Life’s Simple 7 and Risk of Peripheral Artery Disease: Results from the PREDIMED Study and an Updated Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. End-Point
2.3. Life’s Simple 7
2.4. Other Covariates
2.5. Statistical Analysis
2.6. Ethics
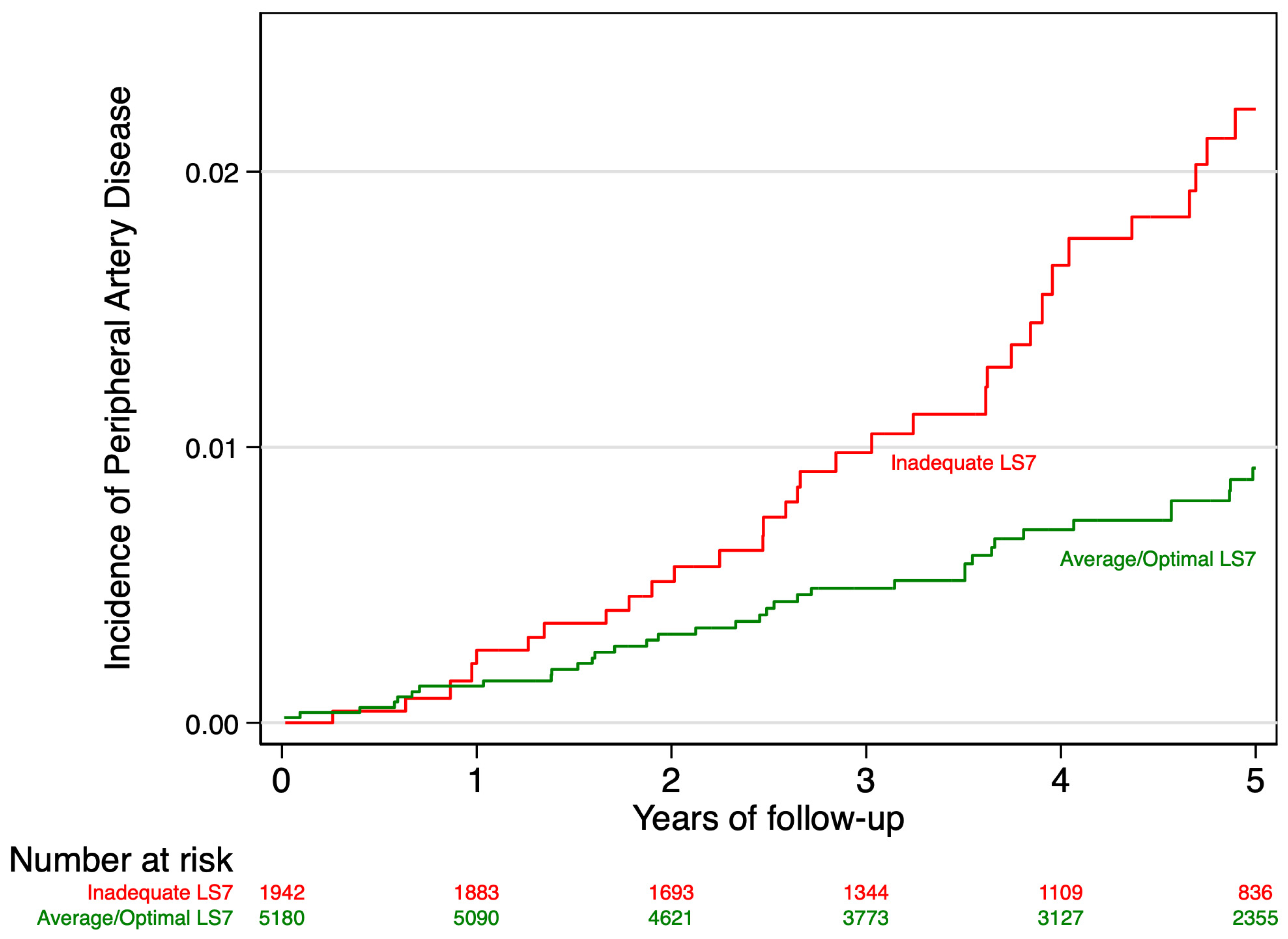
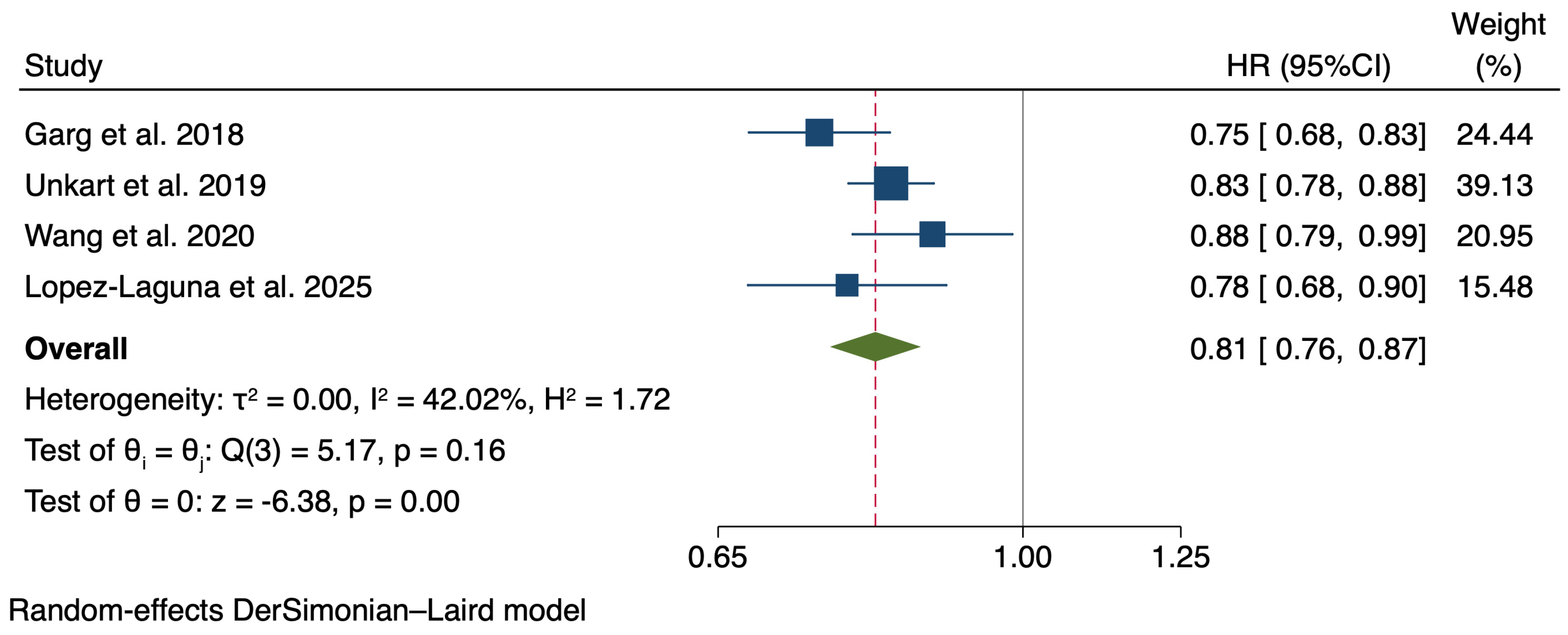
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD 2019 Peripheral Artery Disease Collaborators. Global burden of peripheral artery disease and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2023, 382, 1329–1340. [Google Scholar]
- Lin, J.; Chen, Y.; Jiang, N.; Li, Z.; Zu, S. Burden of Peripheral Artery Disease and Its Attributable Risk Factors in 204 Countries and Territories from 1990 to 2019. Front. Cardiovasc. Med. 2022, 9, 868370. [Google Scholar] [CrossRef] [PubMed]
- Aaron, W.; Aday, K.M. Epidemiology of Peripheral Artery Disease and Polyvascular Disease. Circ. Res. 2021, 176, 139–148. [Google Scholar]
- Berger, J.S.; Hochman, J.; Lobach, I.; Adelman, M.A.; Riles, T.S.; Rockman, C.B. Modifiable risk factor burden and the prevalence of peripheral artery disease in different vascular territories. J. Vasc. Surg. 2013, 58, 673–681.e1. [Google Scholar] [CrossRef]
- Ruiz-Canela, M.; Martínez-González, M.A. Lifestyle and dietary risk factors for peripheral artery disease. Circ. J. 2014, 78, 553–559. [Google Scholar] [CrossRef]
- Eraso, L.H.; Fukaya, E.; Mohler, E.R.; Xie, D.; Sha, D.; Berger, J.S. Peripheral arterial disease, prevalence and cumulative risk factor profile analysis. Eur. J. Prev. Cardiol. 2014, 21, 704–711. [Google Scholar] [CrossRef]
- López-Laguna, N.; Martínez-González, M.A.; Toledo, E.; Babio, N.; Sorlí, J.V.; Ros, E.; Muñoz, M.Á.; Estruch, R.; Lapetra, J.; Muñoz-Bravo, C.; et al. Risk of peripheral artery disease according to a healthy lifestyle score: The PREDIMED study. Atherosclerosis 2018, 275, 133–140. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and Setting National Goals for Cardiovascular Health Promotion and Disease Reduction the American Heart Association’s Strategic Impact Goal Through 2020. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Te Hoonte, F.; Spronk, M.; Sun, Q.; Wu, K.; Fan, S.; Wang, Z.; Bots, M.L.; Van der Schouw, Y.T.; Uijl, A.; Vernooij, R.W.M. Ideal cardiovascular health and cardiovascular-related events: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2024, 31, 966–985. [Google Scholar] [CrossRef]
- Díez-Espino, J.; Buil-Cosiales, P.; Babio, N.; Toledo, E.; Corella, D.; Ros, E.; Fitó, M.; Gómez-Gracia, E.; Estruch, R.; Fiol, M.; et al. Impact of Life’s Simple 7 on the incidence of major cardiovascular events in high-risk Spanish adults in the PREDIMED study cohort. Rev. Esp. Cardiol. 2020, 73, 205–211. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Ros, E.; Covas, M.I.; Fiol, M.; Wärnberg, J.; Arós, F.; Ruíz-Gutiérrez, V.; Lamuela-Raventós, R.M.; et al. Cohort profile: Design and methods of the PREDIMED study. Int. J. Epidemiol. 2012, 41, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salvadó, J.S.; Covas, M.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2018, 34, 1279–1290. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Canela, M.; Estruch, R.; Corella, D.; Salas-Salvadó, J.; Martínez-González, M.A. Association of Mediterranean diet with peripheral artery disease: The PREDIMED randomized trial. JAMA 2014, 311, 415–417, Erratum in: JAMA 2018, 320, 2272. https://doi.org/10.1001/jama.2018.16553. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Fernández-Ballart, J.D.; Piñol, J.L.; Zazpe, I.; Corella, D.; Carrasco, P.; Toledo, E.; Perez-Bauer, M.; Martínez-González, M.Á.; Salas-Salvadó, J.; Martín-Moreno, J.M. Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br. J. Nutr. 2010, 103, 1808–1816. [Google Scholar] [CrossRef]
- Collins, T.C.; Slovut, D.P.; Newton, R., Jr.; Johnson, W.D.; Larrivee, S.; Patterson, J.; Johnston, J.A.; Correa, A. Ideal cardiovascular health and peripheral artery disease in African Americans: Results from the Jackson Heart Study. Prev. Med. Rep. 2017, 7, 20–25. [Google Scholar] [CrossRef]
