Social Media for Nutrition Education—A Randomized Controlled Trial to Promote Fruit and Vegetable Intake in a University Setting: “The University of Valladolid Community Eats Healthy” Study
Abstract
1. Introduction
Objective
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Intervention
- -
- Virtual campus: weekly webinars that were recorded for consultation. Also, documents such as menu planning sheets, and shopping list models were provided.
- -
- Instagram: videos, posts, stories, and Instagram Lives as workshops (recorded).
- -
- Facebook: videos, posts, stories, and Facebook Lives as workshops (recorded).
2.4. Control Group
2.5. Measures
2.5.1. Primary Outcomes: FV Intake
2.5.2. Secondary Outcomes
2.6. Data Analysis
3. Results
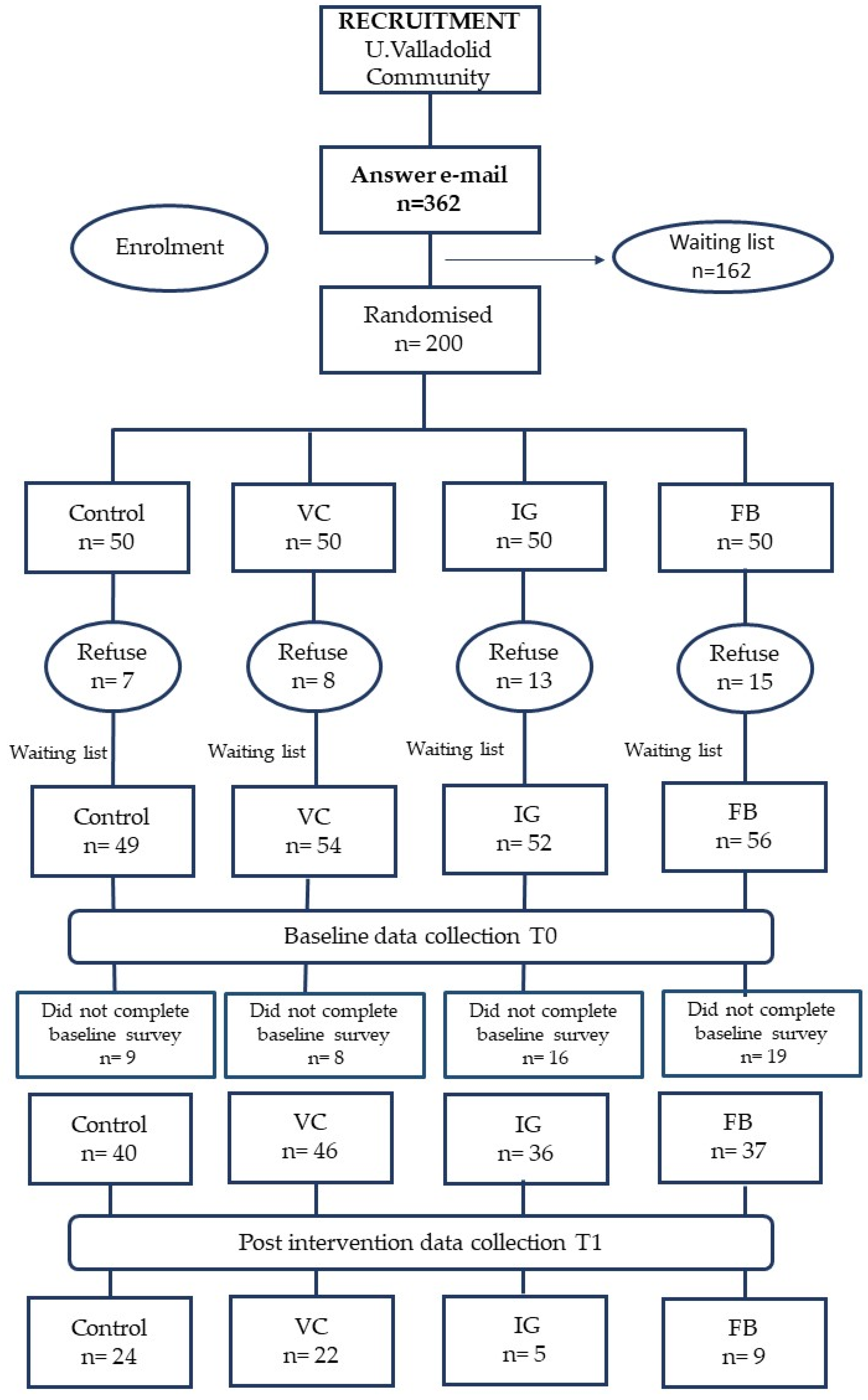
3.1. Recruitment
3.2. Participants at Baseline
3.3. Intervention Effectiveness
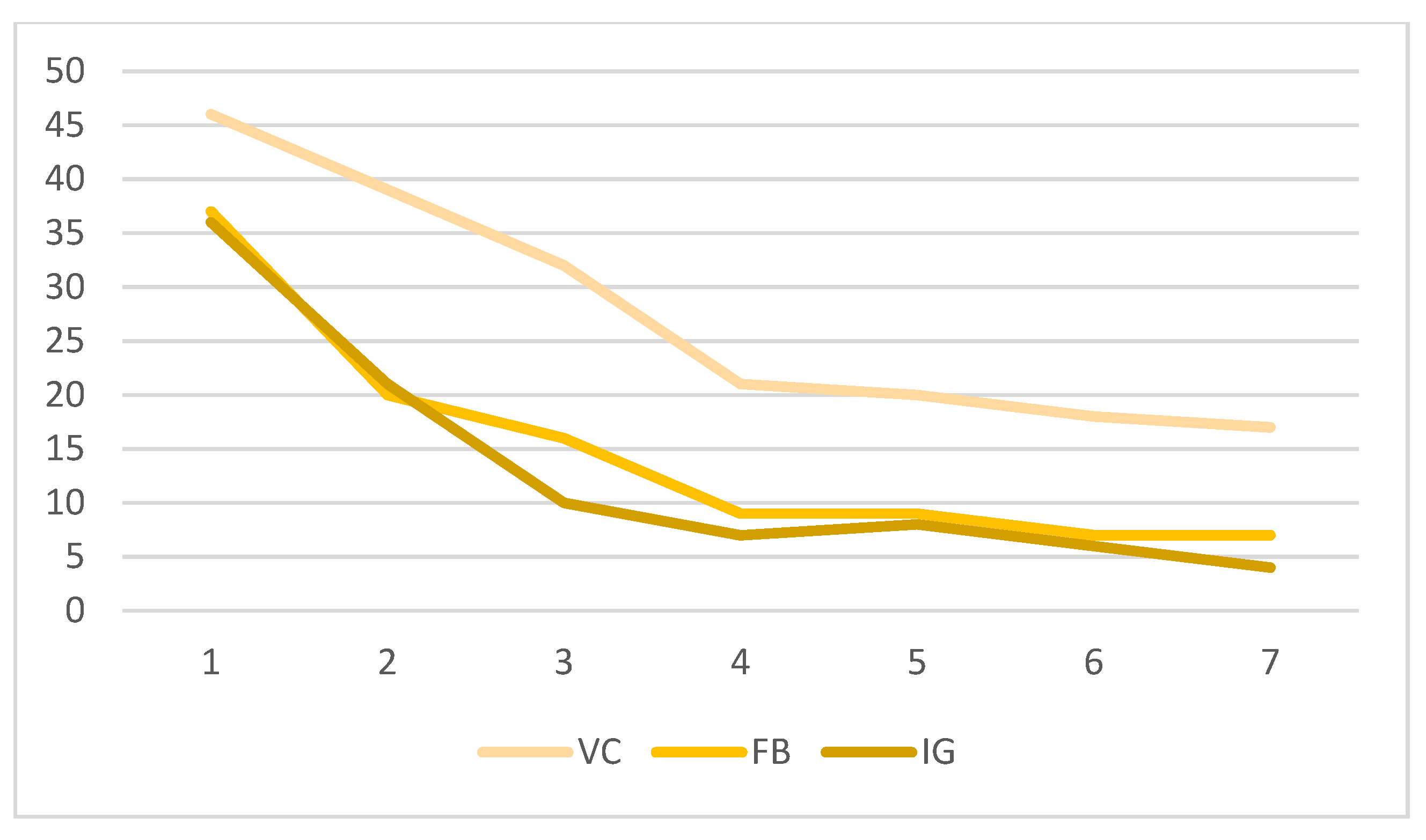
3.4. Participation and Retention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vlismas, K.; Stavrinos, V.; Panagiotakos, D.B. Socio-Economic Status, Dietary Habits and Health-Related Outcomes in Various Parts of the World: A Review. Cent. Eur. J. Public Health 2009, 17, 55–63. [Google Scholar] [CrossRef]
- Ministerio de Agricultura, Pesca y Alimentación. Panel de Consumo Alimentario. Available online: https://www.mapa.gob.es/es/alimentacion/temas/consumo-tendencias/panel-de-consumo-alimentario/ (accessed on 22 January 2024).
