Association Between Multi-Dimensional Sleep Health and Breakfast Skipping in Japanese High School Students
Abstract
1. Introduction
2. Materials and Methods
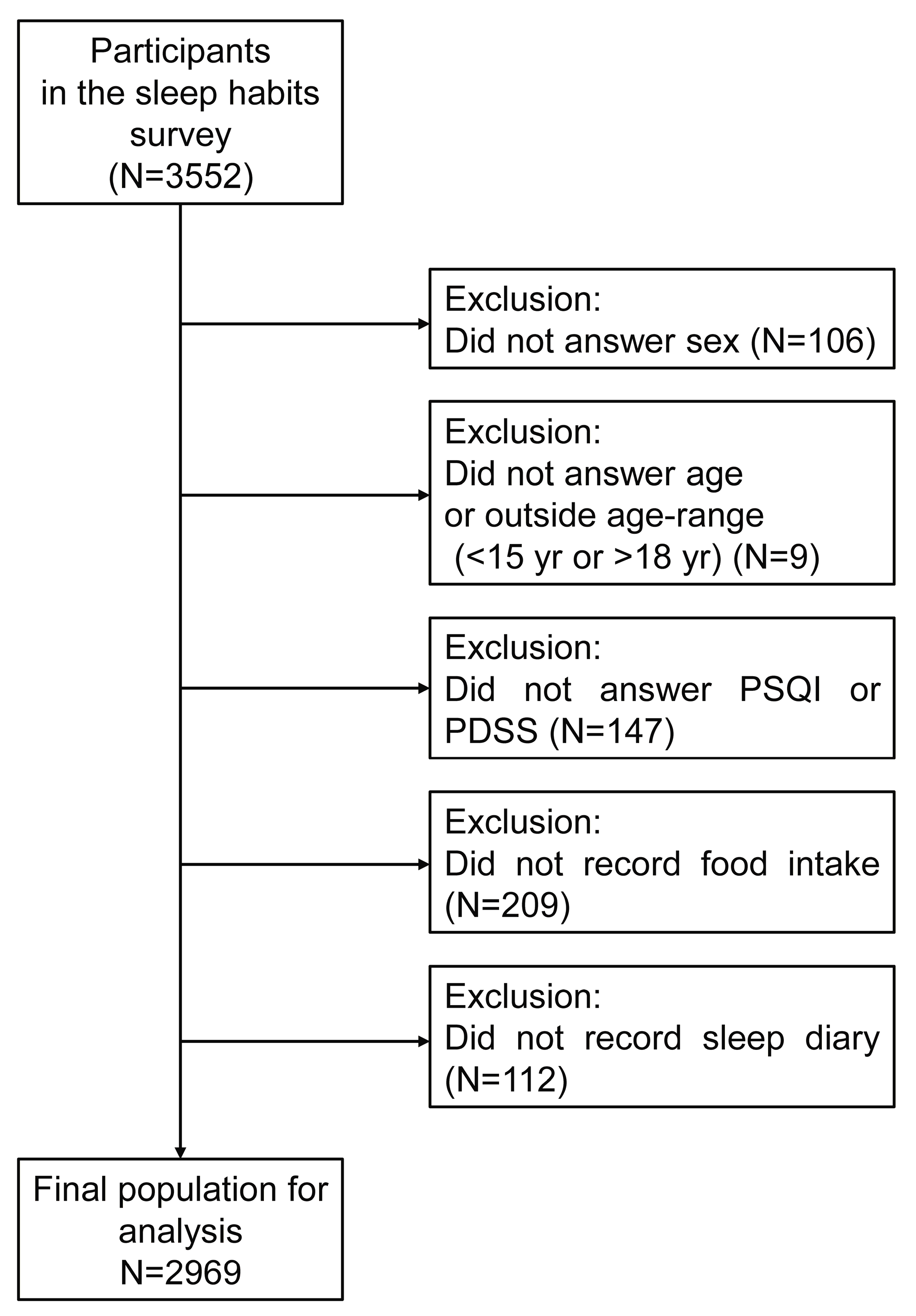
2.1. Participants
2.2. Questionnaire
2.3. Sleep Diary
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
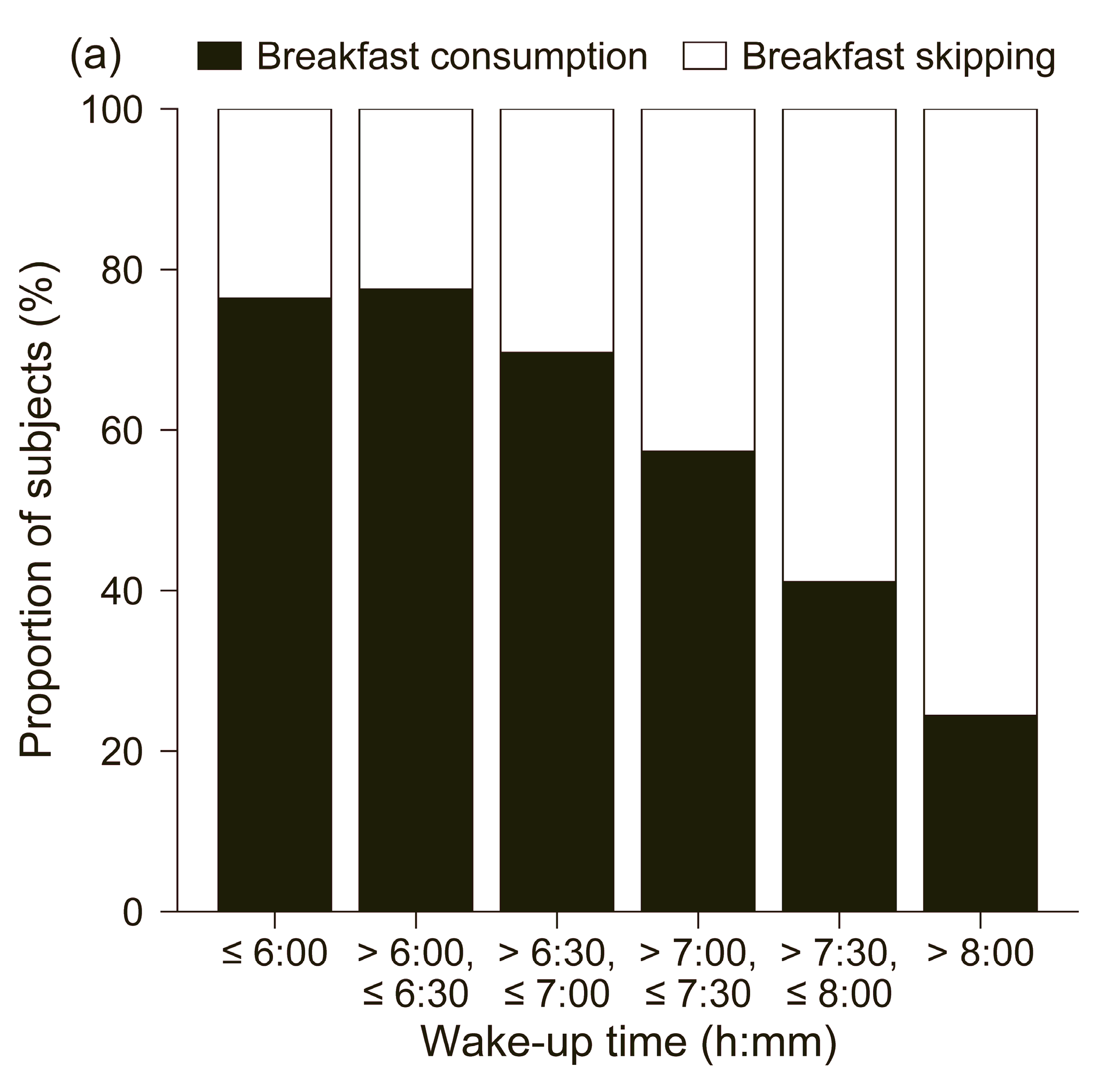
3.2. Relationship Between Breakfast Skipping Rate and Dimensions of Sleep Health
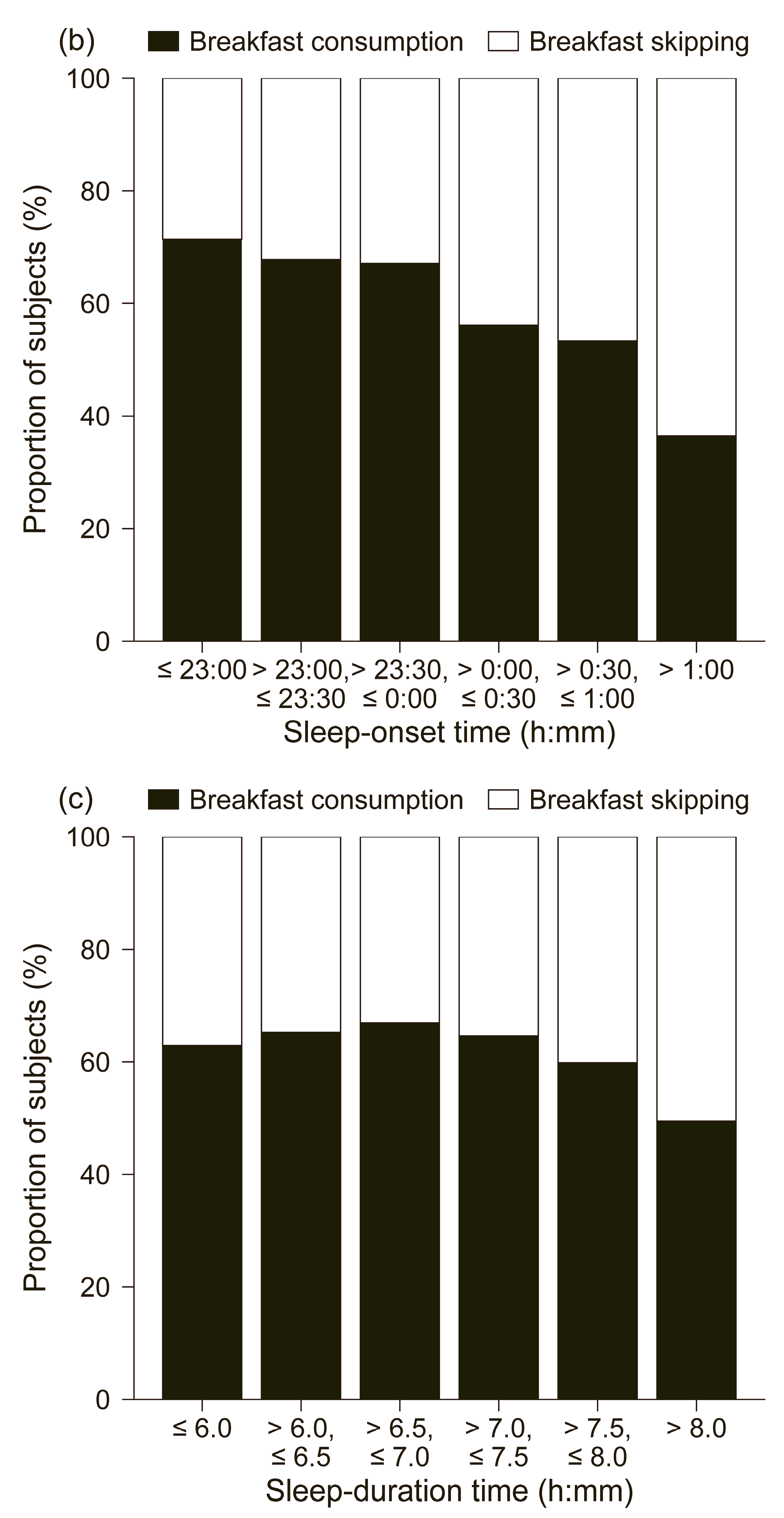
3.3. Interrelationships Between Dimensions of Sleep Health
3.4. Identifying Sleep Health Indicators Associated with Breakfast Skipping Using Multivariable Logistic Regression Analysis
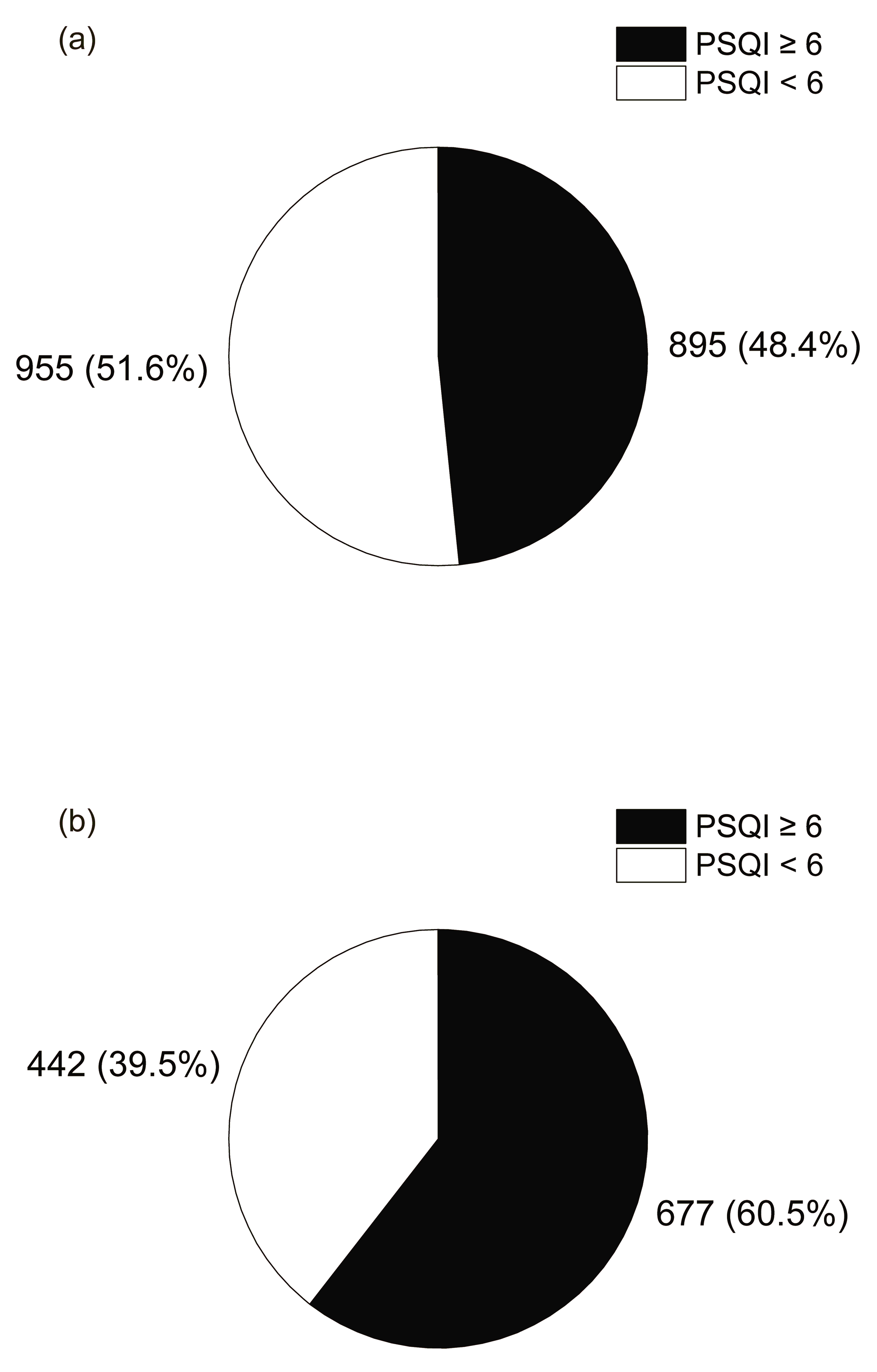
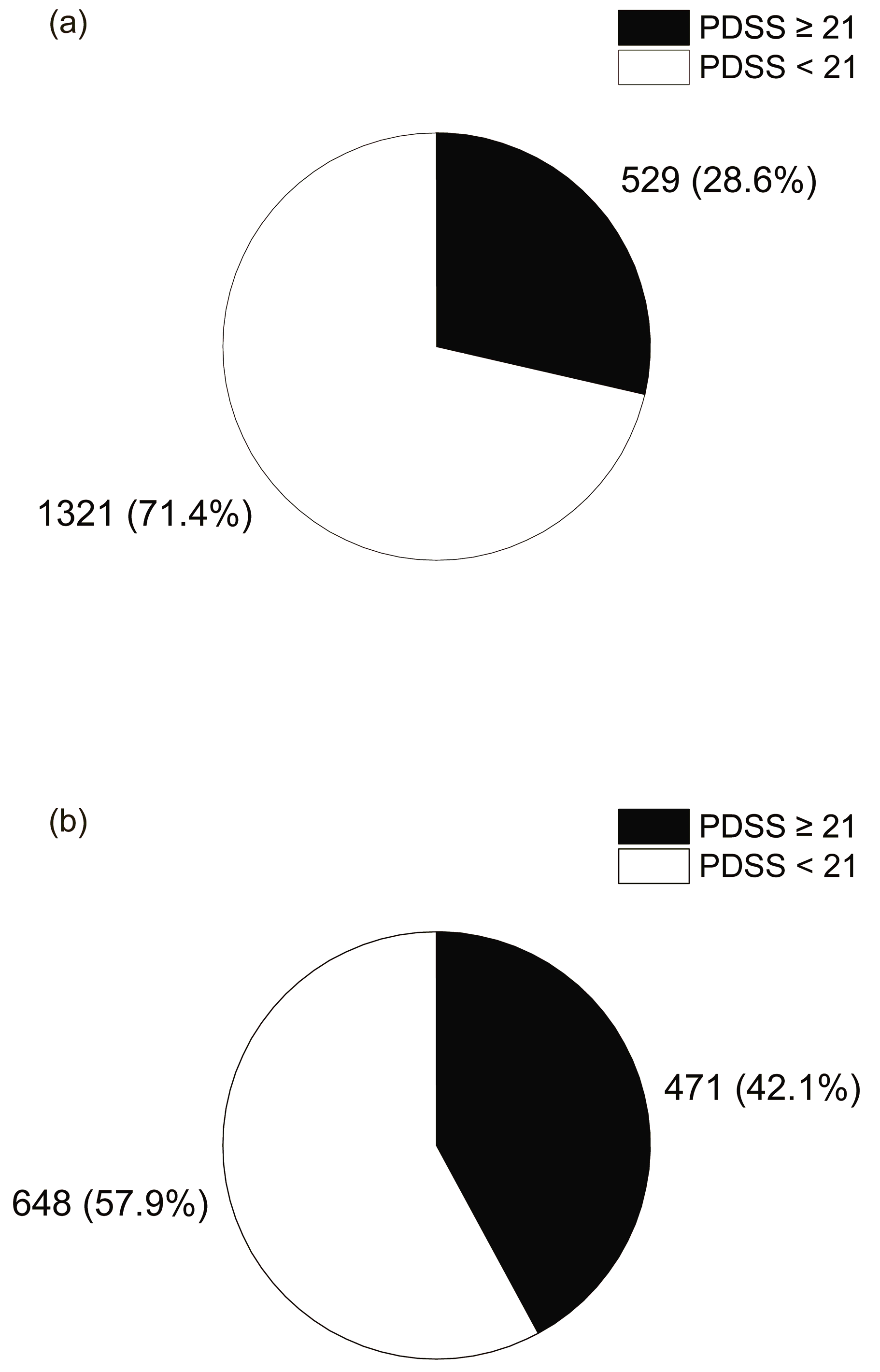
3.5. Association Between PSQI, PDSS and Breakfast Skipping
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sincovich, A.; Sechague Monroy, N.; Smithers, L.G.; Brushe, M.; Boulton, Z.; Rozario, T.; Gregory, T. Breakfast Skipping and Academic Achievement at 8–16 Years: A Population Study in South Australia. Public Health Nutr. 2025, 28, e28. [Google Scholar] [CrossRef] [PubMed]