- Garg, P.K.; O’Neal, W.T.; Mok, Y.; Heiss, G.; Coresh, J.; Matsushita, K. Life’s Simple 7 and Peripheral Artery Disease Risk: The Atherosclerosis Risk in Communities Study. Am. J. Prev. Med. 2018, 55, 642–649. [Google Scholar] [CrossRef]
- Unkart, J.T.; Allison, M.A.; Criqui, M.H.; McDermott, M.M.; Wood, A.C.; Folsom, A.R.; Lloyd-Jones, D.; Rasmussen-Torvik, L.J.; Allen, N.; Burke, G.; et al. Life’s Simple 7 and Peripheral Artery Disease: The Multi-Ethnic Study of Atherosclerosis. Am. J. Prev. Med. 2019, 56, 262–270. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, Q.; Wang, A.; Wu, S.; Zhao, X. Ideal Cardiovascular Health Metrics on the New Occurrence of Peripheral Artery Disease: A Prospective Cohort Study in Northern China. Sci. Rep. 2020, 10, 9660. [Google Scholar] [CrossRef]
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; I Gonzalez-Requero, A.; I Perez-Caballero, A.; Yubero-Serrano, E.M.; et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): A randomised controlled trial. Lancet 2022, 399, 1876–1885. [Google Scholar] [CrossRef]
- Vita, J.A.; Keaney, J.F., Jr. Endothelial function: A barometer for cardiovascular risk? Circulation 2002, 106, 640–642. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, S.S.; Fiore, V. Oxidative stress biomarkers in peripheral arterial disease: Hype or hope? Clin. Biochem. 2017, 50, 656–664. [Google Scholar] [CrossRef]
- Brevetti, G.; Giugliano, G.; Brevetti, L.; Hiatt, W.R. Inflammation in peripheral artery disease. Circulation 2010, 122, 1862–1875. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Mediterranean dietary pattern, inflammation and endothelial function: A systematic review and meta-analysis of intervention trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939. [Google Scholar] [CrossRef]
- Urpi-Sarda, M.; Casas, R.; Sacanella, E.; Corella, D.; Andrés-Lacueva, C.; Llorach, R.; Garrabou, G.; Cardellach, F.; Sala-Vila, A.; Ros, E.; et al. The 3-Year Effect of the Mediterranean Diet Intervention on Inflammatory Biomarkers Related to Cardiovascular Disease. Biomedicines 2021, 9, 862. [Google Scholar] [CrossRef]
| Component | Inadequate (0 Points) | Average (1 Point) | Optimal (2 Points) |
