Moving the Target on the Optimal Adjuvant Strategy for Resected Pancreatic Cancers: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
2. Results
3. Combination Regimens vs. Gemcitabine Alone
4. Indirect Comparisons
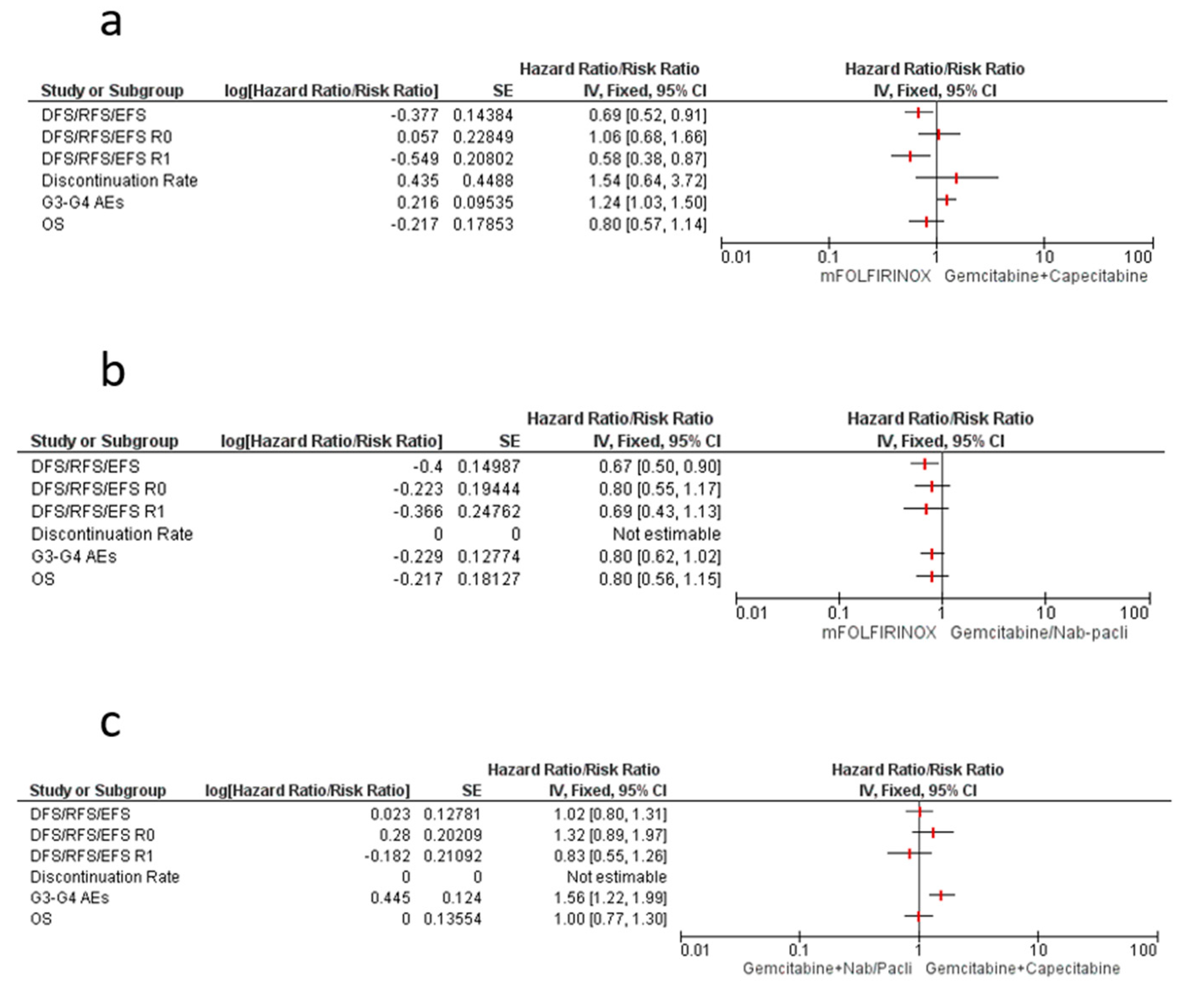
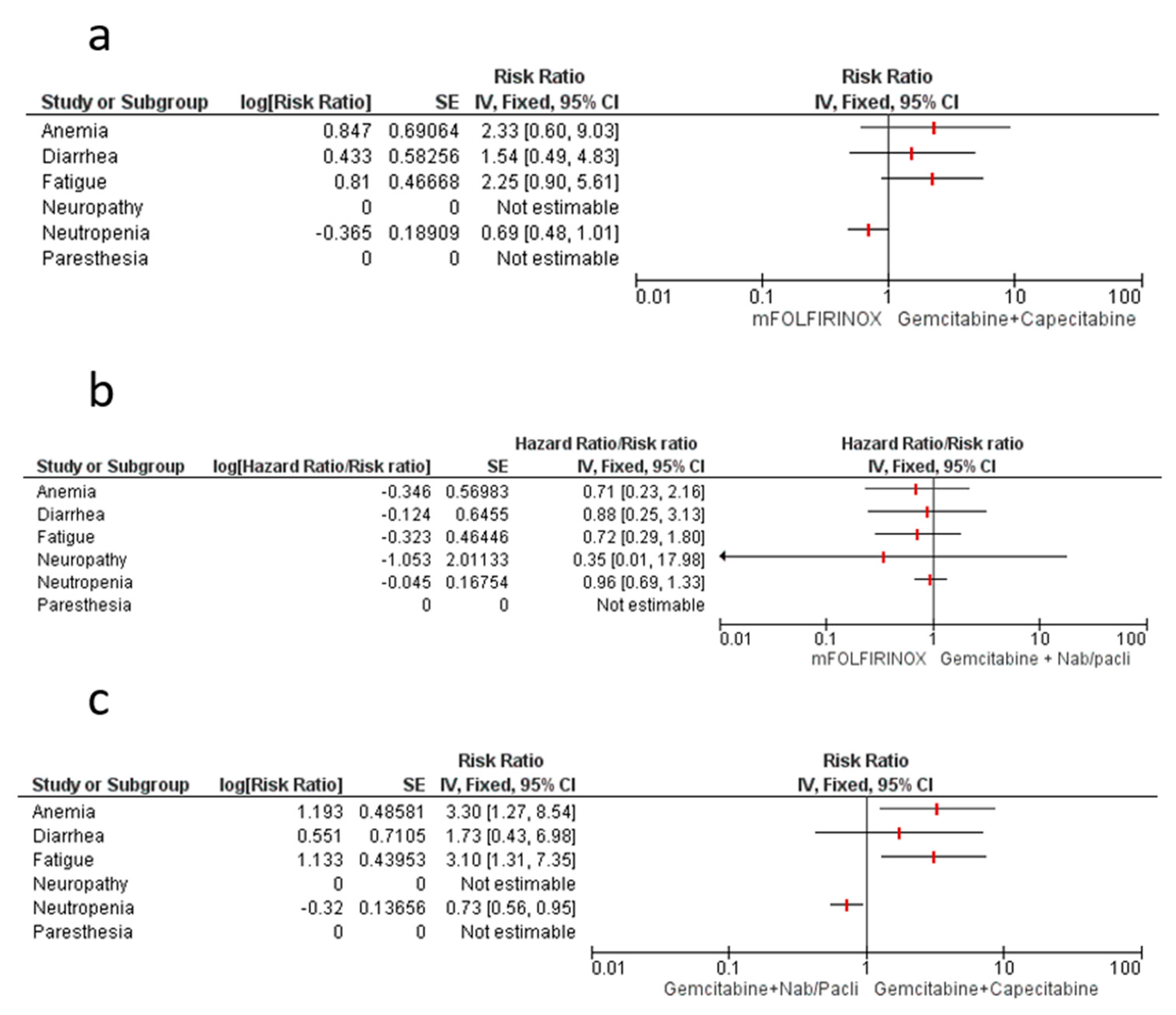
4.1. mFOLFIRINOX vs. Gemcitabine–Capecitabine
4.2. mFOLFIRINOX vs. Gemcitabine–Nab/Paclitaxel
4.3. Gemcitabine–Nab/Paclitaxel vs. Gemcitabine–Capecitabine
5. Risk of Bias Assessment (JADAD Scale)
6. Discussion
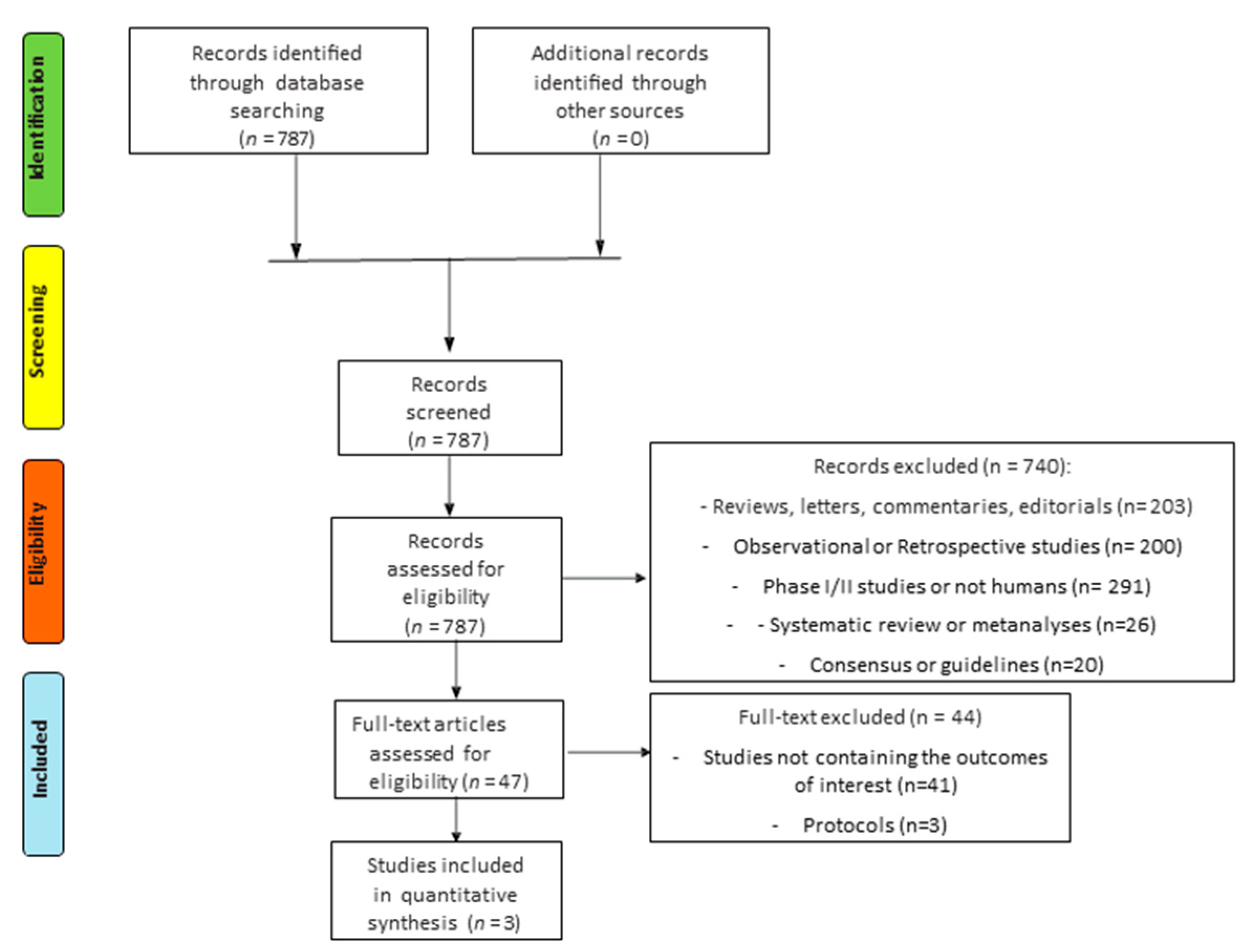
7. Materials and Methods
7.1. Search for Trials
7.2. Selection Criteria
7.3. Data Extraction and Risk of Bias Assessment
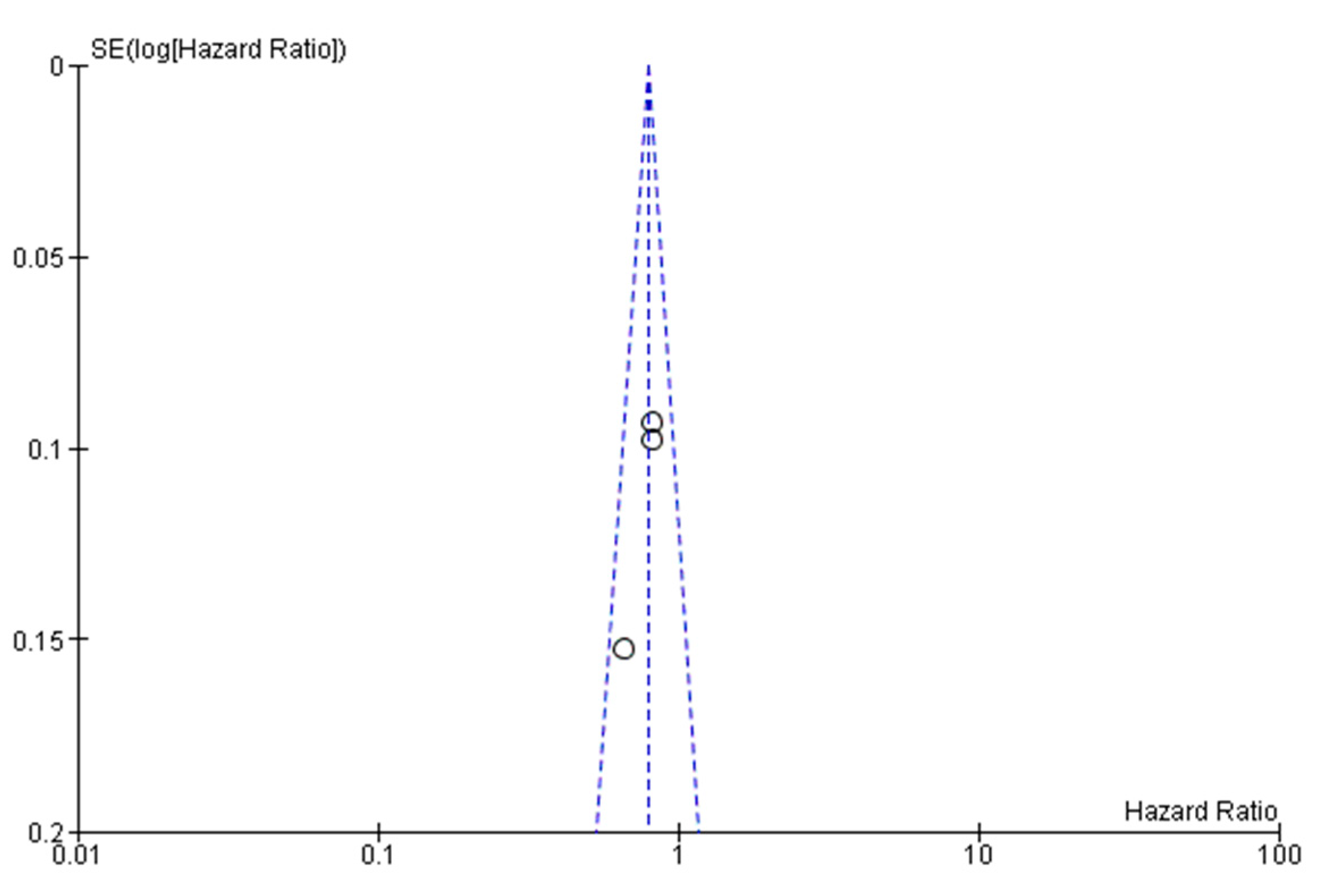
7.4. Assessment of Heterogeneity and Statistical Analysis
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Ryan, D.P.; Hong, T.S.; Bardeesy, N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014, 371, 1039–1049. [Google Scholar] [CrossRef]
- Kleeff, J.; Korc, M.; Apte, M.; La Vecchia, C.; Johnson, C.D.; Biankin, A.V.; Neale, R.E.; Tempero, M.; Tuveson, D.A.; Hruban, R.H.; et al. Pancreatic cancer. Nat. Rev. Dis. Primers 2016, 2, 16022. [Google Scholar] [CrossRef]
- Kamisawa, T.; Wood, L.D.; Itoi, T.; Takaori, K. Pancreatic cancer. Lancet 2016, 388, 73–85. [Google Scholar] [CrossRef]
- Redmond, K.J.; Wolfgang, C.L.; Sugar, E.A.; Ahn, J.; Nathan, H.; Laheru, D.; Edil, B.H.; Choti, M.A.; Pawlik, T.M.; Hruban, R.H.; et al. Adjuvant chemoradiation therapy for adenocarcinoma of the distal pancreas. Ann. Surg. Oncol. 2010, 17, 3112–3119. [Google Scholar] [CrossRef][Green Version]
- Neoptolemos, J.P.; Kleeff, J.; Michl, P.; Costello, E.; Greenhalf, W.; Palmer, D.H. Therapeutic developments in pancreatic cancer: Current and future perspectives. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 333–348. [Google Scholar] [CrossRef]
