Growing Pains and Dietary Habits in Young Athletes: A Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Pain Questionnaire and Stratification
2.3. KIDMED Test
2.4. Endpoints and Variables
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
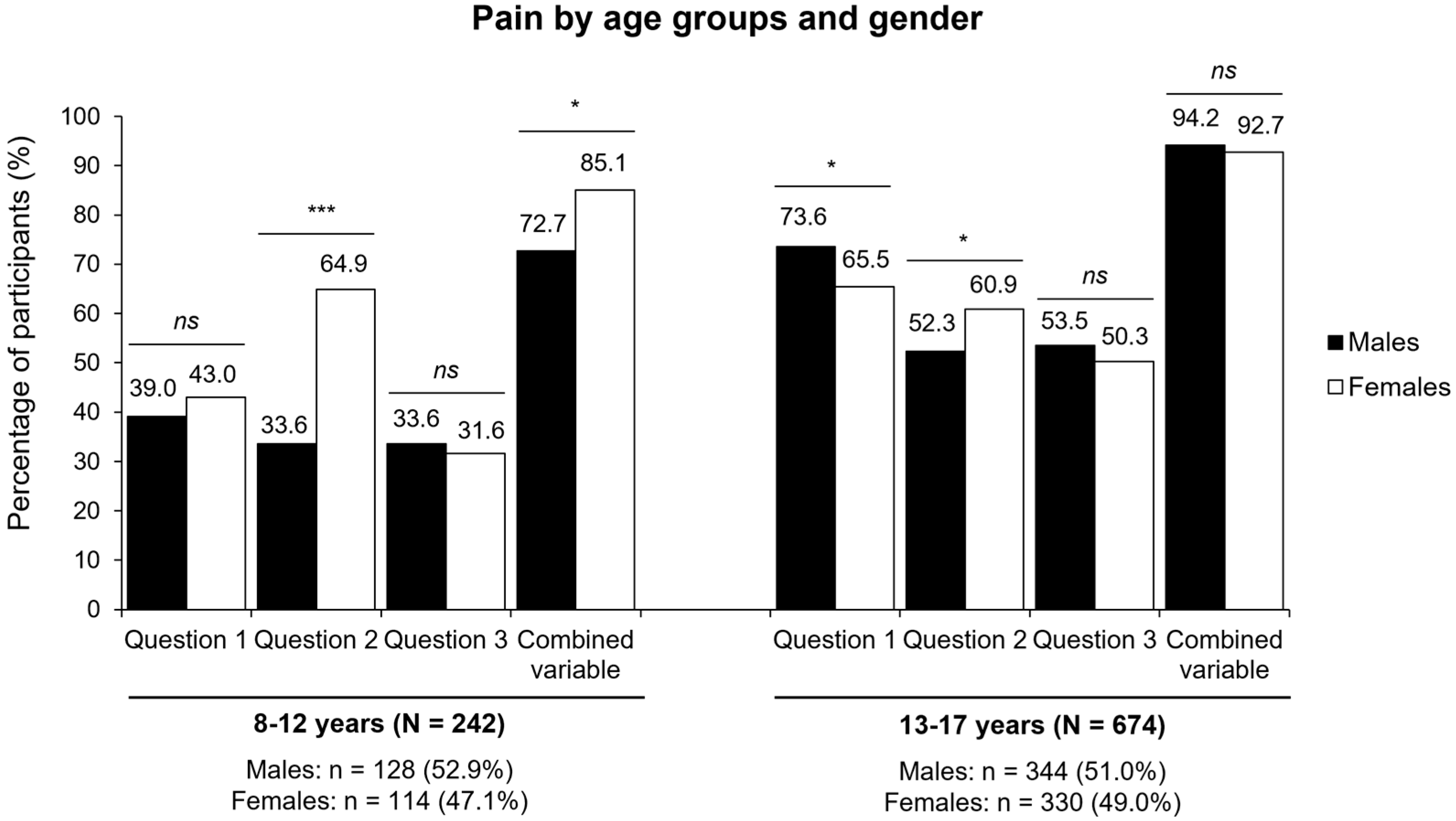
3.2. Prevalence of Pain Based on Questionnaire Responses
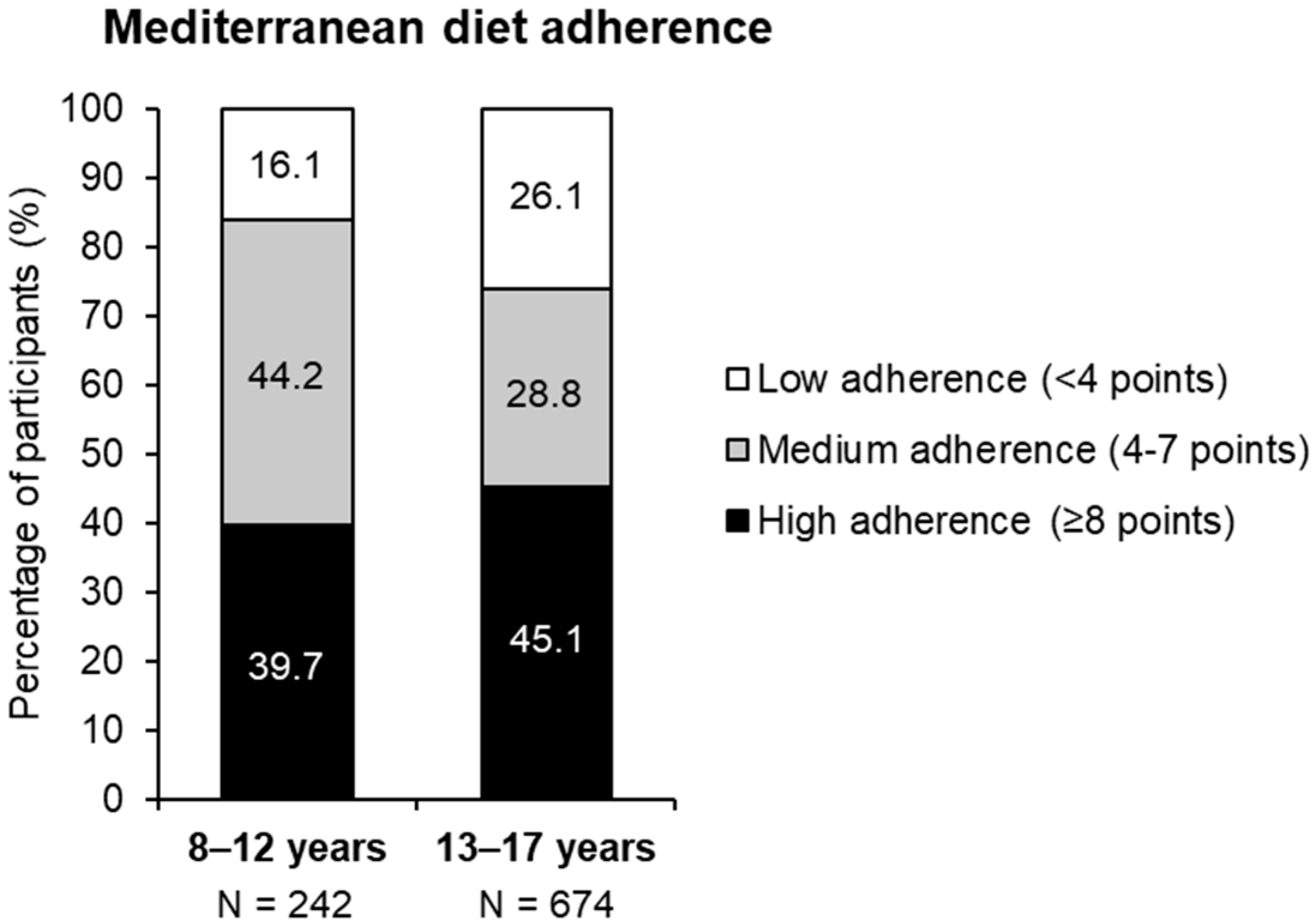
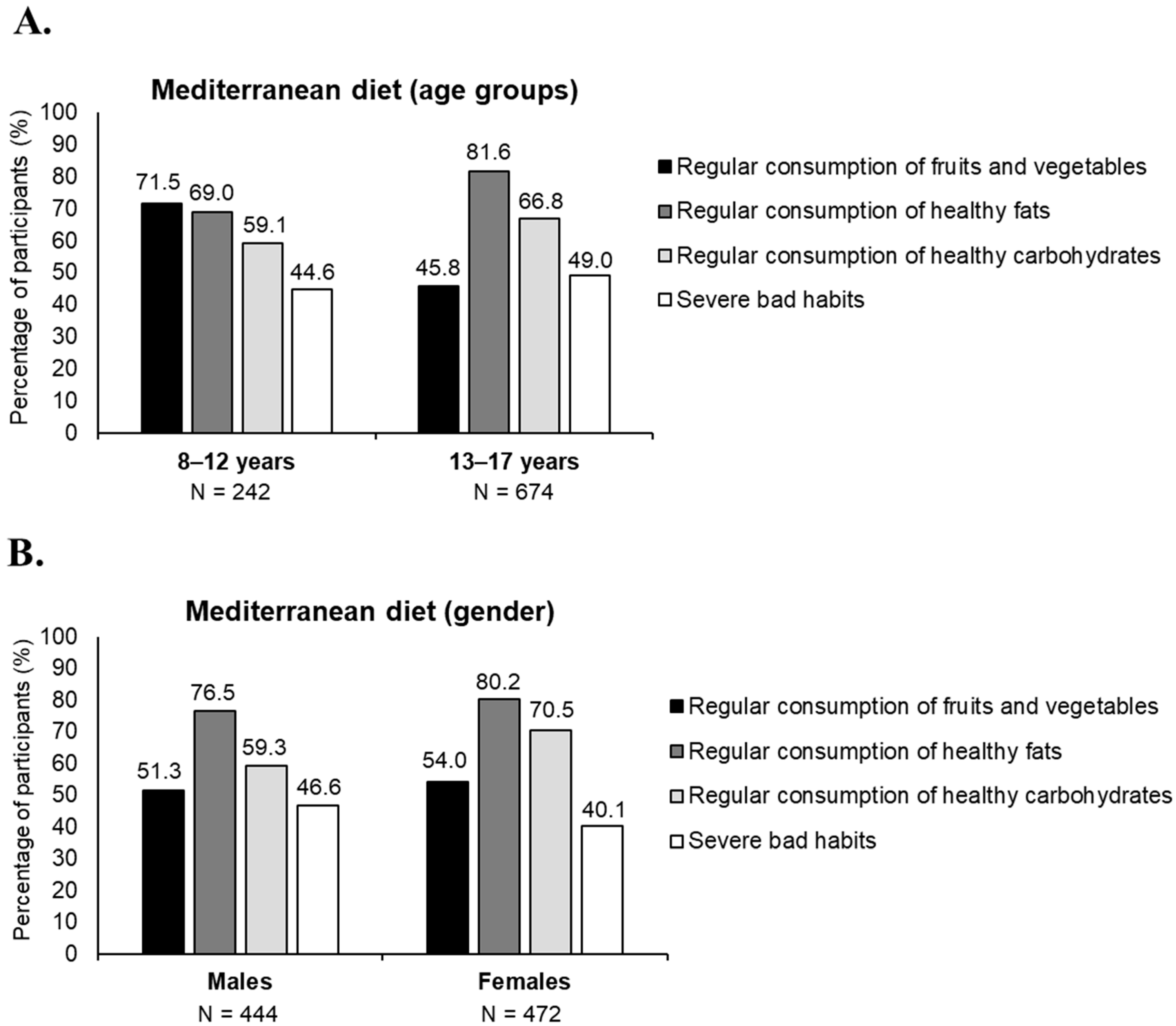
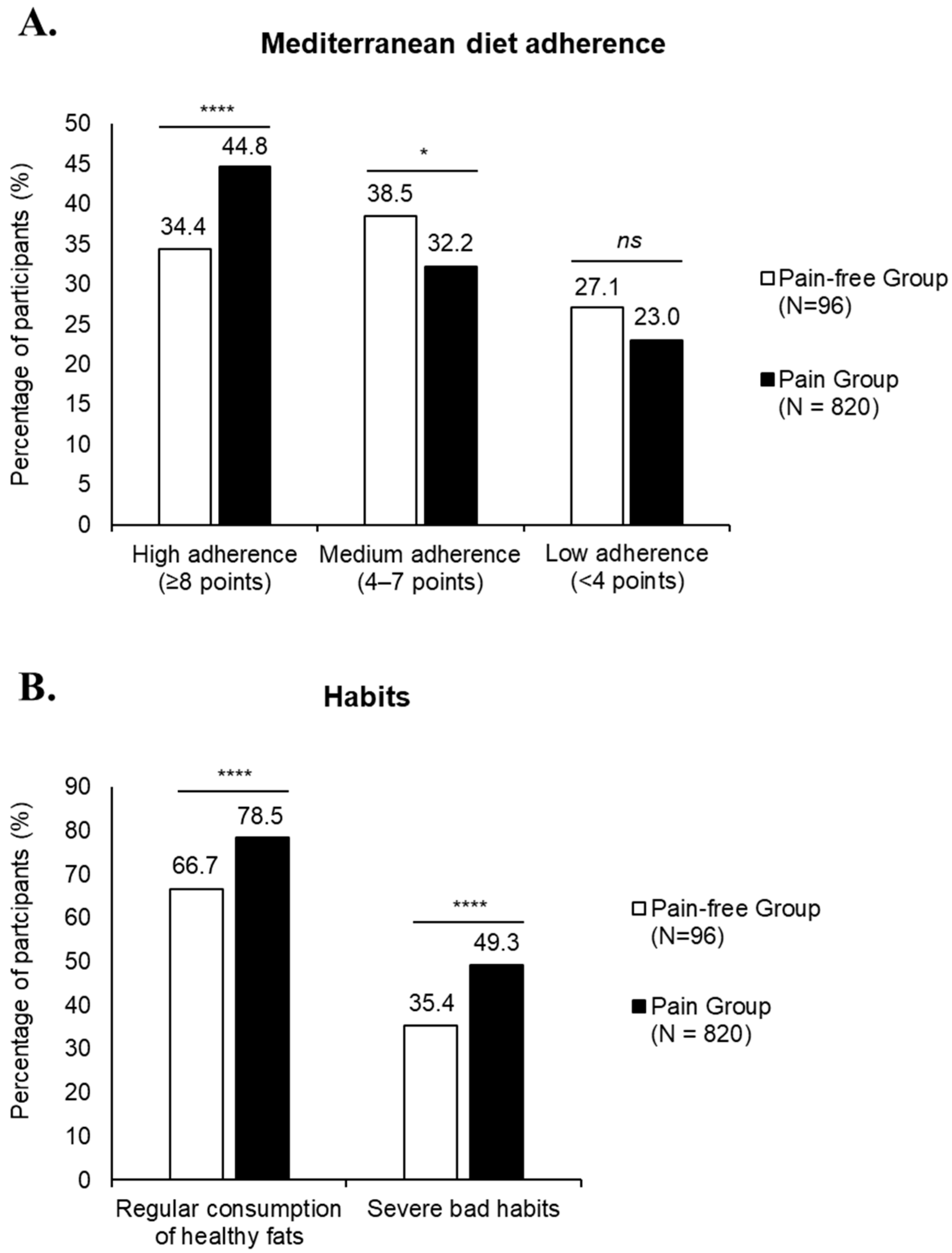
3.3. Dietary Habits
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| KIDMED | Mediterranean Diet Quality Index for children and teenagers |
| PHV | Peak Height Velocity |
References
- Duchamp, M. Maladies de la croissance. In Memoires de Médecine Practique; Levrault, F.G., Ed.; Jean-Frederic Lobstein: Paris, France, 1823. [Google Scholar]
- Øster, J.; Nielsen, A. Growing Pains: A clinical investigation of a school population. Acta Paediatr. 1972, 61, 329–334. [Google Scholar] [CrossRef] [PubMed]
- González, B. Growing pain in children: Myth or true? Rev. Méd. Clín. Las Condes 2009, 20, 892–896. [Google Scholar]
- Khuntdar, B.K.; Mondal, S.; Naik, S.; Mohanta, M.P. Prevalence of growing pains in a general paediatric OPD: A descriptive, observational and cross-sectional study. J. Fam. Med. Prim. Care 2023, 12, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Mollo Tangara, J.C.; Valdivie Rojas, N. Dolores de crecimiento/growing pains. Cienc. Méd. 2014, 17, 37–42. [Google Scholar]
- Evans, A.M.; Scutter, S.D. Prevalence of “growing pains” in young children. J. Pediatr. 2004, 145, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.M. Growing pains: Contemporary knowledge and recommended practice. J. Foot Ankle Res. 2008, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Pavone, V.; Vescio, A.; Valenti, F.; Sapienza, M.; Sessa, G.; Testa, G. Growing pains: What do we know about etiology? A systematic review. World J. Orthop. 2019, 10, 192–205. [Google Scholar] [CrossRef] [PubMed]
