Unsupervised Machine Learning of MRI Radiomics Features Identifies Two Distinct Subgroups with Different Liver Function Reserve and Risks of Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
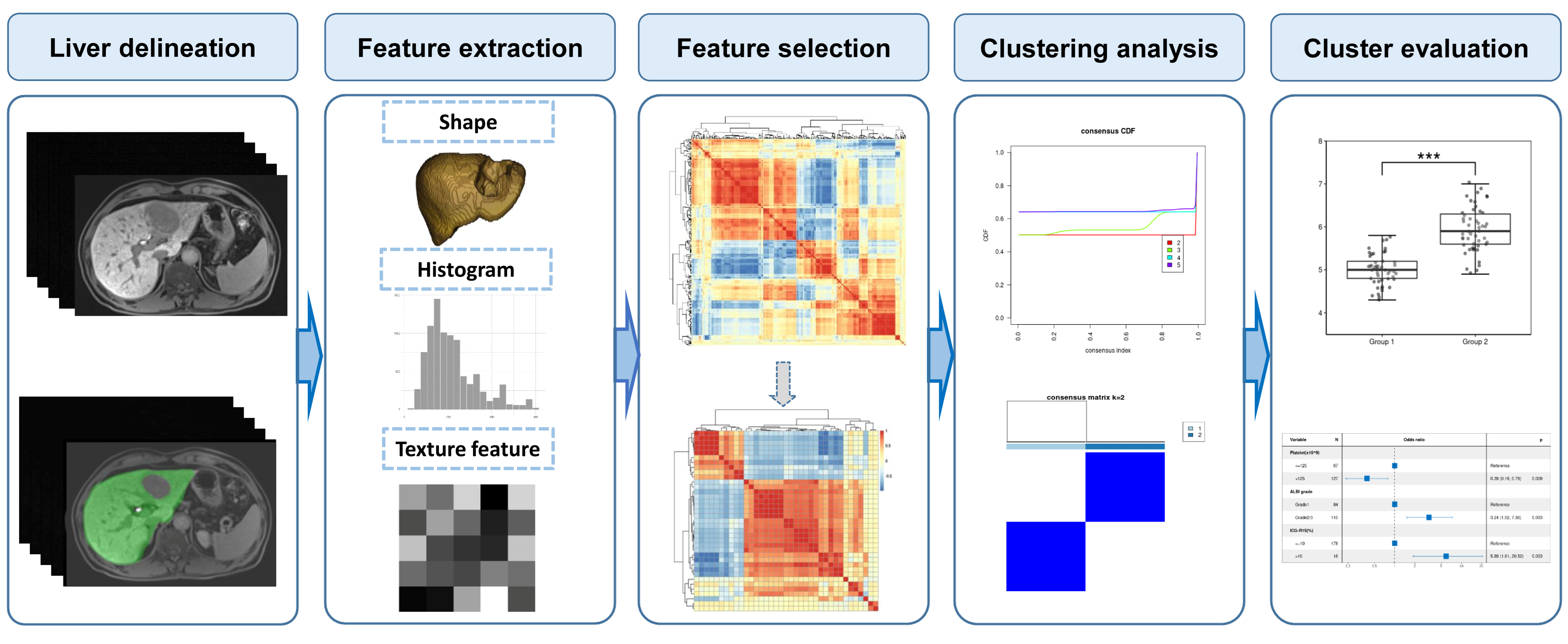
2. Materials and Methods
2.1. Study Design and Patient Inclusion
2.2. Clinical Variables
2.3. Gadoxetic-Acid-Enhanced MRI Exam
2.4. Liver Delineation and Radiomics Feature Extraction
2.5. Radiomics Feature Selection
2.6. Unsupervised Clustering Analysis
2.7. Cluster Comparison and Statistical Analysis
3. Results
3.1. Basic Characteristics of the Entire Cohort
3.2. Radiomics Feature Selection and Unsupervised Clustering Analysis
3.3. Subgroup 1 vs. Subgroup 2
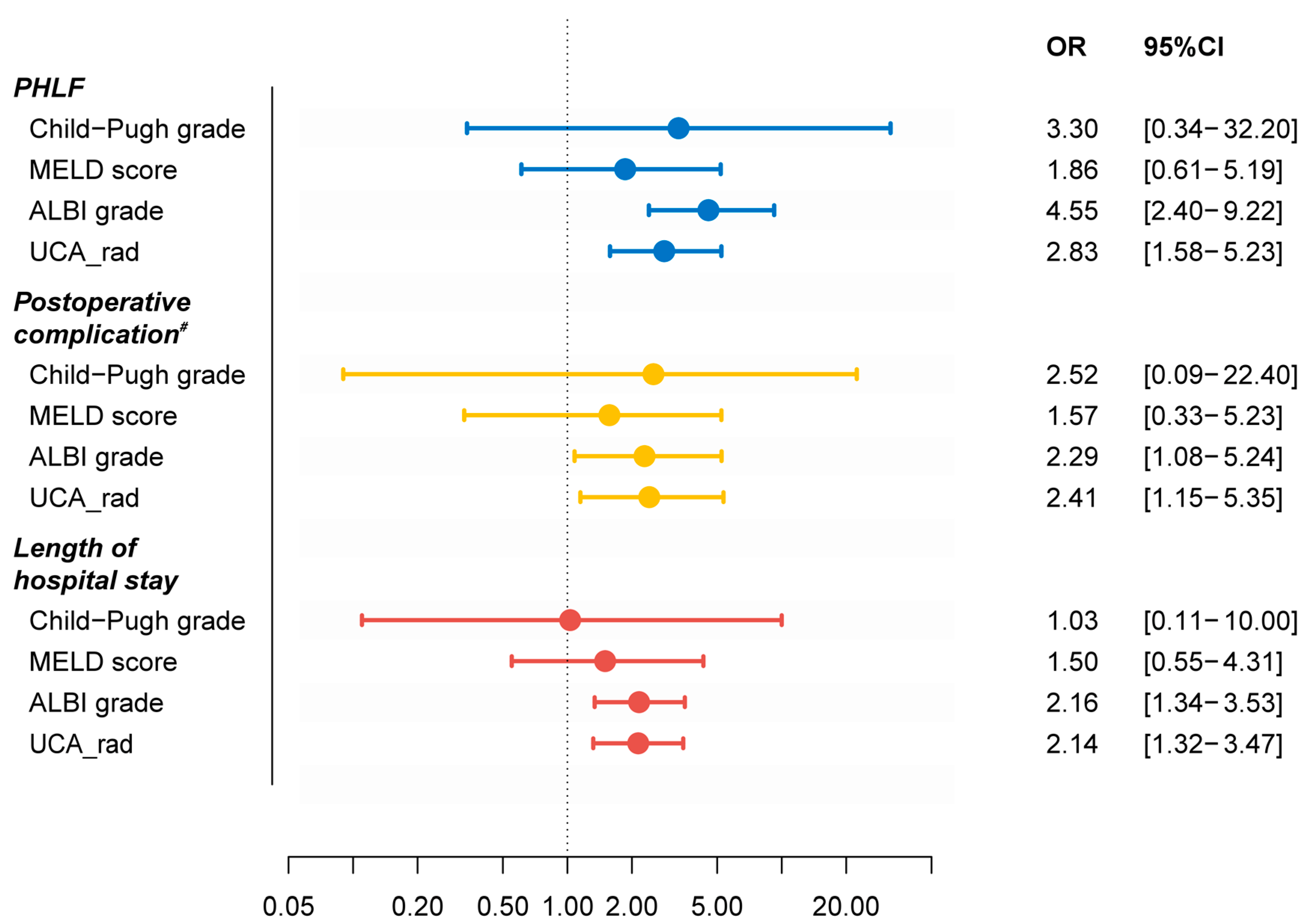
3.4. Comparison among Different Systems
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, J.D.; Hainaut, P.; Gores, G.J.; Amadou, A.; Plymoth, A.; Roberts, L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 589–604. [Google Scholar] [CrossRef] [PubMed]
- Brar, G.; Greten, T.F.; Graubard, B.I.; McNeel, T.S.; Petrick, J.L.; McGlynn, K.A.; Altekruse, S.F. Hepatocellular Carcinoma Survival by Etiology: A SEER-Medicare Database Analysis. Hepatol. Commun. 2020, 4, 1541–1551. [Google Scholar] [CrossRef]
- Zhang, N.; Xiao, X.-H. Integrative medicine in the era of cancer immunotherapy: Challenges and opportunities. J. Integr. Med. 2021, 19, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Kauffmann, R.; Fong, Y. Post-hepatectomy liver failure. Hepatobiliary Surg. Nutr. 2014, 3, 238–246. [Google Scholar] [PubMed]
- Søreide, J.A.; Deshpande, R. Post hepatectomy liver failure (PHLF)–Recent advances in prevention and clinical management. Eur. J. Surg. Oncol. 2020, 47, 216–224. [Google Scholar] [CrossRef]
- Van Mierlo, K.M.C.; Schaap, F.G.; Dejong, C.H.C.; Olde Damink, S.W.M. Liver resection for cancer: New developments in prediction, prevention and management of postresectional liver failure. J. Hepatol. 2016, 65, 1217–1231. [Google Scholar] [CrossRef]
- Hepatocellular Carcinoma. Nat. Rev. Dis. Prim. 2021, 7. Available online: https://www.nature.com/articles/s41572-020-00240-3 (accessed on 26 November 2022). [CrossRef]
- Nilsson, H.; Karlgren, S.; Blomqvist, L.; Jonas, E. The inhomogeneous distribution of liver function: Possible impact on the prediction of post-operative remnant liver function. HPB 2015, 17, 272–277. [Google Scholar] [CrossRef]
- Iimuro, Y. ICG Clearance Test and 99mTc-GSA SPECT/CT Fusion Images. Visc. Med. 2017, 33, 449–454. [Google Scholar] [CrossRef]