- Miyamura, K.; Nawa, N.; Isumi, A.; Doi, S.; Ochi, M.; Fujiwara, T. Association between Skipping Breakfast and Prediabetes among Adolescence in Japan: Results from A-CHILD Study. Front. Endocrinol. 2023, 14, 1051592. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhang, X.; Du, W.; Fan, L.; Zhang, F. Association of Insufficient Sleep and Skipping Breakfast with Overweight/Obesity in Children and Adolescents: Findings from a Cross-Sectional Provincial Surveillance Project in Jiangsu. Pediatr. Obes. 2022, 17, e12950. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhu, H.; Lu, Q.; Ye, W.; Huang, T.; Li, Y.; Li, B.; Wu, Y.; Wang, P.; Chen, T.; et al. Sleep Features and the Risk of Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Ann. Med. 2025, 57, 2447422. [Google Scholar] [CrossRef] [PubMed]
- Hovdenak, I.M.; Helleve, A.; Wolden, I.E.; Bere, E. Socioeconomic Inequality in Breakfast Skipping among Norwegian Adolescents. Nutr. J. 2024, 23, 94. [Google Scholar] [CrossRef] [PubMed]
- Sliwa, S.A.; Merlo, C.L.; McKinnon, I.I.; Self, J.L.; Kissler, C.J.; Saelee, R.; Rasberry, C.N. Skipping Breakfast and Academic Grades, Persistent Feelings of Sadness or Hopelessness, and School Connectedness Among High School Students—Youth Risk Behavior Survey, United States, 2023. MMWR Suppl. 2024, 73, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J. Clin. Sleep Med. 2016, 12, 1549–1561. [Google Scholar] [CrossRef] [PubMed]
- Gwin, J.A.; Leidy, H.J. Breakfast Consumption Augments Appetite, Eating Behavior, and Exploratory Markers of Sleep Quality Compared with Skipping Breakfast in Healthy Young Adults. Curr. Dev. Nutr. 2018, 2, nzy074. [Google Scholar] [CrossRef] [PubMed]
- Sasawaki, Y.; Inokawa, H.; Obata, Y.; Nagao, S.; Yagita, K. Association of Social Jetlag and Eating Patterns with Sleep Quality and Daytime Sleepiness in Japanese High School Students. J. Sleep Res. 2023, 32, e13661. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, D.; Wainstein, J.; Landau, Z.; Raz, I.; Ahren, B.; Chapnik, N.; Ganz, T.; Menaged, M.; Barnea, M.; Bar-Dayan, Y.; et al. Influences of Breakfast on Clock Gene Expression and Postprandial Glycemia in Healthy Individuals and Individuals with Diabetes: A Randomized Clinical Trial. Diabetes Care 2017, 40, 1573–1579. