Recalling Perceptions, Emotions, Behaviours, and Changes in Weight Status Among University Students After the Pandemic Experience
Abstract
1. Introduction
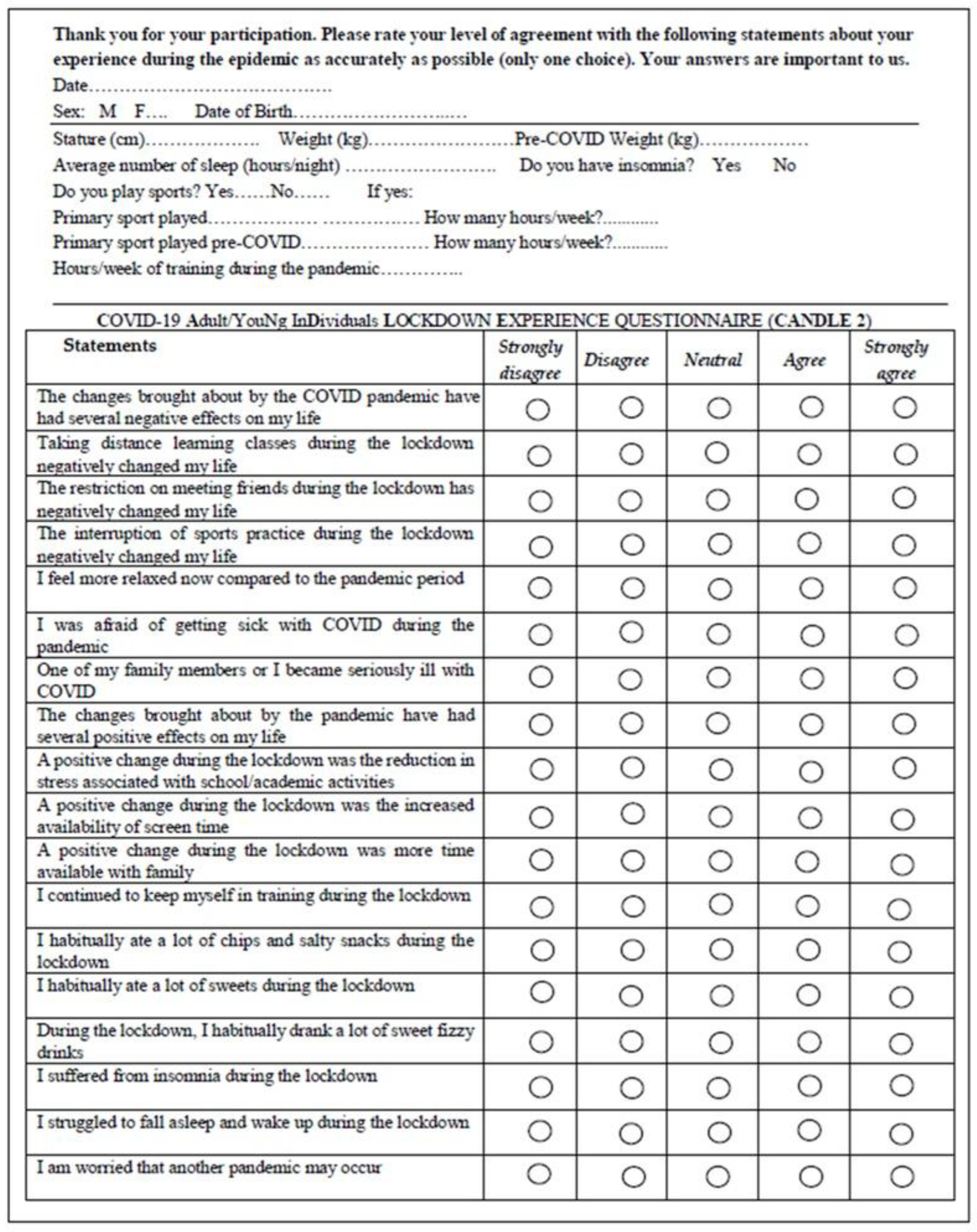
2. Materials and Methods
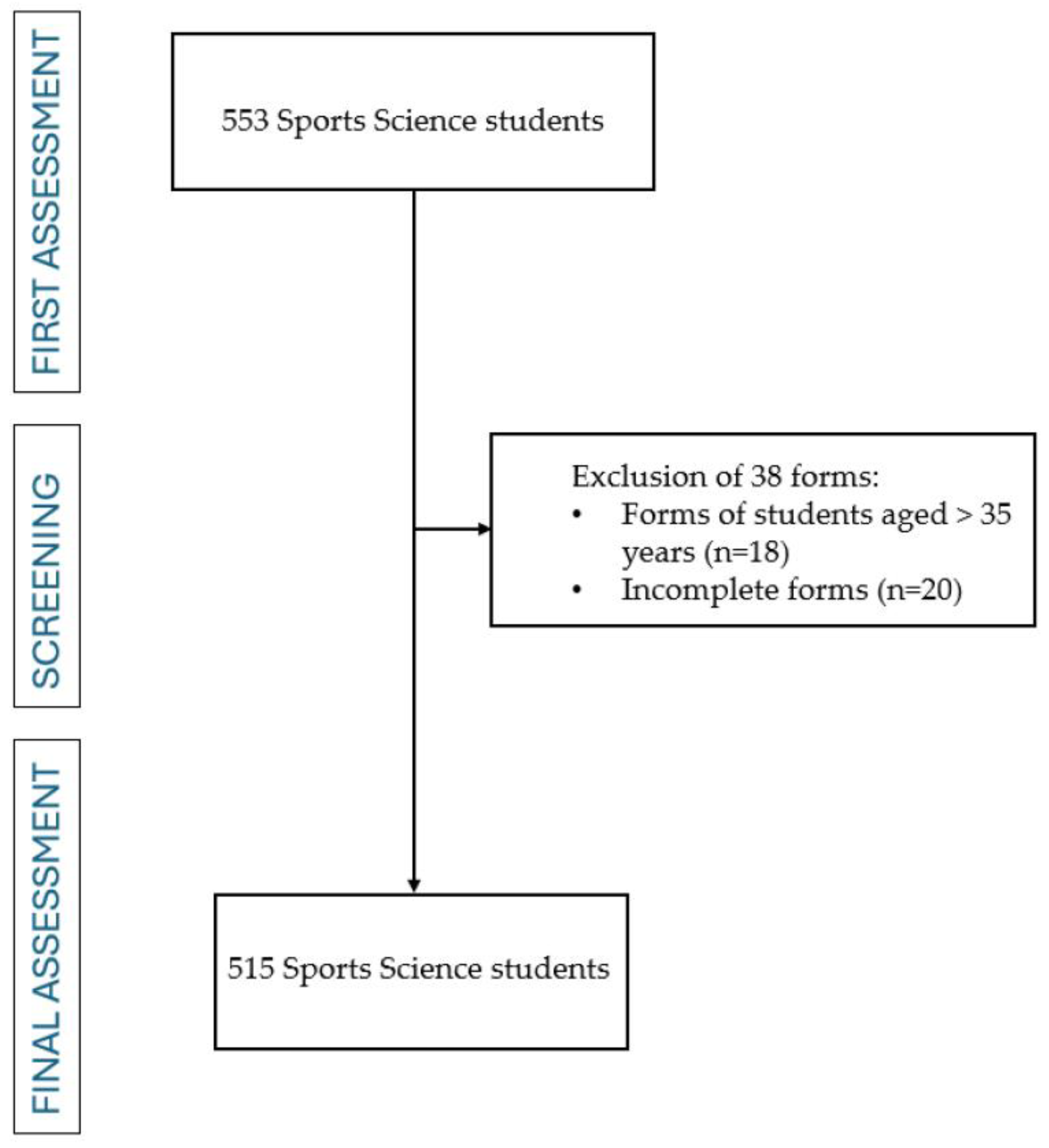
2.1. Research Design, Participants
2.2. Procedures
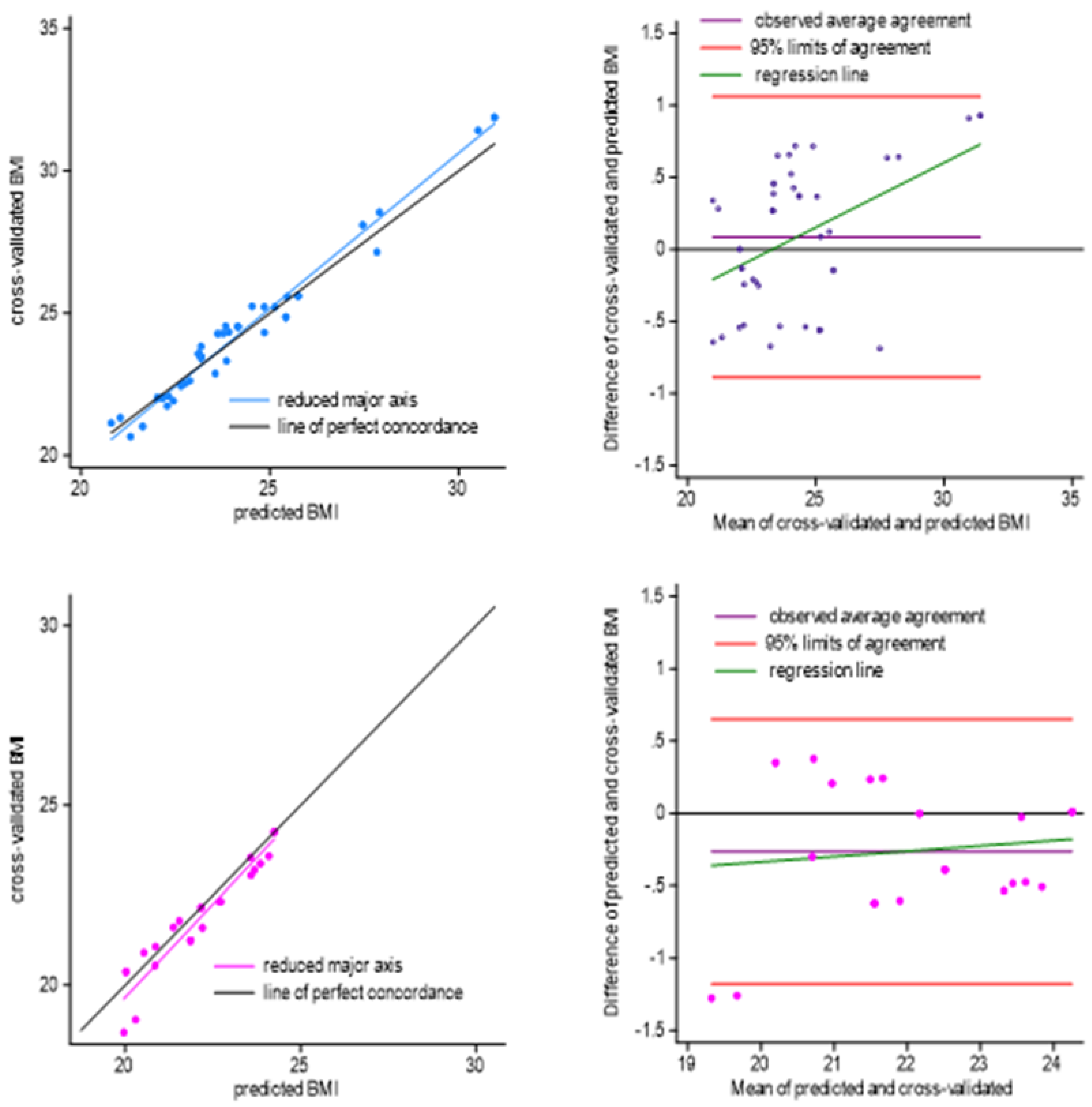
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | COronaVIrus Disease of 2019 |
| PA | Physical Activity |
| CANDLE 2 | COVID-19 Adult/YouNg InDividuals LOCKDOWN EXPERIENCE QUESTIONNAIRE |
| BMI | Body Mass Index |
| df | Degree of freedom |
Appendix A
References
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Podolsky, M.I.; Raquib, R.; Hempstead, K.; Stokes, A.C. Trends in Obesity Care Among US Adults, 2010–2021. Med. Care 2025, 63, 234–240. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Martinez-Ferran, M.; de la Guía-Galipienso, F.; Sanchis-Gomar, F.; Pareja-Galeano, H. Metabolic Impacts of Confinement during the COVID-19 Pandemic Due to Modified Diet and Physical Activity Habits. Nutrients 2020, 12, 1549. [Google Scholar] [CrossRef]
- Akter, T.; Zeba, Z.; Hosen, I.; Al-Mamun, F.; Mamun, M.A. Impact of the COVID-19 pandemic on BMI: Its changes in relation to socio-demographic and physical activity patterns based on a short period. PLoS ONE 2022, 17, e0266024. [Google Scholar] [CrossRef] [PubMed]
- Meade, J. Mental Health Effects of the COVID-19 Pandemic on Children and Adolescents: A Review of the Current Research. Pediatr. Clin. N. Am. 2021, 68, 945–959. [Google Scholar] [CrossRef]
- Zaccagni, L.; Gualdi-Russo, E. Reduced Physical Activity and Increased Weight Status in Children and Adolescents During the COVID-19 Pandemic: A Systematic Review. Children 2025, 12, 178. [Google Scholar] [CrossRef]
- Daniel, M.M.; Liboredo, J.C.; Anastácio, L.R.; Souza, T.C.M.; Oliveira, L.A.; Della Lucia, C.M.; Ferreira, L.G. Incidence and Associated Factors of Weight Gain During the COVID-19 Pandemic. Front. Nutr. 2022, 9, 818632. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the first COVID-19 lockdown 341 on body weight: A combined systematic review and a meta-analysis. Clin. Nutr. 2022, 41, 3046–3054. [Google Scholar] [CrossRef]
