Cardiometabolic Phenotypes and Dietary Patterns in Albanian University-Enrolled Young Adults: Cross-Sectional Findings from the Nutrition Synergies WHO-Aligned Sentinel Platform
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
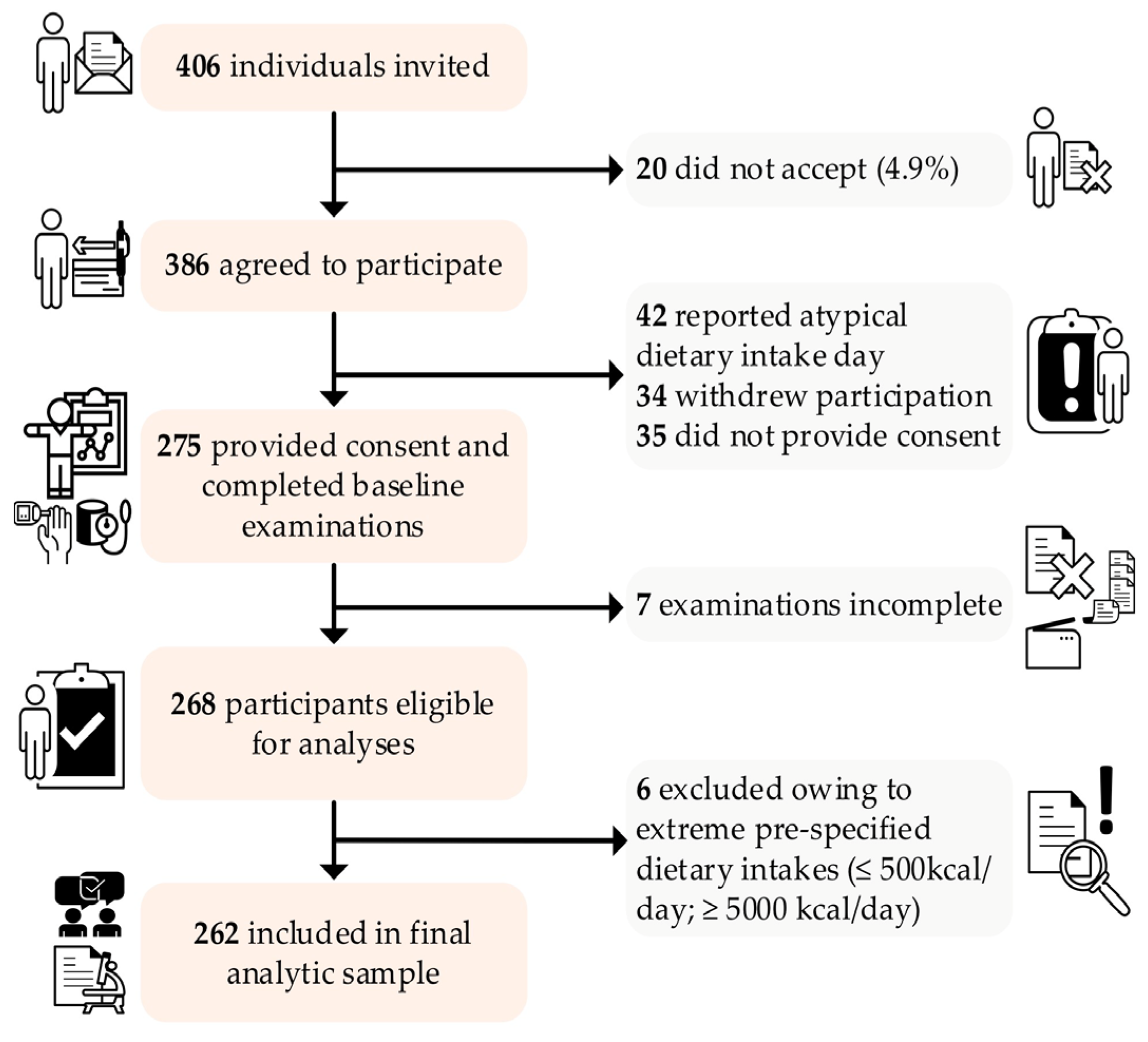
2.2. Participants and Recruitment
2.3. Anthropometrics, BP and Glycemia
2.4. Dietary Assessment and Lifestyle
2.5. Diet Quality and Composite Cardiometabolic Risks Indices
2.6. Energy Intake–Expenditure Plausibility (Goldberg)
2.7. Statistical Analysis
3. Results
3.1. Participant Characteristics and Sample
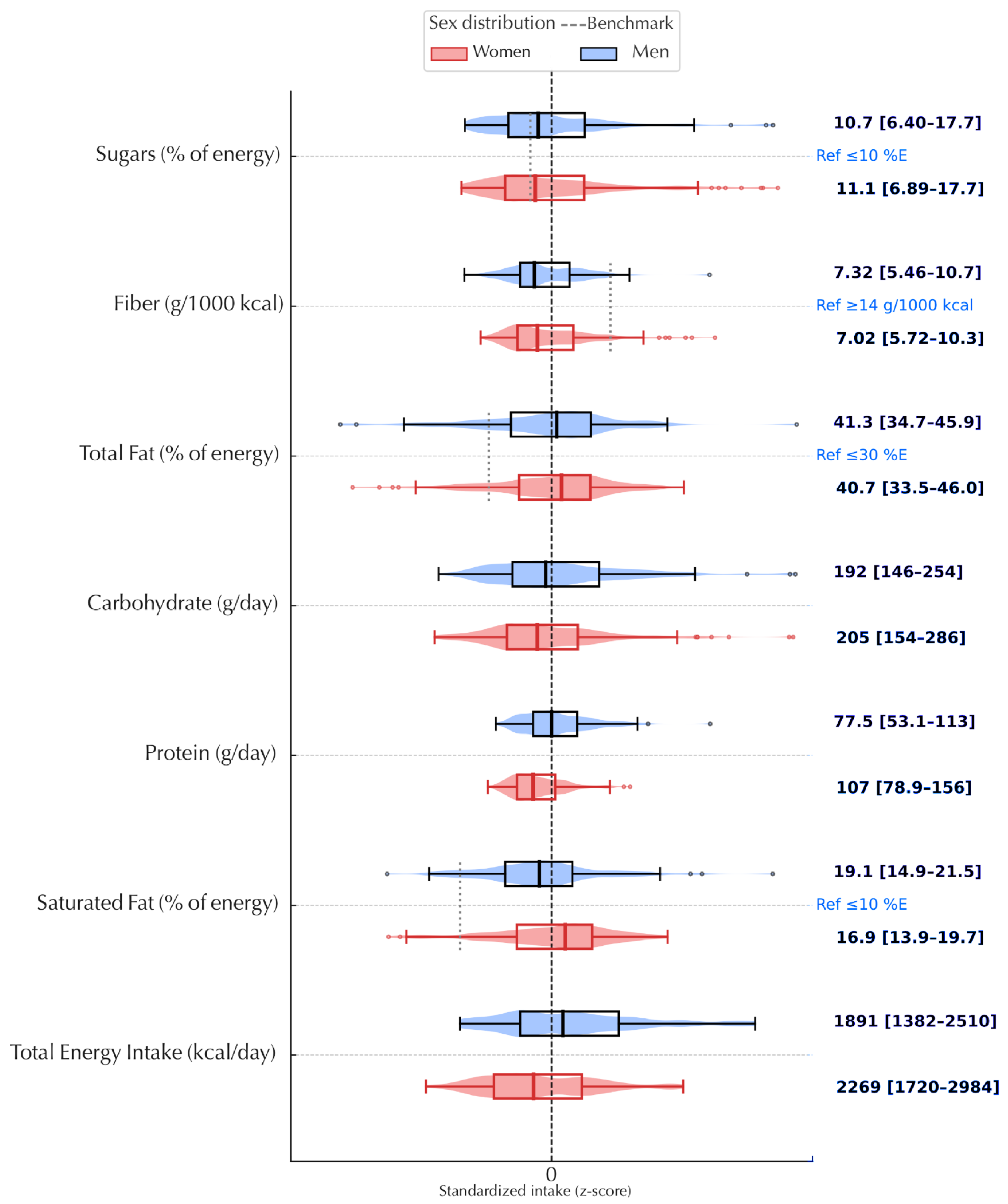
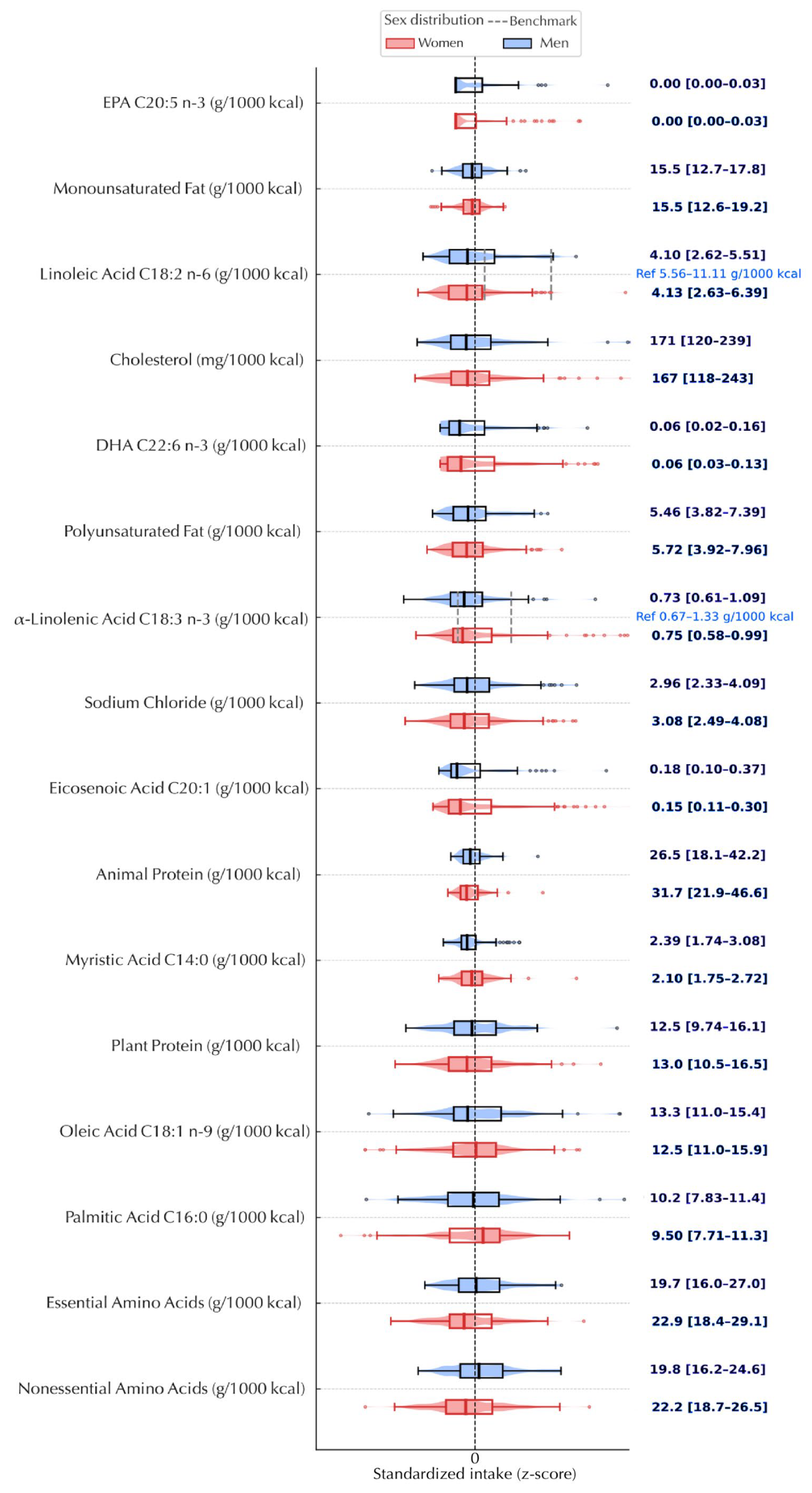
3.2. Phenotypes of Cardiometabolic Risks

3.3. Diet–Phenotype Associations (Isocaloric Substitution)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Definition |