- Noonan, K.J.; Farnum, C.E.; Leiferman, E.M.; Lampl, M.; Markel, M.D.; Wilsman, N.J. Growing pains: Are they due to increased growth during recumbency as documented in a lamb model? J. Pediatr. Orthop. 2004, 24, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Bennie, P. Growing pains. Arch. Pediatr. 1894, 11, 337–347. [Google Scholar]
- Brenning, R. Growing pain. Acta. Soc. Med. Ups. 1960, 65, 185–201. [Google Scholar]
- Hawksley, J.C. The nature of growing pains and their relation to rheumatism in children and adolescents. Br. Med. J. 1939, 1, 155–157. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Naish, J.M.; Apley, J. “Growing pains”: A clinical study of non-arthritic limb pains in children. Arch. Dis. Child. 1951, 26, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Morandi, G.; Maines, E.; Piona, C.; Monti, E.; Sandri, M.; Gaudino, R.; Boner, A.; Antoniazzi, F. Significant association among growing pains, vitamin D supplementation, and bone mineral status: Results from a pilot cohort study. J. Bone Miner. Metab. 2015, 33, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Hashkes, P.J.; Gorenberg, M.; Oren, V.; Friedland, O.; Uziel, Y. “Growing pains” in children are not associated with changes in vascular perfusion patterns in painful regions. Clin. Rheumatol. 2005, 24, 342–345. [Google Scholar] [CrossRef] [PubMed]
- Uziel, Y.; Chapnick, G.; Jaber, L.; Nemet, D.; Hashkes, P.J. Five-year outcome of children with “growing pains”: Correlations with pain threshold. J. Pediatr. 2010, 156, 838–840. [Google Scholar] [CrossRef] [PubMed]
- Sepúlveda, C.; Mericq, V. Mecanismos reguladores de la pubertad normal y sus variaciones. Rev. Méd. Clín. Las Condes 2011, 22, 27–38. [Google Scholar]
- Lima, A.B.; Quinaud, R.T.; Karasiak, F.C.; Galvão, L.G.; Gonçalves, C.E.; Carvalho, H.M. Longitudinal meta-analysis of peak height velocity in young female athletes. Cureus 2024, 16, e59482. [Google Scholar] [CrossRef] [PubMed]