- Zaccagni, L.; Toselli, S.; Barbieri, D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6416. [Google Scholar] [CrossRef] [PubMed]
- Gualdi-Russo, E.; Masotti, S.; Rinaldo, N.; De Luca, F.; Toselli, S.; Mazzoni, G.; Mandini, S.; Zaccagni, L. A Longitudinal Study on Body Image Perception and Size among Italian Early Adolescents: Changes over Time and Discrepancies between Genders. Nutrients 2024, 16, 3439. [Google Scholar] [CrossRef] [PubMed]
- Artymiak, P.; Żegleń, M.; Kryst, Ł. Changes in BMI and the prevalence of overweight and obesity in children and adolescents (11–15 years) from Kraków (Poland) during COVID-19 pandemic. Anthropol. Anz. 2025, 82, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef]
- Chopra, S.; Ranjan, P.; Malhotra, A.; Sahu, A.; Dwivedi, S.N.; Baitha, U.; Goel, A.; Kumar, A. Development and validation of a questionnaire to evaluate the impact of COVID-19 on lifestyle-related behaviours: Eating habits, activity and sleep behaviour. Public Health Nutr. 2021, 24, 1275–1290. [Google Scholar] [CrossRef]
- Stratakis, K.; Todorovic, J.; Mirkovic, M.; Nešić, D.; Tesanovic, T.; Terzić-Šupić, Z. Examination of factors associated with physical activity among medical students pre and post-COVID-19 in Serbia. Sci. Rep. 2025, 15, 5791. [Google Scholar] [CrossRef]
- Bélanger, M.; Giroux, M.A.; Registe, P.P.W.; Gallant, F.; Jemaa, S.; Faivre, P.; Saucier, D.; Mekari, S. Adolescent physical activity profiles as determinants of emerging adults’ physical activity. Int. J. Behav. Nutr. Phys. Act. 2025, 22, 35. [Google Scholar] [CrossRef]
- Keating, X.D.; Guan, J.; Piñero, J.C.; Bridges, D.M. A meta-analysis of college students’ physical activity behaviors. J. Am. Coll. Health 2005, 54, 116–125. [Google Scholar] [CrossRef]
- Silva, I.A.; da Silva Santos, A.M.; Maldonado, A.J.; de Moura, H.; Rossi, P.A.Q.; Neves, L.M.; Dos Santos, M.A.P.; Machado, D.C.D.; Ribeiro, S.L.G.; Rossi, F.E. Detraining and retraining in badminton athletes following 1-year COVID-19 pandemic on psychological and physiological response. Sport Sci. Health 2022, 18, 1427–1437. [Google Scholar] [CrossRef]
