Increased Calcium Supplementation Postpartum Is Associated with Breastfeeding among Chinese Mothers: Finding from Two Prospective Cohort Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Ethical Approval
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Participants
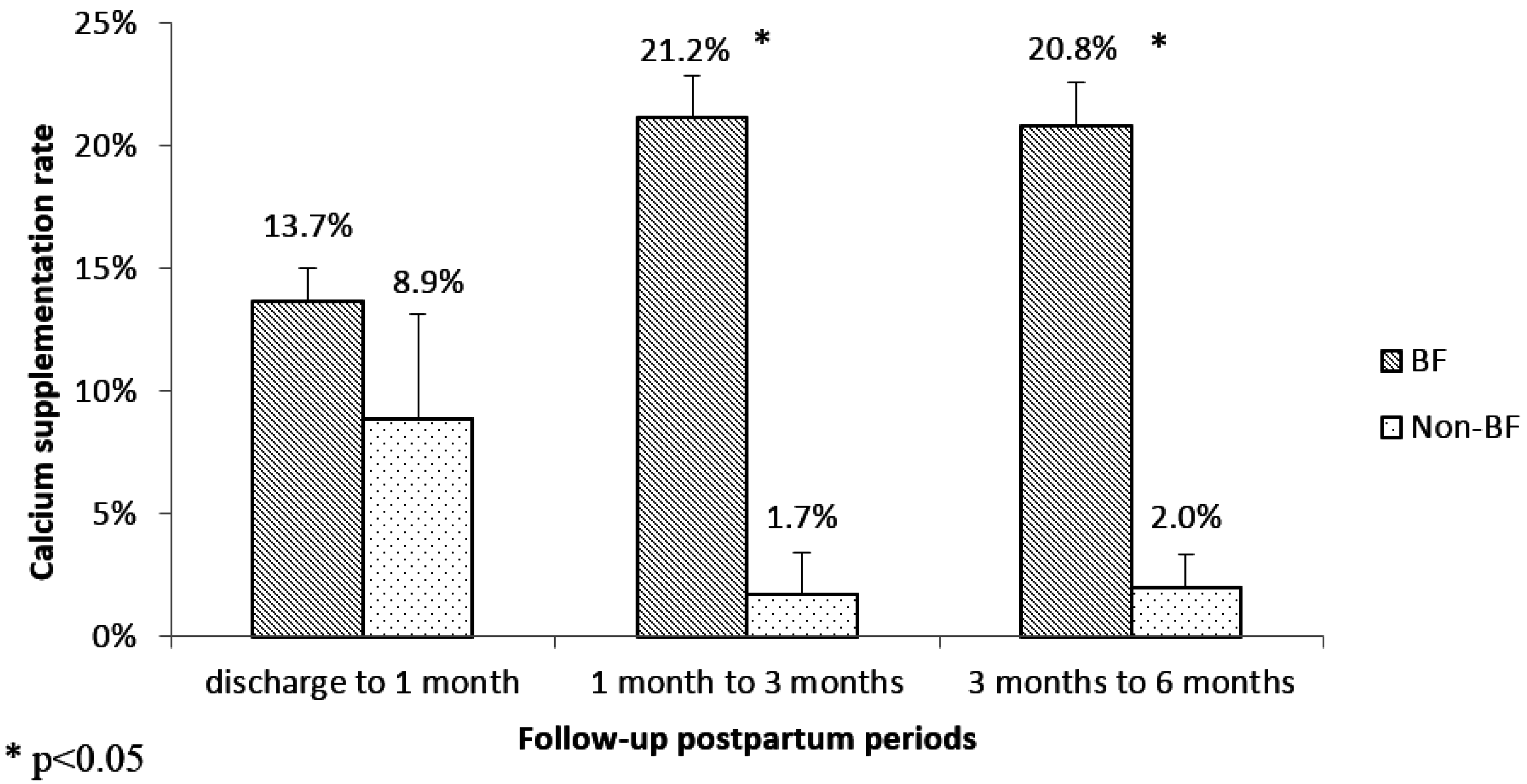
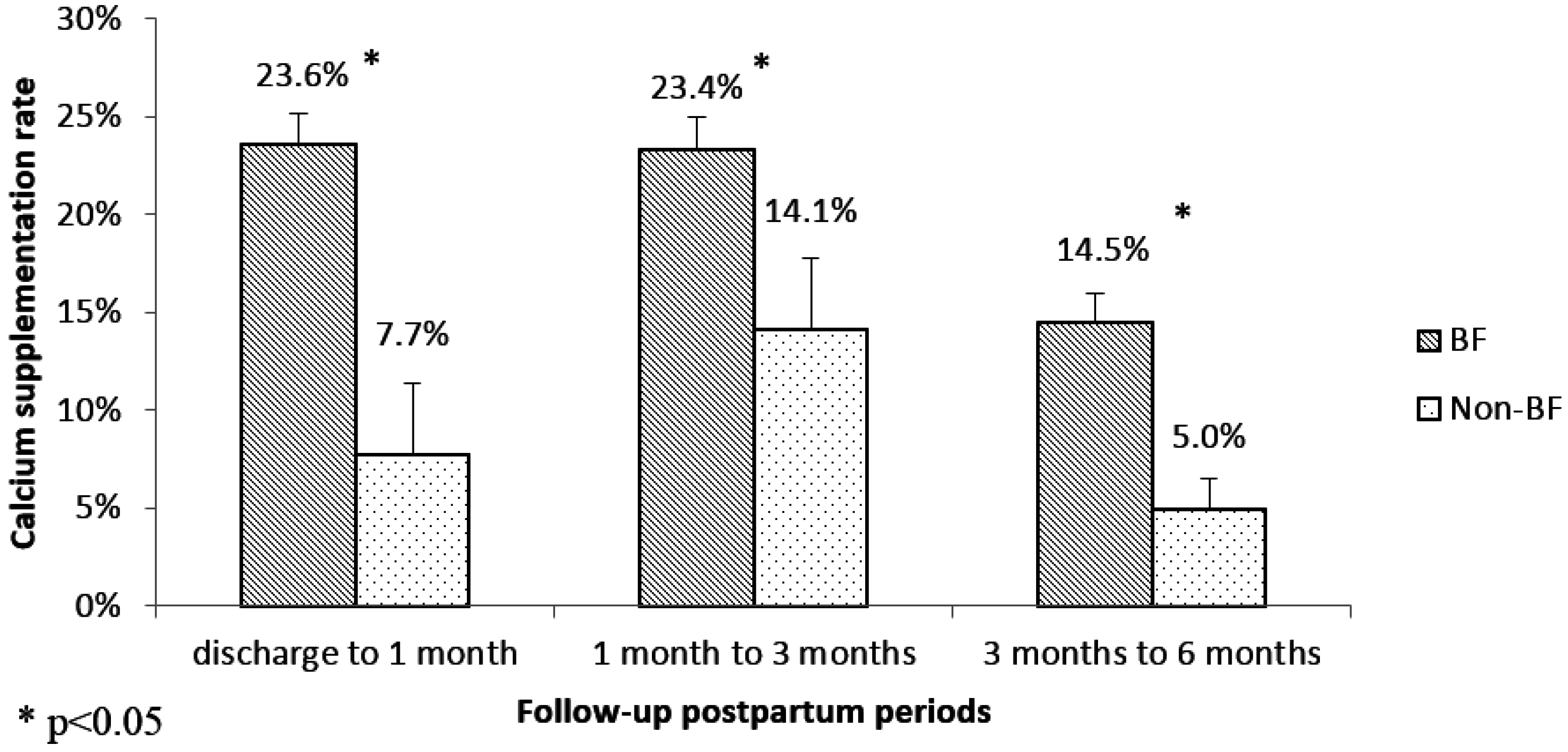
3.2. Calcium Supplementation Status during Postpartum Period
3.3. The Association between Breastfeeding and Calcium Supplementation Postpartum
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Trotter, M.; Hixon, B.B. Sequential changes in weight, density, and percentage ash weight of human skeletons from an early fetal period through old age. Anat. Rec. 1974, 179, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Olausson, H.; Goldberg, G.R.; Laskey, M.A.; Schoenmakers, I.; Jarjou, L.M.; Prentice, A. Calcium economy in human pregnancy and lactation. Nutr. Res. Rev. 2012, 25, 40–67. [Google Scholar] [CrossRef] [PubMed]
- Kalkwarf, H.J.; Specker, B.L.; Ho, M. Effects of calcium supplementation on calcium homeostasis and bone turnover in lactating women. J. Clin. Endocrinol. Metab. 1999, 84, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, C.S.; Ralston, S.H. Presentation and management of osteoporosis presenting in association with pregnancy or lactation. Osteoporos. Int. 2015, 26, 2223–2241. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.; Weisman, S.M. Calcium supplementation during pregnancy and lactation: Effects on the mother and the fetus. Am. J. Obstet. Gynecol. 2006, 194, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A. Calcium in pregnancy and lactation. Annu. Rev. Nutr. 2000, 20, 249–272. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, C.S. Calcium and bone metabolism disorders during pregnancy and lactation. Endocrinol. Metab. Clin. N. Am. 2011, 40, 795–826. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Chen, Y.M.; Teucher, B.; Tang, X.Y.; Dainty, J.R.; Lee, K.K.; Woo, J.L.; Ho, S.C. Calcium absorption in postmenopausal Chinese women: A randomized crossover intervention study. Br. J. Nutr. 2007, 97, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.; Li, Y.; Jin, Y.; Zhai, F.; Kok, F.J.; Yang, X. Phytate intake and molar ratios of phytate to zinc, iron and calcium in the diets of people in China. Eur. J. Clin. Nutr. 2007, 61, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, S. Worldwide trends in dairy production and consumption and calcium intake: Is promoting consumption of dairy products a sustainable solution for inadequate calcium intake? Food Nutr. Bull. 2008, 29, 172–185. [Google Scholar] [CrossRef] [PubMed]
- Shin, A.; Li, H.; Shu, X.O.; Yang, G.; Gao, Y.T.; Zheng, W. Dietary intake of calcium, fiber and other micronutrients in relation to colorectal cancer risk: Results from the Shanghai Women’s Health Study. Int. J. Cancer 2006, 119, 2938–2942. