Validation of KIDMED 2.0 PL—Mediterranean Diet Quality Index for Polish Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
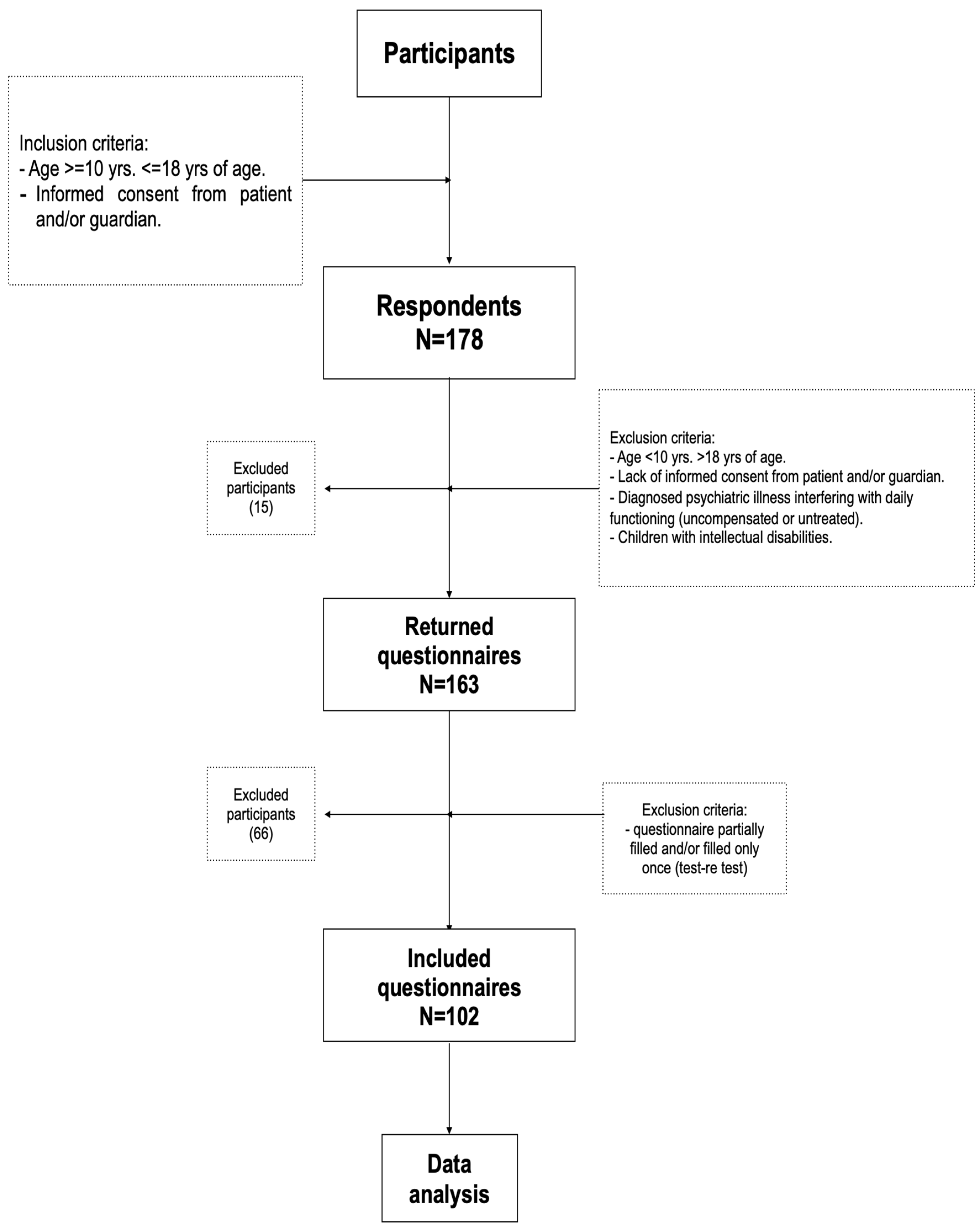
2.1. Study Design and Participants
2.2. Questionnaire Adaptation
2.3. Pilot Testing
2.4. Statistical Analysis
2.4.1. Test–Retest Reliability
2.4.2. Criterion Validity
2.5. Ethical Approval and Consent to Participate
3. Results
3.1. Sample Characteristics
3.2. Adherence to the Mediterranean Diet by Weight Status
3.3. Distribution of KIDMED 2.0 PL Scores
3.4. Reliability and Validity
3.5. Selected Dietary Behaviours
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WHO | World Health Organisation |
| COSI | Childhood Obesity Surveillance Initiative |
| KIDMED | Mediterranean Diet Quality Index |
| KIDMED 2.0 PL | Mediterranean Diet Quality Index for Polish children and adolescents |
| BMI | Body Mass Index |
References
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Pyramid Today. Science and Cultural Updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean Diet: A Literature Review. Nutrients 2015, 7, 5459. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Roman, B.; Estruch, R. Scientific Evidence of Interventions Using the Mediterranean Diet: A Systematic Review. Nutr. Rev. 2019, 77, 901–929. [Google Scholar]
- Dernini, S.; Berry, E.M. Mediterranean Diet: From a Healthy Diet to a Sustainable Dietary Pattern. Front. Nutr. 2015, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- García-Fernández, E.; Rico-Cabanas, L.; Rosgaard, N.; Estruch, R.; Bach-Faig, A. Mediterranean Diet and Cardiodiabesity: A Review. Nutrients 2014, 6, 3474. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA Food Classification and the Trouble with Ultra-Processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Lauria, F.; Dello Russo, M.; Formisano, A.; De Henauw, S.; Hebestreit, A.; Hunsberger, M.; Krogh, V.; Intemann, T.; Lissner, L.; Molnar, D.; et al. Ultra-Processed Foods Consumption and Diet Quality of European Children, Adolescents and Adults: Results from the I.Family Study. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3031–3043. [Google Scholar] [CrossRef]
- Dzielska, A.; Liber, A.; Fijałkowska, A. Sposób żywienia i stan odżywienia niemowląt, dzieci i młodzieży. In Sytuacja Zdrowotna Ludności Polski i Jej Uwarunkowania 2025; Wojtyniak, B., Smaga, A., Eds.; Narodowy Instytut Zdrowia Publicznego PZH–PIB: Warszawa, Poland, 2025; pp. 447–474. [Google Scholar]
- Dernini, S.; Berry, E.M.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.X.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Trichopoulou, A. Med Diet 4.0: The Mediterranean Diet with Four Sustainable Benefits. Public Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef]
