High Prevalence of Vitamin D Deficiency in Patients Undergoing Total Shoulder or Elbow Arthroplasty
Abstract
1. Introduction
2. Patients and Methods
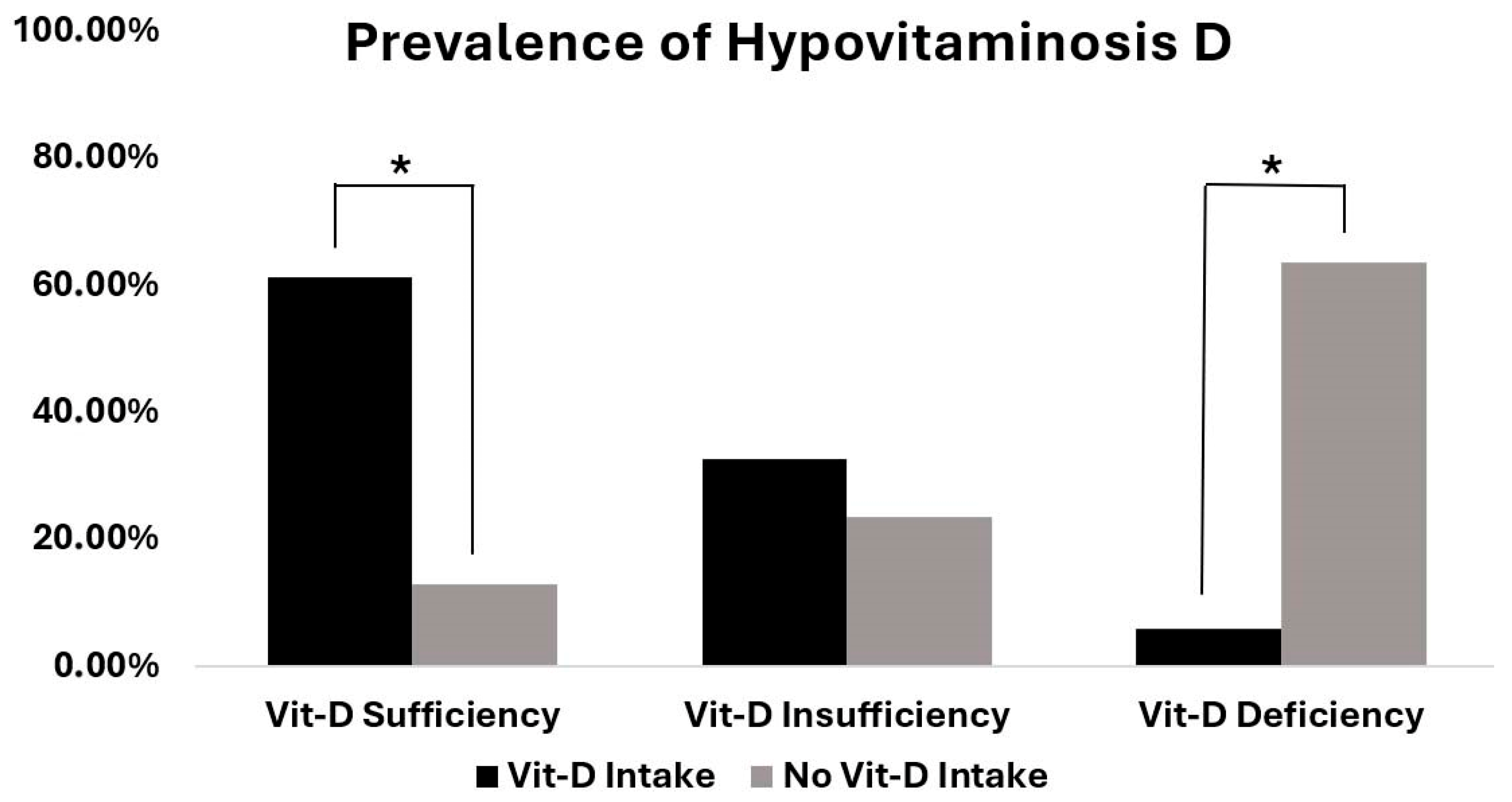
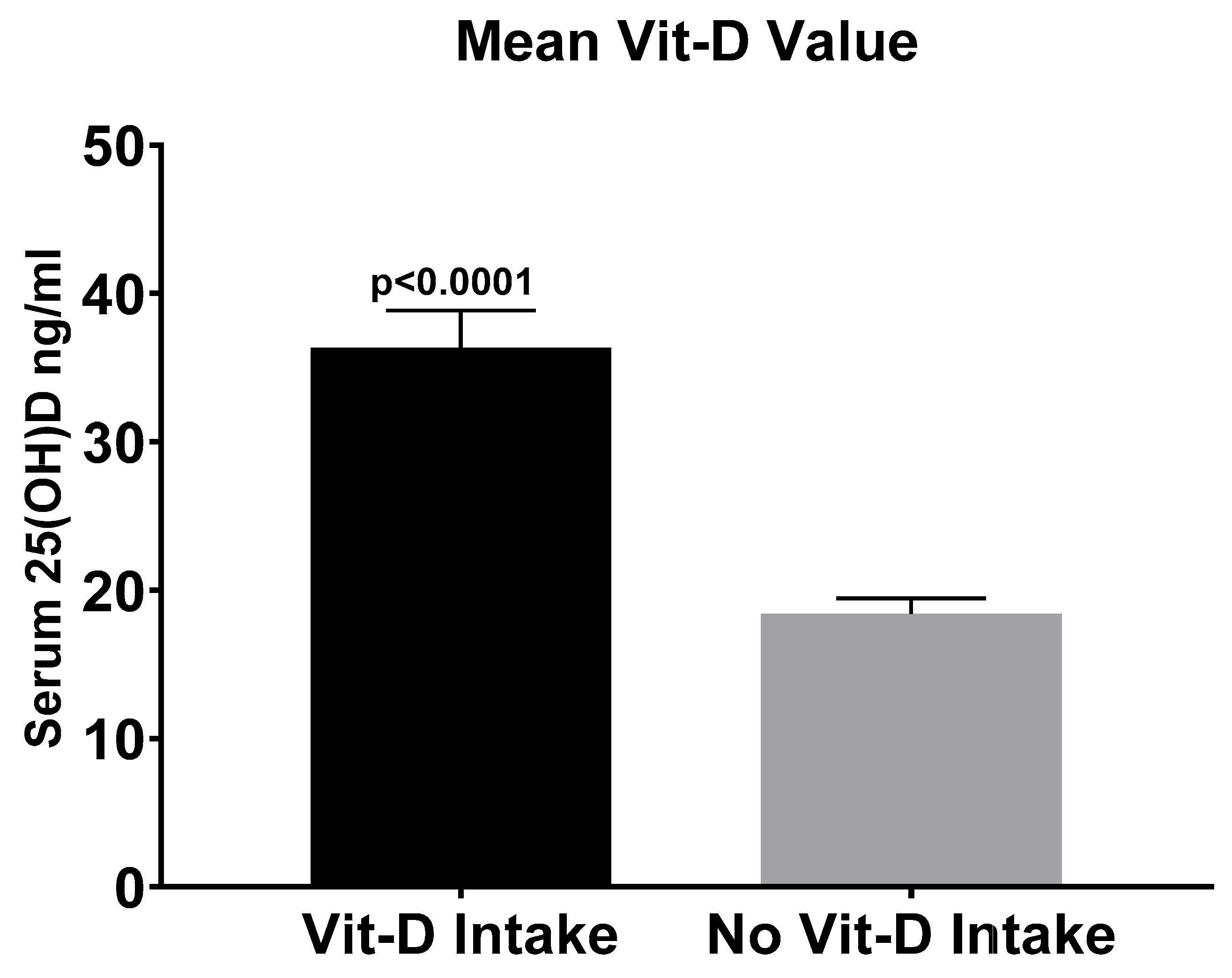
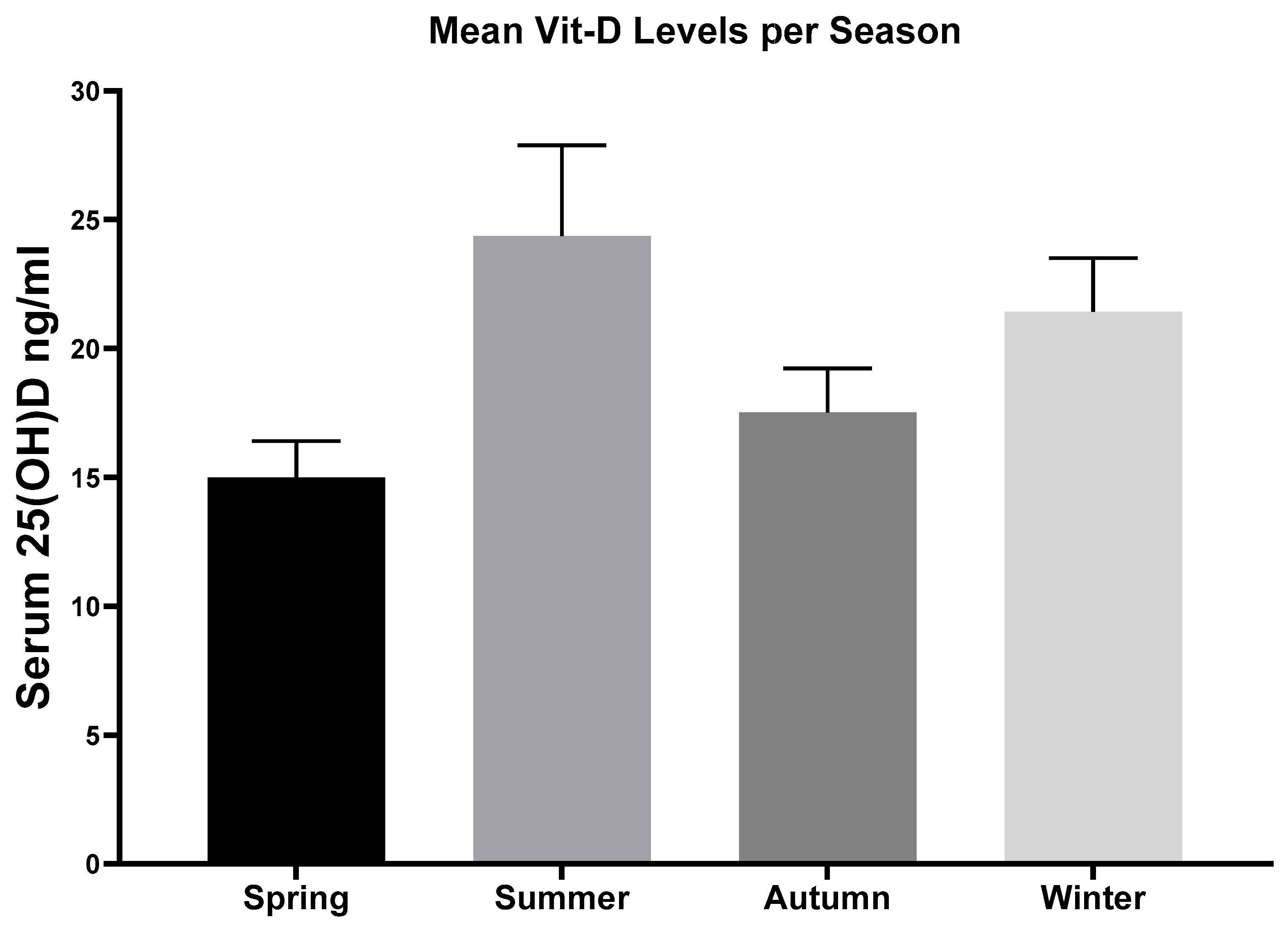
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Izquierdo, R.; Voloshin, I.; Edwards, S.; Freehill, M.Q.; Stanwood, W.; Wiater, J.M.; Watters, W.C., 3rd; Goldberg, M.J.; Keith, M.; Turkelson, C.M.; et al. Treatment of glenohumeral osteoarthritis. J. Am. Acad. Orthop. Surg. 2010, 18, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Day, J.S.; Lau, E.; Ong, K.L.; Williams, G.R.; Ramsey, M.L.; Kurtz, S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J. Shoulder Elb. Surg. 2010, 19, 1115–1120. [Google Scholar] [CrossRef] [PubMed]
- Harjula, J.N.E.; Paloneva, J.; Haapakoski, J.; Kukkonen, J.; Äärimaa, V. Increasing incidence of primary shoulder arthroplasty in Finland—A nationwide registry study. BMC Musculoskelet. Disord. 2018, 19, 245. [Google Scholar] [CrossRef]
- Longo, U.G.; Papalia, R.; Castagna, A.; De Salvatore, S.; Guerra, E.; Piergentili, I.; Denaro, V. Shoulder replacement: An epidemiological nationwide study from 2009 to 2019. BMC Musculoskelet. Disord. 2022, 23, 889. [Google Scholar] [CrossRef]
- Wagner, E.R.; Farley, K.X.; Higgins, I.; Wilson, J.M.; Daly, C.A.; Gottschalk, M.B. The incidence of shoulder arthroplasty: Rise and future projections compared with hip and knee arthroplasty. J. Shoulder Elb. Surg. 2020, 29, 2601–2609. [Google Scholar] [CrossRef] [PubMed]
- Nixon, M.; Taylor, G.; Sheldon, P.; Iqbal, S.J.; Harper, W. Does bone quality predict loosening of cemented total hip replacements? J. Bone Jt. Surg. Br. Vol. 2007, 89, 1303–1308. [Google Scholar] [CrossRef]