- Agencia Española de Seguridad Alimentaria (AESAN). Recomendaciones Dietéticas Saludables y Sostenibles Complementadas con Recomendaciones de Actividad Física Para la Población Española. Come Sano, Muévete y Cuida tu Planeta. AESAN. 2022. Available online: https://www.aesan.gob.es/AECOSAN/docs/documentos/nutricion/RECOMENDACIONES_DIETETICAS.pdf (accessed on 22 January 2024).
- Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C.; Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients 2019, 11, 2675. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Tomaino, L.; Dernini, S.; Berry, E.M.; Lairon, D.; de la Cruz, J.N.; Bach-Faig, A.; Donini, L.M.; Medina, F.X.; Belahsen, R.; et al. Updating the mediterranean diet pyramid towards sustainability: Focus on environmental concerns. Int. J. Environ. Res. Public. Health 2020, 17, 8758. [Google Scholar] [CrossRef]
- WHO. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation; World Health Organ Technical Report Series; WHO: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 15 January 2024).
- Mu, M.; Xu, L.F.; Hu, D.; Wu, J.; Bai, M.J. Dietary Patterns and Overweight/Obesity: A Review Article. Iran. J. Public. Health 2017, 46, 869. [Google Scholar]
- Dinu, M.; Pagliai, G.; Angelino, D.; Rosi, A.; Dall’Asta, M.; Bresciani, L.; Ferraris, C.; Guglielmetti, M.; Godos, J.; Del Bo, C.; et al. Effects of popular diets on anthropometric and cardiometabolic parameters: An umbrella review of meta-analyses of randomized controlled trials. Adv. Nutr. 2020, 11, 815–833. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Portal Estadístico del SNS. Informe Anual del Sistema Nacional de Salud. 2020. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnSNS.htm (accessed on 24 January 2024).
- World Obesity Federation. Calculating the Costs of the Consequences of Obesity. Available online: https://www.worldobesity.org/resources/resource-library/calculating-the-costs-of-the-consequences-of-obesity (accessed on 27 January 2024).
- Catucci, A.; Scognamiglio, U.; Rossi, L. Lifestyle changes related to eating habits, physical activity, and weight status during COVID-19 quarantine in Italy and some European countries. Front. Nutr. 2021, 8, 718877. [Google Scholar] [CrossRef]
- Zeigler, Z. COVID-19 Self-quarantine and Weight Gain Risk Factors in Adults. Curr. Obes. Rep. 2021, 10, 423–433. [Google Scholar] [CrossRef]
- Celorio-Sardà, R.; Comas-Basté, O.; Latorre-Moratalla, M.L.; Zerón-Rugerio, M.F.; Urpi-Sarda, M.; Illán-Villanueva, M.; Farran-Codina, A.; Izquierdo-Pulido, M.; Vidal-Carou, M.D.C. Effect of COVID-19 lockdown on dietary habits and lifestyle of food science students and professionals from Spain. Nutrients 2021, 13, 1494. [Google Scholar] [CrossRef]
- Sánchez, E.; Lecube, A.; Bellido, D.; Monereo, S.; Malagón, M.M.; Tinahones, F.J. Leading factors for weight gain during covid-19 lockdown in a Spanish population: A cross-sectional study. Nutrients 2021, 13, 894. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, M.L.; García-Vigara, A.; Hidalgo-Mora, J.J.; García-Pérez, M.Á.; Tarín, J.; Cano, A. Mediterranean diet and health: A systematic review of epidemiological studies and intervention trials. Maturitas 2020, 136, 25–37. [Google Scholar] [CrossRef]
- Schwingshackl, L.; Morze, J.; Hoffmann, G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br. J. Pharmacol. 2020, 177, 1241–1257. [Google Scholar] [CrossRef]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campà, A.; Martínez-González, M.A.; Ruiz-Canela, M. Mediterranean Diet and health outcomes in the SUN cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef]