- da Silva, R.; Bach-Faig, A.; Raido Quintana, B.; Buckland, G.; Vaz de Almeida, M.D.; Serra-Majem, L. Worldwide Variation of Adherence to the Mediterranean Diet, in 1961–1965 and 2000–2003. Public Health Nutr. 2009, 12, 1676–1684. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; Guallar-Castillón, P.; López-García, E.; Rodríguez-Artalejo, F. Adherence to the Mediterranean Diet Pattern Has Declined in Spanish Adults. J. Nutr. 2012, 142, 1843–1850. [Google Scholar] [CrossRef]
- Kontogianni, M.D.; Vidra, N.; Farmaki, A.E.; Koinaki, S.; Belogianni, K.; Sofrona, S.; Magkanari, F.; Yannakoulia, M. Adherence Rates to the Mediterranean Diet Are Low in a Representative Sample of Greek Children and Adolescents. J. Nutr. 2008, 138, 1951–1956. [Google Scholar] [CrossRef]
- Popkin, B.M. Global Nutrition Dynamics: The World Is Shifting Rapidly toward a Diet Linked with Noncommunicable Diseases. Am. J. Clin. Nutr. 2006, 84, 289–298. [Google Scholar] [CrossRef]
- Rito, A.I.; Dinis, A.; Rascôa, C.; Maia, A.; de Carvalho Martins, I.; Santos, M.; Lima, J.; Mendes, S.; Garcia, E.; Breda, J. Prevalence of Obesity in Portugal: Results from the National Food, Nutrition and Physical Activity Survey, 2015–2016. Obes. Res. Clin. Pract. 2019, 13, 40–48. [Google Scholar]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean Diet and Health Status: Meta-Analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef] [PubMed]
- García Cabrera, S.; Herrera Fernández, N.; Rodríguez Hernández, C.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. KIDMED Test; Prevalence of Low Adherence to the Mediterranean Diet in Children and Young; A Systematic Review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED: Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Altavilla, C.; Caballero-Pérez, P. An update of the KIDMED questionnaire, a Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2019, 22, 2543–2547. [Google Scholar] [CrossRef] [PubMed]
- Gesteiro, E.; García-Carro, A.; Aparicio-Ugarriza, R.; Ortega, R.M.; Partearroyo, T.; Varela-Moreiras, G. Adherence to Mediterranean Diet among Spanish Children and Youth: The Role of Sociodemographic and Lifestyle Factors. Nutrients 2022, 14, 1053. [Google Scholar]
- Bibiloni, M.M.; Pons, A.; Tur, J.A. Compliance with the Mediterranean Diet Profile among the Young Population in Majorca. Nutr. J. 2011, 10, 98. [Google Scholar]
- Pérez-Gallardo, L.; Martínez, A.; Olza, J.; Martínez, R. A High Intake of Ultra-Processed Foods Is Associated with Lower Adherence to the Mediterranean Diet in Spanish Youth. Nutrients 2021, 13, 2332. [Google Scholar]
- Gómez-Martínez, S.; Martínez-Gómez, D.; Pérez de Heredia, F.; Romeo, J.; Cuenca-García, M.; Martín-Matillas, M.; Castillo, M.; Rey-López, J.-P.; Vicente-Rodriguez, G.; Moreno, L.; et al. Eating Habits and Total and Abdominal Fat in Spanish Adolescents: The AVENA Study. Nutr. Hosp. 2012, 27, 208–215. [Google Scholar]
