Recommendations Favoring Anal Cytology as a Method for Anal Cancer Screening: A Systematic Review
Abstract
1. Introduction
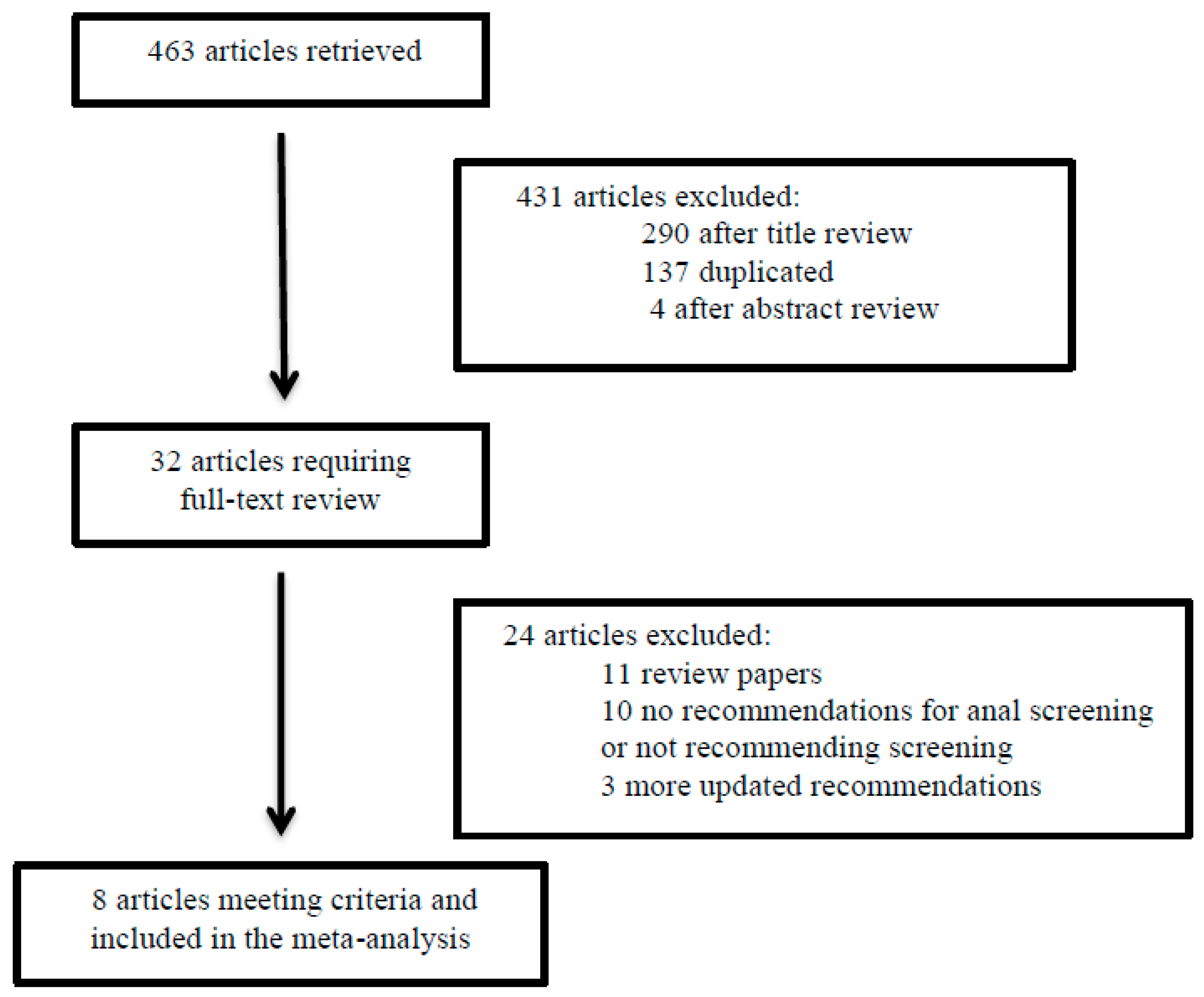
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lin, C.; Franceschi, S.; Clifford, G.M. Human papillomavirus types from infection to cancer in the anus, according to sex and HIV status: A systematic review and meta-analysis. Lancet Infect. Dis. 2018, 18, 198–206. [Google Scholar] [CrossRef]
- Smittenaar, C.R.; Petersen, K.A.; Stewart, K.; Moitt, N. Cancer incidence and mortality projections in the UK until 2035. Br. J. Cancer 2016, 115, 1147–1155. [Google Scholar] [CrossRef] [PubMed]
- Soeberg, M.J.; Rogers, K.; Currow, D.C.; Young, J.M. Trends in incidence and survival for anal cancer in New South Wales, Australia, 1972–2009. Cancer Epidemiol. 2015, 39, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Machalek, D.A.; Poynten, M.; Jin, F.; Fairley, C.K.; Farnsworth, A.; Garland, S.M.; Hillman, R.J.; Petoumenos, K.; Roberts, J.; Tabrizi, S.N.; et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: A systematic review and meta-analysis. Lancet Oncol. 2012, 13, 487–500. [Google Scholar] [CrossRef]
- Piketty, C.; Selinger-Leneman, H.; Bouvier, A.M.; Belot, A.; Mary-Krause, M.; Duvivier, C.; Bonmarchand, M.; Abramowitz, L.; Costagliola, D.; Grabar, S. Incidence of HIV-related anal cancer remains increased despite long-term combined antiretroviral treatment: Results from the French hospital database on HIV. J. Clin. Oncol. 2012, 30, 4360–4366. [Google Scholar] [CrossRef]
- Wang, C.C.; Silverberg, M.J.; Abrams, D.I. Non-AIDS-Defining Malignancies in the HIV-Infected Population. Curr. Infect. Dis. Rep. 2014, 16, 406. [Google Scholar] [CrossRef]
- Grulich, A.E.; van Leeuwen, M.T.; Falster, M.O.; Vajdic, C.M. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: A meta-analysis. Lancet 2007, 370, 59–67. [Google Scholar] [CrossRef]