- Groot, V.P.; Rezaee, N.; Wu, W.; Cameron, J.L.; Fishman, E.K.; Hruban, R.H.; Weiss, M.J.; Zheng, L.; Wolfgang, C.L.; He, J. Patterns, Timing, and Predictors of Recurrence Following Pancreatectomy for Pancreatic Ductal Adenocarcinoma. Ann. Surg. 2018, 267, 936–945. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Dunn, J.A.; Stocken, D.D.; Almond, J.; Link, K.; Beger, H.; Bassi, C.; Falconi, M.; Pederzoli, P.; Dervenis, C.; et al. Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: A randomised controlled trial. Lancet 2001, 358, 1576–1585. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Stocken, D.D.; Friess, H.; Bassi, C.; Dunn, J.A.; Hickey, H.; Beger, H.; Fernandez-Cruz, L.; Dervenis, C.; Lacaine, F.; et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N. Engl. J. Med. 2004, 350, 1200–1210. [Google Scholar] [CrossRef]
- Oettle, H.; Post, S.; Neuhaus, P.; Gellert, K.; Langrehr, J.; Ridwelski, K.; Schramm, H.; Fahlke, J.; Zuelke, C.; Burkart, C.; et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: A randomized controlled trial. JAMA 2007, 297, 267–277. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Stocken, D.D.; Bassi, C.; Ghaneh, P.; Cunningham, D.; Goldstein, D.; Padbury, R.; Moore, M.J.; Gallinger, S.; Mariette, C.; et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs. gemcitabine following pancreatic cancer resection: A randomized controlled trial. JAMA 2010, 304, 1073–1081. [Google Scholar] [CrossRef]
- Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; Nakamori, S.; Sakamoto, H.; et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: A phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 2016, 388, 248–257. [Google Scholar] [CrossRef]
- Neoptolemos, J.P.; Palmer, D.H.; Ghaneh, P.; Psarelli, E.E.; Valle, J.W.; Halloran, C.M.; Faluyi, O.; O’Reilly, D.A.; Cunningham, D.; Wadsley, J.; et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet 2017, 389, 1011–1024. [Google Scholar] [CrossRef]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef]