- Farpour-Lambert, N.J.; Baker, J.L.; Hassapidou, M.; Holm, J.-C.; Nowicka, P.; Weiss, R. Childhood Obesity Is a Chronic Disease Demanding Specific Health Care—A Position Statement from the Childhood Obesity Task Force (COTF) of the European Association for the Study of Obesity (EASO). Obes. Facts 2015, 8, 342–349. [Google Scholar] [CrossRef]
- Rota, M.; Morales-Suárez-Varela, M.; Donzelli, G. Effect of the Mediterranean Diet on BMI and Body Composition: A Preliminary Pre–Post Intervention Study in Pediatric Overweight Patients. Nutrition 2025, 139, 112878. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Brazo-Sayavera, J.; García-Hermoso, A.; Yuste Lucas, J.L. Adherence to Mediterranean Diet Related with Physical Fitness and Physical Activity in Schoolchildren Aged 6–13. Nutrients 2020, 12, 567. [Google Scholar] [CrossRef] [PubMed]
- Grzymisławska, M.; Krzywonos, A.; Foryś, P. Ultra-Processed Foods in Polish School Canteens: Barriers to Implementation of Mediterranean Diet Principles. Rocz. Panstw. Zakl. Hig. 2020, 71, 313–319. [Google Scholar]
- Shafiei, F.; Salari-Moghaddam, A.; Larijani, B.; Esmaillzadeh, A. Adherence to the Mediterranean Diet and Risk of Depression: A Systematic Review and Updated Meta-Analysis of Observational Studies. Nutr. Rev. 2019, 77, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Martínez-González, M.A.; Tong, T.Y.N.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and Potential Health Benefits of the Mediterranean Diet: Views from Experts around the World. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Levy, R.B.; Claro, R.M.; de Castro, I.R.R.; Cannon, G. A New Classification of Foods Based on the Extent and Purpose of Their Processing. Cad. Saude Publica 2010, 26, 2039–2049. [Google Scholar] [CrossRef]
- Popkin, B.M.; Reardon, T. Obesity and the Food System Transformation in Latin America. Obes. Rev. 2018, 19, 1028–1064. [Google Scholar] [CrossRef]
- Vyncke, K.; Cruz Fernandez, E.; Fajó-Pascual, M.; Cuenca-García, M.; De Keyzer, W.; Gonzalez-Gross, M.; Moreno, L.A.; Beghin, L.; Breidenassel, C.; Kersting, M.; et al. Validation of the Diet Quality Index for Adolescents by Comparison with Biomarkers, Nutrient and Food Intakes: The HELENA Study. Public Health Nutr. 2013, 16, 399–408. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. Ser. A 2018, 73, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Hebestreit, A.; Intemann, T.; Siani, A.; De Henauw, S.; Eiben, G.; Kourides, Y.A.; Kovacs, E.; Moreno, L.A.; Veidebaum, T.; Krogh, V.; et al. Dietary Patterns of European Children and Their Parents in Association with Family Food Environment: Results from the I.Family Study. Nutrients 2017, 9, 126. [Google Scholar] [CrossRef] [PubMed]
- Moreno, L.A.; Sarría, A.; Popkin, B.M. The Nutrition Transition in Spain: A European Mediterranean Country. Eur. J. Clin. Nutr. 2002, 56, 992–1003. [Google Scholar] [CrossRef] [PubMed]
- Rosi, A.; Paolella, G.; Biasini, B.; Scazzina, F. Adherence to the Mediterranean Diet Pattern among Italian Adolescents: A Cross-Sectional Study. Nutrients 2020, 12, 2174. [Google Scholar]