|---|---|---|---|
| 1. Smoking Status | Current smoker | Former smoker who quit within the past year | Never smoker or former smoker who quit > 1 year ago |
| 2. Body Mass Index (BMI) | ≥30 kg/m2 | 25–29.9 kg/m2 | <25 kg/m2 |
| 3. Physical Activity | ≤10 METs-min/wk | 11–239 METs-min/wk | ≥240 METs-min/wk |
| 4. Blood Pressure | Systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg | Systolic BP 120–139 mmHg or diastolic BP 80–89 mmHg | Systolic BP < 120 mmHg and diastolic BP < 80 mmHg, without antihypertensive medication |
| 5. Total Cholesterol | ≥240 mg/dL | 200–239 mg/dL | <200 mg/dL, without lipid-lowering medication |
| 6. Glucose Metabolism | Fasting glucose ≥ 120 mg/dL | Fasting glucose 100–119 mg/dL | Fasting glucose < 100 mg/dL, without insulin or oral hypoglycemic medication |
| 7. Mediterranean Diet Adherence | Low adherence (MEDAS score ≤ 6) | Moderate adherence (MEDAS score 7–9) | High adherence (MEDAS score ≥ 10) |
| Inadequate (0–5) | Average (6–8) | Optimal (9–14) | |
|---|---|---|---|
| N | 1941 | 4173 | 1008 |
| Age. years (SD) | 66.4 (6.5) | 67.1 (6.1) | 67.3 (6.1) |
| Sex (% Women) | 1007 (51.9) | 2507 (60.1) | 581 (57.6) |
| Level of studies (% Primary or less) | 1511 (77.9) | 3286 (78.7) | 743 (73.7) |
| Work status | |||
| Employed | 288 (14.8) | 491 (11.8) | 115 (11.4) |
| Unpaid domestic work | 571 (29.4) | 1402 (33.6) | 315 (31.3) |
| Retired | 1004 (51.7) | 2150 (51.5) | 555 (55.1) |
| Other | 78 (4.0%) | 130 (3.1%) | 23 (2.3%) |
| LS7 metrics (SD) | 4.3 (0.9) | 6.7 (0.8) | 9.4 (0.6) |
| Total cholesterol (mg/dL) (SD) | 208.0 (38.6) | 212.4 (34.1) | 209.8 (29.8) |
| SBP (mmHg) (SD) | 153.9 (18.2) | 148.3 (18.6) | 140.0 (17.9) |
| DBP (mmHg) (SD) | 84.4 (9.9) | 82.8 (10.0) | 79.6 (9.9) |
| Glucose (mg/dL) (SD) | 139.0 (41.2) | 118.6 (37.1) | 103.4 (28.5) |
| Hypercholesterolemia (%) | 1517 (78.2) | 2920 (70.0) | 701 (69.5) |
| Hypertension (%) | 1601 (82.5) | 3489 (83.6) | 799 (79.3) |
| Statins (%) | 877 (44.6) | 1614 (38.7) | 380 (37.7) |
| Cardiovascular treatments * (%) | 1406 (72.4) | 2926 (70.1) | 650 (64.5) |