- Tempero, M.A.; Reni, M.; Riess, H.; Pelzer, U.; O’Reilly, E.M.; Winter, J.M.; Oh, D.-Y.; Li, C.-P.; Tortora, G.; Chang, H.-M.; et al. APACT: Phase III, multicenter, international, open-label, randomized trial of adjuvant nab-paclitaxel plus gemcitabine (nab-P/G) vs gemcitabine (G) for surgically resected pancreatic adenocarcinoma. J. Clin. Oncol. 2019, 37, 4000. [Google Scholar] [CrossRef]
- Kang, J.; Hwang, I.; Yoo, C.; Kim, K.P.; Jeong, J.H.; Chang, H.M.; Lee, S.S.; Park, D.H.; Song, T.J.; Seo, D.W.; et al. Nab-paclitaxel plus gemcitabine versus FOLFIRINOX as the first-line chemotherapy for patients with metastatic pancreatic cancer: Retrospective analysis. Invest. New Drugs 2018, 36, 732–741. [Google Scholar] [CrossRef]
- Van den Broeck, A.; Sergeant, G.; Ectors, N.; Van Steenbergen, W.; Aerts, R.; Topal, B. Patterns of recurrence after curative resection of pancreatic ductal adenocarcinoma. Eur. J. Surg. Oncol. 2009, 35, 600–604. [Google Scholar] [CrossRef]
- Kayahara, M.; Nagakawa, T.; Ueno, K.; Ohta, T.; Takeda, T.; Miyazaki, I. An evaluation of radical resection for pancreatic cancer based on the mode of recurrence as determined by autopsy and diagnostic imaging. Cancer 1993, 72, 2118–2123. [Google Scholar] [CrossRef]
- Mayo, S.C.; Gilson, M.M.; Herman, J.M.; Cameron, J.L.; Nathan, H.; Edil, B.H.; Choti, M.A.; Schulick, R.D.; Wolfgang, C.L.; Pawlik, T.M. Management of patients with pancreatic adenocarcinoma: National trends in patient selection, operative management, and use of adjuvant therapy. J. Am. Coll. Surg. 2012, 214, 33–45. [Google Scholar] [CrossRef]
- Aloia, T.A.; Aloia, T.E.; Lee, J.E.; Vauthey, J.N.; Abdalla, E.K.; Wolff, R.A.; Varadhachary, G.R.; Abbruzzese, J.L.; Crane, C.H.; Evans, D.B.; et al. Delayed recovery after pancreaticoduodenectomy: A major factor impairing the delivery of adjuvant therapy? J. Am. Coll. Surg. 2007, 204, 347–355. [Google Scholar] [CrossRef]
