Effects of Uremic Clearance Granules in Uremic Pruritus: A Meta-Analysis
Abstract
:1. Introduction
2. Results
2.1. Study Characteristics
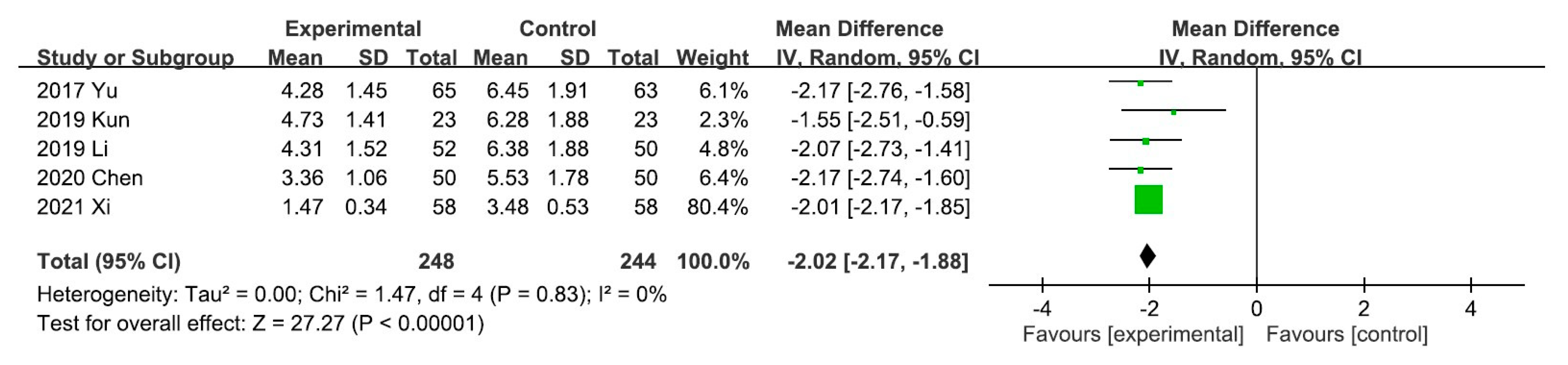
2.2. Primary Outcomes
2.3. Secondary Outcomes
2.3.1. Effect of UCG on Serum Levels of Ca, P, PTH, and iPTH
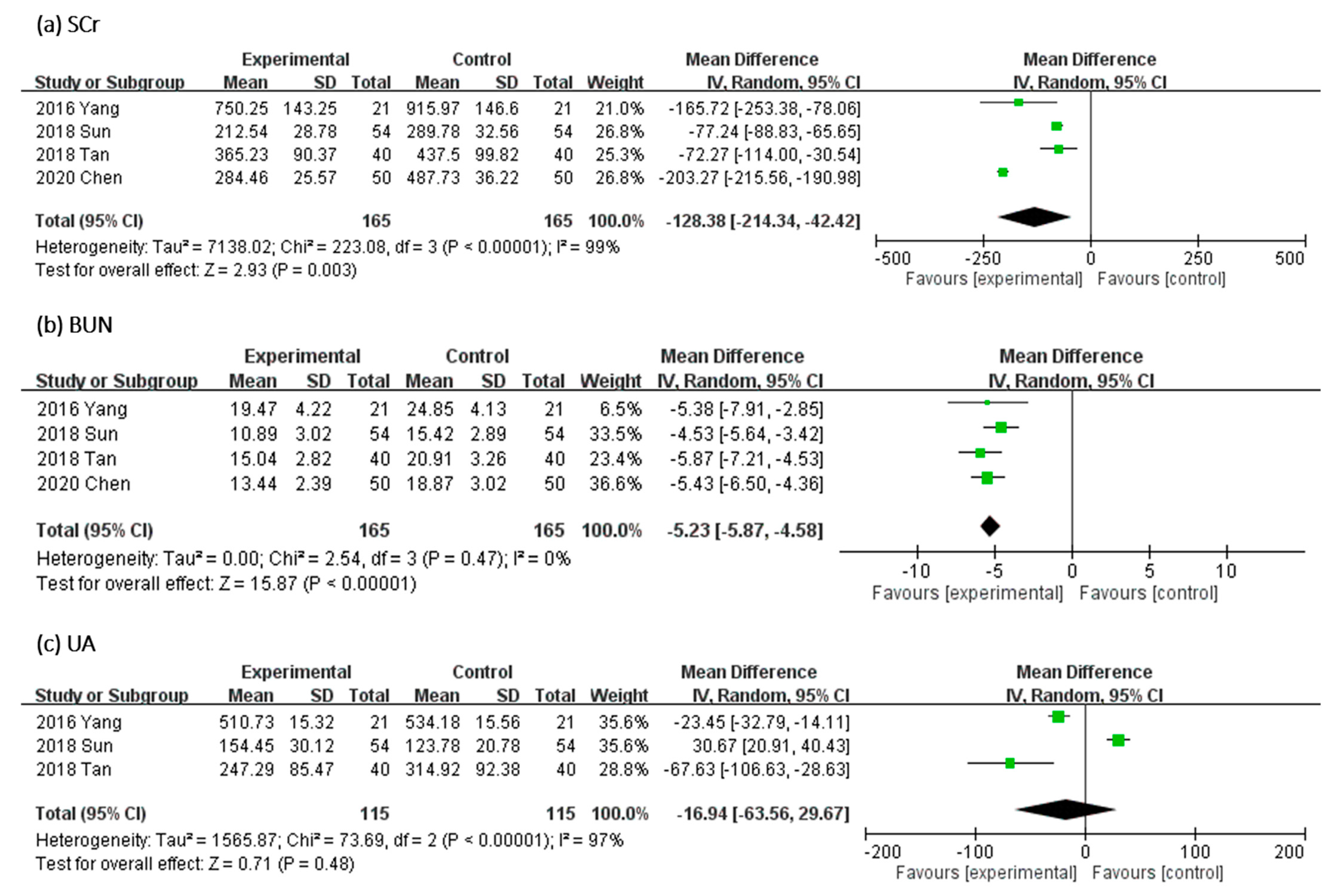
2.3.2. Effect of UCG on SCr, BUN, and Uric Acid Levels
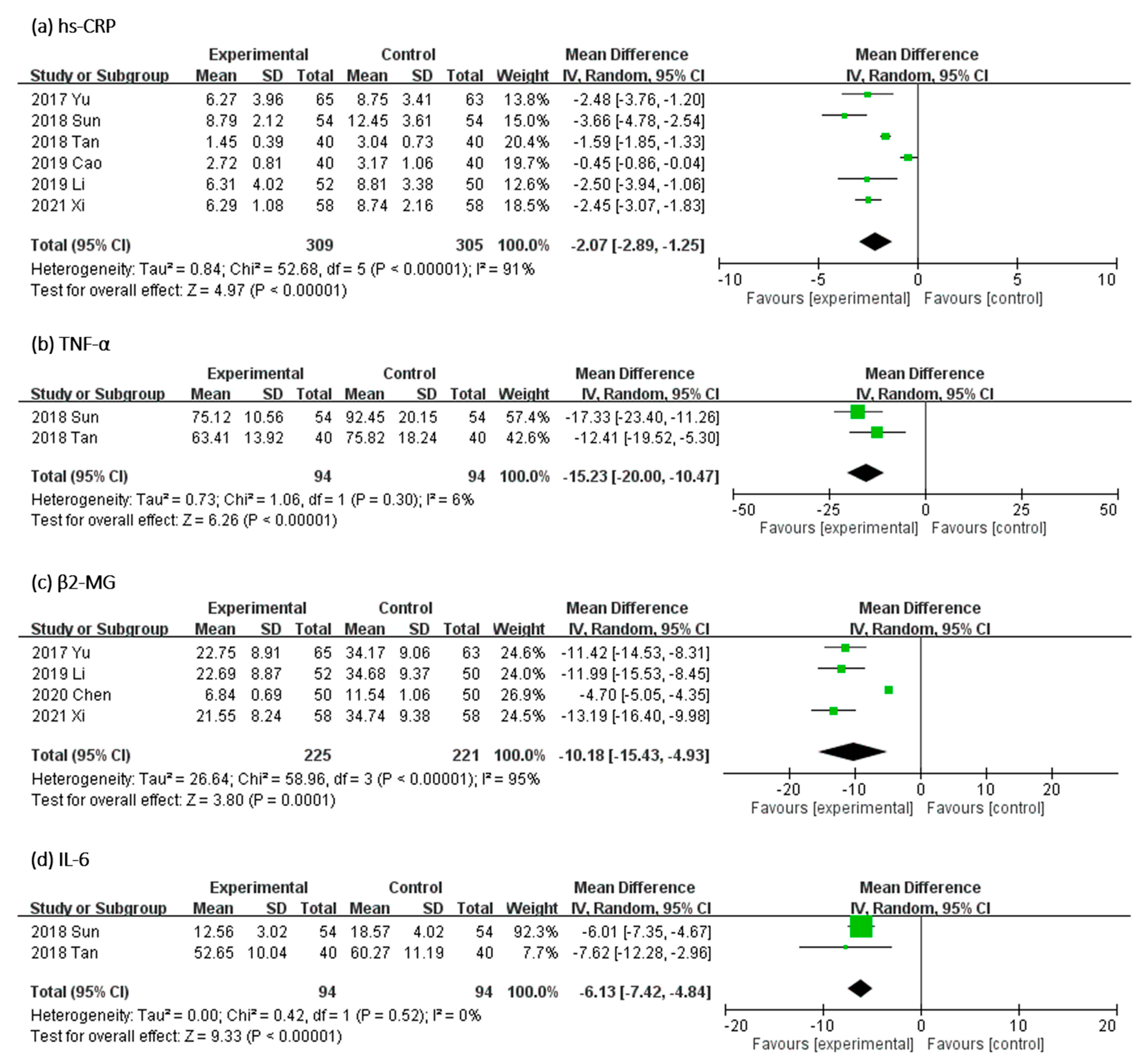
2.3.3. Effect of UCG on Serum Levels of Inflammatory Biomarkers
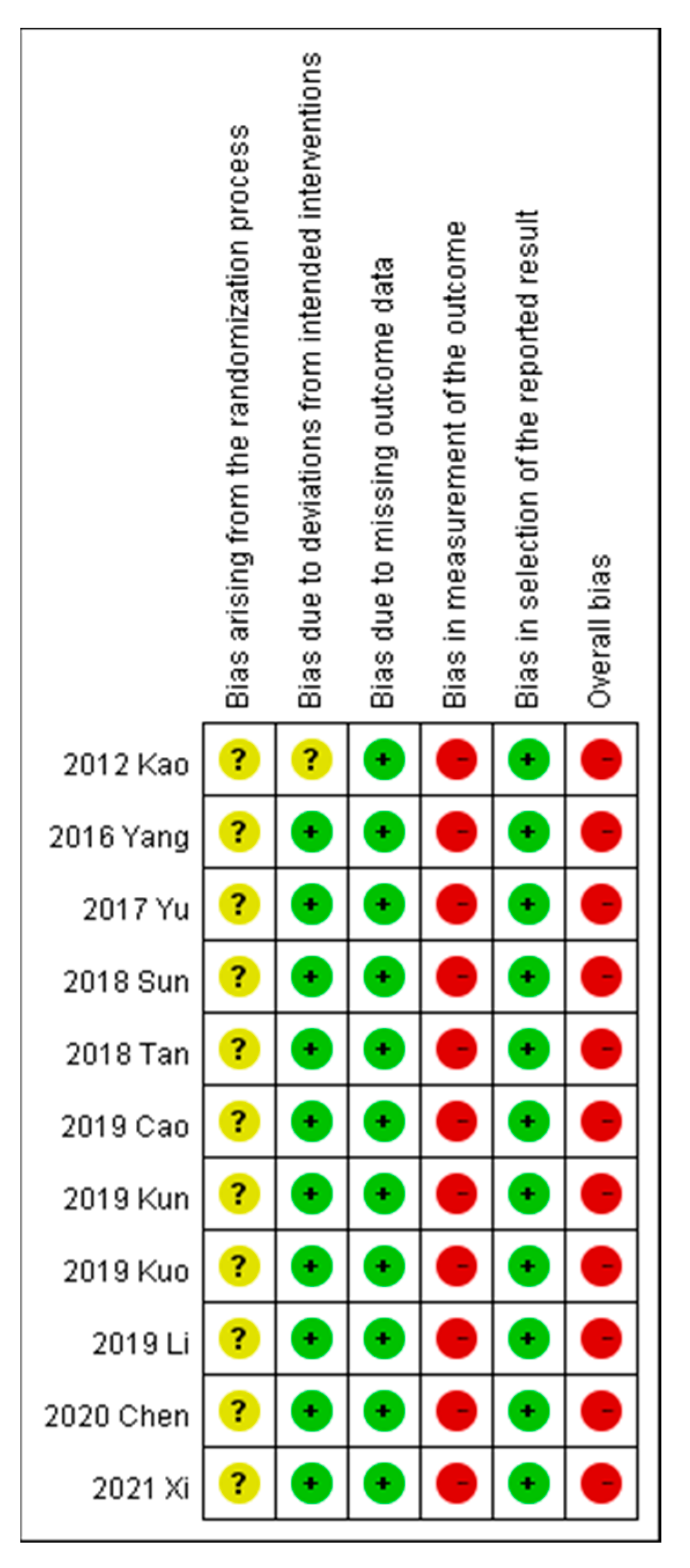
2.4. Quality of Evidence
3. Discussion
4. Conclusions
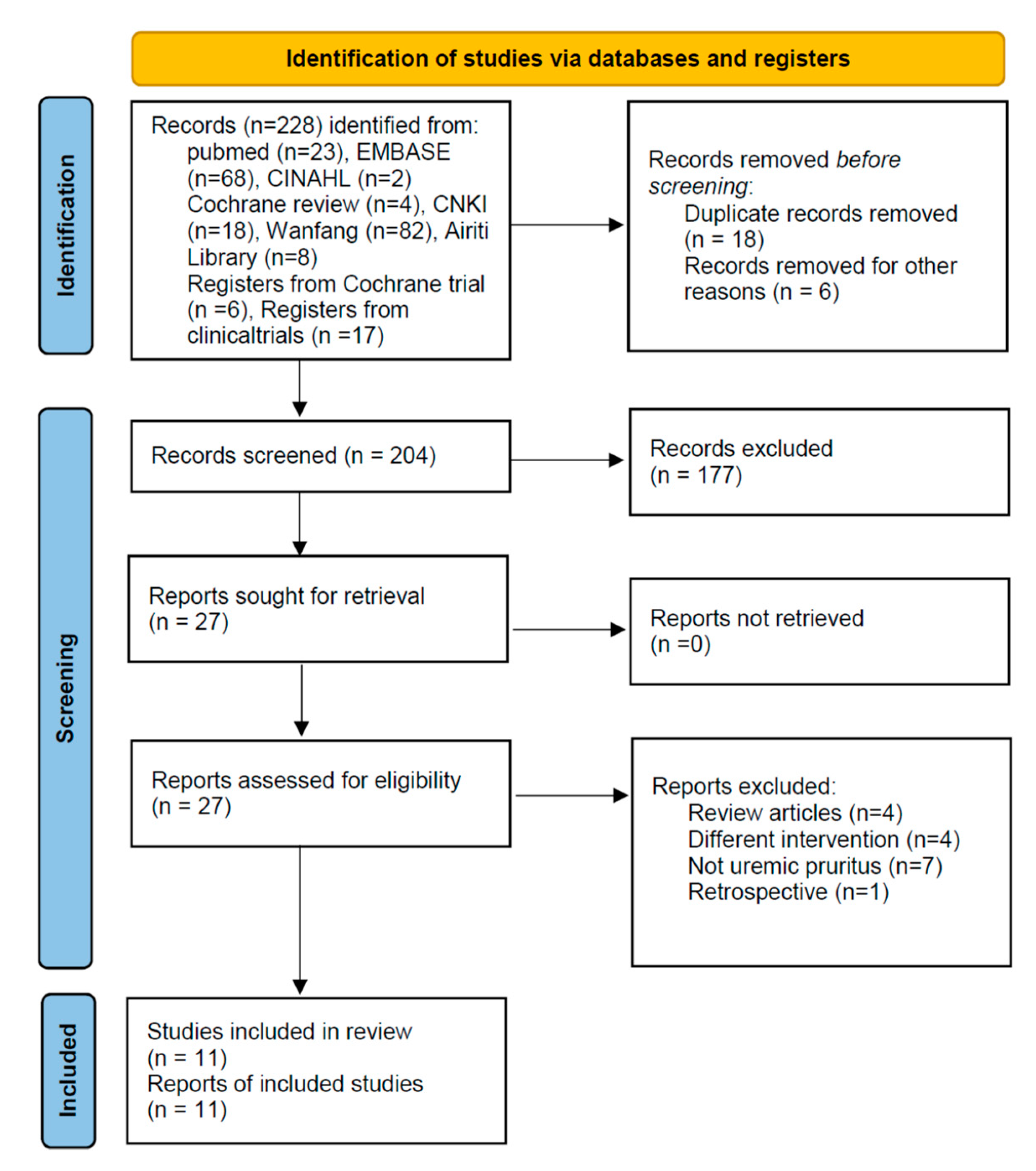
5. Materials and Methods
5.1. Literature Search
5.2. Study Selection
5.3. Data Extraction and Quality Assessment
5.4. Data Synthesis and Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, H.Y.; Peng, Y.S.; Chen, H.Y.; Tsai, W.C.; Yang, J.Y.; Hsu, S.P.; Pai, M.F.; Lu, H.M.; Chiang, J.F.; Ko, M.J.; et al. A Comparison of Uremic Pruritus in Patients Receiving Peritoneal Dialysis and Hemodialysis. Medicine 2016, 95, e2935. [Google Scholar] [CrossRef] [PubMed]
- Mathur, V.S.; Lindberg, J.; Germain, M.; Block, G.; Tumlin, J.; Smith, M.; Grewal, M.; McGuire, D.; Investigators, I.N.R. A longitudinal study of uremic pruritus in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2010, 5, 1410–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narita, I.; Alchi, B.; Omori, K.; Sato, F.; Ajiro, J.; Saga, D.; Kondo, D.; Skatsume, M.; Maruyama, S.; Kazama, J.J.; et al. Etiology and prognostic significance of severe uremic pruritus in chronic hemodialysis patients. Kidney Int. 2006, 69, 1626–1632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verduzco, H.A.; Shirazian, S. CKD-Associated Pruritus: New Insights into Diagnosis, Pathogenesis, and Management. Kidney Int. Rep. 2020, 5, 1387–1402. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.-H.; Tai, Y.-C.; Yu, M.-C.; Lin, I.-H.; Kuo, K.-L. Western and complementary alternative medicine treatment of uremic pruritus: A literature review. Tzu Chi Med. J. 2021, 33, 350–358. [Google Scholar] [CrossRef]
- Ramakrishnan, K.; Bond, T.C.; Claxton, A.; Sood, V.C.; Kootsikas, M.; Agnese, W.; Sibbel, S. Clinical characteristics and outcomes of end-stage renal disease patients with self-reported pruritus symptoms. Int. J. Nephrol. Renov. Dis. 2013, 7, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.-Y.; Chiu, Y.-L.; Hsu, S.-P.; Pai, M.-F.; Lai, C.-F.; Yang, J.-Y.; Peng, Y.-S.; Tsai, T.-J.; Wu, K.-D. Elevated C-reactive protein level in hemodialysis patients with moderate/severe uremic pruritus: A potential mediator of high overall mortality. QJM Int. J. Med. 2010, 103, 837–846. [Google Scholar] [CrossRef] [Green Version]
- Fallahzadeh, M.K.; Roozbeh, J.; Geramizadeh, B.; Namazi, M.R. Interleukin-2 serum levels are elevated in patients with uremic pruritus: A novel finding with practical implications. Nephrol. Dial. Transplant. 2011, 26, 3338–3344. [Google Scholar] [CrossRef] [Green Version]