- Grazioli, R.; Loturco, I.; Baroni, B.M.; Oliveira, G.S.; Saciura, V.; Vanoni, E.; Dias, R.; Veeck, F.; Pinto, R.S.; Cadore, E.L. Coronavirus disease-19 quarantine is more detrimental than traditional off-season on physical conditioning of professional soccer players. J. Strength Cond. Res. 2020, 34, 3316–3320. [Google Scholar] [CrossRef]
- Rosa, B.V.; Maldonado, A.J.; de Araújo, A.O.; Neves, L.M.; Rossi, F.E. Impact of the COVID-19 Lockdown on the Body Composition and Physical Performance of Athletes: A Systematic Review with Meta-Analysis and Meta-Regression. Healthcare 2023, 11, 2319. [Google Scholar] [CrossRef]
- Camera dei Deputati. Le Misure Adottate A Seguito Dell’emergenza Coronavirus (COVID-19) Nell’ambito Dello Sport. 2022. Available online: https://www.camera.it/temiap/documentazione/temi/pdf/1219650.pdf?_1591270897284 (accessed on 26 May 2025).
- Falbová, D.; Beňuš, R.; Sulis, S.; Vorobeľová, L. Effect of COVID-19 pandemic on bioimpedance health indicators in young adults. Am. J. Hum. Biol. 2024, 36, e24110. [Google Scholar] [CrossRef]
- Shpakou, A.; Sokołowska, D.; Krajewska-Kułak, E.; Cybulski, M.; Kowalewska, B.; Korpak, F.; Surkov, S.; Owoc, J.; Krakowiak, J.; Kowalczuk, K. The impact of the COVID-19 pandemic on physical activity, life satisfaction, anxiety, stress perception and coping strategies in student-athletes: A comparison between Belarus and Poland-countries with a different approach of anti-pandemic measures. Front. Public Health 2022, 10, 1052744. [Google Scholar] [CrossRef]
- Ingram, J.; Hand, C.J.; Hijikata, Y.; Maciejewski, G. Exploring the effects of COVID-19 restrictions on wellbeing across different styles of lockdown. Health Psychol. Open 2022, 9, 20551029221099800. [Google Scholar] [CrossRef]
- McLean, C.P.; Anderson, E.R. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 2009, 29, 496–505. [Google Scholar] [CrossRef]