- English, L.K.; Ard, J.D.; Bailey, R.L.; Bates, M.; Bazzano, L.A.; Boushey, C.J.; Brown, C.; Butera, G.; Callahan, E.H.; de Jesus, J.; et al. Evaluation of dietary patterns and all-cause mortality. JAMA Netw. Open 2021, 4, e2122277. [Google Scholar] [CrossRef]
- Ndanuko, R.N.; Tapsell, L.C.; E Charlton, K.; Neale, E.P.; Batterham, M.J. Dietary patterns and blood pressure in adults: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 2016, 7, 76. [Google Scholar] [CrossRef]
- Salas-Salvadó, J.; Becerra-Tomás, N.; García-Gavilán, J.F.; Bulló, M.; Barrubés, L. Mediterranean diet and cardiovascular disease prevention: What do we know? Prog. Cardiovasc. Dis. 2018, 61, 62–67. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean diet and cardiovascular health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Rosato, V.; Temple, N.J.; La Vecchia, C.; Castellan, G.; Tavani, A.; Guercio, V. Mediterranean diet and cardiovascular disease: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2019, 58, 173–191. [Google Scholar] [CrossRef]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean diet: A review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Steck, S.E.; Murphy, E.A. Dietary patterns and cancer risk. Nat. Rev. Cancer 2019, 20, 125–138. [Google Scholar] [CrossRef]
- Dernini, S.; Berry, E.M.; Serra-Majem, L.; La Vecchia, C.; Capone, R.; Medina, F.X.; Aranceta-Bartrina, J.; Belahsen, R.; Burlingame, B.; Calabrese, G.; et al. Med Diet 4.0: The Mediterranean diet with four sustainable benefits. Public. Health Nutr. 2017, 20, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Dernini, S.; Berry, E.; Bach-Faig, A. A Dietary Model Constructed by Scientists: The Mediterranean Diet. In Mediterra; The Mediterranean Diet for Sustainable Regional Development; Presses de Sciences Po: Paris, France, 2012; pp. 71–88. [Google Scholar]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- WHO. Diet, Nutrition and the Prevention of Chronic Diseases; Report of a Joint WHO/FAO Expert Consultation World Health Organ Technical Report Series; WHO: Geneva, Switzerland, 2003; p. 916. Available online: https://apps.who.int/iris/handle/10665/42665 (accessed on 15 January 2024).
- Zurbau, A.; Au-Yeung, F.; Mejia, S.B.; Khan, T.A.; Vuksan, V.; Jovanovski, E.; Leiter, L.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Sievenpiper, J.L. Relation of different fruit and vegetable sources with incident cardiovascular outcomes: A systematic review and meta-analysis of prospective cohort studies. J. Am. Heart. 2020, 9, e017728. [Google Scholar] [CrossRef] [PubMed]
- Bechthold, A.; Boeing, H.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; De Henauw, S.; Michels, N.; Devleesschauwer, B.; Schlesinger, S.; et al. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 1071–1090. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Keum, N.; Giovannucci, E.; Fadnes, L.T.; Boffetta, P.; Greenwood, D.C.; Tonstad, S.; Vatten, L.J.; Riboli, E.; Norat, T. Dietary intake and blood concentrations of antioxidants and the risk of cardiovascular disease, total cancer, and all-cause mortality: A systematic review and dose-response meta-analysis of prospective studies. Am. J. Clin. Nutr. 2018, 108, 1069–1091. [Google Scholar] [CrossRef] [PubMed]
- Aune, D. Plant foods, antioxidant biomarkers, and the risk of cardiovascular disease, cancer, and mortality: A review of the evidence. Adv. Nutr. 2019, 10 (Suppl. S4), S404–S421. [Google Scholar] [CrossRef]