- Kimmel, M.; Alscher, D.M.; Dunst, R.; Braun, N.; Machleidt, C.; Kiefer, T.; Stülten, C.; van der Kuip, H.; Pauli-Magnus, C.; Raub, U. The role of micro-inflammation in the pathogenesis of uraemic pruritus in haemodialysis patients. Nephrol. Dial. Transplant. 2006, 21, 749–755. [Google Scholar] [CrossRef] [Green Version]
- Jaiswal, D.; Uzans, D.; Hayden, J.; Kiberd, B.A.; Tennankore, K.K. Targeting the Opioid Pathway for Uremic Pruritus: A Systematic Review and Meta-analysis. Can. J. Kidney Health Dis. 2016, 3, 2054358116675345. [Google Scholar] [CrossRef] [Green Version]
- Eusebio-Alpapara, K.M.V.; Castillo, R.L.; Dofitas, B.L. Gabapentin for uremic pruritus: A systematic review of randomized controlled trials. Int. J. Dermatol. 2019, 59, 412–422. [Google Scholar] [CrossRef] [PubMed]
- Badiee Aval, S.; Ravanshad, Y.; Azarfar, A.; Mehrad-Majd, H.; Torabi, S.; Ravanshad, S. A Systematic Review and Meta-analysis of Using Acupuncture and Acupressure for Uremic Pruritus. Iran. J. Kidney Dis. 2018, 12, 78–83. [Google Scholar] [PubMed]
- Xue, W.; Zhao, Y.; Yuan, M.; Zhao, Z. Chinese herbal bath therapy for the treatment of uremic pruritus: Meta-analysis of randomized controlled trials. BMC Complement. Altern. Med. 2019, 19, 103. [Google Scholar] [CrossRef] [PubMed]
- Pakfetrat, M.; Basiri, F.; Malekmakan, L.; Roozbeh, J. Effects of turmeric on uremic pruritus in end stage renal disease patients: A double-blind randomized clinical trial. J. Nephrol. 2014, 27, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Cai, G.-Y.; He, L.-Q.; Lin, H.-L.; Cheng, X.-H.; Wang, N.-S.; Jian, G.-H.; Liu, X.-S.; Liu, Y.-N.; Ni, Z.-H. Efficacy and safety of Niaoduqing particles for delaying moderate-to-severe renal dysfunction: A randomized, double-blind, placebo-controlled, multicenter clinical study. Chin. Med. J. 2017, 130, 2402. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yu, S.; Jia, Q.; Chen, L.; Zhong, J.; Pan, Y.; Shen, P.; Shen, Y.; Wang, S.; Wei, Z. NiaoDuQing granules relieve chronic kidney disease symptoms by decreasing renal fibrosis and anemia. Oncotarget 2017, 8, 55920–55937. [Google Scholar] [CrossRef] [Green Version]
- Sun, Y.; Yin, Q.; Hui, Y.D. Analysis of TCM Treatment of Hemodialysis Complications of Uremia. J. Basic Chin. Med. 2017, 23, 1269–1271. [Google Scholar]
- Wang, Z.X. Observation on the clinical therapeutic effect of modified Guomin decoction to treat uremic pruritus. World Latest Med. Inf. 2017, 17, 69–70. [Google Scholar]
- Zhang, J.; Li, J.; Zhang, H.-L.; Qu, H.-S.; Zhang, X.-Z.; Cheng, Y.-Q.; Zhang, Z.-M.; Huang, J.-Q. Meta-analysis of niaoduqing granules combined with raas system blocker in the treatment of diabetic nephropathy. World J. Tradit. Chin. Med. 2019, 5, 193. [Google Scholar]
- Huang, L.; Xie, D.; Yu, Y.; Liu, H.; Shi, Y.; Shi, T.; Wen, C. TCMID 2.0: A comprehensive resource for TCM. Nucleic Acids Res. 2017, 46, D1117–D1120. [Google Scholar] [CrossRef]