- Wild, C.Y.; Steele, J.R.; Munro, B.J. Musculoskeletal and estrogen changes during the adolescent growth spurt in girls. Med. Sci. Sports Exerc. 2013, 45, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Azzolino, D.; Spolidoro, G.C.I.; Saporiti, E.; Luchetti, C.; Agostoni, C.; Cesari, M. Musculoskeletal changes across the lifespan: Nutrition and the life-course approach to prevention. Front. Med. 2021, 8, 697954. [Google Scholar] [CrossRef] [PubMed]
- Faienza, M.F.; Urbano, F.; Chiarito, M.; Lassandro, G.; Giordano, P. Musculoskeletal health in children and adolescents. Front. Pediatr. 2023, 11, 1226524. [Google Scholar] [CrossRef] [PubMed]
- Bustamante-Sanchez, A.; Villegas-Mora, B.E.; Martínez-Guardado, I.; Tornero-Aguilera, J.F.; Ardigò, L.P.; Nobari, H.; Clemente-Suárez, V.J. Physical activity and nutritional pattern related to maturation and development. Sustainability 2022, 14, 16958. [Google Scholar] [CrossRef]
- Magnus, K.K.; Nordqvist, A. Physical activity increases bone mass during growth. Food Nutr. Res. 2008, 52, 1871. [Google Scholar] [CrossRef] [PubMed]
- Carsen, S.; Grammatopoulos, G.; Zaltz, I.; Ward, L.; Smit, K.; Beaulé, P.E. The effects of physical activity on physeal and skeletal development. JBJS Rev. 2021, 9, e21.00060. [Google Scholar] [CrossRef] [PubMed]
- Brenner, J.S.; Watson, A.; Council on Sports Medicine and Fitness; Brooks, M.A.; Carl, R.L.; Briskin, S.M.; Canty, G.; Cuff, S.; Edwards, N.M.; Kinsella, S.; et al. Overuse injuries, over-training, and burnout in young athletes. Pediatrics 2024, 153, e2023065129. [Google Scholar] [CrossRef] [PubMed]
- Mays, S. Micronutrient deficiency diseases: Anemia, scurvy, and rickets. In The International Encyclopedia of Biological Anthropology, 1st ed.; Trevathan, W., Cartmill, M., Dufour, D., Larsen, C., O’Rourke, D., Rosenberg, K., Strier, K.B., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2018; pp. 1–5. [Google Scholar]