- Kapantais, E.; Chala, E.; Kaklamanou, D.; Lanaras, L.; Kaklamanou, M.; Tzotzas, T. Breakfast Skipping and Its Relation to BMI and Health-Compromising Behaviours among Greek Adolescents. Public Health Nutr. 2011, 14, 101–108. [Google Scholar] [CrossRef]
- López-Gil, J.F.; García-Hermoso, A.; Sotos-Prieto, M.; Cavero-Redondo, I.; Martínez-Vizcaíno, V.; Kales, S.N. Mediterranean Diet-Based Interventions to Improve Anthropometric and Obesity Indicators in Children and Adolescents: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2023, 14, 858–869. [Google Scholar] [CrossRef]
- Blair, S.; Henderson, M.; McConnachie, A.; McIntosh, E.; Smillie, S.; Wetherall, K.; Wight, D.; Xin, Y.; Bond, L.; Elliott, L.; et al. The Social and Emotional Education and Development Intervention to Address Wellbeing in Primary School Age Children: The SEED Cluster RCT. Public Health Res. 2024, 12, 1–173. [Google Scholar] [CrossRef]
- Tognon, G.; Hebestreit, A.; Lanfer, A.; Moreno, L.A.; Pala, V.; Siani, A.; Tornaritis, M.; De Henauw, S.; Veidebaum, T.; Molnár, D.; et al. Mediterranean Diet, Overweight and Body Composition in Children from Eight European Countries: Cross-Sectional and Prospective Results from the IDEFICS Study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 205–213. [Google Scholar] [CrossRef]
- Grosso, G.; Bella, F.; Godos, J.; Sciacca, S.; Del Rio, D.; Ray, S.; Galvano, F.; Giovannucci, E.L. Possible Role of Diet in Cancer: Systematic Review and Multiple Meta-Analyses of Dietary Patterns, Lifestyle Factors, and Cancer Risk. Nutr. Rev. 2017, 75, 405–419. [Google Scholar] [CrossRef]
- Ortega, R.M.; Pérez-Rodrigo, C.; López-Sobaler, A.M. Dietary Assessment Methods: Dietary Records. Nutr. Hosp. 2015, 31 (Suppl. S3), 38–45. [Google Scholar]
- Gómez-Pinilla, F. Brain Foods: The Effects of Nutrients on Brain Function. Nat. Rev. Neurosci. 2008, 9, 568–578. [Google Scholar] [CrossRef]
- Gautam, N.; Dessie, G.; Rahman, M.M.; Khanam, R. Socioeconomic Status and Health Behavior in Children and Adolescents: A Systematic Literature Review. Front. Public Health 2023, 11, 1228632. [Google Scholar] [CrossRef]
- Lazarou, C.; Kalavana, T. Urbanization and Its Impact on Children’s Health and Diet in Mediterranean Countries. Int. J. Food Sci. Nutr. 2021, 72, 141–150. [Google Scholar]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What Childhood Obesity Prevention Programmes Work? A Systematic Review and Meta-Analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef] [PubMed]
- González-Jiménez, E.; Cañadas, G.R.; Fernández-Castillo, R.; Cañadas-De la Fuente, G.A. Analysis of the Life-Style and Dietary Habits of a Population of Adolescents. Nutr. Hosp. 2013, 28, 1937–1942. [Google Scholar] [PubMed]
- Castro-Quezada, I.; Román-Viñas, B.; Serra-Majem, L. The Mediterranean Diet and Nutritional Adequacy: A Review. Nutrients 2014, 6, 231. [Google Scholar] [CrossRef] [PubMed]