| ALA/C18:3 | α-Linolenic Acid (per 1000 kcal) |
| BMI | Body Mass Index (kg/m2) |
| cCMRS | Composite Cardiometabolic Risk Score (standardized) |
| C16:0 | Palmitic Acid (per 1000 kcal) |
| C18:1 | Oleic Acid (per 1000 kcal) |
| C18:2 | Linoleic Acid (per 1000 kcal) |
| DBP | Diastolic Blood Pressure (mmHg) |
| EAA | Essential Amino Acids (per 1000 kcal) |
| EI/TEE | Energy Intake/Total Energy Expenditure ratio |
| EPA/1000 kcal | Eicosapentaenoic Acid (per 1000 kcal) |
| FDR (q) | False Discovery Rate (Benjamini–Hochberg) |
| HBSC | Health Behavior in School-aged Children survey (WHO/Europe) |
| IDF | International Diabetes Federation |
| IQR | Interquartile Range |
| K/1000 kcal | Potassium (per 1000 kcal) |
| LE8 | Life’s Essential 8 cardiovascular health score (AHA, 0–100 scale) |
| MET | Metabolic Equivalent of Task |
| MUFA | Monounsaturated Fatty Acids |
| NCDs | Non-Communicable Diseases |
| PRAL | Potential Renal Acid Load (mEq/day) |
| PUFA | Polyunsaturated Fatty Acids |
| SBP | Systolic Blood Pressure (mmHg) |
| SFA | Saturated Fatty Acids |
| WCRF score | World Cancer Research Fund index score |
| WHtR | Waist-to-Height Ratio |
References
- Miranda, J.J.; Barrientos-Gutiérrez, T.; Corvalan, C.; Hyder, A.A.; Lazo-Porras, M.; Oni, T.; Wells, J.C.K. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat. Med. 2019, 25, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Ng, S.W. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes. Rev. 2022, 23, e13366. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Progress Monitor 2025. 2025. Available online: https://www.who.int/publications/i/item/9789240105775 (accessed on 12 September 2025).