- Wu, W.; He, J.; Cameron, J.L.; Makary, M.; Soares, K.; Ahuja, N.; Rezaee, N.; Herman, J.; Zheng, L.; Laheru, D.; et al. The impact of postoperative complications on the administration of adjuvant therapy following pancreaticoduodenectomy for adenocarcinoma. Ann. Surg. Oncol. 2014, 21, 2873–2881. [Google Scholar] [CrossRef]
- Lambert, A.; Gavoille, C.; Conroy, T. Current status on the place of FOLFIRINOX in metastatic pancreatic cancer and future directions. Ther. Adv. Gastroenterol. 2017, 10, 631–645. [Google Scholar] [CrossRef]
- Yang, F.; Jin, C.; Fu, D.L.; Warshaw, A.L. Modified FOLFIRINOX for resected pancreatic cancer: Opportunities and challenges. World J. Gastroenterol. 2019, 25, 2839–2845. [Google Scholar] [CrossRef]
- Wang-Gillam, A.; Hubner, R.A.; Siveke, J.T.; Von Hoff, D.D.; Belanger, B.; de Jong, F.A.; Mirakhur, B.; Chen, L.T. NAPOLI-1 phase 3 study of liposomal irinotecan in metastatic pancreatic cancer: Final overall survival analysis and characteristics of long-term survivors. Eur. J. Cancer 2019, 108, 78–87. [Google Scholar] [CrossRef]
- Kindler, H.L. A Glimmer of Hope for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2463–2464. [Google Scholar] [CrossRef]
- Schlick, K.; Magnes, T.; Ratzinger, L.; Jaud, B.; Weiss, L.; Melchardt, T.; Greil, R.; Egle, A. Novel models for prediction of benefit and toxicity with FOLFIRINOX treatment of pancreatic cancer using clinically available parameters. PLoS ONE 2018, 13, e0206688. [Google Scholar] [CrossRef]
- de Jesus, V.H.F.; Camandaroba, M.P.G.; Donadio, M.D.S.; Cabral, A.; Muniz, T.P.; de Moura Leite, L.; Sant’Ana, L.F. Retrospective comparison of the efficacy and the toxicity of standard and modified FOLFIRINOX regimens in patients with metastatic pancreatic adenocarcinoma. J. Gastrointest. Oncol. 2018, 9, 694–707. [Google Scholar] [CrossRef]