- Mariscal-Arcas, M.; Delgado-Mingorance, S.; de Buruaga, B.S.; Blas-Diaz, A.; Latorre, J.A.; Martinez-Bebia, M.; Gimenez-Blasi, N.; Conde-Pipo, J.; Cantero, L.; Lopez-Moro, A.; et al. Evolution of nutritional habits behaviour of Spanish population confined through social media. Front. Nutr. 2021, 8, 794592. [Google Scholar] [CrossRef] [PubMed]
- Gudiño, D.; Fernández-Sánchez, M.J.; Becerra-Traver, M.T.; Sánchez, S. Social media and the pandemic: Consumption habits of the Spanish population before and during the COVID-19 lockdown. Sustainability 2022, 14, 5490. [Google Scholar] [CrossRef]
- Diddi, P.; Lundy, L.K. Organizational Twitter use: Content analysis of tweets during breast cancer awareness month. J. Health Commun. 2017, 22, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Giustini, D.M.; Ali, S.M.; Fraser, M.; Boulos, M.N.K. Effective uses of social media in public health and medicine: A systematic review of systematic reviews. Online J. Public. Health Inform. 2018, 10, e215. [Google Scholar] [CrossRef] [PubMed]
- Ufholz, K. Peer support groups for weight loss. Curr. Cardiovasc. Risk Rep. 2020, 14, 19. [Google Scholar] [CrossRef]
- Taiminen, H.; Taiminen, K. Usage of Facebook-and anonymous forum—Based peer support groups online and their influence on perceived social support types in weight loss. In Proceedings of the Annual Hawaii International Conference on System Sciences, Koloa, HI, USA, 5–8 January 2016; pp. 3094–3103. [Google Scholar]
- Chen, J.; Wang, Y. Social media use for health purposes: Systematic review. J. Med. Internet Res. 2021, 23, e17917. [Google Scholar] [CrossRef]
- Petkovic, J.; Duench, S.; Trawin, J.; Dewidar, O.; Pardo, J.P.; Simeon, R.; DesMeules, M.; Gagnon, D.; Roberts, J.H.; Hossain, A.; et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst. Rev. 2021, 5, CD012932. [Google Scholar]
- Goodyear, V.A.; Wood, G.; Skinner, B.; Thompson, J.L. The effect of social media interventions on physical activity and dietary behaviours in young people and adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 72. [Google Scholar] [CrossRef]
- Moroni, A.; Degan, R.; Martin, B.; Sciannameo, V.; Berchialla, P.; Gilli, G.; Cremasco, M.M. Effectiveness of Workplace Health Promotion (WHP) interventions in university employees: A scoping review. Health Promot. Int. 2023, 38, daac171. [Google Scholar] [CrossRef]
- Sogari, G.; Velez-Argumedo, C.; Gómez, M.I.; Mora, C. College students and eating habits: A study using an ecological model for healthy behavior. Nutrients 2018, 10, 1823. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.L.; Han, B.; Cohen, D.A. Associations between eating occasions and places of consumption among adults. Appetite 2015, 87, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Almoraie, N.M.; Saqaan, R.; Alharthi, R.; Alamoudi, A.; Badh, L.; Shatwan, I.M. Snacking patterns throughout the life span: Potential implications on health. Nutr. Res. 2021, 91, 81–94. [Google Scholar] [CrossRef]
- Rodrigues, V.M.; Bray, J.; Fernandes, A.C.; Bernardo, G.L.; Hartwell, H.; Martinelli, S.S.; Uggioni, P.L.; Cavalli, S.B.; Proença, R.P.d.C. Vegetable consumption and factors associated with increased intake among college students: A scoping review of the last 10 years. Nutrients 2019, 11, 1634. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Micha, R.; Karageorgou, D.; Bakogianni, I.; Trichia, E.; Whitsel, L.P.; Story, M.; Peñalvo, J.L.; Mozaffarian, D. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0194555. [Google Scholar] [CrossRef]