- Tereszko, A.; Dudek, D. Gender differences in mental disorders. Neuropsychiatr. Neuropsychol. 2017, 12, 162–169. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Cebrino, J.; Portero de la Cruz, S. Psychological impact of COVID-19 and determinants among Spanish university students. Front. Public Health 2023, 11, 1252849. [Google Scholar] [CrossRef]
- Runacres, A.; Mackintosh, K.A.; Knight, R.L.; Sheeran, L.; Thatcher, R.; Shelley, J.; McNarry, M.A. Impact of the COVID-19 Pandemic on Sedentary Time and Behaviour in Children and Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11286. [Google Scholar] [CrossRef]
- Solmi, M.; Thompson, T.; Estradé, A.; Agorastos, A.; Radua, J.; Cortese, S.; Dragioti, E.; Vancampfort, D.; Thygesen, L.C.; Aschauer, H.; et al. Global and risk-group stratified well-being and mental health during the COVID-19 pandemic in adults: Results from the international COH-FIT Study. Psychiatry Res. 2024, 342, 115972. [Google Scholar] [CrossRef]
- Aksunger, N.; Vernot, C.; Littman, R.; Voors, M.; Meriggi, N.F.; Abajobir, A.; Beber, B.; Dai, K.; Egger, D.; Islam, A.; et al. COVID-19 and mental health in 8 low- and middle-income countries: A prospective cohort study. PLoS Med. 2023, 20, e1004081. [Google Scholar] [CrossRef]
- Kinoshita, S.; Cortright, K.; Crawford, A.; Mizuno, Y.; Yoshida, K.; Hilty, D.; Guinart, D.; Torous, J.; Correll, C.U.; Castle, D.J.; et al. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions’ approaches to an evolving healthcare landscape. Psychol. Med. 2022, 52, 2606–2613. [Google Scholar] [CrossRef]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef]
- Luo, Y.; Pang, L.; Guo, C.; Zhang, L.; Zheng, X. Association of Urbanicity with Schizophrenia and Related Mortality in China: Association de l’urbanicité avec la schizophrénie et la mortalité qui y est reliée en Chine. Can. J. Psychiatry 2021, 66, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Peter, N.; Tonia, M.T.; Holloway, M.A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef] [PubMed]