- Sahingoz, S.A.; Sanlier, N. Compliance with Mediterranean Diet Quality Index (KIDMED) and Nutrition Knowledge Levels in Adolescents: A Case Study from Turkey. Appetite 2011, 57, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, G.Ö.; Kabaran, S. Protective Effects of a Mediterranean-Like Dietary Pattern on Obesity, Abdominal Obesity and Large Neck Circumference in a Cohort of Turkish Children Aged 6–9 Years. Asia Pac. J. Clin. Nutr. 2020, 29, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Pira, C.; Trapani, G.; Fadda, M.; Finocchiaro, C.; Bertino, E.; Coscia, A.; Ciocan, C.; Cuciureanu, M.; Hegheş, S.C.; Vranceanu, M.; et al. Comparative Study Regarding the Adherence to the Mediterranean Diet and the Eating Habits of Two Groups—The Romanian Children and Adolescents Living in North-West of Romania and Their Romanian Counterparts Living in Italy. Foods 2021, 10, 2045. [Google Scholar] [CrossRef]
- Melguizo-Ibáñez, E.; Ubago-Jiménez, J.L.; González-Valero, G.; Badicu, G.; Al-Mhanna, S.B.; Puertas-Molero, P. Study of the Effects of Physical-Activity Practice and Adherence to the Mediterranean Diet on Emotional Intelligence in Elementary School Education Students. Children 2023, 10, 1211. [Google Scholar] [CrossRef]
- Warkentin, S.; Stratakis, N.; Fabbri, L.; Wright, J.; Yang, T.C.; Bryant, M.; Heude, B.; Slama, R.; Montazeri, P.; Vafeiadi, M.; et al. Dietary Patterns among European Children and Their Association with Adiposity-Related Outcomes: A Multi-Country Study. Int. J. Obes. 2025, 49, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Mediterranean Dietary Pattern, Inflammation and Endothelial Function: A Systematic Review and Meta-Analysis of Intervention Trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health: A Review of Evidence. Am. J. Cardiol. 2019, 124, 20–27. [Google Scholar]
- Donati Zeppa, S.; Agostini, D.; Piccoli, G.; Stocchi, V.; Sestili, P. Gut–Brain Axis and Inflammation: A Bidirectional Communication. Biomolecules 2020, 10, 12. [Google Scholar]
| Item No. | KIDMED 2.0 (Original, English) | KIDMED 2.0 PL (Adapted, English Translation) | Scoring | Adaptation Type |
|---|---|---|---|---|
| 1 | Consumes two or more servings of fruit per day. | My child consumes two or more servings of fruit per day. | +1 | Direct translation |
| 2 | Consumes at least one serving of vegetables per day. | My child consumes at least one serving of raw and/or cooked vegetables per day. | +1 | Cultural contextualisation |
| 3 | Eats legumes, lean meat, fish, or eggs at lunch and dinner. | My child consumes one portion of legumes, lean meat, fish, and/or eggs at lunch and another one at dinner. | +1 | Content clarification |
| 4 | Diet is mostly plant-based (fruits, vegetables, legumes, nuts, whole grains). | More than half of my child’s diet consists of plant-based products (fruits, vegetables, legumes, nuts, potatoes, whole grains). | +1 | Cultural contextualisation |