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric Assessment of Subjective Sleep Quality Using the Japanese Version of the Pittsburgh Sleep Quality Index (PSQI-J) in Psychiatric Disordered and Control Subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Drake, C.; Nickel, C.; Burduvali, E.; Roth, T.; Jefferson, C.; Badia, P. The Pediatric Daytime Sleepiness Scale (PDSS): Sleep Habits and School Outcomes in Middle-School Children. Sleep 2003, 26, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Komada, Y.; Breugelmans, R.; Drake, C.L.; Nakajima, S.; Tamura, N.; Tanaka, H.; Inoue, S.; Inoue, Y. Social Jetlag Affects Subjective Daytime Sleepiness in School-Aged Children and Adolescents: A Study Using the Japanese Version of the Pediatric Daytime Sleepiness Scale (PDSS-J). Chronobiol. Int. 2016, 33, 1213739. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, Y.; Kaneita, Y.; Itani, O.; Jike, M.; Osaki, Y.; Higuchi, S.; Kanda, H.; Kinjo, A.; Kuwabara, Y.; Yoshimoto, H. Skipping Breakfast, Poor Sleep Quality, and Internet Usage and Their Relation with Unhappiness in Japanese Adolescents. PLoS ONE 2020, 15, e0235252. [Google Scholar] [CrossRef] [PubMed]
- Burnell, S.; Brushe, M.E.; Sechague Monroy, N.; Gregory, T.; Sincovich, A. The Association Between Breakfast Skipping and Positive and Negative Emotional Wellbeing Outcomes for Children and Adolescents in South Australia. Nutrients 2025, 17, 1304. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Subjects (N = 2969) | Breakfast Consumption (N = 1850) | Breakfast Skipping (N = 1119) | p | |
|---|---|---|---|---|---|
| Age, N. | 15 | 754 | 512 | 242 | <0.001 |
| 16 | 1441 | 864 | 577 | ||
| 17 | 767 | 468 | 299 | ||
| 18 | 7 | 6 | 1 | ||
| Sex, N. | Male | 1368 | 862 | 506 | 0.466 |
| Female | 1601 | 988 | 613 | ||
| PSQI, means ± SD | 5.8 ± 2.4 | 5.5 ± 2.2 | 6.3 ± 2.5 | <0.001 | |
| PDSS, means ± SD | 18.2 ± 5.1 | 17.6 ± 5.0 | 19.3 ± 5.1 | <0.001 | |
| Wake-up time, means ± SD (h:min) | 6:52 ± 0:58 | 6:38 ± 0:50 | 7:14 ± 1:02 | <0.001 | |
| Bedtime, means ± SD (h:min) | 23:47 ± 0:59 | 23:39 ± 0:54 | 00:02 ± 1:05 | <0.001 | |