- Mone, I.; Kraja, B.; Roshi, E.; Burazer, G. Overview on health status of the Albanian population. South East. Eur. J. Public Health 2023, 4, 1–6. [Google Scholar] [CrossRef]
- World Obesity Federation. Report Card—Adults: Albania. Global Obesity Observatory. 2025. Available online: https://data.worldobesity.org/country/albania-2/ (accessed on 25 August 2025).
- International Diabetes Federation. Diabetes in Europe, IDF Diabetes Atlas (Albania). Diabetes Atlas. 2025. Available online: https://diabetesatlas.org/data-by-location/region/europe/ (accessed on 17 August 2025).
- World Health Organization Regional Office for Europe. Hypertension Country Profile: Albania. 2023. Available online: https://cdn.who.int/media/docs/default-source/country-profiles/hypertension/hypertension-2023/hypertension_alb_2023.pdf (accessed on 22 July 2025).
- Schlesinger, S.; Neuenschwander, M.; Barbaresko, J.; Lang, A.; Maalmi, H.; Rathmann, W.; Roden, M.; Herder, C. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: Umbrella review of meta-analyses of prospective studies. Diabetologia 2022, 65, 275–285. [Google Scholar] [CrossRef]
- Cai, X.; Zhang, Y.; Li, M.; Wu, J.H.; Mai, L.; Li, J.; Yang, Y.; Hu, Y.; Huang, Y. Association between prediabetes and risk of all cause mortality and cardiovascular disease: Updated meta-analysis. BMJ 2020, 370, m2297. [Google Scholar] [CrossRef]
- Lara-Castor, L.; O’Hearn, M.; Cudhea, F.; Miller, V.; Shi, P.; Zhang, J.; Sharib, J.R.; Cash, S.B.; Barquera, S.; Micha, R.; et al. Burdens of type 2 diabetes and cardiovascular disease attributable to sugar-sweetened beverages in 184 countries. Nat. Med. 2025, 31, 552–564. [Google Scholar] [CrossRef]
- Global Nutrition Report. Albania—Country Nutrition Profile. Global Nutrition Report: Country Nutrition Profiles. 2025. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/europe/southern-europe/albania/ (accessed on 22 July 2025).
- Vincze, F.; Muka, T.; Eichelmann, F.; Llanaj, E. Eating out intensity, ultra-processed foods and BMI among Albanian youth. Public Health Nutr. 2023, 26, 2953–2962. [Google Scholar] [CrossRef]
- Institute of Public Health Albania, U.A., World Health Organization, Regional Office for Europe. Childhood Obesity in Albania: A Comprehensive Assessment. 2023. Available online: https://www.unicef.org/albania/media/6581/file/ASSESSMENT%20OF%20CHILDHOOD%20OBESITY.pdf (accessed on 23 July 2025).
- World Health Organization. Physical Activity Country Profile: Albania. 2022. Available online: https://cdn.who.int/media/docs/default-source/country-profiles/physical-activity/physical-activity-alb-2022-country-profile.pdf (accessed on 23 July 2025).
- European Commission. Albania 2022 Report. Commission Staff Working Document. 2022. Available online: https://enlargement.ec.europa.eu/albania-report-2022_en (accessed on 23 July 2025).
- European Commission. Albania 2023 Report. Commission Staff Working Document. 2023. Available online: https://enlargement.ec.europa.eu/albania-report-2023_en (accessed on 23 July 2025).
- European Commission. Albania 2024 Report. Commission Staff Working Document. 2024. Available online: https://enlargement.ec.europa.eu/albania-report-2024_en (accessed on 23 July 2025).
- Galea, G.; Ekberg, A.; Ciobanu, A.; Corbex, M.; Farrington, J.; Ferreira-Bores, C.; Kokole, D.; Losada, M.L.; Neufeld, M.; Rakovac, I.; et al. Quick buys for prevention and control of noncommunicable diseases. Lancet Reg. Health—Eur. 2025, 52, 101281. [Google Scholar] [CrossRef] [PubMed]
- Remer, T.; Manz, F. Potential renal acid load of foods and its influence on urine pH. J. Am. Diet. Assoc. 1995, 95, 791–797. [Google Scholar] [CrossRef]
- Chan, R.; Wong, V.W.S.; Chu, W.-C.; Wong, G.L.H.; Li, A.M.; Chan, A.W.H.; Chim, A.M.L.; Chan, H.Y.; Choi, P.C.L.; Chan, J.C.N.; et al. Diet-Quality Scores and Prevalence of Nonalcoholic Fatty Liver Disease in Hong Kong Chinese: A Population Study. Sci. Rep. 2015, 5, 11487. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F. Life’s Essential 8: Updating and Enhancing the American Heart Association’s Construct of Cardiovascular Health: A Presidential Advisory from the American Heart Association. Circulation 2022, 146, e18–e43. [Google Scholar] [CrossRef]
- Signorini, D.F. Sample size for Poisson regression. Biometrika 1991, 78, 446–450. [Google Scholar] [CrossRef]
- Magnani, R. Food and Nutrition Technical Assistance Project (FANTA); Academy for Educational Development: Washington, DC, USA, 1997; Available online: https://www.micronutrient.org/nutritiontoolkit/ModuleFolders/5.Sampling/resources/FANTA_-_Sampling_Guide.pdf (accessed on 3 September 2025).