- Akahori, T.; Sho, M.; Yanagimoto, H.; Satoi, S.; Nagai, M.; Nishiwada, S.; Nakagawa, K.; Nakamura, K.; Yamamoto, T.; Hirooka, S.; et al. Phase II Study of the Triple Combination Chemotherapy of SOXIRI (S-1/Oxaliplatin/Irinotecan) in Patients with Unresectable Pancreatic Ductal Adenocarcinoma. Oncologist 2019, 24, 749–e224. [Google Scholar] [CrossRef]
- Yadav, D.K.; Bai, X.; Yadav, R.K.; Singh, A.; Li, G.; Ma, T.; Chen, W.; Liang, T. Liquid biopsy in pancreatic cancer: The beginning of a new era. Oncotarget 2018, 9, 26900–26933. [Google Scholar] [CrossRef]
- Tjensvoll, K.; Lapin, M.; Buhl, T.; Oltedal, S.; Steen-Ottosen Berry, K.; Gilje, B.; Søreide, J.A.; Javle, M.; Nordgård, O.; Smaaland, R. Clinical relevance of circulating KRAS mutated DNA in plasma from patients with advanced pancreatic cancer. Mol. Oncol. 2016, 10, 635–643. [Google Scholar] [CrossRef]
- Berger, A.W.; Schwerdel, D.; Ettrich, T.J.; Hann, A.; Schmidt, S.A.; Kleger, A.; Marienfeld, R.; Seufferlein, T. Targeted deep sequencing of circulating tumor DNA in metastatic pancreatic cancer. Oncotarget 2018, 9, 2076–2085. [Google Scholar] [CrossRef] [PubMed]
- Nakano, Y.; Kitago, M.; Matsuda, S.; Nakamura, Y.; Fujita, Y.; Imai, S.; Shinoda, M.; Yagi, H.; Abe, Y.; Hibi, T.; et al. KRAS mutations in cell-free DNA from preoperative and postoperative sera as a pancreatic cancer marker: A retrospective study. Br. J. Cancer 2018, 118, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.; Cohen, J.; Lipton, L.; Tie, J.; Javed, A.A.; Li, L.; Goldstein, D.; Cooray, P.; Nagrial, A.; Burge, M.E.; et al. Potential role of circulating tumor DNA (ctDNA) in the early diagnosis and post-operative management of localised pancreatic cancer. J. Clin. Oncol. 2017, 35, 4101. [Google Scholar] [CrossRef]