- Inzaghi, E.; Pampanini, V.; Deodati, A.; Cianfarani, S. The effects of nutrition on linear growth. Nutrients 2022, 14, 1752. [Google Scholar] [CrossRef] [PubMed]
- Sociedad Paraguaya de Pediatría. Nutrición. Pediatría Asunción Órgano Soc. Paraguaya Pediatría 2014, 41, 87–91. [Google Scholar]
- Areal, A. Obesidad infantil. Padres Maest. 2006, 303, 28–32. [Google Scholar]
- Prakash, C.; Manjanna, B.P. The role of fueling nutrition in athletic performance. Int. J. Multidiscip. Res. 2024, 6, 14570. [Google Scholar]
- Capra, M.E.; Stanyevic, B.; Giudice, A.; Monopoli, D.; Decarolis, N.M.; Esposito, S.; Biasucci, G. Nutrition for children and adolescents who practice sport: A narrative review. Nutrients 2024, 16, 2803. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, A.; Matu, J.; Whyte, E.; Akin-Nibosun, P.; Clifford, T.; Stevenson, E.; Shannon, O.M. The Mediterranean dietary pattern for optimising health and performance in competitive athletes: A narrative review. Br. J. Nutr. 2022, 128, 1285–1298. [Google Scholar] [CrossRef] [PubMed]
- Romero Pérez, A.; Rivas Velasco, A. Adherencia a la dieta mediterránea y salud ósea. Nutr. Hosp. 2014, 29, 989–996. [Google Scholar] [PubMed]
- Craig, J.V.; Bunn, D.K.; Hayhoe, R.P.; Appleyard, W.O.; Lenaghan, E.A.; Welch, A.A. Relationship between the Mediterranean dietary pattern and musculoskeletal health in children, adolescents, and adults: Systematic review and evidence map. Nutr. Rev. 2017, 75, 830–857. [Google Scholar] [CrossRef] [PubMed]
- Domaradzki, J. Congruence between physical activity patterns and dietary patterns inferred from analysis of sex differences in lifestyle behaviors of late adolescents from Poland: Cophylogenetic approach. Nutrients 2023, 15, 608. [Google Scholar] [CrossRef] [PubMed]
- Godala, M.; Krzyżak, M.; Maślach, D.; Gaszyńska, E. Relationship between dietary behaviors and physical activity and the components of metabolic syndrome: A case-control study. Int. J. Environ. Res. Public Health 2022, 19, 6562. [Google Scholar] [CrossRef] [PubMed]