- World Health Organization. WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance; WHO: Geneva, Switzerland, 2005; Available online: https://iris.who.int/handle/10665/43376 (accessed on 11 September 2025).
- International Diabetes Federation. The IDF Consensus Worldwide Definition of the Metabolic Syndrome. 2005. Available online: https://idf.org/media/uploads/2023/05/attachments-30.pdf (accessed on 11 September 2025).
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. The metabolic syndrome—A new worldwide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Mancia, G.; Kreutz, R.; Brunström, M.; Burnier, M.; Grassi, G.; Januszewicz, A.; Muiesan, M.L.; Tsioufis, K.; Agabiti-Rosei, E.; Algharably, E.A.E.; et al. 2023 ESH Guidelines for the Management of Arterial Hypertension. J. Hypertens. 2023, 41, 1874–2071. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2025. Diabetes Care 2025, 48, S27–S49. [Google Scholar] [CrossRef]
- Llanaj, E.; Hanley-Cook, G.T. Adherence to healthy and sustainable diets is not differentiated by cost, but rather source of foods among young adults in Albania. Br. J. Nutr. 2021, 126, 591–599. [Google Scholar] [CrossRef]
- Llanaj, E.; D’Haese, M.; Lachat, C. Food Intake and Eating Out of Home Patterns Amongst University Students of Tirana, Albania; Ghent University: Ghent, Belgium, 2016. [Google Scholar]
- Finglas, P.M.; Roe, M.A.; Pinchen, H.M.; Berry, R.; Church, S.M.; Dodhia, S.K.; Farron-Wilson, M.; Swan, G. McCance and Widdowson’s the Composition of Foods: Seventh Summary Edition; Royal Society of Chemistry: Cambridge, UK, 2015. [Google Scholar]
- Willett, W. Nutritional Epidemiology, 3rd revised ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Hagströmer, M.; Bergman, P.; De Bourdeaudhuij, I.; Ortega, F.B.; Ruiz, J.R.; Manios, Y.; Sjöström, M. Concurrent validity of a modified IPAQ for adolescents (IPAQ-A): The HELENA Study. Int. J. Obes. 2008, 32, S42–S48. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Shams-White, M.M.; Brockton, N.T.; Mitrou, P.; Romaguera, D.; Brown, S.; Bender, A.; Kahle, L.L.; Reedy, J. Operationalizing the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) Cancer Prevention Recommendations: A Standardized Scoring System. Nutrients 2019, 11, 1572. [Google Scholar] [CrossRef]
- Eisenmann, J.C. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc. Diabetol. 2008, 7, 17. [Google Scholar] [CrossRef]
- Schofield, W.N. Predicting basal metabolic rate, new standards and review of previous work. Hum. Nutr. Clin. Nutr. 1985, 39, 5–41. Available online: https://pubmed.ncbi.nlm.nih.gov/4044297/ (accessed on 11 September 2025).
- Goldberg, G.R.; Black, A.E.; Jebb, S.A.; Cole, T.J.; Murgatroyd, P.R.; Coward, W.A.; Prentice, A.M. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur. J. Clin. Nutr. 1991, 45, 569–581. Available online: https://pubmed.ncbi.nlm.nih.gov/1810719/ (accessed on 11 September 2025).
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. 2000, 24, 1119–1130. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Human Energy Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation; FAO Food and Nutrition Technical Report Series 1; FAO: Rome, Italy, 2004; Available online: https://www.fao.org/4/y5686e/y5686e00.htm (accessed on 11 September 2025).