- Vos, J.J.; Wietasch, J.K.G.; Absalom, A.; Hendriks, H.G.D.; Scheeren, T.W.L. Green light for liver function monitoring using indocyanine green? An overview of current clinical applications. Anaesthesia 2014, 69, 1364–1376. [Google Scholar] [CrossRef]
- Makuuchi, M.; Kokudo, N. Clinical practice guidelines for hepatocellular carcinoma: The first evidence based guidelines from Japan. World J. Gastroenterol. 2006, 12, 828–829. [Google Scholar] [CrossRef] [PubMed]
- Van Beers, B.E.; Pastor, C.M.; Hussain, H.K. Primovist, Eovist: What to expect? J. Hepatol. 2012, 57, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Bae, K.E.; Kim, S.Y.; Lee, S.S.; Kim, K.W.; Won, H.J.; Shin, Y.M.; Kim, P.N.; Lee, M.-G. Assessment of Hepatic Function with Gd-EOB-DTPA-Enhanced Hepatic MRI. Dig. Dis. 2012, 30, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Wang, A.; Sparrelid, E.; Zhang, J.; Zhao, Y.; Ma, K.; Brismar, T.B. Predictive value of gadoxetic acid–enhanced MRI for posthepatectomy liver failure: A systematic review. Eur. Radiol. 2021, 32, 1792–1803. [Google Scholar] [CrossRef] [PubMed]
- Haimerl, M.; Verloh, N.; Zeman, F.; Fellner, C.; Nickel, D.; Lang, S.A.; Teufel, A.; Stroszczynski, C.; Wiggermann, P. Gd-EOB-DTPA-enhanced MRI for evaluation of liver function: Comparison between signal-intensity-based indices and T1 relaxometry. Sci. Rep. 2017, 7, 43347. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Huh, J.; Woo, D.-C.; Kim, K.W. Use of gadoxetate disodium for functional MRI based on its unique molecular mechanism. Br. J. Radiol. 2016, 89, 20150666. [Google Scholar] [CrossRef]
- Brismar, T.B.; Dahlström, N.; Edsborg, N.; Persson, A.; Smedby, Ö.; Albiin, N. Liver vessel enhancement by gd-bopta and gd-eob-dtpa: A comparison in healthy volunteers. Acta Radiol. 2009, 50, 709–715. [Google Scholar] [CrossRef]
- Wang, Q.; Brismar, T.B.; Gilg, S.; Jonas, E.; Nilsson, H.; Tzortzakakis, A.; Isaksson, B.; Axelsson, R.; Sparrelid, E. Multimodal perioperative assessment of liver function and volume in patients undergoing hepatectomy for colorectal liver metastasis: A comparison of the indocyanine green retention test, 99mTc mebrofenin hepatobiliary scintigraphy and gadoxetic acid enhanced MRI. Br. J. Radiol. 2022, 95, 20220370. [Google Scholar] [CrossRef]
- Nagaraju, G.P.; Dariya, B.; Kasa, P.; Peela, S.; El-Rayes, B.F. Epigenetics in hepatocellular carcinoma. Semin. Cancer Biol. 2022, 86, 622–632. [Google Scholar] [CrossRef]