| 5 | When consuming meat, fish, or eggs, they are fresh and minimally processed. | When my child consumes lean meat, eggs, and/or fish, these are usually fresh and minimally processed. | +1 | Direct translation |
| 6 | Eats pre-prepared meals or fast foods (e.g., pizza, burgers) one or more times per week. | My child consumes pre-prepared meals or fast food (e.g., pizza, hamburgers) one or more times per week. | −1 | Cultural contextualisation |
| 7 | Eats three or more servings of legumes per week. | My child eats at least three servings of legumes (chickpeas, beans, soy, lentils, peas) per week. | +1 | Content clarification |
| 8 | Food is usually baked, grilled, or boiled instead of deep-fried. | At home, meals are usually prepared by baking, grilling (with little oil), or boiling (not deep-frying). | +1 | Cultural contextualisation |
| 9 | Chooses whole grains when eating cereals, pasta, rice, etc. | When my child eats cereal-based foods (pasta, rice, groats), these are usually whole-grain products. | +1 | Cultural contextualisation |
| 10 | Eats nuts ≥3 times/week without added salt. | My child eats a portion (min. 15 g) of natural or roasted unsalted nuts at least three times per week. | +1 | Content clarification |
| 11 | Uses extra virgin olive oil at home. | At home, we use extra virgin olive oil (dark green) or virgin rapeseed oil (dark yellow) instead of sunflower or rapeseed oil (bright yellow). | +1 | Cultural contextualisation |
| 12 | Drinks commercial juices, nectars, or soft drinks one or more times per week. | My child drinks store-bought beverages, juices, nectars, and/or smoothies one or more times per week. | −1 | Content clarification |
| 13 | Dairy products are natural or minimally processed (e.g., milk, yoghurt, fresh cheese). | My child always chooses natural or minimally processed dairy products (milk, unsweetened yoghurt, fresh cheese). | +1 | Direct translation |
| 14 | Eats pastries, cookies, or drinks processed beverages for breakfast. | For breakfast, my child eats pastries, cookies, and/or drinks juices, smoothies, or other processed products. | −1 | Cultural contextualisation |
| 15 | Eats whole or minimally processed foods for breakfast (fruit, vegetables, eggs, whole-grain bread, etc.). | For breakfast, my child eats unprocessed or minimally processed foods (e.g., fruits, vegetables, oats, eggs, whole-grain bread). | +1 | Content clarification |
| 16 | Eats sweets, cookies, or processed snacks several times per week. | My child consumes industrially processed sweets (candies, cookies, snacks, chocolate) and/or desserts (chips, cakes, jelly candies) more than once a week. | −1 | Cultural contextualisation |
| Variables | Underweight (n = 12) | Normal Weight (n = 30) | Overweight (n = 30) | Obese (n = 30) | Total (N = 102) |
|---|---|---|---|---|---|
| mean age (SD), years | 15.0 (2.4) | 13.5 (2.5) | 13.6 (2.7) | 13.5 (2.9) | 13.8 (2.6) |
