A Patented Dietary Supplement (Hydroxy-Methyl-Butyrate, Carnosine, Magnesium, Butyrate, Lactoferrin) Is a Promising Therapeutic Target for Age-Related Sarcopenia through the Regulation of Gut Permeability: A Randomized Controlled Trial
Abstract
1. Introduction
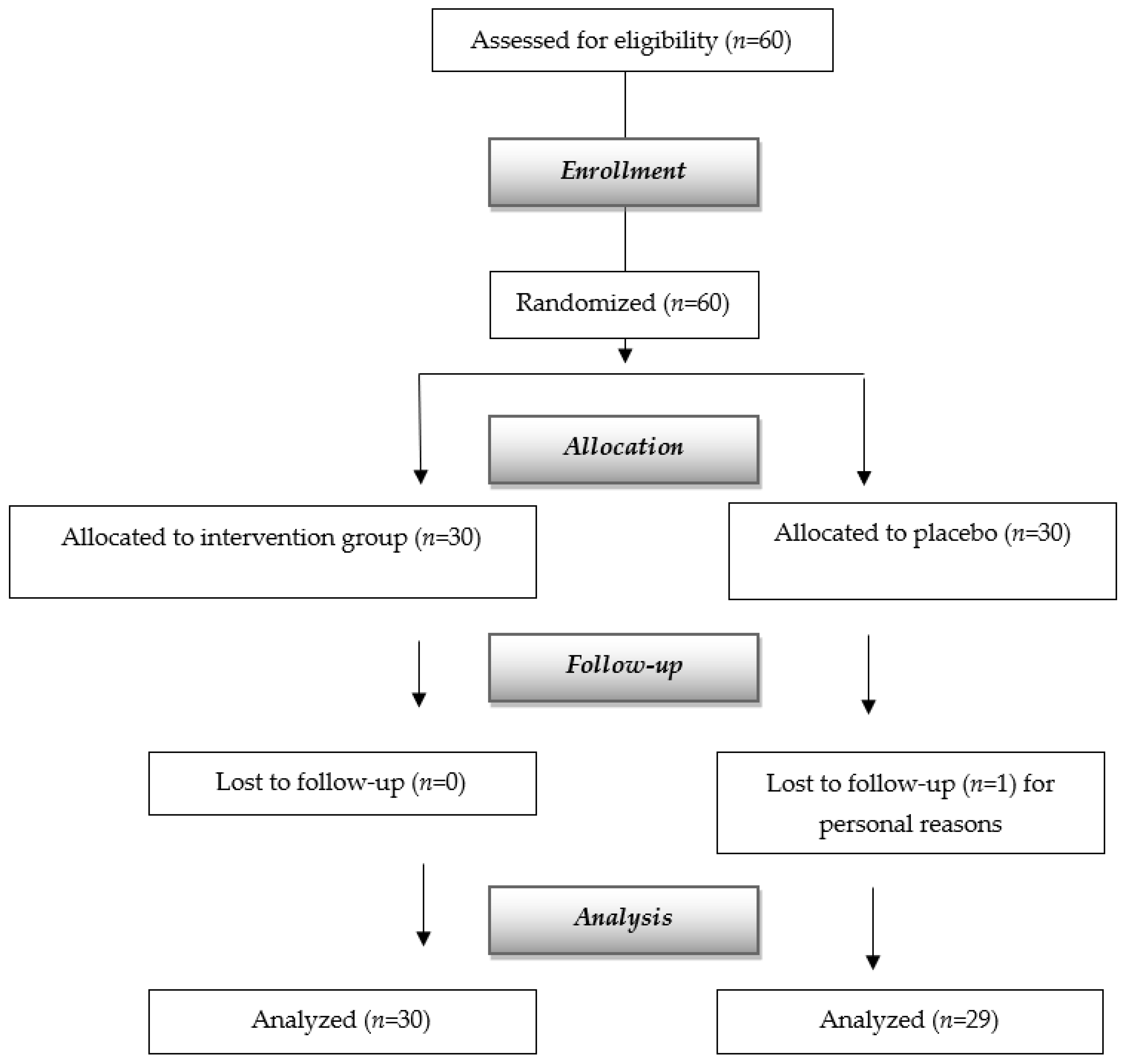
2. Materials and Methods
2.1. Population
2.2. Standard Protocol Approval, Registration, and Patient Consent
2.3. Study Design and Sample Size
2.4. Nutritional Assessment and Interventions
2.5. Biochemical Parameters
2.6. Anthropometric Measurements
2.7. Body Composition Assessment
2.8. Muscle Strength Evaluation
2.9. Physical Performance Assessment
2.10. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anker, S.D.; Morley, J.E.; von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia. Sarcopenia Muscle 2016, 7, 512–514. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Larsson, S.C. Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism 2023, 144, 155533. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Nouvenne, A.; Cerundolo, N.; Catania, P.; Prati, B.; Tana, C.; Meschi, T. Gut Microbiota, Muscle Mass and Function in Aging: A Focus on Physical Frailty and Sarcopenia. Nutrients 2019, 11, 1633. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, P.W.; Jeffery, I.B. Gut microbiota and aging. Science 2015, 350, 1214–1215. [Google Scholar] [CrossRef] [PubMed]
- Odamaki, T.; Kato, K.; Sugahara, H.; Hashikura, N.; Takahashi, S.; Xiao, J.Z.; Abe, F.; Osawa, R. Age-related changes in gut microbiota composition from newborn to centenarian: A cross-sectional study. BMC Microbiol. 2016, 16, 90. [Google Scholar] [CrossRef] [PubMed]
- Claesson, M.J.; Jeffery, I.B.; Conde, S.; Power, S.E.; O’Connor, E.M.; Cusack, S.; Harris, H.M.B.; Coakley, M.; Lakshminarayanan, B.; O’Sullivan, O.; et al. Gut microbiota composition correlates with diet and health in the elderly. Nature 2012, 488, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Bindels, L.B.; Delzenne, N.M. Muscle wasting: The gut microbiota as a new therapeutic target? Int. J. Biochem. Cell Biol. 2013, 45, 2186–2190. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Montoya, I.; Correa-Pérez, A.; Abraha, I.; Soiza, R.L.; Cherubini, A.; O’Mahony, D.; Cruz-Jentoft, A.J. Nonpharmacological interventions to treat physical frailty and sarcopenia in older patients: A systematic overview—The SENATOR Project ONTOP Series. Clin. Interv. Aging 2017, 12, 721–740. [Google Scholar] [CrossRef]
- Rondanelli, M.; Gasparri, C.; Barrile, G.C.; Battaglia, S.; Cavioni, A.; Giusti, R.; Mansueto, F.; Moroni, A.; Nannipieri, F.; Patelli, Z.; et al. Effectiveness of a Novel Food Composed of Leucine, Omega-3 Fatty Acids and Probiotic Lactobacillus paracasei PS23 for the Treatment of Sarcopenia in Elderly Subjects: A 2-Month Randomized Double-Blind Placebo-Controlled Trial. Nutrients 2022, 14, 4566. [Google Scholar] [CrossRef]
