | No | Alive |
| de Kock et al. [48] | 2016 | F | 14 | MNG, SLCT | c.3540C>A | Yes | Alive |
| Wu et al. [15,49,50,51] | 2014, 2016 | 3 F | 0.9 0.7 12 | CN, 2ASK, MNG, OSCT | c.2062C>T c.2450delC c.3540C>G | N/A | 2 Alive 1 N/A |
| Fremerey et al. [52] | 2016 | F | 0.6 | CBME, ERMS, CN, PPB | c.3405dupA | Yes | N/A |
| Bardón-Cancho et al. [14] | 2016 | F | 2 | CN, PPB | c.3540C>G | Yes | Alive |
| Caruso et al. [53] | 2017 | 2 M | 34 32 | 2Liver Cancer | 2c.2455T>C | 2 Yes | 2 Alive |
| Fernández-Martinez et al. [54] | 2017 | F | 0.11 | CN, PPB | c.5387C>T | Yes | Alive |
| Saskin et al. [55] | 2017 | F | 7 | MNG, CN | c.4566_4579dupCTTTG | N/A | Alive |
| Yoshida et al. [56] | 2017 | F | 12 | MNG, DTC | c.5426_5442delGGGATATTTTTGAGTCGinsCA | N/A | Alive |
| Apellaniz et al. [57] | 2019 | 2 M | 2.2 0.9 | 2Liver Cancer, MNG, PPB, CN, polyps | c.4007delC, p.P1336Lfs11; c.5125G→A, p.D1709N; e c.5113G→C, p.E1705Q | 1 Yes 1 No | 2 Alive |
| Bailey et al. [24] | 2019 | 4 M | 4 19 3 5 | 2PPB, RMS, PB | c.5364+1G>A c.1069G>A c.745G>A c.4754C>T | N/A | N/A |
| Dural et al. [58] | 2019 | F | 10 | CN, ERMS | c.5113G>A | N/A | Alive |
| Haley et al. [29] | 2019 | F | 38 | SLCT, MNG | N/A | Yes | Dead |
| Herriges et al. [59] | 2019 | M | 6 | S. Glow, Macrocephaly | N/A | N/A | N/A |
| Nagasaki et al. [60] | 2020 | F | 6 | MNG, DTC | c.4509C>G, p.Y1503X | Yes | Alive |
| Warren et al. [30] | 2020 | 2 F | 5 16 | 2OSCST | c.2223_2230del; P.S742T16 c.3682C>T;p.Q1228 | 1 Yes 1 No | 1 Alive 1 Dead |
| Tutor et al. [61] | 2020 | F | 16 | PPB, MNG | p.Asp940Ter | N/A | Alive |
| Apellaniz et al. [62] | 2020 | M | 0.10 | ERMS, CN | N/A | N/A | N/A |
| Zhang et al. [63] | 2020 | F | 16 | MNG, ERMS | c.3937delG | N/A | Alive |
| Chernock et al. [64] | 2020 | M | 17 | DTC | c.735N/A8T>G (41/69) | No | Alive |
| McCluggage et al. [22] | 2020 | 3 F | 60 13 14 | 3ERMS | c.5428G>C, p.D1810H c.5315_5316del; p.F1772fs c.2805N/A2_2817deletionAGATATCGCAATTTT | 2 No 1 N/A | N/A |
| Zhang et al. [65] | 2020 | F | 0.2 | PPB | c.C3675A (p.Y1225X) | Yes | N/A |
| Chong et al. [66] | 2021 | F | 4 | WT, MNG, PitB | c.890dupT, p.Leu297Phefs23 | Yes | Alive |
| See et al. [67] | 2021 | M | 12 | PPB, Liver CancerPPB like | c.4458dup: p.Ser1487Ilefs5 | N/A | Alive |
| Azzollini et al. [26] | 2021 | F 2 M | 10 0.8 22 | SLCT, MNG, PPB, RMS | c.1630C>T p.(Arg544) | 3 Yes | 3 Alive |
| Venger et al. [17] | 2021 | 2 F 1 M | 0.11 16 3 | Macrosomia, 3macrocephaly, WT, PPB, S. Glow, SLCT, MNG | c.4031C>T; p.(Ser1344Leu) c.3073G>T; p.(Glu1025) c.3234_3237dupTGGC | 1 No 2 Yes | 3 Alive |
| Juhlin et al. [68] | 2021 | F | 13 | DTC | c.2830C>T, p. Arg944Ter (G) | Yes | N/A |
| Miyama et al. [31] | 2021 | M | 26 | RMS | c.5125G>A | N/A | Dead |
| Rossi et al. [69] | 2021 | 2 M | 22 2 | 2RMS | N/A | N/A | 2 Alive |
| Kaspar et al. [18] | 2021 | M | 1.3 | CN, macrosomia, Macrocephaly, PPB | N/A | N/A | N/A |