- Madeleine, M.M.; Finch, J.L.; Lynch, C.F.; Goodman, M.T.; Engels, E.A. HPV-related cancers after solid organ transplantation in the United States. Am. J. Transplant. 2013, 13, 3202–3209. [Google Scholar] [CrossRef]
- Howlader, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. SEER Cancer Statistics Review, 1975–2016. National Cancer Institute: Bethesda, MD, USA. Available online: https://seer.cancer.gov/csr/1975_2016/ (accessed on 13 July 2019).
- Oette, M.; Mosthaf, F.A.; Sautter-Bihl, M.L.; Esser, S. HIV-Associated Anal Dysplasia and Anal Carcinoma. Oncol. Res. Treat. 2017, 40, 100–105. [Google Scholar] [CrossRef]
- Koskan, A.M.; Brennhofer, S.A.; Helitzer, D.L. Screening for anal cancer precursors among patients living with HIV in the absence of national guidelines: practitioners’ perspectives. Cancer Causes Control 2019, 30, 989–996. [Google Scholar] [CrossRef]
- Patel, J.; Salit, I.E.; Berry, M.J.; de Pokomandy, A.; Nathan, M.; Fishman, F.; Palefsky, J.; Tinmouth, J. Environmental scan of anal cancer screening practices: Worldwide survey results. Cancer Med. 2014, 3, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- Chiao, E.Y.; Giordano, T.P.; Palefsky, J.M.; Tyring, S.; El Serag, H. Screening HIV-infected individuals for anal cancer precursor lesions: A systematic review. Clin. Infect. Dis. 2006, 43, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, A.; Sheaff, M.; Stirrup, O.; Cappello, C.; Bowring, J.; Cuming, T.; De Masi, A.; Rosenthal, A.N.; Nathan, M. Performance of anal cytology compared with high-resolution anoscopy and histology in women with lower anogenital tract neoplasia. Clin. Infect. Dis. 2018, 67, 1262–1268. [Google Scholar] [CrossRef] [PubMed]
- Dantal, J.; Soulillou, J.P. Immunosuppressive drugs and the risk of cancer after organ transplantation. N. Engl. J. Med. 2005, 352, 1371–1373. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- New York State Department of Health AIDS Institute. Anal Dysplasia and Cancer Guideline. Available online: https://www.hivguidelines.org/hiv-care/anal-dysplasia-cancer# (accessed on 4 October 2019).