- Feng, Q.; Wan, Y.; Jiang, C.; Wang, C.; Wei, Q.; Zhao, Q. The mechanism and effect of TCM in delaying the progression of chronic renal failure. Chin. J. Tradit Chin. Med. 2011, 36, 1122–1128. [Google Scholar]
- Ye, M.-Y.; Zheng, J.; Zhang, J. The Influence of Niaoduqing Particle on the Calcium and Phosphorus Metabolism and FGF23 in Patients with Chronic Kidney Disease. Med. Innov. China 2015, 23, 16–18. [Google Scholar]
- Yin, X.-F.; Han, L.-L. Effect of uremic clearance granule on the systemic micro-inflammatory state of patients after peritoneal dialysis. Pract. Pharm. Clin. Remedies 2013, 2, 125–126. [Google Scholar]
- Chen, X.; Li, L.J.; Wu, D. A clinical study on uremic clearance granule combined with high-flux hemodialysis in treating uremia pruritus. China Pharm. 2020, 4, 63–65. [Google Scholar]
- Mettang, T.; Pauli-Magnus, C. The pathophysiological puzzle of uremic pruritus - Insights and speculations from therapeutic and epidemiological studies. Perit. Dial. Int. 2000, 20, 493–494. [Google Scholar] [CrossRef] [PubMed]
- Saito, A. Challenge for developing more complete renal replacement technologies in Japan. Blood Purif. 2013, 34, 255. [Google Scholar] [CrossRef]
- Chen, L.M.; Zhao, Y.D.; Wang, T.T.; Huang, B.B.; Liu, X.Q. Research progress of Niaoduqing granules in treating chronic kidney disease. J. MuDanJiang Med. Univ. 2019, 40, 127–129. [Google Scholar]
- Tang, N.; Zhang, X.H. Study on improving effect of Niaoduqing on PTH and micro-inflammatory state in MHD Patients. J. Chin. Med. Mater. 2017, 40, 718–720. [Google Scholar]
- Chu, X.Y. Clinical observation of Niaoduqing granule combined with calcitriol in the treatment of pruritus in dialysis patients. Master’s Thesis, Zhejiang Chinese Medical University, Hangzhou, China, 1 June 2013. [Google Scholar]
- Chu, X.Y.; Jiang, A.L.; Zhang, J.P.; Sun, Y. Clinical observation of Niaoduqing granule combined with calcitriol in the treatment of pruritus in dialysis patients. Chin. J. Integr. Tradit. West. Nephrol. 2012, 9, 825–826. [Google Scholar]
- Dai, W.X.; Li, W.C. Observation on the treatment of hyperphosphatemia complicated with skin itching in hemodialysis patients. Healthmust-Readmagazine 2018, 3, 113. [Google Scholar]
- Guo, K.P.; Yu, K.; Fu, Y.; Wang, J. Clinical observation and nursing experience of treating uremic pruritus by traditional Chinese medicine soaking and washing combined oral treatment. Cardiovasc. Dis. J. Integr. Tradit. Chin. West. Med. 2018, 6, 150–151. [Google Scholar]
- Ji, X. To study the effect of Niaoduqing granule combined with hemodialysis in uremic patients to improve nutrition and protect renal function. Electron. J. Clin. Med. Lit. 2019, 6, 32–33. [Google Scholar]
- Men, W.J.; Ding, Z.M. Effect of Niaoduqing particles on calcium-phosphorus metabolism and parathyroid hormone in patients of end-stage renal failure with maintenance hemodialysis. China Med. 2015, 10, 1818–1821. [Google Scholar]