| Physical activity (METs-min/d) (SD) | 146.3 (192.0) | 242.2 (237.8) | 350.6 (268.9) |
| Body Mass Index (SD) | 31.7 (3.7) | 29.8 (3.7) | 27.3 (2.9) |
| MEDAS (0 to 14 points) (SD) | 7.7 (1.9) | 8.8 (1.8) | 9.9 (1.6) |
| Smoking (%) | |||
| Never | 934 (48.1) | 2753 (66.0) | 682 (67.7) |
| Current smoker | 587 (30.2) | 384 (9.2) | 23 (2.3) |
| Former smoker | 420 (21.6) | 1036 (24.8) | 303 (30.1) |
| Height. meters (SD) | 1.61 (0.1) | 1.60 (0.1) | 1.60 (0.1) |
| Waist circumference (centimeters) (SD) | 105.3 (9.7) | 99.7 (10.2) | 94.1 (9.5) |
| Total energy intake (Kcal/d) (SD) | 2235 (589) | 2240 (545) | 2297 (518) |
| Alcohol (g/d) (SD) | 9.4 (16.0) | 8.1 (13.8) | 7.7 (11.7) |
| Life’s Simple 7 Categories | ||||
|---|---|---|---|---|
| Inadequate (0–5) | Average (6–8) | Optimal (9–14) | Per 1-Unit Increase | |
| N | 1941 | 4173 | 1008 | |
| Cases of PAD | 40 | 40 | 7 | |
| Incidence rate (95% CI), 1000 p-yr | 4.81 (3.53–6.55) | 2.16 (1.58–2.94) | 1.57 (0.75–3.30) | |
| Crude HR (95% CI) | 1 (ref) | 0.45 (0.29–0.69) | 0.33 (0.15–0.73) | 0.82 (0.73–0.92) |
| Adjusted HR (95% CI), model 1 | 1 (ref) | 0.40 (0.25–0.64) | 0.29 (0.12–0.67) | 0.80 (0.72–0.90) |
| Adjusted HR (95% CI), model 2 | 1 (ref) | 0.37 (0.22–0.61) | 0.25 (0.10–0.65) | 0.78 (0.68–0.90) |
| Life’s Simple 7 Component | Cases/N | HR (95% CI) |
|---|---|---|
| Smoking | ||
| Inadequate (current smoker) | 26/994 | 1 (ref) |
| Average (quit ≤ 12 months) | 4/197 | 0.78 (0.27–2.24) |
| Optimum (never/quit > 12 months) | 57/5931 | 0.53 (0.32–0.86) |
| Body Mass Index | ||
| Inadequate (≥30) | 34/3344 | 1 (ref) |
| Average (25−29.9) | 43/3240 | 0.97 (0.61–1.55) |
| Optimum (<25) | 10/538 | 1.47 (0.70–3.09) |
| MEDAS score | ||
| Inadequate (0−6 points) | 15/1096 | 1 (ref) |
| Average (7–10 points) | 53/3993 | 0.89 (0.49–1.59) |
| Optimum (10–14 points) | 19/2033 | 0.70 (0.34–1.42) |
| Physical activity | ||
| Inadequate (<10 METs-h/d) | 9/966 | 1 (ref) |
| Average (10 to <240 METs-h/d) | 52/3592 | 0.94 (0.45–1.96) |
| Optimum (≥240 METs-h/d) | 26/2564 | 0.44 (0.20–0.98) |
| Total cholesterol | ||
| Inadequate (≥240 mg/dL) | 18/1322 | 1 (ref) |