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Huang, Y.M.; Lin, Q. Main sources of dietary calcium in perimenopausal women in Changsha. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2008, 33, 875–879. [Google Scholar] [PubMed]
- Liu, X.; Zhao, X.; Xu, L. Food sources of calcium and iron in the diet of Beijing elderly. Wei Sheng Yan Jiu 2004, 33, 336–338. [Google Scholar] [PubMed]
- He, Y.; Zhai, F.; Wang, Z.; Hu, Y. Status of dietary calcium intake of Chinese residents. Wei Sheng Yan Jiu 2007, 36, 600–602. [Google Scholar] [PubMed]
- Lai, J.; Yin, S.; Ma, G.; Piao, J.; Yang, X. The nutrition and health survery of pregnant women in China. Acta Nutr. Sin. 2007, 29, 4–8. [Google Scholar]
- De Vrese, M.; Stegelmann, A.; Richter, B.; Fenselau, S.; Laue, C.; Schrezenmeir, J. Probiotics—Compensation for lactase insufficiency. Am. J. Clin. Nutr. 2001, 73, 421S–429S. [Google Scholar] [PubMed]
- Wang, Y.G.; Yan, Y.S.; Xu, J.J.; Du, R.F.; Flatz, S.D.; Kuhnau, W.; Flatz, G. Prevalence of primary adult lactose malabsorption in three populations of northern China. Hum. Genet. 1984, 67, 103–106. [Google Scholar] [PubMed]
- National Health and Family Planning Commission of the People’s Republic of China. Maternal and Child Health Basic Knowledge and Skills (Trial Version). Available online: http://www.nhfpc.gov.cn/fys/kpxc/201405/0065ee2071204f0c9b52f7cdcbb392f2.shtml (accessed on 5 July 2016).