- Pao, C.M.; Zhao, S.P.; Yuan, J.; Tian, H. Effects of Niaoduqing granules on end-stage renal failure on maintenance hemodialysis patients with calcium phosphorus metabolism and parathyroid hormone levels. China Health Stand. Manag. 2016, 7, 130–131. [Google Scholar]
- Tang, J.; Wang, L.; Lu, Q.Z.; Zeng, Y.Y.; Sun, Q.L. Nursing care of colon dialysis combined with Niaoduqing granules in the treatment of early and mid-term chronic renal failure. Guizhou Med. J. 2012, 36, 856–857. [Google Scholar]
- Xia, Y.; Zhou, J.J. Observation of Chinese medicine enema on PTH clears in blood for patients of chronic kidney disease. Hebei Tradit. Chin. Med. 2014, 36, 1466–1468. [Google Scholar]
- Xu, L.F. Analysis of curative effect of Niaoduqing granules in treating chronic renal failure. Qinghai Med. J. 2018, 10, 13–14. [Google Scholar]
- Wang, C.P.; Lu, Y.C.; Tsai, I.T.; Tang, W.H.; Hsu, C.C.; Hung, W.C.; Yu, T.H.; Chen, S.C.; Chung, F.M.; Lee, Y.J.; et al. Increased Levels of Total p -Cresylsulfate Are Associated with Pruritus in Patients with Chronic Kidney Disease. Dermatology 2016, 232, 363–370. [Google Scholar] [CrossRef]
- Cao, Y.G. Clinical Observation of Niaoduqing Granule Combined with High Flux Hemodialysis in Treating Uremic Pruritus. Chin. Med. Mod. Distance Educ. China 2019, 2, 117–118. [Google Scholar]
- Kuo, X.W.; Li, X.; Guo, W.J. Study on the Efficacy of Niaoduqing Granules in Treating Pruritus and Removing Blood Toxin in Hemodialysis Patients. Clin. Med. Eng. 2019, 4, 485–486. [Google Scholar]
- Kun, D.Z.; Yu, S.J.; Li, M. The feasibility of Niaoduqing granule in adjuvant treatment of uremic pruritus. World Latest Med. Inf. 2019, 19, 182–183. [Google Scholar]
- Li, X.; Kuo, X.W. The feasibility of Niaoduqing granule in adjuvant treatment of uremic pruritus. Jilin Med. J. 2019, 1, 91. [Google Scholar]
- Sun, J.K.; Chen, J. Hemodialysis for uremic patients with Niaoduqing inflammation and itch of skin effect. Mod. Med. Health Res. 2018, 7, 1–4. [Google Scholar]
- Tan, H.J. Clinical observation of Niaoduqing granule assisted low-frequency hemoperfusion combined with hemodialysis in the treatment of pruritus in patients with uremia. Chin. J. Integr. Tradit. West. Nephrol. 2018, 12, 1099–1101. [Google Scholar]
- Xi, M.M. Clinical Observation of Niaoduqing Granules Combined with High-flux Hemodialysis in Treating Uremic Skin Pruritus. Guide China Med. 2021, 19, 112–113. [Google Scholar]
- Yang, Y.L. The influence of Niaoduqing particle on uremic pruritus in maintenance hemodialysis patients. Master’s Thesis, Hubei University of Chinese Medicine, Wuhan, China, 27 May 2016. [Google Scholar]
- Yu, D.; Li, L.Z.; Zhang, S.Y. Clinical effect of niaoduqing particle combined with high-flux hemodialysis in the treatment of patients with uremic pruritus. Pract. J. Clin. Med. 2017, 6, 204–206. [Google Scholar]