- Ortoski, R.A.; Kell, C.S. Anal cancer and screening guidelines for human papillomavirus in men. J. Am. Osteopath. Assoc. 2011, 111, S35–S43. [Google Scholar] [PubMed]
- Aberg, J.A.; Gallant, J.E.; Ghanem, K.G.; Emmanuel, P.; Zingman, B.S.; Horberg, M.A.; Infectious Diseases Society of America. Primary care guidelines for the management of persons infected with HIV: 2013 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin. Infect. Dis. 2014, 58, 1–10. [Google Scholar] [CrossRef]
- Stewart, D.B.; Gaertner, W.B.; Glasgow, S.C.; Herzig, D.O.; Feingold, D.; Steele, S.R.; Prepared on Behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for Anal Squamous Cell Cancers (Revised 2018). Dis. Colon Rectum 2018, 61, 755–774. [Google Scholar] [CrossRef]
- Chin-Hong, P.V.; Reid, G.E.; AST Infectious Diseases Community of Practice. Human papillomavirus infection in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transplant. 2019, e13590. [Google Scholar] [CrossRef]
- European AIDS Clinical Society (EACS). Guidelines Version 9.1 from October 2018. Available online: http://www.eacsociety.org/files/2018_guidelines-9.1-english.pdf (accessed on 4 October 2019).
- Santos, J.; Valencia, E.; Panel de Expertos de GeSIDA. Consensus statement on the clinical management of non-AIDS defining malignancies. Enferm. Infecc. Microbiol. Clin. 2014, 32, 515–522. [Google Scholar] [CrossRef]
- Esser, S.; Kreuter, A.; Oette, M.; Gingelmaier, A.; Mosthaf, F.; Sautter-Bihl, M.L.; Jongen, J.; Brockmeyer, N.H.; Eldering, G.; Swoboda, J.; et al. German-Austrian guidelines on anal dysplasia and anal cancer in HIV-positive individuals: Prevention, diagnosis, and treatment. J. Dtsch. Dermatol. Ges. 2015, 13, 1302–1319. [Google Scholar] [CrossRef] [PubMed]
- Darragh, T.M.; Winkler, B. Anal cancer and cervical cancer screening: Key differences. Cancer Cytopathol. 2011, 119, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Koliopoulos, G.; Nyaga, V.N.; Santesso, N.; Bryant, A.; Martin-Hirsch, P.P.; Mustafa, R.A.; Schünemann, H.; Paraskevaidis, E.; Arbyn, M. Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database Syst. Rev. 2017, 8, CD008587. [Google Scholar] [CrossRef] [PubMed]
- Dias Gonçalves Lima, F.; Viset, J.D.; Leeflang, M.M.G.; Limpens, J.; Prins, J.M.; de Vries, H.J.C. The Accuracy of Anal Swab-Based Tests to Detect High-Grade Anal Intraepithelial Neoplasia in HIV-Infected Patients: A Systematic Review and Meta-analysis. Open Forum Infect. Dis. 2019, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, A. Cytology in Anal Cancer Screening: Practical Review for Clinicians. Acta Cytol. 2019, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hillman, R.J.; Cuming, T.; Darragh, T.; Nathan, M.; Berry-Lawthorn, M.; Goldstone, S.; Law, C.; Palefsky, J.; Barroso, L.F.; Stier, E.A.; et al. 2016 IANS International Guidelines for Practice Standards in the Detection of Anal Cancer Precursors. J. Low. Genit. Tract Dis. 2016, 20, 283–291. [Google Scholar] [CrossRef]
- Topical or Ablative Treatment in Preventing Anal Cancer in Patients with HIV and Anal High-Grade Squamous Intraepithelial Lesions (ANCHOR). Available online: https://clinicaltrials.gov/ct2/show/NCT02135419 (accessed on 18 November 2019).