- Ronca, D.B.; Mesquita, L.O.; Oliveira, D.; Figueiredo, A.C.M.G.; Wen, J.; Song, M.; de Carvalho, K.M.B. Excess weight is associated with neurological and neuropsychiatric symptoms in post-COVID-19 condition: A systematic review and meta-analysis. PLoS ONE 2025, 20, e0314892. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, J.; Seto, S.; Fukuda, Y.; Funakoshi, S.; Amae, S.; Onobe, J.; Izumi, S.; Ito, K.; Imamura, F. Mental Health and Physical Activity among Children and Adolescents during the COVID-19 Pandemic. Tohoku J. Exp. Med. 2021, 253, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Zaccagni, L.; De Luca, F.; Rinaldo, N.; Mazzoni, G.; Mandini, S.; Gualdi-Russo, E. The COVID-19 Experience in Adolescents: Emotional and Behavioral Recall at the End of the Pandemic. Diseases 2024, 12, 116. [Google Scholar] [CrossRef]
- Beisland, E.G.; Gjeilo, K.H.; Andersen, J.R.; Bratås, O.; Bø, B.; Haraldstad, K.; Hjelmeland, I.H.H.; Iversen, M.M.; Løyland, B.; Norekvål, T.M.; et al. Quality of life and fear of COVID-19 in 2600 baccalaureate nursing students at five universities: A cross-sectional study. Health-Relat. Qual. Life 2021, 19, 198. [Google Scholar] [CrossRef]
- Flølo, T.N.; Gjeilo, K.H.; Andersen, J.R.; Haraldstad, K.; Hjelmeland, I.H.H.; Iversen, M.M.; Løyland, B.; Norekvål, T.M.; Riiser, K.; Rohde, G.; et al. The impact of educational concerns and satisfaction on baccalaureate nursing students’ distress and quality of life during the COVID-19 pandemic; a cross-sectional study. BMC Nurs. 2022, 21, 185. [Google Scholar] [CrossRef]
- Rosenblum, H.G.; Segaloff, H.E.; Cole, D.; Lee, C.C.; Currie, D.W.; Abedi, G.R.; Remington, P.L.; Kelly, G.P.; Pitts, C.; Langolf, K.; et al. Behaviors and attitudes of college students during an academic semester at two Wisconsin universities during the COVID-19 pandemic. J. Am. Coll. Health 2024, 72, 1450–1457. [Google Scholar] [CrossRef]
- Ladouceur, C.D. COVID-19 Adolescent Symptom & Psychological Experience (CASPE) Questionnaire. 2020. Available online: https://www.phenxtoolkit.org/toolkit_content/PDF/CASPE_Parent_Emotional.pdf (accessed on 3 April 2025).
- CRISIS. The Coronavirus Health Impact Survey. Available online: http://www.crisissurvey.org/ (accessed on 3 April 2025).