| Average (200−239 mg/dL) | 37/3148 | 1.01 (0.57–1.81) |
| Optimum (<200 mg/dL) | 18/929 | 1.15 (0.57–2.34) |
| Glucose | ||
| Inadequate (≥120 mg/dL) | 52/2941 | 1 (ref) |
| Average (100 to <120 mg/d) | 16/1571 | 0.48 (0.27–0.85) |
| Optimum (<100 mg/dL) | 16/2448 | 0.35 (0.20–0.63) |
| Blood pressure | ||
| Inadequate (SBP ≥ 140 or DBP ≥ 90 mmHg) | 63/4816 | 1 (ref) |
| Average (SBP 120−139 mmHg, DBP 80−89 mmHg) | 21/1981 | 1.06 (0.65–1.75) |
| Optimum (SBP < 120 mmHg and DBP < 80 mmHg) | 1/159 | 0.64 (0.08–4.86) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Laguna, N.; Toledo, E.; Hershey, M.S.; Babio, N.; Sorlí, J.V.; Ros, E.; Muñoz, M.Á.; Estruch, R.; Lapetra, J.; Muñoz-Bravo, C.; et al. Life’s Simple 7 and Risk of Peripheral Artery Disease: Results from the PREDIMED Study and an Updated Meta-Analysis. Nutrients 2025, 17, 2058. https://doi.org/10.3390/nu17132058
López-Laguna N, Toledo E, Hershey MS, Babio N, Sorlí JV, Ros E, Muñoz MÁ, Estruch R, Lapetra J, Muñoz-Bravo C, et al. Life’s Simple 7 and Risk of Peripheral Artery Disease: Results from the PREDIMED Study and an Updated Meta-Analysis. Nutrients. 2025; 17(13):2058. https://doi.org/10.3390/nu17132058
Chicago/Turabian StyleLópez-Laguna, Nieves, Estefanía Toledo, María S. Hershey, Nancy Babio, José V. Sorlí, Emilio Ros, Miguel Ángel Muñoz, Ramón Estruch, José Lapetra, Carlos Muñoz-Bravo, and et al. 2025. "Life’s Simple 7 and Risk of Peripheral Artery Disease: Results from the PREDIMED Study and an Updated Meta-Analysis" Nutrients 17, no. 13: 2058. https://doi.org/10.3390/nu17132058
APA StyleLópez-Laguna, N., Toledo, E., Hershey, M. S., Babio, N., Sorlí, J. V., Ros, E., Muñoz, M. Á., Estruch, R., Lapetra, J., Muñoz-Bravo, C., Fiol, M., Bautista-Castaño, I., Pinto, X., Ortega-Azorín, C., Hernando-Redondo, J., Salas-Salvadó, J., Tojal-Sierra, L., Martínez-González, M. A., & Ruiz-Canela, M. (2025). Life’s Simple 7 and Risk of Peripheral Artery Disease: Results from the PREDIMED Study and an Updated Meta-Analysis. Nutrients, 17(13), 2058. https://doi.org/10.3390/nu17132058