| Sleep duration, means ± SD (h) | 7.0 ± 1.0 | 6.9 ± 0.9 | 7.1 ± 0.9 | <0.001 |
| aOR | 95%CI | p | ||
|---|---|---|---|---|
| Age | (a) 15 years old | ref | ||
| (b) 16 years old | 1.42 | 1.17–1.75 | 0.0005 | |
| (c) 17 and 18 years old | 1.39 | 1.10–1.75 | 0.0051 | |
| Sex | (a) Male | ref | ||
| (b) Female | 1.11 | 0.94–1.30 | 0.2255 | |
| Wake-up time | (a) ≤6:00 | ref | ||
| (b) >6:00 and ≤6:30 | 1.00 | 0.75–1.35 | 0.9776 | |
| (c) >6:30 and ≤7:00 | 1.49 | 1.14–1.95 | 0.0034 | |
| (d) >7:00 and ≤7:30 | 2.58 | 1.97–3.40 | <0.0001 | |
| (e) >7:30 and ≤8:00 | 4.83 | 3.54–6.59 | <0.0001 | |
| (f) >8:00 | 9.43 | 6.62–13.45 | <0.0001 | |
| Sleep duration | (a) ≤6.0 h | ref | ||
| (b) >6.0 h and ≤6.5 h | 0.87 | 0.65–1.18 | 0.3684 | |
| (c) >6.5 h and ≤7.0 h | 0.83 | 0.63–1.09 | 0.1782 | |
| (d) >7.0 h and ≤7.5 h | 0.80 | 0.60–1.06 | 0.1199 | |
| (e) >7.5 h and ≤8.0 h | 0.86 | 0.63–1.17 | 0.3283 | |
| (f) >8.0 h | 1.07 | 0.78–1.48 | 0.6728 | |
| PSQI | (a) <6 | ref | ||
| (b) ≥ 6 | 1.39 | 1.17–1.65 | 0.0001 | |
| PDSS | (a) <21 | ref | ||
