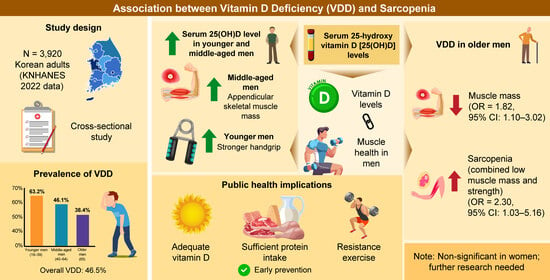
Associations Between Vitamin D Deficiency and Sarcopenia in South Korean Adults: Based on the 2022 Korea National Health and Nutrition Examination Survey
Abstract
1. Introduction
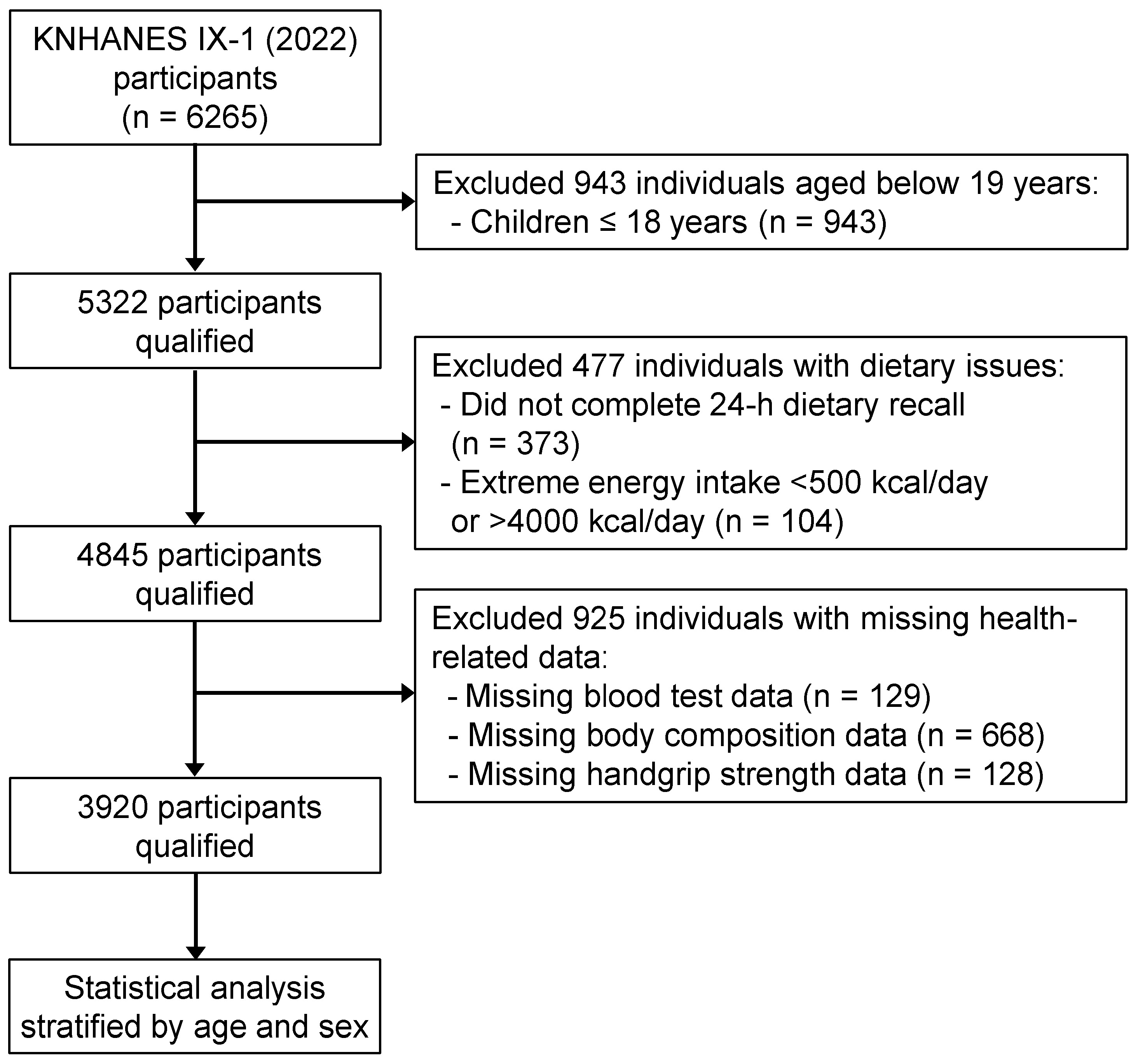
2. Materials and Methods
2.1. Data Source and Participants
2.2. Vitamin D Status, Body Composition, and Handgrip Strength Measures
2.3. Covariate Measures
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| VDR | vitamin D receptor |
| ATP | adenosine triphosphate |
| AI | adequate intake |
| BIA | bioelectrical impedance analysis |
| VDD | vitamin D deficiency |
| ROS | reactive oxygen species |
| 25(OH)D | 25-hydroxyvitamin D3 |
| KNHANES | Korea National Health and Nutrition Examination Survey |
| PTH | parathyroid hormone |
References
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, Y.; Gong, M.; Feng, X.-M.; Yan, Y.-X. Bidirectional association between sarcopenia and diabetes: A prospective cohort study in middle-aged and elderly adults. Clin. Nutr. ESPEN 2025, 66, 556–563. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.M.; Moon, J.S.; Chang, M.C. Prevalence of sarcopenia and its association with diabetes: A meta-analysis of community-dwelling Asian population. Front. Med. 2021, 8, 681232. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zeng, Q.; Zhao, L.; Zhong, Q.; An, Z.; Li, S. Changes in sarcopenia and incident cardiovascular disease in prospective cohorts. BMC Med. 2024, 22, 607. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
- Park, W.T.; Shon, O.-J.; Kim, G.B. Multidisciplinary approach to sarcopenia: A narrative review. Yeungnam Univ. J. Med. 2023, 40, 352–363. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Supriya, R.; Singh, K.P.; Gao, Y.; Li, F.; Dutheil, F.; Baker, J.S. A multifactorial approach for sarcopenia assessment: A literature review. Biology 2021, 10, 1354. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Girgis, C.M.; Mokbel, N.; Cha, K.M.; Houweling, P.J.; Abboud, M.; Fraser, D.R.; Mason, R.S.; Clifton-Bligh, R.J.; Gunton, J.E. The vitamin D receptor (VDR) is expressed in skeletal muscle of male mice and modulates 25-Hydroxyvitamin D (25OHD) uptake in myofibers. Endocrinology 2014, 155, 3227–3237. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, F.; Li, W. Vitamin D and sarcopenia in the senior people: A review of mechanisms and comprehensive prevention and treatment strategies. Ther. Clin. Risk Manag. 2024, 20, 577–595. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Latham, C.M.; Brightwell, C.R.; Keeble, A.R.; Munson, B.D.; Thomas, N.T.; Zagzoog, A.M.; Fry, C.S.; Fry, J.L. Vitamin D pro-motes skeletal muscle regeneration and mitochondrial health. Front. Physiol. 2021, 12, 660498. [Google Scholar] [CrossRef] [PubMed Central]