- Domaradzki, J. The discriminant power of specific physical activity and dietary behaviors to distinguish between lean, normal and excessive fat groups in late adolescents. Nutrients 2023, 15, 1230. [Google Scholar] [CrossRef] [PubMed]
- Lake, A.A.; Mathers, J.C.; Rugg-Gunn, A.J.; Adamson, A.J. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): The ASH30 Study. J. Public Health 2006, 28, 10–16. [Google Scholar] [CrossRef] [PubMed]
- García-Cabrera, S.; Herrera Fernández, N.; Rodríguez Hernández, C.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. KIDMED test: Prevalence of low adherence to the Mediterranean diet in children and young: A systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Oberklaid, F.; Amos, D.; Liu, C.; Jarman, F.; Sanson, A.; Prior, M. “Growing pains”: Clinical and behavioral correlates in a community sample. J. Dev. Behav. Pediatr. 1997, 18, 102–106. [Google Scholar] [CrossRef] [PubMed]
- De Inocencio, J. Epidemiology of musculoskeletal pain in primary care. Arch. Dis. Child. 2004, 89, 431–434. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, G.J.; van den Heuvel, M.M.; Bindels, P.J.E.; Bierma-Zeinstra, S.M.A.; van Middelkoop, M. Musculoskeletal pain in 13-year-old children: The Generation R Study. Pain 2024, 165, 1806–1813. [Google Scholar] [CrossRef] [PubMed]
- Athnaiel, O.; Cantillo, S.; Paredes, S.; Knezevic, N.N. The role of sex hormones in pain-related conditions. Int. J. Mol. Sci. 2023, 24, 1866. [Google Scholar] [CrossRef] [PubMed]
- Vierhausl, M.; Lohaus, A.; Schmitz, A.-K. Sex, gender, coping, and self-efficacy: Mediation of sex differences in pain perception in children and adolescents. Eur. J. Pain 2011, 15, 621.e1–621.e8. [Google Scholar] [CrossRef] [PubMed]