- Frisancho, A.R. New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am. J. Clin. Nutr. 1984, 40, 808–819. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, A.; De Lucia Rolfe, E.; Sleigh, A.; Kivisild, T.; Behbehani, K.; Wareham, N.J.; Brage, S.; Mohammad, T. Validity of visceral adiposity estimates from DXA against MRI in Kuwaiti men and women. Nutr. Diabetes 2017, 7, e238. [Google Scholar] [CrossRef] [PubMed]
- Walowski, C.O.; Braun, W.; Maisch, M.J.; Jensen, B.; Peine, S.; Norman, K.; Müller, M.J.; Bosy-Westphal, A. Reference values for skeletal muscle mass—Current concepts and methodological considerations. Nutrients 2020, 12, 755. [Google Scholar] [CrossRef]
- Moon, J.J.; Park, S.-G.; Ryu, S.M.; Park, C.-H. New Skeletal Muscle Mass Index in Diagnosis of Sarcopenia. J. Bone Metab. 2018, 25, 15. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed Up Go: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Borg, G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand. J. Work. Environ. Health 1990, 16, 55–58. [Google Scholar] [CrossRef]
- Engelen, M.P.K.J.; Deutz, N.E.P. Is β-hydroxy β-methylbutyrate an effective anabolic agent to improve outcome in older diseased populations? Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Oktaviana, J.; Zanker, J.; Vogrin, S.; Duque, G. The Effect of β-hydroxy-β-methylbutyrate (HMB) on Sarcopenia and Functional Frailty in Older Persons: A Systematic Review. J. Nutr. Health Aging 2019, 23, 145–150. [Google Scholar] [CrossRef]
- Deutz, N.E.P.; Pereira, S.L.; Hays, N.P.; Oliver, J.S.; Edens, N.K.; Evans, C.M.; Wolfe, R.R. Effect of β-hydroxy-β-methylbutyrate (HMB) on lean body mass during 10 days of bed rest in older adults. Clin. Nutr. 2013, 32, 704–712. [Google Scholar] [CrossRef]
- Holeček, M. Beta-hydroxy-beta-methylbutyrate supplementation and skeletal muscle in healthy and muscle-wasting conditions. J. Cachexia. Sarcopenia Muscle 2017, 8, 529–541. [Google Scholar] [CrossRef]
- Yang, H.; Hou, X.; Xing, L.; Tian, F. Carnosine and bone (Review). Mol. Med. Rep. 2023, 27, 12. [Google Scholar] [CrossRef] [PubMed]
- Stuerenburg, H.J. The Roles of Carnosine in Aging of Skeletal Muscle and in Neuromuscular Diseases. Biochem. Biokhimiia 2000, 65, 862–865. [Google Scholar]
- Furst, T.; Massaro, A.; Miller, C.; Williams, B.T.; LaMacchia, Z.M.; Horvath, P.J. β-Alanine supplementation increased physical performance and improved executive function following endurance exercise in middle aged individuals. J. Int. Soc. Sports Nutr. 2018, 15, 32. [Google Scholar] [CrossRef] [PubMed]
- Cesak, O.; Vostalova, J.; Vidlar, A.; Bastlova, P.; Student, V. Carnosine and Beta-Alanine Supplementation in Human Medicine: Narrative Review and Critical Assessment. Nutrients 2023, 15, 1770. [Google Scholar] [CrossRef] [PubMed]
- Ganapathy, A.; Nieves, J.W. Nutrition and Sarcopenia-What Do We Know? Nutrients 2020, 12, 1755. [Google Scholar] [CrossRef] [PubMed]