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Tamaki, T.; Nozawa, W.; Kitsuki, A. How did you perceive the lifestyle changes caused by the COVID-19 pandemic? Humanit. Soc. Sci. Commun. 2024, 11, 70. [Google Scholar] [CrossRef]
- Andrade, C. Sample Size and its Importance in Research. Indian J. Psychol. Med. 2020, 42, 102–103. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.I. A concordance correlation coefficient to evaluate reproducibility. Biometrics 1989, 45, 255–268. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Gemignani, A.; Cipriani, E.; Miccoli, M.; Ciacchini, R.; Cancemi, C.; Menicucci, D.; Montiel, C.B.; Piarulli, A.; Conversano, C. The Hidden Impact of COVID-19 on Memory: Disclosing Subjective Complaints. Clin. Neuropsychiatry 2023, 20, 495–504. [Google Scholar] [CrossRef]
- Reed, A.E.; Chan, L.; Mikels, J.A. Meta-analysis of the age-related positivity effect: Age differences in preferences for positive over negative information. Psychol. Aging 2014, 29, 1–15. [Google Scholar] [CrossRef]
- Aizpurua, A.; Migueles, M.; Aranberri, A. Prospective Memory and Positivity Bias in the COVID-19 Health Crisis: The Effects of Aging. Front. Psychol. 2021, 12, 666977. [Google Scholar] [CrossRef]
- Schacter, D.L.; Guerin, S.A.; Jacques, P. Memory distortion: An adaptive perspective. Trends Cogn. Sci. 2011, 15, 467–474. [Google Scholar] [CrossRef]
- Fayyaz, K.; Bataineh, M.F.; Ali, H.I.; Al-Nawaiseh, A.M.; Al-Rifai’, R.H.; Shahbaz, H.M. Validity of Measured vs. Self-Reported Weight and Height and Practical Considerations for Enhancing Reliability in Clinical and Epidemiological Studies: A Systematic Review. Nutrients 2024, 16, 1704. [Google Scholar] [CrossRef]
- Pietrobelli, A.; Pecoraro, L.; Ferruzzi, A.; Heo, M.; Faith, M.; Zoller, T.; Antoniazzi, F.; Piacentini, G.; Fearnbach, S.N.; Heymsfield, S.B. Effects of COVID-19 Lockdown on Lifestyle Behaviors in Children with Obesity Living in Verona, Italy: A Longitudinal Study. Obesity 2020, 28, 1382–1385. [Google Scholar] [CrossRef]
- Wang, Y.; Bi, C.; Liu, H.; Lin, H.; Cai, R.; Zhang, J. Association of sugar-sweetened beverage consumption with psychological symptoms among Chinese university students during the COVID-19 pandemic. Front. Psychol. 2022, 13, 1024946. [Google Scholar] [CrossRef] [PubMed]
- McAtamney, K.; Mantzios, M.; Egan, H.; Wallis, D.J. Emotional eating during COVID-19 in the United Kingdom: Exploring the roles of alexithymia and emotion dysregulation. Appetite 2021, 161, 105120. [Google Scholar] [CrossRef]
- Moore, E.W.G.; Petrie, T.A.; Slavin, L.E. College Student-athletes’ COVID-19 Worry and Psychological Distress Differed by Gender, Race, and Exposure to COVID-19-related Events. J. Adolesc. Health 2022, 70, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Falbová, D.; Kovalčíková, V.; Beňuš, R.; Vorobeľová, L. Long-term consequences of COVID-19 on mental and physical health in young adults. Cent. Eur. J. Public Health 2024, 32, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Sulis, S.; Falbová, D.; Hozáková, A.; Vorobeľová, L. Sex-Specific Interrelationships of Sleeping and Nutritional Habits with Somatic Health Indicators in Young Adults; Physical Activity, Eating Habits and Sleep During Social Isolation: From Young Adult to Elderly. Bratisl. Med. J. 2025, 126, 2410–2425. [Google Scholar] [CrossRef]
- Miskulin, I.; Candrlic, S.; Dumic, J.; Fotez, I.; Britvic, P.P.; Dumic, L.; Candrlic, M.; Kovacevic, J.; Simic, I.K.; Miskulin, M. The relationship between sleep quality and emotional eating during the pandemic in Croatian adults. Eur. J. Public Health 2024, 34 (Suppl. 3), ckae144.1730. [Google Scholar] [CrossRef]