- Ahn, H.; Kim, S.; Jung, J.; Park, C.Y. Discovering vitamin-D-deficiency-associated factors in Korean adults using KNHANES data based on an integrated analysis of machine learning and statistical techniques. Nutrients 2025, 17, 618. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, K.N.; Lee, J.-S.; Shim, J.-S.; Yoon, M.O.; Lee, H.S. Estimated dietary vitamin D intake and major vitamin D food sources of Koreans: Based on the Korea national health and nutrition examination survey 2016–2019. Nutr. Res. Pract. 2023, 17, 451–463. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhao, S.; Qian, F.; Wan, Z.; Chen, X.; Pan, A.; Liu, G. Vitamin D and major chronic diseases. Trends Endocrinol. Metab. 2024, 35, 1050–1061. [Google Scholar] [CrossRef] [PubMed]
- Argano, C.; Mirarchi, L.; Amodeo, S.; Orlando, V.; Torres, A.; Corrao, S. The role of vitamin D and its molecular bases in insulin resistance, diabetes, metabolic syndrome, and cardiovascular disease: State of the art. Int. J. Mol. Sci. 2023, 24, 15485. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kweon, S.; Kim, Y.; Jang, M.-J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data resource profile: The Korea national health and nutrition examination survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oh, K.; Kim, Y.; Kweon, S.; Kim, S.; Yun, S.; Park, S.; Lee, Y.-K.; Kim, Y.-T.; Park, O.; Jeong, E.K. Korea national health and nutrition examination survey, 20th anniversary: Accomplishments and future directions. Epidemiol. Health 2021, 43, e2021025. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alshahrani, F.; Aljohani, N. Vitamin D: Deficiency, sufficiency and toxicity. Nutrients 2013, 5, 3605–3616. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Basińska-Lewandowska, M.; Lewiński, A.; Horzelski, W.; Skowrońska-Jóźwiak, E. Effect of summer sunshine exposure on vitamin D status in young and middle age poles: Is 30 ng/mL vitamin D cut-off really suitable for the polish population? Int. J. Environ. Res. Public Health 2021, 18, 8116. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, J.; Atkins, A.; Downes, M.; Wei, Z. Vitamin D in diabetes: Uncovering the sunshine hormone’s role in glucose metabolism and beyond. Nutrients 2023, 15, 1997. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Korean Food Composition Database; Rural Development Administration—National Institute of Agricultural Sciences: Jeonju, Republic of Korea, 2021; Volume 9.
- Paddon-Jones, D.; Short, K.R.; Campbell, W.W.; Volpi, E.; Wolfe, R.R. Role of dietary protein in the sarcopenia of aging. Am. J. Clin. Nutr. 2008, 87, 1562S–1566S. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.; Ryu, H.K. Association of low hand grip strength with protein intake in Korean female elderly: Based on the seventh Korea national health and nutrition examination survey (KNHANES VII), 2016–2018. Korean J. Community Nutr. 2020, 25, 226–235. [Google Scholar] [CrossRef]