- van Dronkelaar, C.; van Velzen, A.; Abdelrazek, M.; van der Steen, A.; Weijs, P.J.M.; Tieland, M. Minerals and Sarcopenia; The Role of Calcium, Iron, Magnesium, Phosphorus, Potassium, Selenium, Sodium, and Zinc on Muscle Mass, Muscle Strength, and Physical Performance in Older Adults: A Systematic Review. J. Am. Med. Dir. Assoc. 2018, 19, 6–11.e3. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.W.; Chen, Y.Y.; Chen, W.L. Association between oral intake magnesium and sarcopenia: A cross-sectional study. BMC Geriatr. 2022, 22, 816. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Berton, L.; Carraro, S.; Bolzetta, F.; De Rui, M.; Perissinotto, E.; Toffanello, E.D.; Bano, G.; Pizzato, S.; Miotto, F.; et al. Effect of oral magnesium supplementation on physical performance in healthy elderly women involved in a weekly exercise program: A randomized controlled trial. Am. J. Clin. Nutr. 2014, 100, 974–981. [Google Scholar] [CrossRef]
- Haran, J.P.; Bucci, V.; Dutta, P.; Ward, D.; McCormick, B. The nursing home elder microbiome stability and associations with age, frailty, nutrition and physical location. J. Med. Microbiol. 2018, 67, 40–51. [Google Scholar] [CrossRef]
- Ticinesi, A.; Mancabelli, L.; Tagliaferri, S.; Nouvenne, A.; Milani, C.; Del Rio, D.; Lauretani, F.; Maggio, M.G.; Ventura, M.; Meschi, T. The Gut-Muscle Axis in Older Subjects with Low Muscle Mass and Performance: A Proof of Concept Study Exploring Fecal Microbiota Composition and Function with Shotgun Metagenomics Sequencing. Int. J. Mol. Sci. 2020, 21, 8946. [Google Scholar] [CrossRef]
- Lv, W.Q.; Lin, X.; Shen, H.; Liu, H.M.; Qiu, X.; Li, B.Y.; Di Shen, W.; Ge, C.L.; Lv, F.Y.; Shen, J.; et al. Human gut microbiome impacts skeletal muscle mass via gut microbial synthesis of the short-chain fatty acid butyrate among healthy menopausal women. J. Cachexia. Sarcopenia Muscle 2021, 12, 1860–1870. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Peng, Z.; Chen, L.; Zhang, Y.; Cheng, Q.; Nüssler, A.K.; Bao, W.; Liu, L.; Yang, W. Prospective Views for Whey Protein and/or Resistance Training Against Age-related Sarcopenia. Aging Dis. 2019, 10, 158–174. [Google Scholar] [CrossRef] [PubMed]
- Berlutti, F.; Pantanella, F.; Natalizi, T.; Frioni, A.; Paesano, R.; Polimeni, A.; Valenti, P. Antiviral properties of lactoferrin--a natural immunity molecule. Molecules 2011, 16, 6992–7012. [Google Scholar] [CrossRef] [PubMed]
- Frioni, A.; Conte, M.P.; Cutone, A.; Longhi, C.; Musci, G.; Di Patti, M.C.B.; Natalizi, T.; Marazzato, M.; Lepanto, M.S.; Puddu, P.; et al. Lactoferrin differently modulates the inflammatory response in epithelial models mimicking human inflammatory and infectious diseases. Biometals 2014, 27, 843–856. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, S.; Naidu, T.A.G.; Betageri, G.V.; Prasadarao, N.V.; Naidu, A.S. Inflammatory responses improve with milk ribonuclease-enriched lactoferrin supplementation in postmenopausal women. Inflamm. Res. 2010, 59, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A. Intestinal permeability and its regulation by zonulin: Diagnostic and therapeutic implications. Clin. Gastroenterol. Hepatol. 2012, 10, 1096–1100. [Google Scholar] [CrossRef] [PubMed]