- Ogilvie, R.P.; Lutsey, P.L.; Widome, R.; Laska, M.N.; Larson, N.; Neumark-Sztainer, D. Sleep indices and eating behaviours in young adults: Findings from Project EAT. Public Health Nutr. 2018, 21, 689–701. [Google Scholar] [CrossRef]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B.; Coca, A. Physical Activity Change during COVID-19 Confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- Bertocchi, L.; Vecchio, R.; Sorbello, S.; Correale, L.; Gentile, L.; Buzzachera, C.; Gaeta, M.; Odone, A. Impact of the COVID-19 pandemic on physical activity among university students in Pavia, Northern Italy. Acta Biomed. 2021, 92, e2021443. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Wiium, N.; Säfvenbom, R. Participation in Organized Sports and Self-Organized Physical Activity: Associations with Developmental Factors. Int. J. Environ. Res. Public Health 2019, 16, 585. [Google Scholar] [CrossRef]
| Statements |
|---|
| S1. The changes brought about by the COVID pandemic have had several negative effects on my life. |
| S2. Taking distance learning classes during the lockdown negatively changed my life. |
| S3. The restriction on meeting friends during the lockdown has negatively changed my life. |
| S4. The interruption of sports practice during the lockdown negatively changed my life. |
| S5. I feel more relaxed now compared to the pandemic period. |
| S6. I was afraid of getting sick with COVID during the pandemic. |
| S7. One of my family members or I became seriously ill with COVID. |
| S8. The changes brought about by the pandemic have had several positive effects on my life. |
| S9. A positive change during the lockdown was the reduction in stress associated with school/academic activities. |
| S10. A positive change during the lockdown was the increased availability of screen time. |
| S11. A positive change during the lockdown was more time available with family. |
| S12. I continued to keep myself in training during the lockdown. |
| S13. I habitually ate a lot of chips and salty snacks during the lockdown. |
| S14. I habitually ate a lot of sweets during the lockdown. |
| S15. During the lockdown, I habitually drank a lot of sweet fizzy drinks. |
| S16. I suffered from insomnia during the lockdown. |
| S17. I struggled to fall asleep and wake up during the lockdown. |
| S18. I am worried that another pandemic may occur. |
| Statement | Correlation Value | p-Value |
|---|---|---|
| S1 | 0.89 | <0.001 |
| S2 | 0.97 | <0.001 |
| S3 | 0.93 | <0.001 |
| S4 | 0.94 | <0.001 |
| S5 | 0.93 | <0.001 |
| S6 | 0.82 | <0.001 |
| S7 | 0.78 | <0.001 |
| S8 | 0.95 | <0.001 |
| S9 | 0.84 | <0.001 |
| S10 | 0.93 | <0.001 |
| S11 | 0.93 | <0.001 |
| S12 | 0.82 | <0.001 |
| S13 | 0.85 | <0.001 |
| S14 | 0.97 | <0.001 |
| S15 | 0.80 | <0.001 |
| S16 | 0.97 | <0.001 |
| S17 | 0.91 | <0.001 |
| S18 | 0.90 | <0.001 |
| Variables | Males | Females | F(1, 514) χ2(1) | p-Value | ||
|---|---|---|---|---|---|---|
| Age (years) | 23.06 | 2.01 | 23.00 | 1.61 | 0.11 | 0.744 a |
| Anthropometric traits | ||||||
| Weight (kg) | 76.03 | 9.13 | 58.54 | 8.25 | 380.26 | <0.001 a |
| Stature (cm) | 178.82 | 6.82 | 164.53 | 6.40 | 449.66 | <0.001 a |
| BMI (kg/m2) | 23.77 | 2.43 | 21.63 | 2.72 | 71.20 | <0.001 a |
| Pre-COVID Weight (kg) | 72.79 | 10.07 | 57.64 | 7.89 | 234.16 | <0.001 a |
| Pre-COVID BMI (kg/m2) | 22.70 | 2.84 | 21.32 | 2.54 | 22.97 | <0.001 a |
| Weight change (kg) | 3.49 | 7.23 | 0.76 | 4.55 | 15.78 | <0.001 a |
| Sports participation | ||||||
| Actual sports practice (%) | 92.3 | 86.0 | 4.13 | 0.030 b | ||
| Actual sport amount (h/week) | 7.5 | 3.8 | 6.5 | 4.0 | 10.12 | 0.002 a |
| PA during the COVID (h/week) | 5.7 | 4.1 | 5.4 | 4.3 | 0.63 | 0.429 a |
| Pre-COVID sport amount (h/week) | 8.4 | 8.0 | 8.0 | 5.5 | 0.11 | 0.743 a |
| Sleep duration and disorders | ||||||