- Fanale, D.; Iovanna, J.L.; Calvo, E.L.; Berthezene, P.; Belleau, P.; Dagorn, J.C.; Ancona, C.; Catania, G.; D’Alia, P.; Galvano, A.; et al. Analysis of germline gene copy number variants of patients with sporadic pancreatic adenocarcinoma reveals specific variations. Oncology 2013, 85, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Sinn, M.; Bahra, M.; Liersch, T.; Gellert, K.; Messmann, H.; Bechstein, W.; Waldschmidt, D.; Jacobasch, L.; Wilhelm, M.; Rau, B.M.; et al. CONKO-005: Adjuvant Chemotherapy with Gemcitabine Plus Erlotinib Versus Gemcitabine Alone in Patients After R0 Resection of Pancreatic Cancer: A Multicenter Randomized Phase III Trial. J. Clin. Oncol. 2017, 35, 3330–3337. [Google Scholar] [CrossRef] [PubMed]
- Oettle, H.; Neuhaus, P.; Hochhaus, A.; Hartmann, J.T.; Gellert, K.; Ridwelski, K.; Niedergethmann, M.; Zülke, C.; Fahlke, J.; Arning, M.B.; et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA 2013, 310, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.W.; Palmer, D.; Jackson, R.; Cox, T.; Neoptolemos, J.P.; Ghaneh, P.; Rawcliffe, C.L.; Bassi, C.; Stocken, D.D.; Cunningham, D.; et al. Optimal duration and timing of adjuvant chemotherapy after definitive surgery for ductal adenocarcinoma of the pancreas: Ongoing lessons from the ESPAC-3 study. J. Clin. Oncol. 2014, 32, 504–512. [Google Scholar] [CrossRef]
- Labori, K.J.; Katz, M.H.; Tzeng, C.W.; Bjørnbeth, B.A.; Cvancarova, M.; Edwin, B.; Kure, E.H.; Eide, T.J.; Dueland, S.; Buanes, T.; et al. Impact of early disease progression and surgical complications on adjuvant chemotherapy completion rates and survival in patients undergoing the surgery first approach for resectable pancreatic ductal adenocarcinoma—A population-based cohort study. Acta Oncol. 2016, 55, 265–277. [Google Scholar] [CrossRef]