- Cho, J.M.; Bae, J. Nutritional, physical, and body composition profiles of the Korean sarcopenic population. J. Nutr. Health 2025, 58, 315–331. [Google Scholar] [CrossRef]
- Choi, R.; Cho, S.-E.; Lee, S.G.; Lee, E.H. Recent information on vitamin D deficiency in an adult Korean population visiting local clinics and hospitals. Nutrients 2022, 14, 1978. [Google Scholar] [CrossRef]
- Yang, C.; Dai, Y.; Li, Z.; Peng, Y.; Zhang, L.; Jia, H. Relationship of serum 25-hydroxyvitamin D levels with sarcopenia and body composition in community-dwelling older adults: A paired case-control study. J. Am. Med. Dir. Assoc. 2023, 24, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Minamino, H.; Katsushima, M.; Torii, M.; Yamamoto, W.; Fujita, Y.; Ikeda, K.; Okamura, E.; Murakami, K.; Watanabe, R.; Murata, K.; et al. Serum vitamin D status inversely associates with a prevalence of severe sarcopenia among female patients with rheumatoid arthritis. Sci. Rep. 2021, 11, 20485. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iolascon, G.; Mauro, G.L.; Fiore, P.; Cisari, C.; Benedetti, M.G.; Panella, L.; De Sire, A.; Calafiore, D.; Moretti, A.; Gimigliano, F. Can vitamin D deficiency influence muscle performance in postmenopausal women? A multicentre retrospective study. Eur. J. Phys. Rehabil. Med. 2018, 54, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Roh, S.; Kim, K.-S. Relationship between vitamin D levels and sarcopenia: Insights from a Korean population study. Korean J. Fam. Pr. 2024, 14, 203–210. [Google Scholar] [CrossRef]
- Wei, Y.; He, Q.; Di, Q.; Li, J.; Zhang, J.; Na, L. Individual and joint association of serum 25-hydroxyvitamin D and folate levels with the risk of sarcopenia: A cross-sectional study from the NHANES 2011–2018. Front. Nutr. 2025, 12, 1576705. [Google Scholar] [CrossRef]
- Kim, Y.; Chang, Y.; Ryu, S.; Cho, I.Y.; Kwon, M.-J.; Wild, S.H.; Byrne, C.D. Serum 25-hydroxy vitamin D and the risk of low muscle mass in young and middle-aged Korean adults. Eur. J. Endocrinol. 2022, 186, 477–487. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yu, S.; Ren, B.; Chen, H.; Goltzman, D.; Yan, J.; Miao, D. 1,25-Dihydroxyvitamin D deficiency induces sarcopenia by inducing skeletal muscle cell senescence. Am. J. Transl. Res. 2021, 13, 12638–12649. [Google Scholar] [PubMed] [PubMed Central]