- O’Brien, K.O.; Donangelo, C.M.; Ritchie, L.D.; Gildengorin, G.; Abrams, S.; King, J.C. Serum 1,25-dihydroxyvitamin D and calcium intake affect rates of bone calcium deposition during pregnancy and the early postpartum period. Am. J. Clin. Nutr. 2012, 96, 64–72. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.O.; Donangelo, C.M.; Zapata, C.L.; Abrams, S.A.; Spencer, E.M.; King, J.C. Bone calcium turnover during pregnancy and lactation in women with low calcium diets is associated with calcium intake and circulating insulin-like growth factor 1 concentrations. Am. J. Clin. Nutr. 2006, 83, 317–323. [Google Scholar] [PubMed]
- Chan, G.M.; McMurry, M.; Westover, K.; Engelbert-Fenton, K.; Thomas, M.R. Effects of increased dietary calcium intake upon the calcium and bone mineral status of lactating adolescent and adult women. Am. J. Clin. Nutr. 1987, 46, 319–323. [Google Scholar] [PubMed]
- Yoneyama, K.; Ikeda, J. The effects of increased dietary calcium intake on bone mineral density in long-term lactating women, and recovery of bone loss caused by long-term lactation with low calcium diet. Nihon Koshu Eisei Zasshi 2004, 51, 1008–1017. [Google Scholar] [PubMed]
- Li, Y.; Liao, D.; Miao, L.; Qian, X. Analysis on dietary investigation of pregnant and lactating women. Chin. Prim. Health Care 2004, 18, 27–28. [Google Scholar]
- Huang, Z. The Dietary Status of 269 Lactating Women and the Content of Minerals in Breast Milk. Master’s Thesis, Central South University, Changsha, China, 2014. [Google Scholar]
- Yang, T.; Zhang, Y.; Ma, D.; Li, W.; Yang, X.; Wang, P. Survey on the nutrients intake of lactating women in three cities of China. Acta Nutr. Sin. 2014, 36, 84–86. [Google Scholar]
- Chen, H.; Wang, P.; Han, Y.; Ma, J.; Troy, F.A., II; Wang, B. Evaluation of dietary intake of lactating women in China and its potential impact on the health of mothers and infants. BMC Women’s Health 2012, 12, 18. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Fei, J.; Zhai, Y.; Feng, Y.; Li, J. Dietary survey of lactating mothers during the puerperal state. China Med. Her. 2016, 13, 49–68. [Google Scholar]
- Qiu, L.; Zhao, Y.; Binns, C.W.; Lee, A.H.; Xie, X. A cohort study of infant feeding practices in city, suburban and rural areas in Zhejiang Province, PR China. Int. Breastfeed. J. 2008, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Liu, X.; Binns, C.W.; Xiao, C.; Wu, J.; Lee, A.H. A decade of change in breastfeeding in China’s far north-west. Int. Breastfeed. J. 2006, 1, 22. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.A.; Landers, M.C.; Hughes, R.M.; Binns, C.W. Factors associated with breastfeeding at discharge and duration of breastfeeding. J. Paediatr. Child Health 2001, 37, 254–261. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Indicators for assessing infant and young child feeding practices: Part 1: Definitions. In Proceedings of the Conclusions of a Consensus Meeting, Washington, DC, USA, 6–8 November 2007.
- Chan, S.M.; Nelson, E.A.; Leung, S.S.; Cheng, J.C. Bone mineral density and calcium metabolism of Hong Kong Chinese postpartum women—A 1-y longitudinal study. Eur. J. Clin. Nutr. 2005, 59, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Laskey, M.A.; Prentice, A.; Hanratty, L.A.; Jarjou, L.M.; Dibba, B.; Beavan, S.R.; Cole, T.J. Bone changes after 3 mo of lactation: Influence of calcium intake, breast-milk output, and vitamin D-receptor genotype. Am. J. Clin. Nutr. 1998, 67, 685–692. [Google Scholar] [PubMed]