- Edgren, G.; Sparen, P. Risk of anogenital cancer after diagnosis of cervical intraepithelial neoplasia: A prospective population-based study. Lancet Oncol. 2007, 8, 311–316. [Google Scholar] [CrossRef]
- Saleem, A.M.; Paulus, J.K.; Shapter, A.P.; Baxter, N.N.; Roberts, P.L.; Ricciardi, R. Risk of anal cancer in a cohort with human papillomavirus-related gynecologic neoplasm. Obstet. Gynecol. 2011, 117, 643–649. [Google Scholar] [CrossRef]
- Evans, H.S.; Newnham, A.; Hodgson, S.V.; Møller, H. Second primary cancers after cervical intraepithelial neoplasia III and invasive cervical cancer in Southeast England. Gynecol. Oncol. 2003, 90, 131–136. [Google Scholar] [CrossRef]
- Jimenez, W.; Paszat, L.; Kupets, R.; Wilton, A.; Tinmouth, J. Presumed previous human papillomavirus (HPV) related gynecological cancer in women diagnosed with anal cancer in the province of Ontario. Gynecol. Oncol. 2009, 114, 395–398. [Google Scholar] [CrossRef]
- Koppe, D.C.; Bandeira, C.B.; Rosa, M.R.; Cambruzzi, E.; Meurer, L.; Fagundes, R.B. Prevalence of anal intraepithelial neoplasia in women with genital neoplasia. Dis. Colon Rectum 2011, 54, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Jacyntho, C.M.; Giraldo, P.C.; Horta, A.A.; Grandelle, R.; Gonçalves, A.K.; Fonseca, T.; Eleutério, J., Jr. Association between genital intraepithelial lesions and anal squamous intraepithelial lesions in HIV-negative women. Am. J. Obstet. Gynecol. 2011, 205, 115 e1–115 e5. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, M.J.; Lau, B.; Justice, A.C.; Engels, E.; Gill, M.J.; Goedert, J.J.; Kirk, G.D.; D’Souza, G.; Bosch, R.J.; Brooks, J.T.; et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin. Infect. Dis. 2012, 54, 1026–1034. [Google Scholar] [CrossRef] [PubMed]
- Schlecht, H.P.; Fugelso, D.K.; Murphy, R.K.; Wagner, K.T.; Doweiko, J.P.; Proper, J.; Dezube, B.J.; Panther, L.A. Frequency of occult high-grade squamous intraepithelial neoplasia and invasive cancer within anal condylomata in men who have sex with men. Clin. Infect. Dis. 2010, 51, 107–110. [Google Scholar] [CrossRef]
- Richel, O.; Hallensleben, N.D.; Kreuter, A.; van Noesel, C.J.; Prins, J.M.; de Vries, H.J. High-resolution anoscopy: Clinical features of anal intraepithelial neoplasia in HIV-positive men. Dis. Colon Rectum 2013, 56, 1237–1242. [Google Scholar] [CrossRef]
- Siegenbeek van Heukelom, M.L.; Richel, O.; de Vries, H.J.; van de Sandt, M.M.; Beck, S.; van den Munckhof, H.A.; Pirog, E.C.; de Koning, M.N.; Prins, J.M.; Quint, K.D. Low- and high-risk human papillomavirus genotype infections in intra-anal warts in HIV-positive men who have sex with men. Br. J. Dermatol. 2016, 175, 735–743. [Google Scholar] [CrossRef]
- Kreuter, A.; Siorokos, C.; Oellig, F.; Silling, S.; Pfister, H.; Wieland, U. High-grade Dysplasia in Anogenital Warts of HIV-Positive Men. JAMA Dermatol. 2016, 152, 1225–1230. [Google Scholar] [CrossRef]
- Blomberg, M.; Friis, S.; Munk, C.; Bautz, A.; Kjaer, S.K. Genital warts and risk of cancer: A Danish study of nearly 50 000 patients with genital warts. J. Infect. Dis. 2012, 205, 1544–1553. [Google Scholar] [CrossRef]
- Prise en Charge Médicale des Personnes Vivant Avec le VIH. Recommandations du groupe d’experts. Available online: https://cns.sante.fr/wp-content/uploads/2017/10/experts-vih_cancers.pdf (accessed on 18 November 2019).