- Sponchiado, I.M.; Limirio, L.S.; de Branco, F.M.S.; de Oliveira, E.P. Sex-dependent association of serum vitamin D with muscle strength in older adults: NHANES 2001–2002. Eur. J. Clin. Nutr. 2024, 78, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Baek, K.H.; Song, K.-H.; Kang, M.I.; Park, C.Y.; Lee, W.Y.; Oh, K.W. Vitamin D deficiency is associated with sarcopenia in older Koreans, regardless of obesity: The fourth Korea national health and nutrition examination surveys (KNHANES IV) 2009. J. Clin. Endocrinol. Metab. 2011, 96, 3250–3256. [Google Scholar] [CrossRef] [PubMed]
- Wierzbicka, A.; Oczkowicz, M. Sex differences in vitamin D metabolism, serum levels and action. Br. J. Nutr. 2022, 128, 2115–2130. [Google Scholar] [CrossRef] [PubMed]
- Bollen, S.E.; Bass, J.J.; Fujita, S.; Wilkinson, D.; Hewison, M.; Atherton, P.J. The Vitamin D/Vitamin D receptor (VDR) axis in muscle atrophy and sarcopenia. Cell. Signal. 2022, 96, 110355. [Google Scholar] [CrossRef] [PubMed]
- Dzik, K.P.; Kaczor, J.J. Mechanisms of vitamin D on skeletal muscle function: Oxidative stress, energy metabolism and anabolic state. Graefe’s Arch. Clin. Exp. Ophthalmol. 2019, 119, 825–839. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bauer, J.M.; Verlaan, S.; Bautmans, I.; Brandt, K.; Donini, L.M.; Maggio, M.; McMurdo, M.E.; Mets, T.; Seal, C.; Wijers, S.L.; et al. Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the PROVIDE study: A randomized, double-blind, placebo-controlled trial. J. Am. Med. Dir. Assoc. 2015, 16, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Widajanti, N.; Hadi, U.; Soelistijo, S.A.; Syakdiyah, N.H.; Rosaudyn, R.; Putra, H.B.P. The effect of vitamin D supplementation to parameter of sarcopenia in elderly people: A systematic review and meta-analysis. Can. Geriatr. J. 2024, 27, 63–75. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gkekas, N.K.; Anagnostis, P.; Paraschou, V.; Stamiris, D.; Dellis, S.; Kenanidis, E.; Potoupnis, M.; Tsiridis, E.; Goulis, D.G. The effect of vitamin D plus protein supplementation on sarcopenia: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2021, 145, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Sha, T.; Wang, Y.; Zhang, Y.; Lane, N.E.; Li, C.; Wei, J.; Zeng, C.; Lei, G. Genetic variants, serum 25-hydroxyvitamin D Levels, and sarcopenia: A Mendelian randomization analysis. JAMA Netw. Open 2023, 6, e2331558. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mądra-Gackowska, K.; Szewczyk-Golec, K.; Gackowski, M.; Hołyńska-Iwan, I.; Parzych, D.; Czuczejko, J.; Graczyk, M.; Husejko, J.; Jabłoński, T.; Kędziora-Kornatowska, K. Selected biochemical, hematological, and immunological blood parameters for the identification of malnutrition in Polish senile inpatients: A cross-sectional study. J. Clin. Med. 2025, 14, 1494. [Google Scholar] [CrossRef]
- Mądra-Gackowska, K.; Szewczyk-Golec, K.; Gackowski, M.; Woźniak, A.; Kędziora-Kornatowska, K. Evaluation of selected parameters of oxidative stress and adipokine levels in hospitalized older patients with diverse nutritional status. Antioxidants 2023, 12, 569. [Google Scholar] [CrossRef] [PubMed]