- James, S.J.; Mirza, S.B.; Culliford, D.J.; Taylor, P.A.; Carr, A.J.; Arden, N.K. Baseline bone mineral density and boneturnover in pre-operative hip and knee arthroplasty patients. Bone Jt. Res. 2014, 3, 14–19. [Google Scholar] [CrossRef]
- Franklin, J.; Malchau, H. Risk factors for periprosthetic femoral fracture. Injury 2007, 38, 655–660. [Google Scholar] [CrossRef]
- Smith, J.M.; Cancienne, J.M.; Brockmeier, S.F.; Werner, B.C. Vitamin D deficiency and total shoulder arthroplasty complications. Shoulder Elb. 2021, 13, 99–105. [Google Scholar] [CrossRef]
- Maier, G.S.; Weissenberger, M.; Rudert, M.; Roth, K.E.; Horas, K. The role of vitamin D and vitamin D deficiency in orthopaedics and traumatology-a narrative overview of the literature. Ann. Transl. Med. 2021, 9, 942. [Google Scholar] [CrossRef]
- Wintermeyer, E.; Ihle, C.; Ehnert, S.; Stöckle, U.; Ochs, G.; de Zwart, P.; Flesch, I.; Bahrs, C.; Nussler, A.K. Crucial Role of Vitamin D in the Musculoskeletal System. Nutrients 2016, 8, 319. [Google Scholar] [CrossRef]
- Lips, P.; van Schoor, N.M. The effect of vitamin D on bone and osteoporosis. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 585–591. [Google Scholar] [CrossRef]
- Callegari, E.T.; Reavley, N.; Garland, S.M.; Gorelik, A.; Wark, J.D. Vitamin D Status, Bone Mineral Density and Mental Health in Young Australian Women: The Safe-D Study. J. Public Health Res. 2015, 4, 594. [Google Scholar] [CrossRef]
- Nair, R.; Maseeh, A. Vitamin D: The “sunshine” vitamin. J. Pharmacol. Pharmacother. 2012, 3, 118–126. [Google Scholar] [CrossRef]
- Hegde, V.; Arshi, A.; Wang, C.; Buser, Z.; Wang, J.C.; Jensen, A.R.; Adams, J.S.; Zeegen, E.N.; Bernthal, N.M. Preoperative Vitamin D Deficiency Is Associated with Higher Postoperative Complication Rates in Total Knee Arthroplasty. Orthopedics 2018, 41, e489–e495. [Google Scholar] [CrossRef]