- Tzeng, C.W.; Tran Cao, H.S.; Lee, J.E.; Pisters, P.W.; Varadhachary, G.R.; Wolff, R.A.; Abbruzzese, J.L.; Crane, C.H.; Evans, D.B.; Wang, H.; et al. Treatment sequencing for resectable pancreatic cancer: Influence of early metastases and surgical complications on multimodality therapy completion and survival. J. Gastrointest. Surg. 2014, 18, 16–24. [Google Scholar] [CrossRef]
- Altman, A.M.; Wirth, K.; Marmor, S.; Lou, E.; Chang, K.; Hui, J.Y.C.; Tuttle, T.M.; Jensen, E.H.; Denbo, J.W. Completion of Adjuvant Chemotherapy After Upfront Surgical Resection for Pancreatic Cancer Is Uncommon Yet Associated With Improved Survival. Ann. Surg. Oncol. 2019, 26, 4108–4116. [Google Scholar] [CrossRef]
- Tong, H.; Fan, Z.; Liu, B.; Lu, T. The benefits of modified FOLFIRINOX for advanced pancreatic cancer and its induced adverse events: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 8666. [Google Scholar] [CrossRef]
- Chllamma, M.K.; Cook, N.; Dhani, N.C.; Giby, K.; Dodd, A.; Wang, L.; Hedley, D.W.; Moore, M.J.; Knox, J.J. FOLFIRINOX for advanced pancreatic cancer: The Princess Margaret Cancer Centre experience. Br. J. Cancer 2016, 115, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Jüni, P.; Altman, D.G.; Egger, M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001, 323, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Bucher, H.C.; Guyatt, G.H.; Griffith, L.E.; Walter, S.D. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J. Clin. Epidemiol. 1997, 50, 683–691. [Google Scholar] [CrossRef]
- Glenny, A.M.; Altman, D.G.; Song, F.; Sakarovitch, C.; Deeks, J.J.; D’Amico, R.; Bradburn, M.; Eastwood, A.J.; Group, I.S.T.C. Indirect comparisons of competing interventions. Health Technol. Assess 2005, 9, 1–134. [Google Scholar] [CrossRef]
- Lumley, T. Network meta-analysis for indirect treatment comparisons. Stat. Med. 2002, 21, 2313–2324. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Review Manager (RevMan) [Computer Program], version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014.