- Liu, Z.; Suo, C.; Jiang, Y.; Zhao, R.; Zhang, T.; Jin, L.; Chen, X. Phenome-Wide Association Analysis Reveals Novel Links Between Genetically Determined Levels of Liver Enzymes and Disease Phenotypes. Phenomics 2022, 2, 295–311. [Google Scholar] [CrossRef]
- Cao, X.; Shao, Y.; Meng, P.; Cao, Z.; Yan, G.; Yao, J.; Zhou, X.; Liu, C.; Zhang, L.; Shu, H.; et al. Nascent Proteome and Glycoproteome Reveal the Inhibition Role of ALG1 in Hepatocellular Carcinoma Cell Migration. Phenomics 2022, 2, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef] [PubMed]
- Miranda Magalhaes Santos, J.M.; Clemente Oliveira, B.; Araujo-Filho, J.D.A.B.; Assuncao, A.N., Jr.; de, M. Machado, F.A.; Carlos Tavares Rocha, C.; Horvat J.V.; Menezes M.R.; Horvat N. State-of-the-art in radiomics of hepatocellular carcinoma: A review of basic principles, applications, and limitations. Abdom. Radiol. 2020, 45, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Tan, H.; Gao, F.; Hai, J.; Ning, P.; Chen, J.; Zhu, S.; Wang, M.; Dou, S.; Shi, D. Predicting the grade of hepatocellular carcinoma based on non-contrast-enhanced MRI radiomics signature. Eur. Radiol. 2019, 29, 2802–2811. [Google Scholar] [CrossRef]
- Chong, H.-H.; Yang, L.; Sheng, R.-F.; Yu, Y.-L.; Wu, D.-J.; Rao, S.-X.; Yang, C.; Zeng, M.-S. Multi-scale and multi-parametric radiomics of gadoxetate disodium–enhanced MRI predicts microvascular invasion and outcome in patients with solitary hepatocellular carcinoma ≤ 5 cm. Eur. Radiol. 2021, 31, 4824–4838. [Google Scholar] [CrossRef]
- Fu, J.; Cao, S.-J.; Song, L.; Tong, X.-Q.; Wang, J.; Yang, M.; Zou, Y.-H. Radiomics/Radiogenomics in hepatocellular carcinoma: Applications and challenges in interventional management. Iliver 2022, 1, 96–100. [Google Scholar] [CrossRef]
- Papadimitroulas, P.; Brocki, L.; Chung, N.C.; Marchadour, W.; Vermet, F.; Gaubert, L.; Eleftheriadis, V.; Plachouris, D.; Visvikis, D.; Kagadis, G.C.; et al. Artificial intelligence: Deep learning in oncological radiomics and challenges of interpretability and data harmonization. Phys. Med. 2021, 83, 108–121. [Google Scholar] [CrossRef]
- Avanzo, M.; Wei, L.; Stancanello, J.; Vallières, M.; Rao, A.; Morin, O.; Mattonen, S.A.; El Naqa, I. Machine and deep learning methods for radiomics. Med. Phys. 2020, 47, e185–e202. [Google Scholar] [CrossRef]