- Qaisar, R.; Karim, A.; Muhammad, T.; Shah, I.; Iqbal, M.S. The coupling between sarcopenia and COVID-19 is the real problem. Eur. J. Intern. Med. 2021, 93, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Karim, A.; Muhammad, T.; Ustrana, S.; Qaisar, R. Intestinal permeability marker zonulin as a predictor of sarcopenia in chronic obstructive pulmonary disease. Respir. Med. 2021, 189, 106662. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.F.; Goel, R.; Kim, S.; Richards, E.M.; Carter, C.S.; Pepine, C.J.; Raizada, M.K.; Buford, T.W. Intestinal Permeability Biomarker Zonulin is Elevated in Healthy Aging. J. Am. Med. Dir. Assoc. 2017, 18, 810.e1–810.e4. [Google Scholar] [CrossRef]
- Kiani, A.K.; Bonetti, G.; Donato, K.; Bertelli, M. Dietary supplements for intestinal inflammation. J. Prev. Med. Hyg. 2022, 63, E214–E220. [Google Scholar]
- Picca, A.; Fanelli, F.; Calvani, R.; Mulè, G.; Pesce, V.; Sisto, A.; Pantanelli, C.; Bernabei, R.; Landi, F.; Marzetti, E. Gut Dysbiosis and Muscle Aging: Searching for Novel Targets against Sarcopenia. Mediators Inflamm. 2018, 2018, 7026198. [Google Scholar] [CrossRef] [PubMed]
- Buchmann, N.; Fielitz, J.; Spira, D.; König, M.; Norman, K.; Pawelec, G.; Goldeck, D.; Demuth, I.; Steinhagen-Thiessen, E. Muscle Mass and Inflammation in Older Adults: Impact of the Metabolic Syndrome. Gerontology 2022, 68, 989–998. [Google Scholar] [CrossRef]
- Alexopoulos, N.; Katritsis, D.; Raggi, P. Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis 2014, 233, 104–112. [Google Scholar] [CrossRef]
- Dalla Nora, E.; Testoni, L.; Vigna, G.; Di Vece, F.; Passaro, A. Tessuto adiposo e infiammazione sistemica. G. Ital. dell’Arteriosclerosi 2012, 3, 72–83. [Google Scholar]
- Yende, S.; Waterer, G.W.; Tolley, E.A.; Newman, A.B.; Bauer, D.C.; Taaffe, D.R.; Jensen, R.; Crapo, R.; Rubin, S.; Nevitt, M.; et al. Inflammatory markers are associated with ventilatory limitation and muscle dysfunction in obstructive lung disease in well functioning elderly subjects. Thorax 2006, 61, 10–16. [Google Scholar] [CrossRef]
- Dirks, A.J.; Leeuwenburgh, C. Tumor necrosis factor alpha signaling in skeletal muscle: Effects of age and caloric restriction. J. Nutr. Biochem. 2006, 17, 501–508. [Google Scholar] [CrossRef]
- Nicklas, B.J.; Brinkley, T.E. Exercise training as a treatment for chronic inflammation in the elderly. Exerc. Sport Sci. Rev. 2009, 37, 165–170. [Google Scholar] [CrossRef]