- Casadei, R.; Di Marco, M.; Ricci, C.; Santini, D.; Serra, C.; Calculli, L.; D’Ambra, M.; Guido, A.; Morselli-Labate, A.M.; Minni, F. Neoadjuvant Chemoradiotherapy and Surgery Versus Surgery Alone in Resectable Pancreatic Cancer: A Single-Center Prospective, Randomized, Controlled Trial Which Failed to Achieve Accrual Targets. J. Gastrointest. Surg. 2015, 19, 1802–1812. [Google Scholar] [CrossRef]
- Motoi, F.; Unno, M.; Takahashi, H.; Okada, T.; Wada, K.; Sho, M.; Nagano, H.; Matsumoto, I.; Satoi, S.; Murakami, Y.; et al. Influence of preoperative anti-cancer therapy on resectability and perioperative outcomes in patients with pancreatic cancer: Project study by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J. Hepato Biliary Pancreat. Sci. 2014, 21, 148–158. [Google Scholar] [CrossRef]

| Study (Reference) | Drug | n | DFS/RFS/EFS HR (95% CI) | OS HR (95% CI) | G3–G5 AEs n. (%) | Discontinuation Rate n. (%) | R1 DFS/RFS/EFS HR (95% CI) | R0 DFS/RFS/EFS HR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Neoptolemos J.P.et al (ESPAC-4) [13] | Gem + Cape | 364 | 0.86 (0.73–1.02) | 0.82 (0.68–0.98) | 226/359 (63) | 11/364 | 0.90 (0.72–1.13) | 0.68 (0.49–0.93) |
| Gem | 366 | 199/366 (54) | 11/366 | |||||
| Tampero M.A. et al (APACT) [15] | Gem + Nab-P | 432 | 0.88 (0.73–1.06) | 0.82 (0.68–1.00) | 176/429 | NA | 0.75 (0.53–1.07) | 0.90 (0.72–1.13) |
| Gem | 434 | 96/423 | ||||||
| Conroy T. et al (PRODIGE 24) [14] | Folfirinox | 247 | 0.59 (0.47–0.74) | 0.66 (0.49–0.89) | 180 (75.5) | 80/247 | 0.52 (0.37–0.72) | 0.72 (0.53–0.98) |
| Gem | 246 | 128 (51.1) | 51/246 |
| Study (Reference) | Drug | Neutropenia n. (%) | Anemia n. (%) | Fatigue n. (%) | Diarrhea n. (%) | Neuropathy n. (%) | Paresthesia n. (%) |
|---|---|---|---|---|---|---|---|
| Neoptolemos J.P. et al. (ESPAC-4) [13] | Gem + Cape Gem | 137 (38) 89 (24) | 8 (2) 14 (4) | 20 (6) 19 (5) | 19 (5) 6 (2) | NA | NA |
| Tampero M.A. et al. (APACT) [15] | Gem + Nab-P Gem | 212 (49) 184 (43) | 63 (14) 33 (8) | 43 (10) 13 (3) | 22 (5) 4 (1) | 64 (15) 0 (0) | NA |
| Conroy T. et al. (PRODIGE 24) [14] | Folfirinox Gem | 67/238 (28.4) 63/243 (26) | 8 (3.4) 6 (2.5) | 26 (11) 11 (4.6) | 44 (18.6) 9 (3.7) | 22 (9.3) 0 (0) | 30 (12.7) 0 (0) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galvano, A.; Castiglia, M.; Rizzo, S.; Silvestris, N.; Brunetti, O.; Vaccaro, G.; Gristina, V.; Barraco, N.; Bono, M.; Guercio, G.; et al. Moving the Target on the Optimal Adjuvant Strategy for Resected Pancreatic Cancers: A Systematic Review with Meta-Analysis. Cancers 2020, 12, 534. https://doi.org/10.3390/cancers12030534
Galvano A, Castiglia M, Rizzo S, Silvestris N, Brunetti O, Vaccaro G, Gristina V, Barraco N, Bono M, Guercio G, et al. Moving the Target on the Optimal Adjuvant Strategy for Resected Pancreatic Cancers: A Systematic Review with Meta-Analysis. Cancers. 2020; 12(3):534. https://doi.org/10.3390/cancers12030534
Chicago/Turabian StyleGalvano, Antonio, Marta Castiglia, Sergio Rizzo, Nicola Silvestris, Oronzo Brunetti, Giovanni Vaccaro, Valerio Gristina, Nadia Barraco, Marco Bono, Giovanni Guercio, and et al. 2020. "Moving the Target on the Optimal Adjuvant Strategy for Resected Pancreatic Cancers: A Systematic Review with Meta-Analysis" Cancers 12, no. 3: 534. https://doi.org/10.3390/cancers12030534
APA StyleGalvano, A., Castiglia, M., Rizzo, S., Silvestris, N., Brunetti, O., Vaccaro, G., Gristina, V., Barraco, N., Bono, M., Guercio, G., Graceffa, G., Fulfaro, F., Gori, S., Bazan, V., & Russo, A. (2020). Moving the Target on the Optimal Adjuvant Strategy for Resected Pancreatic Cancers: A Systematic Review with Meta-Analysis. Cancers, 12(3), 534. https://doi.org/10.3390/cancers12030534