- Cai, W.; He, B.; Hu, M.; Zhang, W.; Xiao, D.; Yu, H.; Song, Q.; Xiang, N.; Yang, J.; He, S.; et al. A radiomics-based nomogram for the preoperative prediction of posthepatectomy liver failure in patients with hepatocellular carcinoma. Surg. Oncol. 2019, 28, 78–85. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, L.; Jiang, B.; Zhao, K.; Zhang, Y.; Xie, X. Clinical application of deep learning and radiomics in hepatic disease imaging: A systematic scoping review. Br. J. Radiol. 2022, 95, 20211136. [Google Scholar] [CrossRef] [PubMed]
- Xiang, F.; Liang, X.; Yang, L.; Liu, X.; Yan, S. CT radiomics nomogram for the preoperative prediction of severe post-hepatectomy liver failure in patients with huge (≥10 cm) hepatocellular carcinoma. World J. Surg. Oncol. 2021, 19, 344. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Liu, Z.; Mo, Y.; Li, B.; Zhou, Q.; Peng, S.; Li, S.; Kuang, M. Prediction of Post-hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma Based on Radiomics Using Gd-EOB-DTPA-Enhanced MRI: The Liver Failure Model. Front. Oncol. 2021, 11, 605296. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, D.; Wu, T.-J.; Lee, C.-F.; Chan, K.-M.; Lee, W.-C.; Chen, M.-F. Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: A 20-year experience. Surgery 2010, 147, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Rahbari, N.N.; Garden, O.J.; Padbury, R.; Brooke-Smith, M.; Crawford, M.; Adam, R.; Koch, M.; Makuuchi, M.; Dematteo, R.P.; Christophi, C.; et al. Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011, 149, 713–724. [Google Scholar] [CrossRef]
- Liang, M.; Zhao, J.; Xie, B.; Li, C.; Yin, X.; Cheng, L.; Wang, J.; Zhang, L. MR liver imaging with Gd-EOB-DTPA: The need for different delay times of the hepatobiliary phase in patients with different liver function. Eur. J. Radiol. 2016, 85, 546–552. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Xie, Y.; Wei, J.; Li, W.; Ye, Z.; Zhu, Z.; Tian, J.; Li, X. MRI-Based Radiomics Signature: A Potential Biomarker for Identifying Glypican 3-Positive Hepatocellular Carcinoma. J. Magn. Reson. Imaging 2020, 52, 1679–1687. [Google Scholar] [CrossRef]
- Monti, S.; Tamayo, P.; Mesirov, J.; Golub, T. Consensus Clustering: A Resampling-Based Method for Class Discovery and Visualization of Gene Expression Microarray Data. Mach. Learn. 2003, 52, 91–118. [Google Scholar] [CrossRef]
- Șenbabaoğlu, Y.; Michailidis, G.; Li, J.Z. Critical limitations of consensus clustering in class discovery. Sci. Rep. 2014, 4, 6207. [Google Scholar] [CrossRef]