- Henry, C.J.K. Basal metabolic rate studies in humans: Measurement and development of new equations. Public Health Nutr. 2005, 8, 1133–1152. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Society. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef]
- Lachat, C.; Hawwash, D.; Ocké, M.C.; Berg, C.; Forsum, E.; Hörnell, A.; Larsson, C.; Sonestedt, E.; Wirfält, E.; Åkesson, A.; et al. Strengthening the Reporting of Observational Studies in Epidemiology—Nutritional Epidemiology (STROBE-nut): An Extension of the STROBE Statement. PLOS Med. 2016, 13, e1002036. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Šimunović, M.; Božić, J.; Milić, L.; Unić, I.; Škrabić, V. The Prevalence of Metabolic Syndrome and Cardiovascular Risk Factors in Obese Children and Adolescents in Dalmatia: A Hospital Based Study. Int. J. Endocrinol. 2016, 2016, 1823561. [Google Scholar] [CrossRef]
- González-Gil, E.M.; Peruchet-Noray, L.; Sedlmeier, A.M.; Christakoudi, S.; Biessy, C.; Navionis, A.-S.; Mahamat-Saleh, Y.; Jaafar, R.F.; Baurecht, H.; Guevara, M.; et al. Association of body shape phenotypes and body fat distribution indexes with inflammatory biomarkers in the European Prospective Investigation into Cancer and Nutrition (EPIC) and UK Biobank. BMC Med. 2024, 22, 334. [Google Scholar] [CrossRef]
- Chrissini, M.K.; Panagiotakos, D.B. Public health interventions tackling childhood obesity at European level: A literature review. Prev. Med. Rep. 2022, 30, 102068. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B. Metabolic health in normal-weight and obese individuals. Diabetologia 2019, 62, 558–566. [Google Scholar] [CrossRef]
- Sattar, N.; Rawshani, A.; Franzén, S.; Rawshani, A.; Svensson, A.M.; Rosengren, A.; McGuire, D.K.; Eliasson, B.; Gudbjörnsdottir, S. Age at Diagnosis of Type 2 Diabetes Mellitus and Associations with Cardiovascular and Mortality Risks. Circulation 2019, 139, 2228–2237. [Google Scholar] [CrossRef]
- Bitew, Z.W.; Alemu, A.; Ayele, E.G.; Tenaw, Z.; Alebel, A.; Worku, T. Metabolic syndrome among children and adolescents in low and middle income countries: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 2020, 12, 93. [Google Scholar] [CrossRef]
- Šoštarič, A.; Jenko, B.; Kozjek, N.R.; Ovijač, D.; Šuput, D.; Milisav, I.; Dolžan, V. Detection of metabolic syndrome burden in healthy young adults may enable timely introduction of disease prevention. Arch. Med. Sci. 2019, 15, 1184–1194. [Google Scholar] [CrossRef]
- Lee, M.-K.; Lee, J.-H.; Sohn, S.Y.; Ahn, J.; Hong, O.-K.; Kim, M.-K.; Baek, K.-H.; Song, K.-H.; Han, K.; Kwon, H.-S. Cumulative exposure to metabolic syndrome in a national population-based cohort of young adults and sex-specific risk for type 2 diabetes. Diabetol. Metab. Syndr. 2023, 15, 78. [Google Scholar] [CrossRef]
- Anton-Păduraru, D.-T.; Mindru, D.E.; Stănescu, R.S.; Trofin, F.; Cobuz, C.; Cobuz, M.; Sur, L.M.; Petroaie, A.; Slănină, A.M.; Manole, M.; et al. Unraveling Metabolic Syndrome in Youth: The Obesity Epidemic’s Hidden Complication. Children 2025, 12, 482. [Google Scholar] [CrossRef]
- Bacha, F.; Hannon, T.S.; Tosur, M.; Pike, J.M.; Butler, A.; Tommerdahl, K.L.; Zeitler, P.S. Pathophysiology and Treatment of Prediabetes and Type 2 Diabetes in Youth. Diabetes Care 2024, 47, 2038–2049. [Google Scholar] [CrossRef]
- Pulgaron, E.R.; Delamater, A.M. Obesity and type 2 diabetes in children: Epidemiology and treatment. Curr. Diab Rep. 2014, 14, 508. [Google Scholar] [CrossRef]
- Nishida, C.; Uauy, R.; Kumanyika, S.; Shetty, P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: Process, product and policy implications. Public Health Nutr. 2004, 7, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine; Food and Nutrition Board; Standing Committee on the Scientific Evaluation of Dietary Reference Intakes; Subcommittee on Interpretation and Uses of Dietary Reference Intakes. Dietary Reference Intakes: Applications in Dietary Assessment; National Academies Press: Washington, DC, USA, 2000. [Google Scholar] [CrossRef]
- Stefan, N.; Yki-Järvinen, H.; Neuschwander-Tetri, B.A. Metabolic dysfunction-associated steatotic liver disease: Heterogeneous pathomechanisms and effectiveness of metabolism-based treatment. Lancet Diabetes Endocrinol. 2025, 13, 134–148. [Google Scholar] [CrossRef]
- Eichelmann, F.; Prada, M.; Sellem, L.; Jackson, K.G.; Salas Salvadó, J.; Razquin Burillo, C.; Estruch, R.; Friedén, M.; Rosqvist, F.; Risérus, U.; et al. Lipidome changes due to improved dietary fat quality inform cardiometabolic risk reduction and precision nutrition. Nat. Med. 2024, 30, 2867–2877. [Google Scholar] [CrossRef] [PubMed]
- Iruzubieta, P.; de Vega, T.; Crespo, J. Overlooked determinants and unequal outcomes: Rethinking metabolic dysfunction-associated steatotic liver disease beyond the biomedical model. Lancet Gastroenterol. Hepatol. 2025. [Google Scholar] [CrossRef] [PubMed]
- Institute of Statistics of Albania. Students in Higher Education by Region, Sex, and Form of Study. Tirana, Albania, 2024. 2024. Available online: https://databaza.instat.gov.al:8083/pxweb/sq/DST/START__ED__REG/Ars005/table/tableViewLayout1/ (accessed on 21 October 2025).