- Vivek, K.; Kamal, R.; Perera, E.; Gupte, C.M. Vitamin D Deficiency Leads to Poorer Health Outcomes and Greater Length of Stay After Total Knee Arthroplasty and Supplementation Improves Outcomes: A Systematic Review and Meta-Analysis. JBJS Rev. 2024, 12, e23.00150. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Maier, G.S.; Jakob, P.; Horas, K.; Roth, K.E.; Kurth, A.A.; Maus, U. Vitamin D deficiency in orthopaedic patients: A single center analysis. Acta Orthop. Belg. 2013, 79, 587–591. [Google Scholar] [PubMed]
- Bogunovic, L.; Kim, A.D.; Beamer, B.S.; Nguyen, J.; Lane, J.M. Hypovitaminosis D in patients scheduled to undergo orthopaedic surgery: A single-center analysis. J. Bone Jt. Surg. Am. Vol. 2010, 92, 2300–2304. [Google Scholar] [CrossRef] [PubMed]
- Emara, A.K.; Nageeb, E.; George, J.; Buttaro, M.A.; Higuera, C.; Piuzzi, N.S. Hypovitaminosis D in lower extremity Joint Arthroplasty: A systematic review and meta-analysis. J. Orthop. 2020, 21, 109–116. [Google Scholar] [CrossRef]
- Piuzzi, N.S.; George, J.; Khlopas, A.; Klika, A.K.; Mont, M.A.; Muschler, G.F.; Higuera, C.A. High prevalence and seasonal variation of hypovitaminosis D in patients scheduled for lower extremity total joint arthroplasty. Ann. Transl. Med. 2018, 6, 321. [Google Scholar] [CrossRef]
- Inkrott, B.P.; Koberling, J.L.; Noel, C.R. Hypovitaminosis D in Patients Undergoing Shoulder Arthroplasty: A Single-Center Analysis. Orthopedics 2016, 39, e651–e656. [Google Scholar] [CrossRef] [PubMed]
- MacConnell, A.E.; Anderson, J.; Stanila, T.; Shivdasani, K.; Hand, R.; Boubekri, A.; Garbis, N.; Salazar, D. The effect of vitamin D insufficiency on outcomes and complication rates after shoulder arthroplasty: A single center retrospective examination. Semin. Arthroplast. JSES 2024, 34, 182–189. [Google Scholar] [CrossRef]