- Kao, C.M.; Li, J.H. The observation on the efficacy of Niaoduqing retention enema combined with low-frequency hemoperfusion and hemodialysis on uremia pruritus. China Health Care Nutr. 2012, 22, 1846–1847. [Google Scholar] [CrossRef]
- Cupisti, A.; Piccoli, G.B.; Gallieni, M. Charcoal for the management of pruritus and uremic toxins in patients with chronic kidney disease. Curr. Opin. Nephrol. Hypertens 2020, 29, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Lu, P.-H.; Yu, M.-C.; Wei, M.-J.; Kuo, K.-L. The Therapeutic Strategies for Uremic Toxins Control in Chronic Kidney Disease. Toxins 2021, 13, 573. [Google Scholar] [CrossRef] [PubMed]
- Pisoni, R.L.; Wikström, B.; Elder, S.J.; Akizawa, T.; Asano, Y.; Keen, M.L.; Saran, R.; Mendelssohn, D.C.; Young, E.W.; Port, F.K. Pruritus in haemodialysis patients: International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transplant. 2006, 21, 3495–3505. [Google Scholar] [CrossRef] [Green Version]
- Kimata, N.; Fuller, D.S.; Saito, A.; Akizawa, T.; Fukuhara, S.; Pisoni, R.L.; Robinson, B.M.; Akiba, T. Pruritus in hemodialysis patients: Results from the Japanese Dialysis Outcomes and Practice Patterns Study (JDOPPS). Hemodial. Int. 2014, 18, 657–667. [Google Scholar] [CrossRef] [PubMed]
- Rayner, H.C.; Larkina, M.; Wang, M.; Graham-Brown, M.; van der Veer, S.N.; Ecder, T.; Hasegawa, T.; Kleophas, W.; Bieber, B.A.; Tentori, F.; et al. International Comparisons of Prevalence, Awareness, and Treatment of Pruritus in People on Hemodialysis. Clin. J. Am. Soc. Nephrol. 2017, 12, 2000–2007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozen, N.; Cinar, F.I.; Askin, D.; Mut, D. Uremic pruritus and associated factors in hemodialysis patients: A multi-center study. Kidney Res. Clin. Pract. 2018, 37, 138–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vanholder, R.; Pletinck, A.; Schepers, E.; Glorieux, G. Biochemical and Clinical Impact of Organic Uremic Retention Solutes: A Comprehensive Update. Toxins 2018, 10, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andoh, T.; Maki, T.; Li, S.; Uta, D. β2-Microglobulin elicits itch-related responses in mice through the direct activation of primary afferent neurons expressing transient receptor potential vanilloid 1. Eur. J. Pharmacol. 2017, 810, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Kaysen, G.A. The microinflammatory state in uremia: Causes and potential consequences. J. Am. Soc. Nephrol. 2001, 12, 1549–1557. [Google Scholar] [CrossRef]
- Tseng, C.Y.; Wu, T.T.; Lai, C.W.; Lin, H.J.; Chou, C.Y.; Chang, C.T.; Chen, H.C. Vegetarian diet may ameliorate uremic pruritus in hemodialysis patients. Ren. Fail. 2018, 40, 514–519. [Google Scholar] [CrossRef]
- Dezfouli, M.; Moeinzadeh, F.; Taheri, S.; Feizi, A. The Effect of Omega-3 Supplementation on Serum Levels of Inflammatory Biomarkers and Albumin in Hemodialysis Patients: A Systematic Review and Meta-analysis. J. Ren. Nutr. 2020, 30, 182–188. [Google Scholar] [CrossRef]