| Variable (Unit) | Women (N = 172) | Men (N = 90) | Total | |
|---|---|---|---|---|
| Age (years) | 21 (21–22) | 21 (21–22) | 21 (21–22) | |
| Height (cm) | 163.5 (159.0–168.0) | 177.0 (173.0–184.0) | 167.0 (161.0–174.0) | |
| Weight (kg) | 59.03 (58–61.50) | 74.50 (68.50–77.50) | 64.43 (61.70–66.35) | |
| Waist circumference (cm) | 75 (73.30–77) | 88.18 (84–90.75) | 79.25 (77.75–81) | |
| Hip circumference (cm) | 99.82 (98.50–101) | 102.75 (100–106.50) | 100.38 (99.50–101.80) | |
| WHtR | 0.46 (0.43–0.50) | 0.51 (0.46–0.53) | 0.47 (0.43–0.51) | |
| BMI (kg/m2) * | 24.08 (23.03–25.12) | 22.98 (22.42–23.55) | 23.36 (22.84–23.87) | |
| SBP (mmHg) | 109.0 (100.0–110.0) | 120.0 (110.0–128.8) | 110.0 (105.0–120.0) | |
| DBP (mmHg) | 70.0 (70.0–80.0) | 80.0 (75.0–85.0) | 75.0 (70.0–80.0) | |
| MAP (mmHg) | 83.33 (83.33–86.67) | 90.83 (88.33–95) | 86.67 (86.67–88.33) | |
| Blood glucose (mg/dL) | 95.2 (88.7–103.0) | 102.0 (95.3–107.4) | 97.7 (90.7–105.0) | |
| Total PA time (min/week) | 1676 (1386–1979.50) | 2821.50 (1872.50–3465) | 1923.75 (1626–2238) | |
| Sitting time (min/day) | 480 (480–540) | 450 (420–480) | 450 (450–480) | |
| PA energy expenditure (kcal/day) | 1742.93 (1358–1986.50) | 3542.25 (2191.04–4439) | 1996.48 (1740–2214) | |
| Essential amino acids (g/1000 kcal) | 19.73 (18.41–21.37) | 22.93 (21.17–25.25) | 21.08 (19.76–21.94) | |
| Alcohol intake ** (drinks/day) | 0.03 (max 1.4), 29.7% any | 0.17 (max 2.6), 35.6% any | 0.08 (max 2.6), 31.7% any | |
| PRAL (mEq/day) | 14.50 (10.46–20.29) | 32.58 (24.98–40.04) | 20.46 (15.37–25.56) | |
| WCRF score (points) | 5.25 (5.25–6.12) | 4.81 (4.38–5.25) | 5.25 (5.25–6.12) | |
| Life’s Essential 8 (0–100) | 54.17 (50–58.33) | 50 (50–58.33) | 50 (50–58.33) | |
| cCMRS (z-score) | −0.27 (−0.37 to −0.16) | 0.38 (0.24–0.49) | −0.05 (−0.16–0.04) | |
| MASLD nutrient score (points) | 2 (2–3) | 2 (2–3) | 2 (2–3) | |
| WHtR ≥ 0.5 (n/%) | 42 (24.4%) | 46 (51.1%) | 88 (33.6%) | |
| IDF (≥94 cm men, ≥80 cm women) | 54 (31.4%) | 32 (35.6%) | 86 (32.8%) | |
| Nicotine use | No | 160 (69.3%) | 71 (30.7%) | 231 (100.0%) |
| Yes | 12 (38.7%) | 19 (61.3%) | 31 (100.0%) | |
| Habitual activity level | Low | 66 (62.3%) | 40 (37.7%) | 106 (100.0%) |
| Moderate | 80 (76.9%) | 24 (23.1%) | 104 (100.0%) | |
| High | 26 (50.0%) | 26 (50.0%) | 52 (100.0%) | |
Food Sources Substituted (Orientation) † | |||||
|---|---|---|---|---|---|
| Domain | Outcome | Substitution (from → to) | Effect per +5%E (95% CI) | p Value | q (BH) |
| Metabolic signatures | PRAL (%) | SFA (%E) → PUFA (%E) | −32.8% (−56.6, −9.1) | 0.007 | 0.054 |
| PRAL (%) | SFA (%E) → MUFA (%E) | −20.9% (−42.7, +0.8) | 0.060 | 0.238 | |
| MASLD | SFA (%E) → PUFA (%E) | −28.2% (−39.0, −17.4) | <0.001 | <0.001 | |