- Liao, P.; Zhou, J.; Ji, L.L.; Zhang, Y. Eccentric contraction induces inflammatory responses in rat skeletal muscle: Role of tumor necrosis factor-alpha. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 298, R599–R607. [Google Scholar] [CrossRef]
- Narici, M.V.; Maffulli, N. Sarcopenia: Characteristics, mechanisms and functional significance. Br. Med. Bull. 2010, 95, 139–159. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Bruunsgaard, H. Possible beneficial role of exercise in modulating low-grade inflammation in the elderly. Scand. J. Med. Sci. Sports 2003, 13, 56–62. [Google Scholar] [CrossRef]
- Hamada, K.; Vannier, E.; Sacheck, J.M.; Witsell, A.L.; Roubenoff, R. Senescence of human skeletal muscle impairs the local inflammatory cytokine response to acute eccentric exercise. FASEB J. 2005, 19, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Reid, M.B.; Li, Y.P. Tumor necrosis factor-alpha and muscle wasting: A cellular perspective. Respir. Res. 2001, 2, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Bano, G.; Trevisan, C.; Carraro, S.; Solmi, M.; Luchini, C.; Stubbs, B.; Manzato, E.; Sergi, G.; Veronese, N. Inflammation and sarcopenia: A systematic review and meta-analysis. Maturitas 2017, 96, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Zupo, R.; Moroni, A.; Castellana, F.; Gasparri, C.; Catino, F.; Lampignano, L.; Perna, S.; Clodoveo, M.L.; Sardone, R.; Rondanelli, M. A Machine-Learning Approach to Target Clinical and Biological Features Associated with Sarcopenia: Findings from Northern and Southern Italian Aging Populations. Metabolites 2023, 13, 565. [Google Scholar] [CrossRef]


| Variable | Placebo Group (n = 29) | Intervention Group (n = 30) | Total (n = 59) | p-Value between Groups |
|---|---|---|---|---|
| Diseases (n) | 4.17 ± 1.37 | 4.10 ± 1.13 | 4.14 ± 1.24 | 0.825 |
| Medicines (n) | 4.10 ± 1.24 | 4.00 ± 1.02 | 4.05 ± 1.12 | 0.726 |
| Height (m) | 1.55 ± 0.08 | 1.59 ± 0.09 | 1.57 ± 0.09 | 0.055 |
| Weight (kg) | 51.59 ± 8.84 | 53.26 ± 8.35 | 52.44 ± 8.56 | 0.459 |
| BMI (kg/m2) | 21.12 ± 2.21 | 20.87 ± 2.06 | 20.99 ± 2.12 | 0.651 |
| Handgrip test (kg) | 17.41 ± 4.30 | 17.27 ± 3.41 | 17.34 ± 3.84 | 0.885 |
| Chair test (s) | 24.52 ± 5.50 | 25.11 ± 6.73 | 24.82 ± 6.11 | 0.717 |
| SPPB test (score) | 4.48 ± 0.51 | 4.63 ± 1.10 | 4.56 ± 0.86 | 0.504 |
| Walking speed (m/s) | 1.92 ± 0.28 | 1.81 ± 0.32 | 1.86 ± 0.30 | 0.164 |
| SMI | 5.36 ± 0.42 | 5.50 ± 0.57 | 5.43 ± 0.50 | 0.277 |
| Fat Mass (kg) | 15.78 ± 6.92 | 14.66 ± 5.59 | 15.21 ± 6.25 | 0.498 |
| VAT (g) | 757.61 ± 236.94 | 739.13 ± 378.61 | 748.21 ± 314.42 | 0.824 |
| CRP (mg/dL) | 1.43 ± 1.47 | 0.99 ± 1.33 | 1.21 ± 1.41 | 0.228 |
| Zonulin (ng/mL) | 2.80 ± 0.22 | 2.82 ± 0.22 | 2.81 ± 0.22 | 0.686 |
| TNF-alfa (pg/mL) | 12.87 ± 4.81 | 12.68 ± 4.50 | 12.78 ± 4.61 | 0.877 |
| Variable | Placebo Group (n = 29); Intra-Group Δ Change (CI 95%) | Intervention Group (n = 30); Intra-Group Δ Change (CI 95%) | Effects between Groups (Intervention Minus Placebo) Δ Change (CI 95%) | p-Value between Groups * |