- Shayanpour, S.; Beladi Mousavi, S.S.; Lakhaye Rizi, P.; Cheraghian, B. The effect of the omega-3 supplement on uremic pruritus in hemodialysis patients; a double-blind randomized controlled clinical trial. J. Nephropathol. 2017, 8, 13. [Google Scholar] [CrossRef]
- Yin, J.Z.; Zhu, B.; Chen, H.Y.; Li, P.; Lu, J.C.; Yan, M.H.; Li, P. Meta-analysis of Niaoduqing granules in the treatment of chronic kidney disease stages 3~5. Chin. J. Integr. Tradit. West. Nephrol. 2020, 21, 136–142. [Google Scholar]
- Liu, M.; Zhu, J. Effects of hemodialysis combined with uremic clearance granule on serum protein-bound uremic toxins in patients with end-stage renal disease. Chin. J. Prim. Med. Pharm. 2020, 2613–2617. [Google Scholar] [CrossRef]
- Ji, C.; Deng, Y.; Yang, A.; Lu, Z.; Chen, Y.; Liu, X.; Han, L.; Zou, C. Rhubarb Enema Improved Colon Mucosal Barrier Injury in 5/6 Nephrectomy Rats May Associate With Gut Microbiota Modification. Front. Pharmacol. 2020, 11, 1092. [Google Scholar] [CrossRef]
- Cui, H.-X.; Zhang, L.-S.; Luo, Y.; Yuan, K.; Huang, Z.-Y.; Guo, Y. A Purified Anthraquinone-Glycoside Preparation From Rhubarb Ameliorates Type 2 Diabetes Mellitus by Modulating the Gut Microbiota and Reducing Inflammation. Front. Microbiol. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.R.; Wei, Q.X.; Wan, Y.G.; Sun, W.; Mao, Z.M.; Chen, H.L.; Meng, X.J.; Shi, X.M.; Tu, Y.; Zhu, Q. Ureic clearance granule, alleviates renal dysfunction and tubulointerstitial fibrosis by promoting extracellular matrix degradation in renal failure rats, compared with enalapril. J. Ethnopharmacol. 2014, 155, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xu, C.W.; Li, H. Observation of curative effect of Niaoduqing enema in treating uremic pruritus. Tianjin Med. J. 2011, 39, 272–274. [Google Scholar]
- Reich, A.; Bożek, A.; Janiszewska, K.; Szepietowski, J.C. 12-Item Pruritus Severity Scale: Development and Validation of New Itch Severity Questionnaire. BioMed Res. Int. 2017, 2017, 3896423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altinok Ersoy, N.; Akyar, I. Multidimensional pruritus assessment in hemodialysis patients. BMC Nephrol. 2019, 20, 42. [Google Scholar] [CrossRef] [Green Version]
- Esmaeili, A.; Abbasi, M.R.; Namazi, S. Validity and reliability of a Persian version of the 12-Item Pruritus Severity Scale in hemodialysis patients with uremic pruritus. Iran. J. Dermatol. 2021, 24, 73–79. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Cochrane: Chichester, UK; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- GRADEpro, GDT. Gradepro guideline development tool [software]. McMaster University 2015. p. 435. Available online: https://gradepro.org/ (accessed on 19 July 2021).


| Chinese Name | English/Latin Name | Family | Species | Prescription Functions (TCM Patterns) |
|---|---|---|---|---|
| Dahuang | Rheum palmatum/Rheum officinale | Polygonaceae | R. officinale | To drain heat, cool blood, resolve toxins, and expel stasis |