- Brière, G.; Darbo, É.; Thébault, P.; Uricaru, R. Consensus clustering applied to multi-omics disease subtyping. BMC Bioinformatics. 2021, 6, 361. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, M.D.; Hayes, D.N. ConsensusClusterPlus: A class discovery tool with confidence assessments and item tracking. Bioinforma. Oxf. Engl. 2010, 26, 1572–1573. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.-A.; Petrowsky, H.; DeOliveira, M.L.; Graf, R. Strategies for Safer Liver Surgery and Partial Liver Transplantation. New Engl. J. Med. 2007, 356, 1545–1559. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of Liver Function in Patients with Hepatocellular Carcinoma: A New Evidence-Based Approach—The ALBI Grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Shimose, S.; Yamamura, S.; Nakano, D.; Tanaka, M.; Torimura, T. Changes in prognostic factors for patients with hepatocellular carcinoma underwent transarterial chemoembolization with the transition of the time: Child-Pugh class, Albumin-Bilirubin grade, and then. Ann. Transl. Med. 2020, 8, 1045. [Google Scholar] [CrossRef]
- Reig, M.; Forner, A.; Rimola, J.; Ferrer-Fàbrega, J.; Burrel, M.; Garcia-Criado, Á.; Kelley, R.K.; Galle, P.R.; Mazzaferro, V.; Salem, R.; et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J. Hepatol. 2022, 76, 681–693. [Google Scholar] [CrossRef]
- Cieslak, K.P.; Runge, J.H.; Heger, M.; Stoker, J.; Bennink, R.J.; van Gulik, T.M. New Perspectives in the Assessment of Future Remnant Liver. Dig. Surg. 2014, 31, 255–268. [Google Scholar] [CrossRef]
- Shi, Z.; Cai, W.; Feng, X.; Cai, J.; Liang, Y.; Xu, J.; Zhen, J.; Liang, X. Radiomics Analysis of Gd-EOB-DTPA Enhanced Hepatic MRI for Assessment of Functional Liver Reserve. Acad. Radiol. 2022, 29, 213–218. [Google Scholar] [CrossRef]
- Hosny, A.; Aerts, H.J.; Mak, R.H. Handcrafted versus deep learning radiomics for prediction of cancer therapy response. Lancet Digit. Health 2019, 1, e106–e107. [Google Scholar] [CrossRef]
- Fan, M.; Chen, H.; You, C.; Liu, L.; Gu, Y.; Peng, W.; Gao, X.; Li, L. Radiomics of Tumor Heterogeneity in Longitudinal Dynamic Contrast-Enhanced Magnetic Resonance Imaging for Predicting Response to Neoadjuvant Chemotherapy in Breast Cancer. Front. Mol. Biosci. 2021, 8, 622219. [Google Scholar] [CrossRef]
- Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; Depristo, M.; Chou, K.; Cui, C.; Corrado, G.; Thrun, S.; Dean, J. A guide to deep learning in healthcare. Nat. Med. 2019, 25, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Yoon, J.S.; Lee, S.S.; Suk, H.-I.; Park, B.; Sung, Y.S.; Hong, S.B.; Ryu, H. Deep Learning-Based Assessment of Functional Liver Capacity Using Gadoxetic Acid-Enhanced Hepatobiliary Phase MRI. Korean J. Radiol. 2022, 23, 720. [Google Scholar] [CrossRef]