|---|---|---|---|---|
| Weight (kg) | −1.31 (−1.62; −0.99) | 2.13 (1.85; 2.47) | 3.47 (3.02; 3.92) | 0.001 |
| BMI (kg/m2) | −0.37 (−0.67; −0.06) | 0.91 (0.60; 1.21) | 1.27 (0.83; 1.71) | 0.001 |
| Handgrip test (kg) | −2.76 (−4.13; −1.39) | 6.17 (4.82; 7.51) | 8.92 (6.68; 10.87) | 0.001 |
| Chair test (s) | 1.99 (0.91; 3.06) | −5.41 (−6.47; −4.35) | −7.40 (−8.93; −5.84) | 0.001 |
| SPPB test (score) | 0.38 (0.10; 0.86) | 3.33 (2.86; 3.81) | 2.96 (2.26; 3.64) | 0.001 |
| Walking speed (m/s) | 0.11 (0.05; 0.17) | −0.22 (−0.28; −0.16) | −0.33 (−0.42; −0.24) | 0.001 |
| SMI | −0.22 (−0.39; −0.05) | 0.80 (0.63; 0.97) | 1.02 (0.77; 1.26) | 0.001 |
| Fat Mass (kg) | −1.24 (−2.39; −0.822) | 1.55 (0.42; 2.69) | 2.79 (1.15; 4.43) | 0.001 |
| VAT (g) | −4.53 (−51.01; 41.94) | −75.45 (−121.12; −29.78) | −70.91 (−137.13; −4.70) | 0.036 |
| CRP (mg/dL) | 0.24 (−0.16; 0.63) | −0.50 (−0.89; −0.12) | −0.74 (−1.30; −0.18) | 0.011 |
| Zonulin (ng/mL) | 0.02 (−0.03; −0.07) | −0.28 (−0.33; −0.23) | −0.30 (−0.37; −0.23) | 0.001 |
| TNF-alfa (pg/mL) | 0.85 (−0.74; 2.44) | −5.60 (−7.16; −4.04) | −6.45 (−8.71; −4.18) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rondanelli, M.; Gasparri, C.; Cavioni, A.; Sivieri, C.; Barrile, G.C.; Mansueto, F.; Perna, S. A Patented Dietary Supplement (Hydroxy-Methyl-Butyrate, Carnosine, Magnesium, Butyrate, Lactoferrin) Is a Promising Therapeutic Target for Age-Related Sarcopenia through the Regulation of Gut Permeability: A Randomized Controlled Trial. Nutrients 2024, 16, 1369. https://doi.org/10.3390/nu16091369
Rondanelli M, Gasparri C, Cavioni A, Sivieri C, Barrile GC, Mansueto F, Perna S. A Patented Dietary Supplement (Hydroxy-Methyl-Butyrate, Carnosine, Magnesium, Butyrate, Lactoferrin) Is a Promising Therapeutic Target for Age-Related Sarcopenia through the Regulation of Gut Permeability: A Randomized Controlled Trial. Nutrients. 2024; 16(9):1369. https://doi.org/10.3390/nu16091369
Chicago/Turabian StyleRondanelli, Mariangela, Clara Gasparri, Alessandro Cavioni, Claudia Sivieri, Gaetan Claude Barrile, Francesca Mansueto, and Simone Perna. 2024. "A Patented Dietary Supplement (Hydroxy-Methyl-Butyrate, Carnosine, Magnesium, Butyrate, Lactoferrin) Is a Promising Therapeutic Target for Age-Related Sarcopenia through the Regulation of Gut Permeability: A Randomized Controlled Trial" Nutrients 16, no. 9: 1369. https://doi.org/10.3390/nu16091369
APA StyleRondanelli, M., Gasparri, C., Cavioni, A., Sivieri, C., Barrile, G. C., Mansueto, F., & Perna, S. (2024). A Patented Dietary Supplement (Hydroxy-Methyl-Butyrate, Carnosine, Magnesium, Butyrate, Lactoferrin) Is a Promising Therapeutic Target for Age-Related Sarcopenia through the Regulation of Gut Permeability: A Randomized Controlled Trial. Nutrients, 16(9), 1369. https://doi.org/10.3390/nu16091369