| Gancao | Glycyrrhiza inflata/Glycyrrhiza uralensis | Fabaceae | G. uralensis | To supplement center and boost qi, drain fire, and resolve toxins |
| Chaihu | Bupleurum scorzonerifolium/Bupleurum chinense | Apiaceae | - | To harmonize exterior and interior |
| Huangqi | Astragalus mongholicus/Astragalus membranaceus | Fabaceae | - | To boost qi and secure exterior, and draw toxins |
| Sangbaipi | White Mulberry Root/Morus alba | Moraceae | M. alba | To disinhibit water and disperse edema |
| Dangshen | Codonopsis tangshen/Codonopsis pilosula | Campanulaceae | C. pilosula | To fortify the spleen and supplement lung, boost qi, and engender liquid |
| Baishao | Common Peony/Paeonia lactiflora | Paeoniaceae | P. lactiflora | To calm the liver and relieve pain, nourish the blood and constrain yin |
| Chuanxiong | Cnidium officinale/Ligusticum chuanxiong | Apiaceae | L. chuanxiong | To move qi, quicken the blood, and dispel wind |
| Kushen | Light yellow Sophora/Sophora flavescens | Fabaceae | S. flavescens | To clear heat and dry damp, dispel wind, and kill worms |
| Juhua | Florists Chrysanthemum Flower/Chrysanthemum morifolium | Asteraceae | C. morifolium | To dispel wind, clear heat, and resolve toxins |
| Banxia | Ternate Pinellia/Pinellia ternata | Araceae | P. ternata | To eliminate damp, resolve cold phlegm, and dissipate binds |
| Baizhu | Large head Atractylodes/Atractylodes macrocephala | Asteraceae | A. macrocephala | To boost qi, fortify the spleen, dry damp, and disinhibit water |
| Fuling | Indian Bread/Poria cocos | Fomitopsidaceae | W. cocos | To disinhibit water, percolate dampness, fortify the spleen, and quiet the heart |
| Heshouwu | Tuber Fleeceflower/Polygonum multiflorum | Polygonaceae | F. multiflora | To enrich yin, nourish the blood, moisten intestines to free stool, dispel wind, and resolve toxins |
| Danshen | Salvia przewalskii/Salviae Miltiorrhizae | Lamiaceae | S. miltiorrhiza | To quicken the blood, dispel stasis, nourish the blood, quiet the spirit, cool the blood, and disperse welling abscess |
| Cheqiancao | All-grass of Rippleseed plantain/Herba Plantaginis | Plantaginaceae | P. asiatica | Treatment of edema with oliguria, urinary infection with difficult painful urination |
| Study (Year) | Study Design | Inclusion Criteria | No. of Patients | Age (Years) | Route, Dosage, and Frequency | Duration | Inspection Data | Pruritus Severity Assessment | Pruritus Score (Before → After), |
|---|---|---|---|---|---|---|---|---|---|
| Kao et al. 2012 [49] | RCT | HD + HP | U: 16 C: 16 | 25–74 25–74 | Enema, 15 g, 2 times/d | 18 M | overall effectiveness | Duo PS | U: 29.18(1.52) → 12.69(3.16) C: 26.54(4.03) → 17.13(3.24) |
| Yang et al. 2016 [47] | RCT | U: HD + HP (14); HD (7) C: HD + HP (11); HD (10) | U: 21 C: 21 | U: 51.48(13.49) C: 51.67(11.68) | Oral, 2.5 g, 2 times/d | 1 M | Ca, P, PTH, Scr, BUN, UA, FGF23, CRP, overall effectiveness | Kuypers PS | U: 11.57(2.45) →6.43 (3.02) C: 11.67(4.98) → 11.86(4.33) |