| (b) ≥ 21 | 1.46 | 1.23–1.74 | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagao, S.; Sasawaki, Y.; Inokawa, H.; Kitagawa, N.; Takashima, N.; Yagita, K. Association Between Multi-Dimensional Sleep Health and Breakfast Skipping in Japanese High School Students. Nutrients 2025, 17, 3005. https://doi.org/10.3390/nu17183005
Nagao S, Sasawaki Y, Inokawa H, Kitagawa N, Takashima N, Yagita K. Association Between Multi-Dimensional Sleep Health and Breakfast Skipping in Japanese High School Students. Nutrients. 2025; 17(18):3005. https://doi.org/10.3390/nu17183005
Chicago/Turabian StyleNagao, Suzune, Yuh Sasawaki, Hitoshi Inokawa, Nobuko Kitagawa, Naoyuki Takashima, and Kazuhiro Yagita. 2025. "Association Between Multi-Dimensional Sleep Health and Breakfast Skipping in Japanese High School Students" Nutrients 17, no. 18: 3005. https://doi.org/10.3390/nu17183005
APA StyleNagao, S., Sasawaki, Y., Inokawa, H., Kitagawa, N., Takashima, N., & Yagita, K. (2025). Association Between Multi-Dimensional Sleep Health and Breakfast Skipping in Japanese High School Students. Nutrients, 17(18), 3005. https://doi.org/10.3390/nu17183005