- Girgis, C.M.; Clifton-Bligh, R.J.; Hamrick, M.W.; Holick, M.F.; Gunton, J.E. The Roles of Vitamin D in Skeletal Muscle: Form, Function, and Metabolism. Endocr. Rev. 2013, 34, 33–83. [Google Scholar] [CrossRef]
- Maier, G.S.; Maus, U.; Lazovic, D.; Horas, K.; Roth, K.E.; Kurth, A.A. Is there an association between low serum 25-OH-D levels and the length of hospital stay in orthopaedic patients after arthroplasty? J. Orthop. Traumatol. 2016, 17, 297–302. [Google Scholar] [CrossRef]
- Birinci, M.; Hakyemez, Ö.S.; Geçkalan, M.A.; Mutlu, M.; Yildiz, F.; Bilgen, Ö.F.; Azboy, İ. Effect of Vitamin D Deficiency on Periprosthetic Joint Infection and Complications After Primary Total Joint Arthroplasty. J. Arthroplast. 2024, 39, S151–S157. [Google Scholar] [CrossRef]
- Kong, Y.; Han, M.; Lee, M.; Kim, E.H.; Jung, I.; Park, K.K. The Association of Calcium and Vitamin D Use with Implant Survival of Total Knee Arthroplasty: A Nationwide Population-Based Cohort Study. J. Arthroplast. 2021, 36, 542–549.e543. [Google Scholar] [CrossRef]
- Maniar, R.N.; Maniar, A.R.; Jain, D.; Bhatnagar, N.; Gajjar, A. Vitamin D Trajectory after Total Knee Arthroplasty: A Method for Quick Correction in Deficient Patients. Clin. Orthop. Surg. 2021, 13, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, M.T.; Guntin, J.; Yang, J.; DeBenedetti, A.; Karas, V.; Della Valle, C.J.; Nam, D. Vitamin D(3) Supplementation Prior to Total Knee Arthroplasty: A Randomized Controlled Trial. J. Arthroplast. 2023, 38, S114–S119. [Google Scholar] [CrossRef] [PubMed]