- Lopez, J.M.; Gonzalez, G.; Reyes, V.; Campino, C.; Diaz, S. Bone turnover and density in healthy women during breastfeeding and after weaning. Osteoporos. Int. 1996, 6, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Kalkwarf, H.J.; Specker, B.L.; Bianchi, D.C.; Ranz, J.; Ho, M. The effect of calcium supplementation on bone density during lactation and after weaning. N. Engl. J. Med. 1997, 337, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Prentice, A.; Jarjou, L.M.; Cole, T.J.; Stirling, D.M.; Dibba, B.; Fairweather-Tait, S. Calcium requirements of lactating Gambian mothers: Effects of a calcium supplement on breast-milk calcium concentration, maternal bone mineral content, and urinary calcium excretion. Am. J. Clin. Nutr. 1995, 62, 58–67. [Google Scholar] [PubMed]
- Jarjou, L.M.; Prentice, A.; Sawo, Y.; Laskey, M.A.; Bennett, J.; Goldberg, G.R.; Cole, T.J. Randomized, placebo-controlled, calcium supplementation study in pregnant Gambian women: Effects on breast-milk calcium concentrations and infant birth weight, growth, and bone mineral accretion in the first year of life. Am. J. Clin. Nutr. 2006, 83, 657–666. [Google Scholar] [PubMed]
- Zhang, Z.Q.; Chen, Y.M.; Wang, R.Q.; Huang, Z.W.; Yang, X.G.; Su, Y.X. The effects of different levels of calcium supplementation on the bone mineral status of postpartum lactating Chinese women: A 12-month randomised, double-blinded, controlled trial. Br. J. Nutr. 2016, 115, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Cross, N.A.; Hillman, L.S.; Allen, S.H.; Krause, G.F. Changes in bone mineral density and markers of bone remodeling during lactation and postweaning in women consuming high amounts of calcium. J. Bone Miner. Res. 1995, 10, 1312–1320. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, C.S. Maternal mineral and bone metabolism during pregnancy, lactation, and post-weaning recovery. Physiol. Rev. 2016, 96, 449–547. [Google Scholar] [PubMed]
- Wang, J.; Yang, F.; Mao, M.; Liu, D.H.; Yang, H.M.; Yang, S.F. High prevalence of vitamin D and calcium deficiency among pregnant women and their newborns in Chengdu, China. World J. Pediatr. WJP 2010, 6, 265–267. [Google Scholar] [CrossRef] [PubMed]
| Study Location | Study Design | Study Period | Average Daily Dietary Calcium Intake (Postpartum) |
|---|---|---|---|
| Guangzhou [24] | Prospective cohort | 2002 | 786.45 mg (12 weeks) |
| Hunan [25] | Cross-sectional | 2011–2012 | 426 mg |
| Beijing, Suzhou & Guangzhou [26] | Cross-sectional | 2011–2012 | 401.4 mg (0–1 month) |
| 585.3 mg (1–2 months) | |||
| 591.2 mg (2–4 months) | |||
| 649.0 mg (4–8 months) | |||
| Fujian [27] | Prospective cohort | 2012 | 428 mg (2 days) |
| 454 mg (7 days) | |||
| 595 mg (30 days) | |||
| 544 mg (90 days) | |||
| Shanghai [28] | Prospective cohort | 2014–2015 | 749.3 mg (1–3 days) |
| 781.1 mg (7–9 days) | |||
| 762.3 mg (14–17 days) | |||
| 768.4 mg (25–27 days) | |||
| 678.5 mg (39–41 days) |
| Variable | Cohort in Jiangyou (n = 695) | Cohort in Chengdu (n = 845) | ||
|---|---|---|---|---|
| BF | Non-BF | BF | Non-BF | |
| Number of participants | 650 (93.5) | 45 (6.5) | 786 (93.0) | 59 (7.0) |
| Household annual income (Chinese yuan) | ||||
| <2000 | 186 (31.0) | 9 (23.1) | 1 (0.2) | 0 (0.0) |