- Lehman, P.J.; Carl, R.L. Growing pains: When to be concerned. Sports Health 2017, 9, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Baxter, M.P.; Dulberg, C. “Growing pains” in childhood: A proposal for treatment. J. Pediatr. Orthop. 1988, 8, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.M.; Hashkes, P.J. Growing pains: A noninflammatory pain syndrome of early childhood. Nat. Clin. Pract. Rheumatol. 2008, 4, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Martínez-González, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Cayetano, A.; Becerro, Y.; De Mena, J.; Sánchez, A.; Pérez, S. Nutrición infantil, actividad física y adherencia a la dieta mediterránea en alumnos de educación primaria. J. Sport Health Res. 2021, 13, 259–270. [Google Scholar]
- Ayechu, A.; Durá, T. Quality of dietary habits (adherence to a Mediterranean diet) in pupils of compulsory secondary education. An. Sist. Sanit. Navar. 2010, 33, 35–42. [Google Scholar]
- Rosi, A.; Scazzina, F.; Giampieri, F.; Álvarez-Córdova, L.; Abdelkarim, O.; Ammar, A.; Aly, M.; Frias-Toral, E.; Pons, J.; Vázquez-Araújo, L.; et al. Lifestyle factors associated with children’s and adolescents’ adherence to the Mediterranean diet living in Mediterranean countries: The DELICIOUS project. Nutrients 2024, 17, 26. [Google Scholar] [CrossRef] [PubMed]
- Casini, I.; Ladisa, V.; Clemente, L.; Delussi, M.; Rostanzo, E.; Peparini, S.; Aloisi, A.M.; de Tommaso, M. A personalized Mediterranean diet improves pain and quality of life in patients with fibromyalgia. Pain Ther. 2024, 13, 609–620. [Google Scholar] [CrossRef] [PubMed]
- Ortolá, R.; García-Esquinas, E.; Sotos-Prieto, M.; Struijk, E.A.; Caballero, F.F.; Lopez-Garcia, E.; Rodríguez-Artalejo, F. Mediterranean diet and changes in frequency, severity, and localization of pain in older adults: The Seniors-ENRICA cohorts. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Yüksel, A.; Yilmaz Önal, H. Relationship between the presence of chronic pain and adherence to the Mediterranean diet in university students. J. Basic Clin. Health Sci. 2023, 7, 660–670. [Google Scholar] [CrossRef]