- Horas, K.; Hoxha, M.; Heinz, T.; Jakuscheit, A.; List, K.; Maier, G.S.; Weißenberger, M.; Rudert, M. Prevalence and Risk Factors of Vitamin D Deficiency in Patients Scheduled to Undergo Revision Arthroplasty of the Hip, Knee and Shoulder-Data from a Single-Centre Analysis. Nutrients 2024, 16, 3060. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.S.; Bowles, S.; Evans, A.L. Vitamin D in obesity. Curr. Opin. Endocrinol. Diabetes 2017, 24, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Vranić, L.; Mikolašević, I.; Milić, S. Vitamin D Deficiency: Consequence or Cause of Obesity? Medicina 2019, 55, 541. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Zhao, H.; Liu, K.; Wang, Y.; Liu, Q.; Sun, T.; Chen, S.; Ren, L. Smoking behavior and circulating vitamin D levels in adults: A meta-analysis. Food Sci. Nutr. 2021, 9, 5820–5832. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, E.; Oleröd, G.; Konar, J.; Petzold, M.; Hammarsten, O. Seasonal variations in serum 25-hydroxy vitamin D levels in a Swedish cohort. Endocrine 2015, 49, 800–808. [Google Scholar] [CrossRef]
| Characteristics | Values (Mean, Value, Precent) |
|---|---|
| No. of patients | 108 |
| Sex | |
| Men | 39 (36.6%) |
| Women | 69 (63.4%) |
| Mean Age (years ± SD) | 71 ± 10.7 |
| Reason for admission | |
| Shoulder arthroplasty | 105 (97.2%) |
| Elbow arthroplasty | 3 (2.8%) |
| Comorbidities | |
| Nicotine abuse | 18 (16.7%) |
| Obesity (BMI ≥ 30 kg/m2) | 27 (25.0%) |
| Tumour disease | 4 (04.0%) |
| Rheumatoid arthritis | 4 (4.0%) |
| Diabetes | 20 (18.5%) |
| Pulmonary disease (COPD) | 5 (5.0%) |
| Medication | |
| Glucocorticoids | 12 (11.1%) |
| Protone pump inhibitors (PPI) | 38 (35.2%) |
| Vitamin D supplementation, oral | 31 (28.7%) |
| Predictor | Coefficient | Std. Error | p-Value | Exp(B) | 95% Confidence Interval for Exp(B) |
|---|---|---|---|---|---|