| girls, n (%) | 6 (50.0%) | 17 (56.7%) | 16 (53.3%) | 19 (63.3%) | 55 (53.9%) |
| boys, n (%) | 6 (50.0%) | 13 (43.3%) | 14 (46.7%) | 11 (36.7%) | 47 (46.1%) |
| Weight Status | n | Mean KIDMED 2.0 PL Score | Standard Deviation (SD) | Statistical Comparison |
|---|---|---|---|---|
| Underweight | 12 | 7.0 | 1.5 | Underweight and normal weight scored significantly higher on the KIDMED 2.0 PL than overweight and obese. |
| Normal weight | 30 | 8.6 | 1.7 | |
| Overweight | 30 | 3.7 | 0.8 | |
| Obese | 30 | 1.7 | 1.4 | |
| Kruskal–Wallis H test | H = 38.72, p < 0.001 | |||
| Adherence Level | Score Range | n | % of Total Sample |
|---|---|---|---|
| low adherence | ≥3 | 54 | 52.9% |
| moderate adherence | 4–7 | 29 | 28.5% |
| high adherence | ≥8 | 19 | 18.6% |
| total | — | 102 | 100.0% |
| Measure | Statistic | Value | Interpretation |
|---|---|---|---|
| test–retest (Time 1) | Mean ± SD | 5.24 ± 2.89 | – |
| test–retest (Time 2) | Mean ± SD | 5.31 ± 2.92 | – |
| reliability | Spearman’s ρ | 0.876 (p < 0.001) | High reproducibility over a 2-week interval |
| criterion validity | Spearman’s ρ (KIDMED vs. BMI centile) | −0.854 (p < 0.001) | Strong inverse correlation |
| Item No. | KIDMED 2.0 PL Item (English Translation) | Type | n (%) Responding “Yes” |
|---|---|---|---|
| 1 | My child consumes two or more servings of fruit per day. | Positive (+1) | 74 (72.5%) |
| 2 | My child consumes at least one serving of raw and/or cooked vegetables per day. | Positive (+1) | 66 (64.7%) |
| 7 | My child eats at least three servings of legumes per week. | Positive (+1) | 12 (11.8%) |
| 11 | At home, we use extra virgin olive oil (dark green) or virgin rapeseed oil (dark yellow) instead of sunflower or rapeseed oil (yellow). | Positive (+1) | 19 (18.6%) |
| 16 | My child consumes industrially processed sweets and/or desserts several times per week. | Negative (−1) | 76 (74.5%) |
| 12 | My child drinks store-bought beverages, juices, nectars, and/or smoothies one or more times per week. | Negative (−1) | 62 (60.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bober, J.; Gaszyńska, E. Validation of KIDMED 2.0 PL—Mediterranean Diet Quality Index for Polish Children and Adolescents. Nutrients 2025, 17, 2636. https://doi.org/10.3390/nu17162636
Bober J, Gaszyńska E. Validation of KIDMED 2.0 PL—Mediterranean Diet Quality Index for Polish Children and Adolescents. Nutrients. 2025; 17(16):2636. https://doi.org/10.3390/nu17162636
Chicago/Turabian StyleBober, Julia, and Ewelina Gaszyńska. 2025. "Validation of KIDMED 2.0 PL—Mediterranean Diet Quality Index for Polish Children and Adolescents" Nutrients 17, no. 16: 2636. https://doi.org/10.3390/nu17162636
APA StyleBober, J., & Gaszyńska, E. (2025). Validation of KIDMED 2.0 PL—Mediterranean Diet Quality Index for Polish Children and Adolescents. Nutrients, 17(16), 2636. https://doi.org/10.3390/nu17162636