- Binda, G.A.; Gagliardi, G.; Dal Conte, I.; Verra, M.; Cassoni, P.; Cavazzoni, E.; Stocco, E.; Delmonte, S.; De Nardi, P.; Sticchi, L.; et al. Practice parameters for the diagnosis and treatment of anal intraepithelial neoplasia (AIN) on behalf of the Italian Society of Colorectal Surgery (SICCR). Tech. Coloproctol. 2019, 23, 513–528. [Google Scholar] [CrossRef]
- Nederlandse Vereniging van HIV Behandelaren (NVHB)/Dutch Association of HIV-treating physicians. Available online: https://nvhb.nl/richtlijnen/ (accessed on 18 November 2019).
- Bower, M.; Palfreeman, A.; Alfa-Wali, M.; Bunker, C.; Burns, F.; Churchill, D.; Collins, S.; Cwynarski, K.; Edwards, S.; Fields, P.; et al. British HIV Association guidelines for HIV-associated malignancies 2014. HIV Med. 2014, 15, 1–92. [Google Scholar] [CrossRef]
- Nathan, M.; Singh, N.; Garrett, N.; Hickey, N.; Prevost, T.; Sheaff, M. Performance of anal cytology in a clinical setting when measured against histology and high-resolution anoscopy findings. AIDS 2010, 24, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Goldie, S.J.; Kuntz, K.M.; Weinstein, M.C.; Freedberg, K.A.; Welton, M.L.; Palefsky, J.M. The clinical effectiveness and cost-effectiveness of screening for anal squamous intraepithelial lesions in homosexual and bisexual HIV-positive men. JAMA 1999, 281, 1822–1829. [Google Scholar] [CrossRef] [PubMed]
- Karnon, J.; Jones, R.; Czoski-Murray, C.; Smith, K.J. Cost-utility analysis of screening high-risk groups for anal cancer. J. Public Health 2008, 30, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Czoski-Murray, C.; Karnon, J.; Jones, R.; Smith, K.; Kinghorn, G. Cost-effectiveness of screening high-risk HIV-positive men who have sex with men (MSM) and HIV-positive women for anal cancer. Health Technol. Assess. 2010, 14, 1–131. [Google Scholar] [CrossRef]
- Howard, K. The cost-effectiveness of screening for anal cancer in men who have sex with men: A systematic review. Sex Health 2012, 9, 610–619. [Google Scholar] [CrossRef]
- Colón-López, V.; Shiels, M.S.; Machin, M.; Ortiz, A.P.; Strickler, H.; Castle, P.E.; Pfeiffer, R.M.; Engels, E.A. Anal Cancer Risk Among People With HIV Infection in the United States. J Clin. Oncol. 2018, 36, 68–75. [Google Scholar] [CrossRef]
- Wells, J.S.; Holstad, M.M.; Thomas, T.; Bruner, D.W. An integrative review of guidelines for anal cancer screening in HIV-infected persons. AIDS Patient Care STDS 2014, 28, 350–357. [Google Scholar] [CrossRef]
- Daling, J.R.; Weiss, N.S.; Hislop, T.G.; Maden, C.; Coates, R.J.; Sherman, K.J.; Ashley, R.L.; Beagrie, M.; Ryan, J.A.; Corey, L. Sexual practices, sexually transmitted diseases, and the incidence of anal cancer. N. Engl. J. Med. 1987, 317, 973–977. [Google Scholar] [CrossRef]
- Stier, E.A.; Sebring, M.C.; Mendez, A.E.; Ba, F.S.; Trimble, D.D.; Chiao, E.Y. Prevalence of anal human papillomavirus infection and anal HPV-related disorders in women: A systematic review. Am. J. Obstet. Gynecol. 2015, 213, 278–309. [Google Scholar] [CrossRef]
- Gaisa, M.; Ita-Nagy, F.; Sigel, K.; Arens, Y.; Hennessy, M.A.; Rodriguez-Caprio, G.; Mullen, M.; Aberg, J.A.; Cespedes, M. High rates of anal high-grade squamous intraepithelial lesions in HIV-infected women who do not meet screening guidelines. Clin. Infect. Dis. 2017, 64, 289–294. [Google Scholar] [CrossRef]
| Society/Institute/Group | Year | Country | Target Population | Recommendation | Management after Cytology | Age | Grade | HPV Testing |
|---|---|---|---|---|---|---|---|---|
| New York State Department of Health AIDS Institute [17] | 2007 | USA | HIV-positive patients | Anal cytology at baseline in HIV-infected populations: - MSM - History of anogenital condylomas - Women with abnormal cervical and/or vulvar histology | - Normal cytology to be repeated annually. - Refer patients with abnormal results ≥ ASC-US for HRA. | Any age. | ND | ND |