| Ni et al. [70] | 2021 | F | 2 | CN, SLCT, MNG | c.1088_1089delCTinsAA p.F363X) | N/A | N/A |
| Darbinyan et al. [23] | 2021 | 7 F | 14 12 17 35 37 58 65 | 7MNG 1ERMS | 2 c.5428G>T c.5113G>T c.5428G>T c.5126A>G 2 c.5113G>A | 7 Yes | 7N/A |
| Karnak et al. [71] | 2021 | F | 5.1 | SLCT, DTC, cERMS, PPB | c.3377delC, c.71delC | N/A | N/A |
| Gupte et al. [72] | 2022 | F | 13 | PB, CBME | c.1847T>A | Yes | Alive |
| Wilson et al. [73] | 2022 | F | 0.6 | ERMS | N/A | N/A | Alive |
| Pontén et al. [19] | 2022 | M | 1.3 | Macrocephaly, WT, S. Glow, PPB, CN | c.4031C>T | Yes | Alive |
| Hammad et al. [20] | 2022 | F | 0.1 | Spinal amarthroma | c.3118_3119insCA | Yes | N/A |
| Garcia et al. [74] | 2022 | F | 2.6 | SLCT | N/A | N/A | N/A |
| Lau et al. [75] | 2022 | F | 4 | SLCT | N/A | N/A | N/A |
| Factor | Our Study (n = 7) | Literature Review (n = 132) | p-Value |
|---|---|---|---|
| Males | 4 (57.1) | 45 (37.5 out of 120 cases) | 0.575 |
| Age first surgery (years) | 1.7 (1.4) | 10 (7 out of 120 cases) | 0.002 |
| Familial | 6 (85.7) | 55 (70.5 out of 78 cases) | 0.676 |
| Death | 1 (14.29) | 6 (7.1 out of 84 cases) | 0.959 |
| PPB | 4 (57.1) | 54 (40.7) | 0.642 |
| CN | 3 (42.86) | 19 (15.91) | 0.186 |
| ASK | 1 (14.29) | 3 (1.52) | 0.351 |
| MNG | 3 (28.57) | 46 (34.09) | 0.912 |
| DTC | 1 (14.29) | 7 (5.34) | 0.874 |
| CBME | 1 (14.29) | 3 (2.27) | 0.488 |
| S.GLOW | 1 (14.29) | 3 (2.27) | 0.488 |
| RMS | 1 (14.29) | 22 (19.7) | 0.721 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spinelli, C.; Ghionzoli, M.; Sahli, L.I.; Guglielmo, C.; Frascella, S.; Romano, S.; Ferrari, C.; Gennari, F.; Conzo, G.; Morganti, R.; et al. DICER1 Syndrome: A Multicenter Surgical Experience and Systematic Review. Cancers 2023, 15, 3681. https://doi.org/10.3390/cancers15143681
Spinelli C, Ghionzoli M, Sahli LI, Guglielmo C, Frascella S, Romano S, Ferrari C, Gennari F, Conzo G, Morganti R, et al. DICER1 Syndrome: A Multicenter Surgical Experience and Systematic Review. Cancers. 2023; 15(14):3681. https://doi.org/10.3390/cancers15143681
Chicago/Turabian StyleSpinelli, Claudio, Marco Ghionzoli, Linda Idrissi Sahli, Carla Guglielmo, Silvia Frascella, Silvia Romano, Carlo Ferrari, Fabrizio Gennari, Giovanni Conzo, Riccardo Morganti, and et al. 2023. "DICER1 Syndrome: A Multicenter Surgical Experience and Systematic Review" Cancers 15, no. 14: 3681. https://doi.org/10.3390/cancers15143681
APA StyleSpinelli, C., Ghionzoli, M., Sahli, L. I., Guglielmo, C., Frascella, S., Romano, S., Ferrari, C., Gennari, F., Conzo, G., Morganti, R., De Napoli, L., Quaglietta, L., De Martino, L., Picariello, S., Grandone, A., Luongo, C., Gambale, A., Patrizio, A., Fallahi, P., ... Ferrari, S. M. (2023). DICER1 Syndrome: A Multicenter Surgical Experience and Systematic Review. Cancers, 15(14), 3681. https://doi.org/10.3390/cancers15143681