- Aspell, N.; Laird, E.; Healy, M.; Lawlor, B.; O’Sullivan, M. Vitamin D deficiency is associated with impaired muscle strength and physical performance in community-dwelling older adults: Findings from the English longitudinal study of ageing. Clin. Interv. Aging 2019, 14, 1751–1761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mendes, J.; Santos, A.; Borges, N.; Afonso, C.; Moreira, P.; Padrão, P.; Negrão, R.; Amaral, T.F. Vitamin D status and functional parameters: A cross-sectional study in an older population. PLoS ONE 2018, 13, e0201840. [Google Scholar] [CrossRef] [PubMed]
- Granic, A.; Hill, T.R.; Davies, K.; Jagger, C.; Adamson, A.; Siervo, M.; Kirkwood, T.B.L.; Mathers, J.C.; Sayer, A.A. Vitamin D status, muscle strength and physical performance decline in very old adults: A prospective study. Nutrients 2017, 9, 379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Serum 25(OH)D Level | Unadjusted | Model 1 * | Model 2 † | Model 3 ‡ | ||||
|---|---|---|---|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Younger adults | ||||||||
| Men (n § = 447) | 0.009 (0.000, 0.018) | 0.061 | 0.010 (0.004, 0.016) | 0.002 | 0.006 (0.000, 0.013) | 0.058 | 0.006 (0.000, 0.013) | 0.060 |
| Women (n § = 549) | −0.004 (−0.011, 0.003) | 0.241 | 0.003 (−0.001, 0.007) | 0.204 | 0.003 (−0.001, 0.007) | 0.184 | 0.003 (−0.001, 0.007) | 0.180 |
| Middle-aged adults | ||||||||
| Men (n § = 731) | −0.001 (−0.008, 0.006) | 0.801 | 0.005 (0.001, 0.009) | 0.007 | 0.005 (0.001, 0.009) | 0.007 | 0.005 (0.001, 0.009) | 0.007 |
| Women (n § = 1057) | −0.007 (−0.011, −0.003) | 0.002 | <0.001 (−0.004, 0.004) | 0.981 | <0.001 (−0.004, 0.003) | 0.841 | <0.001 (−0.004, 0.003) | 0.862 |
| Older adults | ||||||||
| Men (n § = 547) | 0.005 (−0.002, 0.011) | 0.141 | 0.003 (0.000, 0.007) | 0.086 | 0.003 (0.000, 0.007) | 0.059 | 0.003 (0.000, 0.007) | 0.079 |
| Women (n § = 589) | −0.009 (−0.014, −0.004) | 0.001 | −0.001 (−0.005, 0.002) | 0.404 | −0.002 (−0.005, 0.001) | 0.284 | −0.002 (−0.005, 0.001) | 0.269 |
| Serum 25(OH)D Level | Unadjusted | Model 1 * | Model 2 † | Model 3 ‡ | ||||
|---|---|---|---|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Younger adults | ||||||||
| Men (n § = 447) | 0.168 (0.064, 0.272) | 0.002 | 0.151 (0.056, 0.246) | 0.002 | 0.099 (0.003, 0.194) | 0.043 | 0.097 (0.001, 0.194) | 0.048 |
| Women (n § = 549) | −0.011 (−0.060, 0.038) | 0.668 | −0.022 (−0.068, 0.024) | 0.351 | −0.018 (−0.065, 0.028) | 0.437 | −0.015 (−0.063, 0.032) | 0.519 |
| Middle-aged adults | ||||||||
| Men (n § = 731) | −0.005 (−0.065, 0.055) | 0.874 | 0.020 (−0.036, 0.076) | 0.475 | 0.017 (−0.041, 0.074) | 0.567 | 0.017 (−0.040, 0.074) | 0.555 |