| MASLD | SFA (%E) → MUFA (%E) | −12.4% (−22.3, −2.6) | 0.013 | 0.070 | |
| Clinical signatures | SBP (mmHg) | SFA (%E) → PUFA (%E) | −1.00 mmHg (−2.88, +0.90) | 0.300 | 0.791 |
| SBP (mmHg) | SFA (%E) → MUFA (%E) | −0.57 mmHg (−1.88, +0.75) | 0.396 | 0.791 | |
| Glucose (mg/dL) | SFA (%E) → PUFA (%E) | +0.40 mg/dL (−1.58, +2.41) | 0.696 | 0.827 | |
| Glucose (mg/dL) | SFA (%E) → MUFA (%E) | +0.23 mg/dL (−1.46, +1.96) | 0.788 | 0.841 | |
| WHtR | SFA (%E) → MUFA (%E) | −0.6% (−2.5, +1.4) | 0.583 | 0.827 | |
| WHtR | SFA (%E) → PUFA (%E) | −0.7% (−4.2, +3.0) | 0.711 | 0.827 | |
| Composite signatures | Life’s Essential 8 (SD) | SFA (%E) → PUFA (%E) | +0.11 SD (−0.13, +0.36) | 0.386 | 0.791 |
| Life’s Essential 8 (SD) | SFA (%E) → MUFA (%E) | +0.06 SD (−0.12, +0.25) | 0.509 | 0.827 | |
| WCRF (SD) | SFA (%E) → PUFA (%E) | +0.09 SD (−0.08, +0.26) | 0.303 | 0.791 | |
| WCRF (SD) | SFA (%E) → MUFA (%E) | +0.02 SD (−0.10, +0.14) | 0.724 | 0.827 | |
| cCMRS (SD) | SFA (%E) → MUFA (%E) | −0.03 SD (−0.17, +0.11) | 0.667 | 0.827 | |
| cCMRS (SD) | SFA (%E) → PUFA (%E) | −0.01 SD (−0.20, +0.19) | 0.929 | 0.929 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gurazi, V.; Zejnelhoxha, S.; Sulenji, M.; Koxha, L.; Protoduari, H.; Arapi, K.; Rexha, E.; Gjata, F.; Spahiu, O.; Llanaj, E. Cardiometabolic Phenotypes and Dietary Patterns in Albanian University-Enrolled Young Adults: Cross-Sectional Findings from the Nutrition Synergies WHO-Aligned Sentinel Platform. Nutrients 2025, 17, 3395. https://doi.org/10.3390/nu17213395
Gurazi V, Zejnelhoxha S, Sulenji M, Koxha L, Protoduari H, Arapi K, Rexha E, Gjata F, Spahiu O, Llanaj E. Cardiometabolic Phenotypes and Dietary Patterns in Albanian University-Enrolled Young Adults: Cross-Sectional Findings from the Nutrition Synergies WHO-Aligned Sentinel Platform. Nutrients. 2025; 17(21):3395. https://doi.org/10.3390/nu17213395
Chicago/Turabian StyleGurazi, Vilma, Sanije Zejnelhoxha, Megisa Sulenji, Lajza Koxha, Herga Protoduari, Kestjana Arapi, Elma Rexha, Flavia Gjata, Orgesa Spahiu, and Erand Llanaj. 2025. "Cardiometabolic Phenotypes and Dietary Patterns in Albanian University-Enrolled Young Adults: Cross-Sectional Findings from the Nutrition Synergies WHO-Aligned Sentinel Platform" Nutrients 17, no. 21: 3395. https://doi.org/10.3390/nu17213395
APA StyleGurazi, V., Zejnelhoxha, S., Sulenji, M., Koxha, L., Protoduari, H., Arapi, K., Rexha, E., Gjata, F., Spahiu, O., & Llanaj, E. (2025). Cardiometabolic Phenotypes and Dietary Patterns in Albanian University-Enrolled Young Adults: Cross-Sectional Findings from the Nutrition Synergies WHO-Aligned Sentinel Platform. Nutrients, 17(21), 3395. https://doi.org/10.3390/nu17213395