| Northwest Pennsylvania Rural AIDS Alliance [18] | 2011 | USA | HIV-positive patients | Anal cytology at baseline in all HIV-positive. | - Normal cytology to be repeated annually, especially for HIV-positive MSM. - Patients with a low CD4+ T-cell count (<500 cells/mm3) should be monitored 6–9 months (author suggestion). - Refer patients with abnormal results ≥ ASC-US for HRA. | ND | ND | High and low-risk HPV. Not included in the algorithm management. |
| HIV Medicine Association of the Infectious Diseases Society of America [19] | 2014 | USA | HIV-positive patients | Anal cytology in HIV-positive patients: - MSM - Women with receptive anal sex - Women with abnormal cervical cytology - History of genital warts | ND | ND | Weak. Moderate quality evidence. | ND |
| The American Society of Colon and Rectal Surgeons [20] | 2018 | USA | High-risk populations: - HIV-positive - MSM - History of cervical dysplasia | Anal cytology may be considered in high-risk populations. Not for universal screening. | ND | ND | Weak. Moderate quality evidence, 2B. | HPV testing may be used as an adjunct to screening. |
| American Society of Transplantation Infectious Diseases Community of Practice [21] | 2019 | USA | Solid-organ transplanted patients | Anal cytology for solid-organ transplant patients: - History of receptive anal intercourse - History of cervical dysplasia | - Normal cytology to be repeated every 1–3 years. - Refer patients with abnormal results ≥ ASC-US for HRA. | ND | Weak. Low quality evidence. | ND |
| European AIDS Clinical Society [22] | 2018 | - | HIV-positive patients | Digital rectal exam ± anal cytology in HIV-positive patients: - MSM - Persons with anogenital HPV-associated dysplasia | - Normal cytology to be repeated in 1–3 years. - Patients with abnormal results should be referred for anoscopy. | ND | ND | ND |
| Spanish AIDS Study Group/Grupo de Estudio de SIDA (GeSIDA) [23] | 2014 | Spain | HIV-positive patients | Anal cytology in HIV-positive patients: - MSM - Women with cervical cancer or HSIL - History of anogenital condylomas | - Normal cytology to be repeated annually. - Refer patients with abnormal results ≥ ASC-US for HRA. | ND | ND | HPV PCR increases sensitivity. Not included in the algorithm management. |
| Several German Societies. Lead Management: Deutsche AIDS-Gesellschaft (DAIG)/German AIDS Society [24] | 2015 | Germany Austria | HIV-positive patients | Anal cytology in all HIV-positive patients | - Normal cytology to be repeated annually. -Refer patients with cytology HSIL for anoscopy (within 3 months). - Other cytology results to repeat cytology in 3–6 months. If the second is abnormal, to refer for anoscopy. | ND | ND | If necessary HPV typing. In case of high-risk HPV > 1 year, these are high-risk patients and should be submitted to anoscopy. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albuquerque, A.; Rios, E.; Schmitt, F. Recommendations Favoring Anal Cytology as a Method for Anal Cancer Screening: A Systematic Review. Cancers 2019, 11, 1942. https://doi.org/10.3390/cancers11121942
Albuquerque A, Rios E, Schmitt F. Recommendations Favoring Anal Cytology as a Method for Anal Cancer Screening: A Systematic Review. Cancers. 2019; 11(12):1942. https://doi.org/10.3390/cancers11121942
Chicago/Turabian StyleAlbuquerque, Andreia, Elisabete Rios, and Fernando Schmitt. 2019. "Recommendations Favoring Anal Cytology as a Method for Anal Cancer Screening: A Systematic Review" Cancers 11, no. 12: 1942. https://doi.org/10.3390/cancers11121942
APA StyleAlbuquerque, A., Rios, E., & Schmitt, F. (2019). Recommendations Favoring Anal Cytology as a Method for Anal Cancer Screening: A Systematic Review. Cancers, 11(12), 1942. https://doi.org/10.3390/cancers11121942