| Sex | −0.517 | 0.771 | 0.502 | 0.596 | [0.132–2.693] |
| Age | −0.006 | 0.037 | 0.876 | 0.994 | [0.924–1.069] |
| BMI | −0.051 | 0.070 | 0.463 | 0.950 | [0.829–1.089] |
| Smoking | −0.965 | 1.233 | 0.434 | 0.381 | [0.035–4.100] |
| Predictor | OR | 95% CI | p-Value |
|---|---|---|---|
| Sex [Male] | 1.371 | 0.485–3.88 | 0.552 |
| Season [Autumn] | 2.094 | 0.47–9.33 | 0.333 |
| Season [Spring] | 4.323 | 1.037–18.013 | 0.044 |
| Season [Winter] | 0.648 | 0.125–3.36 | 0.606 |
| Age | 1.006 | 0.963–1.05 | 0.793 |
| BMI | 1.079 | 0.987–1.18 | 0.095 |
| Supplement | 0.062 | 0.013–0.305 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoxha, M.; Heinz, T.; Rudert, M.; List, K.; Achenbach, L.; Maier, G.; Weißenberger, M.; Horas, K. High Prevalence of Vitamin D Deficiency in Patients Undergoing Total Shoulder or Elbow Arthroplasty. Nutrients 2025, 17, 2635. https://doi.org/10.3390/nu17162635
Hoxha M, Heinz T, Rudert M, List K, Achenbach L, Maier G, Weißenberger M, Horas K. High Prevalence of Vitamin D Deficiency in Patients Undergoing Total Shoulder or Elbow Arthroplasty. Nutrients. 2025; 17(16):2635. https://doi.org/10.3390/nu17162635
Chicago/Turabian StyleHoxha, Miledi, Tizian Heinz, Maximilian Rudert, Kilian List, Leonard Achenbach, Gerrit Maier, Manuel Weißenberger, and Konstantin Horas. 2025. "High Prevalence of Vitamin D Deficiency in Patients Undergoing Total Shoulder or Elbow Arthroplasty" Nutrients 17, no. 16: 2635. https://doi.org/10.3390/nu17162635
APA StyleHoxha, M., Heinz, T., Rudert, M., List, K., Achenbach, L., Maier, G., Weißenberger, M., & Horas, K. (2025). High Prevalence of Vitamin D Deficiency in Patients Undergoing Total Shoulder or Elbow Arthroplasty. Nutrients, 17(16), 2635. https://doi.org/10.3390/nu17162635