| Occurrence of insomnia (%) | 9.8 | 16.9 | 5.32 | 0.025 b | ||
| Sleep duration (hours/night) | 7.46 | 5.02 | 7.33 | 0.90 | 1.54 | 0.215 a |
| Weight Status | Males | p-Value | Females | p-Value | ||
|---|---|---|---|---|---|---|
| Pre-COVID % | Current % | Pre-COVID % | Current % | |||
| Underweight | 5.3 | 0.8 | <0.001 | 8.7 | 8.2 | 0.969 |
| Normal weight | 76.9 | 74.3 | 82.5 | 80.6 | ||
| Overweight | 16.6 | 23.0 | 8.7 | 10.4 | ||
| Obese | 1.1 | 1.9 | 0.0 | 0.7 | ||
| Statements | Males | Females | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| S1 | 3.7 | 20.6 | 37.2 | 27.2 | 11.1 | 8.1 | 15.4 | 33.8 | 33.8 | 8.8 | 0.1018 |
| S2 | 8.2 | 23.2 | 34.3 | 24.8 | 9.5 | 8.8 | 29.4 | 24.3 | 27.69 | 9.6 | 0.2709 |
| S3 | 4.7 | 10.6 | 25.1 | 41.4 | 18.2 | 5.1 | 15.4 | 22.8 | 37.5 | 19.1 | 0.6112 |
| S4 | 3.7 | 9.8 | 16.4 | 41.7 | 28.5 | 4.4 | 16.2 | 22.1 | 37.5 | 19.9 | 0.0521 |
| S5 | 5.5 | 19.0 | 37.2 | 26.9 | 11.3 | 4.4 | 28.7 | 28.7 | 27.2 | 11.0 | 0.1533 |
| S6 | 12.1 | 24.8 | 24.3 | 29.8 | 9.0 | 8.8 | 23.5 | 16.2 | 32.4 | 19.1 | 0.0110 |
| S7 | 23.5 | 43.0 | 8.7 | 19.8 | 5.0 | 18.4 | 42.6 | 11.8 | 18.4 | 8.8 | 0.3219 |
| S8 | 7.7 | 19.3 | 44.1 | 25.9 | 3.2 | 5.9 | 26.5 | 40.4 | 23.5 | 3.7 | 0.4790 |
| S9 | 6.1 | 14.0 | 26.69 | 39.3 | 13.7 | 7.4 | 24.3 | 16.9 | 34.6 | 16.9 | 0.0173 |
| S10 | 14.0 | 34.0 | 25.6 | 19.5 | 6.9 | 22.8 | 46.3 | 22.1 | 7.4 | 1.5 | 0.0001 |
| S11 | 2.4 | 4.5 | 19.3 | 49.1 | 24.8 | 0.7 | 5.9 | 14.0 | 47.8 | 31.6 | 0.2735 |
| S12 | 5.5 | 11.1 | 9.2 | 45.9 | 28.2 | 0.7 | 12.5 | 9.6 | 47.8 | 29.4 | 0.2208 |
| S13 | 16.9 | 40.4 | 22.4 | 16.4 | 4.0 | 22.1 | 41.9 | 18.4 | 16.2 | 1.5 | 0.3835 |
| S14 | 16.9 | 36.7 | 26.1 | 16.9 | 3.4 | 18.4 | 38.2 | 18.4 | 24.9 | 0.7 | 0.0828 |
| S15 | 21.4 | 43.0 | 20.3 | 12.7 | 2.6 | 32.4 | 44.9 | 16.9 | 4.4 | 1.5 | 0.0126 |
| S16 | 24.3 | 46.2 | 12.4 | 12.4 | 4.7 | 15.4 | 44.1 | 16.2 | 20.6 | 3.7 | 0.0481 |
| S17 | 20.8 | 43.3 | 12.9 | 17.7 | 5.3 | 12.5 | 42.2 | 14.7 | 25.0 | 6.6 | 0.1290 |
| S18 | 13.8 | 23.2 | 37.2 | 20.8 | 5.5 | 3.7 | 16.2 | 33.1 | 36.0 | 11.0 | <0.0001 |
| Predictor Variables | Males | Females | ||||
|---|---|---|---|---|---|---|
| β | p-Value | VIF | β | p-Value | VIF | |
| Weight change | 0.727 | <0.001 | 1.407 | 0.469 | <0.001 | 1.041 |
| S4 | 0.070 | 0.039 | 1.006 | |||
| S7 | −0.089 | 0.009 | 1.007 | −0.132 | 0.026 | 1.024 |
| S11 | 0.130 | 0.030 | 1.053 | |||
| Weight status pre-COVID * | ||||||
| −0.666 | <0.001 | 1.375 | |||
| −0.449 | <0.001 | 1.680 | −0.161 | 0.011 | 1.153 |
| 0.258 | <0.001 | 1.515 | 0.719 | <0.001 | 1.139 |
| R2 | 0.643 | 0.660 | ||||
| R2 adjusted | 0.636 | 0.643 | ||||
| p-value | <0.001 | <0.001 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaccagni, L.; Toselli, S.; Gualdi-Russo, E. Recalling Perceptions, Emotions, Behaviours, and Changes in Weight Status Among University Students After the Pandemic Experience. Nutrients 2025, 17, 3132. https://doi.org/10.3390/nu17193132
Zaccagni L, Toselli S, Gualdi-Russo E. Recalling Perceptions, Emotions, Behaviours, and Changes in Weight Status Among University Students After the Pandemic Experience. Nutrients. 2025; 17(19):3132. https://doi.org/10.3390/nu17193132
Chicago/Turabian StyleZaccagni, Luciana, Stefania Toselli, and Emanuela Gualdi-Russo. 2025. "Recalling Perceptions, Emotions, Behaviours, and Changes in Weight Status Among University Students After the Pandemic Experience" Nutrients 17, no. 19: 3132. https://doi.org/10.3390/nu17193132
APA StyleZaccagni, L., Toselli, S., & Gualdi-Russo, E. (2025). Recalling Perceptions, Emotions, Behaviours, and Changes in Weight Status Among University Students After the Pandemic Experience. Nutrients, 17(19), 3132. https://doi.org/10.3390/nu17193132