- Khoury, N.; Martínez, M.Á.; Garcidueñas-Fimbres, T.E.; Pastor-Villaescusa, B.; Leis, R.; De Las Heras-Delgado, S.; Miguel-Berges, M.L.; Navas-Carretero, S.; Portoles, O.; Pérez-Vega, K.A.; et al. Ultraprocessed food consumption and cardiometabolic risk factors in children. JAMA Netw. Open. 2024, 7, e2411852. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Iglesias, R.; Álvarez-Pereira, S.; Tardón, A.; Fernández-García, B.; Iglesias-Gutiérrez, E. Adherence to the Mediterranean diet in a school population in the Principality of Asturias (Spain): Relationship with physical activity and body weight. Nutrients 2021, 13, 1507. [Google Scholar] [CrossRef] [PubMed]
- Patil, A.; Singh, N. From the plate to the mind: How children’s eating habits affect their physical and mental health. J. Neurol. Psychiatr. Ment. Health Nurs. 2023, 5, 40–53. [Google Scholar] [CrossRef]
- Dudley, D.A.; Cotton, W.G.; Peralta, L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Jagim, A.R.; Kerksick, C.M. Creatine supplementation in children and adolescents. Nutrients 2021, 13, 664. [Google Scholar] [CrossRef] [PubMed]
- Blancquaert, L.; Everaert, I.; Derave, W. Beta-alanine supplementation, muscle carnosine and exercise performance. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Claus, G.M.; Redkva, P.E.; Brisola, G.M.P.; Malta, E.S.; De Araujo Bonetti De Poli, R.; Miyagi, W.E.; Zagatto, A.M. Beta-alanine supplementation improves throwing velocities in repeated sprint ability and 200-m swimming performance in young water polo players. Pediatr. Exerc. Sci. 2017, 29, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Martin-Bautista, E.; Martin-Matillas, M.; Martin-Lagos, J.A.; Miranda-Leon, M.T.; Muñoz-Torres, M.; Ruiz-Requena, E.; Rivero, M.; Quer, J.; Puigdueta, I.; Campoy, C. A nutritional intervention study with hydrolyzed collagen in pre-pubertal Spanish children: Influence on bone modeling biomarkers. J. Pediatr. Endocrinol. Metab. 