| Yu et al. 2017 [48] | RCT | HD | U: 65 C: 63 | U: 35–68 C: 36–70 | Oral, 5 g, 4 times/d | 3 M | Ca, P, PTH, β2-MG, hs-CRP, overall effectiveness | VAS | U: 8.17(1.94) → 4.28(1.45) C: 8.21(1.78) → 6.45(1.91) |
| Sun et al. 2018 [44] | RCT | HD | U: 54 C: 54 | U: 54.12(5.78) C: 54.08(6.23) | Oral, 2.5 g, 2 times/d | -- | Scr, BUN, UA, hs-CRP, IL-6, TNF-α, Alb, Hb | PS1 | U: 11.56(3.02) → 5.12(0.89) C: 11.89(3.12) → 8.28(2.02) |
| Tan et al. 2018 [45] | RCT | HD + HP | U: 40 C: 40 | U: 48.83(8.95) C: 48.92(3.87) | Oral, 5 g, 4 times/d | 3 M | Ca, P, PTH, Scr, BUN, UA, IL-6, TNF-α,hs-CRP, overall effectiveness | PS2 | U: 8.37(0.89) → 4.6(0.38) C: 8.14(0.96) → 6.44(0.55) |
| Cao et al. 2019 [40] | RCT | HD | U: 40 C: 40 | U: 59.7 C: 59.8 | Oral, 5 g, 4 times/d | 2 M | hs-CRP, overall effectiveness | NRS | U: 7.89(1.31) → 3.10(0.93) C: 7.95(1.43) → 5.37(1.02) |
| Kuo et al. 2019 [41] | RCT | HD + Ca+ Calcitriol | U: 30 C: 30 | U: 42.6(3.2) C: 41.9(3.4) | Oral, 5 g, 4 times/d | 3 M | Ca, P, PTH, overall effectiveness | -- | -- |
| Kun et al. 2019 [42] | RCT | HD | U: 23 C: 23 | U:45.3(5.3) C:46.1(4.9) | Oral, 5 g, 4 times/d | 3 M | overall effectiveness | VAS | U: 8.13(1.77) → 4.73(1.41) C: 8.40(2.07) → 6.28(2.19) |
| Li et al. 2019 [43] | RCT | HD | U: 52 C: 50 | U: 47.2(3.7) C: 46.7(4.2) | Oral, 5 g, 4 times/d | 3 M | Ca, P, PTH, β2-MG, hs-CRP, overall effectiveness | VAS | U: 8.18(1.69) → 4.31(1.52) C: 8.20(1.96) → 6.38(1.88) |
| Chen et al. 2020 [24] | RCT | HD | U: 50 C: 50 | U:65.72(10.33) C:64.12(10.54) | Oral, 5 g, 4 times/d | 3 M | Ca, P, PTH, SCr, BUN, β2-MG, overall effectiveness, ADR | VAS | U: 7.62(1.02) → 3.36(1.06) C: 7.54(0.98) → 5.53 (1.78) |
| 5-DIS | U: 17.37(3.56) → 6.44(1.59) C: 16.98(3.72) → 10.82(2.31) | ||||||||
| DLQI | U: 21.84(5.53) → 8.36(2.21) C: 21.54(5.70) → 10.55(3.88) | ||||||||
| Xi 2020 [46] | RCT | HD | U: 58 C: 58 | U: 47.88(3.52) C: 47.79(3.41) | Oral, 5 g, 4 times/d | -- | P, PTH, β2-MG, hs-CRP, overall effectiveness | VAS | U: 7.21(1.72) → 1.47(0.34) C: 7.23(1.71) → 3.48(0.53) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, P.-H.; Wang, J.-Y.; Chuo, H.-E.; Lu, P.-H. Effects of Uremic Clearance Granules in Uremic Pruritus: A Meta-Analysis. Toxins 2021, 13, 702. https://doi.org/10.3390/toxins13100702
Lu P-H, Wang J-Y, Chuo H-E, Lu P-H. Effects of Uremic Clearance Granules in Uremic Pruritus: A Meta-Analysis. Toxins. 2021; 13(10):702. https://doi.org/10.3390/toxins13100702
Chicago/Turabian StyleLu, Ping-Hsun, Jen-Yu Wang, Hui-En Chuo, and Po-Hsuan Lu. 2021. "Effects of Uremic Clearance Granules in Uremic Pruritus: A Meta-Analysis" Toxins 13, no. 10: 702. https://doi.org/10.3390/toxins13100702
APA StyleLu, P.-H., Wang, J.-Y., Chuo, H.-E., & Lu, P.-H. (2021). Effects of Uremic Clearance Granules in Uremic Pruritus: A Meta-Analysis. Toxins, 13(10), 702. https://doi.org/10.3390/toxins13100702