- Ba-Ssalamah, A.; Bastati, N.; Wibmer, A.; Fragner, R.; Hodge, J.C.; Trauner, M.; Herold, C.J.; Bashir, M.R.; Van Beers, B.E. Hepatic gadoxetic acid uptake as a measure of diffuse liver disease: Where are we? Hepatic GA Uptake as a Measure of Diffuse Liver Disease. J. Magn. Reson. Imaging. 2017, 45, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, M.R.; Gillies, R.J. The Biological Meaning of Radiomic Features. Radiology 2021, 298, 505–516. [Google Scholar] [CrossRef] [PubMed]



| Overall (n = 276) | Subgroup 1 (n = 138) | Subgroup 2 (n = 138) | p Value | |
|---|---|---|---|---|
| Gender | 0.382 | |||
| Female | 38 (13.8%) | 22 (15.9%) | 16 (11.6%) | |
| Male | 238 (86.2%) | 116 (84.1%) | 122 (88.4%) | |
| Age (years) | 0.003 * | |||
| ≤55 | 197 (71.4%) | 110 (79.7%) | 87 (63.0%) | |
| >55 | 79 (28.6%) | 28 (20.3%) | 51 (37.0%) | |
| BMI (kg/m2) | 0.224 | |||
| ≤27 | 249 (90.2%) | 121 (87.7%) | 128 (92.8%) | |
| >27 | 27 (9.8%) | 17 (12.3%) | 10 (7.2%) | |
| Etiology | 0.887 | |||
| HBV | 212 (76.8%) | 105 (76.1%) | 107 (77.5%) | |
| Non-HBV | 64 (23.2%) | 33 (23.9%) | 31 (22.5%) | |
| Cirrhosis | 0.070 | |||
| Cirrhosis | 146 (52.9%) | 65 (47.1%) | 81 (58.7%) | |
| Non-cirrhosis | 130 (47.1%) | 73 (52.9%) | 57 (41.3%) | |
| Tumor size (cm) | 0.278 | |||
| ≤5 | 130 (47.1%) | 70 (50.7%) | 60 (43.5%) | |
| >5 | 146 (52.9%) | 68 (49.3%) | 78 (56.5%) | |
| Resection extent | 0.691 | |||
| Major | 80 (29.0%) | 38 (27.5%) | 42 (30.4%) | |
| Minor | 196 (71.0%) | 100 (72.5%) | 96 (69.6%) | |
| Laparoscopy | 1.000 | |||
| No | 234 (84.8%) | 117 (84.8%) | 117 (84.8%) | |
| Yes | 42 (15.2%) | 21 (15.2%) | 21 (15.2%) | |
| Blood loss (mL) | 0.288 | |||
| ≤400 | 222 (80.4%) | 107 (77.5%) | 115 (83.3%) | |
| >400 | 54 (19.6%) | 31 (22.5%) | 23 (16.7%) | |
| Hepatectomy time (min) | 0.753 | |||
| ≤60 | 227 (82.2%) | 112 (81.2%) | 115 (83.3%) | |
| >60 | 49 (17.8%) | 26 (18.8%) | 23 (16.7%) | |
| ALT (IU/L) | 0.181 | |||
| ≤42 | 158 (57.2%) | 85 (61.6%) | 73 (52.9%) | |
| >42 | 118 (42.8%) | 53 (38.4%) | 65 (47.1%) | |
| AST (IU/L) | 0.181 | |||
| ≤42 | 158 (57.2%) | 85 (61.6%) | 73 (52.9%) | |
| >42 | 118 (42.8%) | 53 (38.4%) | 65 (47.1%) | |
| Platelet (×109/L) | 0.164 | |||
| ≤125 | 96 (34.8%) | 42 (30.4%) | 54 (39.1%) | |
| >125 | 180 (65.2%) | 96 (69.6%) | 84 (60.9%) | |
| Child–Pugh grade | 0.622 | |||
| A | 272 (98.6%) | 137 (99.3%) | 135 (97.8%) | |