2011, 24, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Clifford, T.; Ventress, M.; Allerton, D.M.; Stansfield, S.; Tang, J.C.Y.; Fraser, W.D.; Vanhoecke, B.; Prawitt, J.; Stevenson, E. The effects of collagen peptides on muscle damage, inflammation and bone turnover following exercise: A randomized, controlled trial. Amino Acids 2019, 51, 691–704. [Google Scholar] [CrossRef] [PubMed]
- Koyama, Y. Effects of collagen ingestion and their biological significance. J. Nutr. Food Sci. 2016, 6, 504. [Google Scholar]

| 8–12 Years (N = 242) | 13–17 Years (N = 674) | |
|---|---|---|
| Males, n (%) | 128 (52.9) | 344 (51.0) |
| Females, n (%) | 114 (47.1) | 330 (49.0) |
| BMI (kg/m2), mean | 18.2 | 20.1 |
| Practiced sport a (hours), mean ± SD | 3.7 ± 1.1 | 7.2 ± 1.2 |
| Use of nutritional supplements, n (%) | 0 (0%) | 52 (7.7%) |
| Participants experiencing pain b, n (%) | 190 (78.51) | 630 (93.47) |
| Use of analgesics c, n (%) | 23 (9.5) | 102 (15.1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elvira-Aranda, C.; Pérez-Turpin, J.A.; Suárez-Llorca, C.; Pérez, M.; De-Castellar, R. Growing Pains and Dietary Habits in Young Athletes: A Cross-Sectional Survey. Nutrients 2025, 17, 2384. https://doi.org/10.3390/nu17142384
Elvira-Aranda C, Pérez-Turpin JA, Suárez-Llorca C, Pérez M, De-Castellar R. Growing Pains and Dietary Habits in Young Athletes: A Cross-Sectional Survey. Nutrients. 2025; 17(14):2384. https://doi.org/10.3390/nu17142384
Chicago/Turabian StyleElvira-Aranda, Carlos, José Antonio Pérez-Turpin, Concepción Suárez-Llorca, Maite Pérez, and Roser De-Castellar. 2025. "Growing Pains and Dietary Habits in Young Athletes: A Cross-Sectional Survey" Nutrients 17, no. 14: 2384. https://doi.org/10.3390/nu17142384
APA StyleElvira-Aranda, C., Pérez-Turpin, J. A., Suárez-Llorca, C., Pérez, M., & De-Castellar, R. (2025). Growing Pains and Dietary Habits in Young Athletes: A Cross-Sectional Survey. Nutrients, 17(14), 2384. https://doi.org/10.3390/nu17142384