| Women (n § = 1057) | −0.025 (−0.048, −0.001) | 0.041 | 0.004 (−0.022, 0.029) | 0.784 | −0.002 (−0.027, 0.024) | 0.906 | −0.002 (−0.028, 0.023) | 0.853 |
| Older adults | ||||||||
| Men (n § = 547) | 0.048 (−0.006, 0.102) | 0.081 | 0.029 (−0.020, 0.078) | 0.241 | 0.033 (−0.015, 0.080) | 0.179 | 0.028 (−0.020, 0.076) | 0.251 |
| Women (n § = 589) | 0.017 (−0.016, 0.049) | 0.322 | 0.026 (−0.003, 0.056) | 0.083 | 0.020 (−0.009, 0.048) | 0.171 | 0.018 (−0.010, 0.047) | 0.202 |
| Serum 25(OH)D Level | Unadjusted | Model 1 * | Model 2 † | Model 3 ‡ | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Low muscle mass | ||||||||
| Men | ||||||||
| Normal (n § = 355) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 192) | 1.56 | 1.06, 2.28 | 1.77 | 1.08, 2.90 | 1.50 | 1.07, 3.02 | 1.82 | 1.10, 3.02 |
| Women | ||||||||
| Normal (n § = 430) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 159) | 0.66 | 0.42, 1.04 | 0.80 | 0.45, 1.43 | 0.72 | 0.40, 1.27 | 0.71 | 0.40, 1.28 |
| Low muscle strength | ||||||||
| Men | ||||||||
| Normal (n § = 355) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 192) | 2.05 | 1.15, 3.65 | 1.89 | 1.04, 3.46 | 1.84 | 1.01, 3.37 | 1.80 | 0.99, 3.26 |
| Women | ||||||||
| Normal (n § = 430) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 159) | 1.53 | 0.89, 2.64 | 1.62 | 0.91, 2.88 | 1.39 | 0.75, 2.58 | 1.42 | 0.77, 2.62 |
| Sarcopenia | ||||||||
| Men | ||||||||
| Normal (n § = 355) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 192) | 2.54 | 1.23, 5.25 | 2.58 | 1.18, 5.63 | 2.35 | 1.03, 5.33 | 2.30 | 1.03, 5.16 |
| Women | ||||||||
| Normal (n § = 430) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | ||||
| Vitamin D deficiency (n § = 159) | 1.10 | 0.54, 2.24 | 1.21 | 0.54, 2.69 | 0.93 | 0.40, 2.13 | 0.94 | 0.41, 2.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Kim, M.J. Associations Between Vitamin D Deficiency and Sarcopenia in South Korean Adults: Based on the 2022 Korea National Health and Nutrition Examination Survey. Nutrients 2025, 17, 3292. https://doi.org/10.3390/nu17203292
Shin S, Kim MJ. Associations Between Vitamin D Deficiency and Sarcopenia in South Korean Adults: Based on the 2022 Korea National Health and Nutrition Examination Survey. Nutrients. 2025; 17(20):3292. https://doi.org/10.3390/nu17203292
Chicago/Turabian StyleShin, Sunhye, and Mi Joung Kim. 2025. "Associations Between Vitamin D Deficiency and Sarcopenia in South Korean Adults: Based on the 2022 Korea National Health and Nutrition Examination Survey" Nutrients 17, no. 20: 3292. https://doi.org/10.3390/nu17203292
APA StyleShin, S., & Kim, M. J. (2025). Associations Between Vitamin D Deficiency and Sarcopenia in South Korean Adults: Based on the 2022 Korea National Health and Nutrition Examination Survey. Nutrients, 17(20), 3292. https://doi.org/10.3390/nu17203292