| B | 4 (1.4%) | 1 (0.7%) | 3 (2.2%) | |
| MELD score | 1.000 | |||
| ≤9 | 259 (93.8%) | 130 (94.2%) | 129 (93.5%) | |
| >9 | 17 (6.16%) | 8 (5.80%) | 9 (6.52%) | |
| ALBI grade | 0.011 * | |||
| Grade 1 | 126 (45.7%) | 74 (53.6%) | 52 (37.7%) | |
| Grade 2/3 | 150 (54.3%) | 64 (46.4%) | 86 (62.3%) | |
| ICG-R15 (%) | 3.7 (0.3–33.5) | 3.2 (0.3–25.3) | 4.1(0.3–33.5) | 0.002 * |
| ICG-PDR (%/min) | 21.9 (7.3–39.4) | 22.9 (8.5–39.4) | 21.1 (7.3–35.7) | 0.002 * |
| PHLF | 0.001 * | |||
| Non-PHLF | 211 (76.4%) | 118 (85.5%) | 93 (67.4%) | |
| PHLF | 65 (23.6%) | 20 (14.5%) | 45 (32.6%) | |
| Postoperative complication # | 0.030 * | |||
| Not significant | 241 (87.3%) | 127 (92.0%) | 114 (82.6%) | |
| Significant | 35 (12.7%) | 11 (8.0%) | 24 (17.4%) | |
| Length of hospital stay (days) | 0.003 * | |||
| ≤18 | 140 (50.7%) | 83 (60.1%) | 57 (41.3%) | |
| >18 | 136 (49.3%) | 55 (39.9%) | 81% (58.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Li, C.; Chen, G.; Feng, K.; Chen, Z.; Xia, F.; Cai, P.; Zhang, L.; Sparrelid, E.; Brismar, T.B.; et al. Unsupervised Machine Learning of MRI Radiomics Features Identifies Two Distinct Subgroups with Different Liver Function Reserve and Risks of Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers 2023, 15, 3197. https://doi.org/10.3390/cancers15123197
Wang Q, Li C, Chen G, Feng K, Chen Z, Xia F, Cai P, Zhang L, Sparrelid E, Brismar TB, et al. Unsupervised Machine Learning of MRI Radiomics Features Identifies Two Distinct Subgroups with Different Liver Function Reserve and Risks of Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers. 2023; 15(12):3197. https://doi.org/10.3390/cancers15123197
Chicago/Turabian StyleWang, Qiang, Changfeng Li, Geng Chen, Kai Feng, Zhiyu Chen, Feng Xia, Ping Cai, Leida Zhang, Ernesto Sparrelid, Torkel B. Brismar, and et al. 2023. "Unsupervised Machine Learning of MRI Radiomics Features Identifies Two Distinct Subgroups with Different Liver Function Reserve and Risks of Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma" Cancers 15, no. 12: 3197. https://doi.org/10.3390/cancers15123197
APA StyleWang, Q., Li, C., Chen, G., Feng, K., Chen, Z., Xia, F., Cai, P., Zhang, L., Sparrelid, E., Brismar, T. B., & Ma, K. (2023). Unsupervised Machine Learning of MRI Radiomics Features Identifies Two Distinct Subgroups with Different Liver Function Reserve and Risks of Post-Hepatectomy Liver Failure in Patients with Hepatocellular Carcinoma. Cancers, 15(12), 3197. https://doi.org/10.3390/cancers15123197