| 2000–5000 | 309 (51.4) | 23 (59.0) | 155 (23.5) | 12 (24.0) |
| >5000 | 106 (17.6) | 7 (17.9) | 503 (76.3) | 38 (76.0) |
| Maternal age (years) | ||||
| <25 | 373 (57.4) | 26 (57.8) | 156 (19.9) | 5 (8.5) |
| 25–29 | 163 (25.1) | 13 (28.9) | 372 (47.3) | 28 (47.5) |
| >29 | 114 (17.5) | 6 (13.3) | 258 (32.8) | 26 (44.0) |
| Maternal education | ||||
| Secondary school or lower | 355 (54.6) | 25 (55.6) | 90 (11.5) | 11 (18.6) |
| Senior school | 215 (33.1) | 18 (40.0) | 165 (21.0) | 11 (18.6) |
| University or higher | 80 (12.3) | 2 (4.4) | 531 (67.5) | 37 (62.8) |
| Parity | ||||
| Primiparous | 518 (79.7) | 37 (82.2) | 700 (89.1) | 51 (86.4) |
| Multiparous | 132 (20.3) | 8 (17.8) | 86 (10.9) | 8 (13.6) |
| Gravidity | ||||
| Primigravida | 249 (38.3) | 18 (40.0) | 430 (54.7) | 26 (44.1) |
| Multigravida | 401 (61.7) | 27 (60.0) | 356 (45.3) | 33 (55.9) |
| Infant gender | ||||
| Male | 328 (50.5) | 26 (57.8) | 412 (52.4) | 34 (57.6) |
| Female | 322 (49.5) | 19 (42.2) | 374 (47.6) | 25 (42.4) |
| Infant birth weight (g) | ||||
| <2500 | 10 (1.5) | 2 (4.4) | 13 (1.7) | 0 (0.0) |
| ≥2500 | 640 (98.5) | 43 (95.6) | 773 (98.3) | 59 (100.0) |
| Infant gestational week | ||||
| <37 | 8 (1.2) | 3 (6.8) | 9 (1.2) | 2 (3.4) |
| ≥37 | 640 (98.8) | 41 (93.2) | 777 (98.8) | 57 (96.6) |
| Calcium supplementation during pregnancy | ||||
| Yes | 410 (63.1) | 25 (55.6) | 627 (79.8) | 47 (79.7) |
| No | 240 (36.9) | 20 (44.4) | 159 (20.2) | 12 (20.3) |
| Variable | Model II | Model IV |
|---|---|---|
| Crude ORs (95% CI) | Adjusted ORs (95% CI) | |
| Jiangyou Cohort | ||
| Measurement times * | ||
| At discharge (ref) | 1 | 1 |
| 1 month | 1.72 (1.24, 2.38) | 1.90 (1.33, 2.70) |
| 3 months | 1.57 (1.12, 2.20) | 1.69 (1.18, 2.44) |
| Breastfeeding status * | ||
| Non-breastfeeding (ref) | 1 | 1 |
| Any breastfeeding | 5.85 (2.50, 13.72) | 6.95 (2.68, 18.04) |
| Chengdu Cohort | ||
| Measurement times * | ||
| At discharge (ref) | 1 | 1 |
| 1 month | 1.02 (0.74, 1.43) | 1.02 (0.72, 1.45) |
| 3 months | 0.31 (0.21, 0.46) | 0.30 (0.20, 0.45) |
| Breastfeeding status * | ||
| Non-breastfeeding (ref) | 1 | 1 |
| Any breastfeeding | 2.88 (1.50, 5.54) | 3.03 (1.52, 6.02) |
| Pooled effect size of two studies | ||
| Non-breastfeeding (ref) | - | 1 |
| Any breastfeeding | - | 4.02 (2.30, 7.03) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, J.; Zhao, Y.; Binns, C.W.; Lee, A.H. Increased Calcium Supplementation Postpartum Is Associated with Breastfeeding among Chinese Mothers: Finding from Two Prospective Cohort Studies. Nutrients 2016, 8, 622. https://doi.org/10.3390/nu8100622
Zhao J, Zhao Y, Binns CW, Lee AH. Increased Calcium Supplementation Postpartum Is Associated with Breastfeeding among Chinese Mothers: Finding from Two Prospective Cohort Studies. Nutrients. 2016; 8(10):622. https://doi.org/10.3390/nu8100622
Chicago/Turabian StyleZhao, Jian, Yun Zhao, Colin W. Binns, and Andy H. Lee. 2016. "Increased Calcium Supplementation Postpartum Is Associated with Breastfeeding among Chinese Mothers: Finding from Two Prospective Cohort Studies" Nutrients 8, no. 10: 622. https://doi.org/10.3390/nu8100622
APA StyleZhao, J., Zhao, Y., Binns, C. W., & Lee, A. H. (2016). Increased Calcium Supplementation Postpartum Is Associated with Breastfeeding among Chinese Mothers: Finding from Two Prospective Cohort Studies. Nutrients, 8(10), 622. https://doi.org/10.3390/nu8100622