- Langford, R.; Bonell, C.P.; Jones, H.E.; Pouliou, T.; Murphy, S.M.; Waters, E.; Komro, K.A.; Gibbs, L.F.; Magnus, D.; Campbell, R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014, 4, CD008958. [Google Scholar] [CrossRef] [PubMed]
- Hodder, R.K.; O’Brien, K.M.; Stacey, F.G.; Wyse, R.J.; Clinton-McHarg, T.; Tzelepis, F.; Wyse, R.J.; Wolfenden, L. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst. Rev. 2018, 5, CD008552. [Google Scholar] [PubMed]
- Rodriguez Rocha, N.P.; Kim, H. eHealth Interventions for Fruit and Vegetable Intake: A Meta-Analysis of Effectiveness. Health Educ. Behav. 2019, 6, 947–959. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Barnes, C.; Lane, C.; McCrabb, S.; Brown, H.M.; Gerritsen, S.; Barquera, S.; Véjar, L.S.; Munguía, A.; Yoong, S.L. Consolidating evidence on the effectiveness of interventions promoting fruit and vegetable consumption: An umbrella review. Int. J. Behav. Nutr. Phys. 2021, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Jabbari, M.; Namazi, N.; Irandoost, P.; Rezazadeh, L.; Ramezani-Jolfaie, N.; Babashahi, M.; Pourmoradian, S.; Barati, M. Meta-analysis of community-based interventions on fruits and vegetables consumption in adults. Nutr. Food Sci. 2023, 54, 164–191. [Google Scholar] [CrossRef]
- Al-Awadhi, B.; Fallaize, R.; Zenun Franco, R.; Hwang, F.; Lovegrove, J.A. Insights into the Delivery of Personalized Nutrition: Evidence from Face-To-Face and Web-Based Dietary Interventions. Front. Nutr. 2021, 7, 570531. [Google Scholar] [CrossRef]
- Livingstone, K.M.; Rawstorn, J.C.; Partridge, S.R.; Godrich, S.L.; McNaughton, S.A.; Hendrie, G.A.; Blekkenhorst, L.C.; Maddison, R.; Zhang, Y.; Barnett, S.; et al. Digital behaviour change interventions to increase vegetable intake in adults: A systematic review. Int. J. Behav. Nutr. Phys. 2023, 20, 36. [Google Scholar] [CrossRef]
- Chirumamilla, S.; Gulati, M. Patient Education and Engagement through Social Media. Curr. Cardiol. Rev. 2019, 17, 137–143. [Google Scholar]
- Rose, T.; Barker, M.; Jacob, C.; Lawrence, W.; Strommer, S.; Vogel, C.; Woods-Townsend, K.; Inskip, H.; Baird, J. A systematic review of digital interventions for improving the diet and physical activity behaviours of adolescents. J. Adolesc. Health 2017, 61, 669. [Google Scholar] [CrossRef]
| Intervention | Control | |
|---|---|---|
| Week 1 | Presentation of the program. Healthy eating | Healthy eating |
| Week 2 | FV: nutritional value, types, seasonality, benefits for health | MD—principal foods |
| Week 3 | Shopping FV: tips, places, conservation methods | MD—a lifestyle |
| Week 4 | Healthy menu planning with “My Plate” | MD—pyramid |
| Week 5 | How to cook FV avoiding food waste | Health benefits of the MD |
| Week 6 | Healthy snacks using FV | How to practice the MD on a daily basis |
| Week 7 | Batch cooking | Myths of the MD |
| Total Sample (n = 159) | VC (n = 46) | FB (n = 37) | IG (n = 36) | Control (n = 40) | |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 75.2% | 84.8% | 62.2% | 80.6% | 72.5% |
| Male | 24.8% | 15.2% | 37.8% | 19.4% | 27.5% |
| Age (years) mean (SD) | 37.1 (15.2) | 40.1 (13.6) | 36.1 (15.3) | 34.5 (16.4) | 36.2 (16.2) |
| Nutritional status | |||||
| BMI (kg/m2) mean (SD) | 24.2 (4.1) | 23.6 (3.7) | 24.1 (3.7) | 24.9 (4.0) | 24.4 (4.9) |
| Underweight | 0.6% | 6.7% | 2.7% | 0 | 2.5% |
| Healthy weight | 63.3% | 64.4% | 70.3% | 55.6% | 62.5% |
| Overweight | 21.5% | 20% | 16.2% | 30.6% | 20% |
| Obese | 12% | 8.9% | 10.8% | 13.9% | 15% |
| Work activity | |||||
| Student | 51.6% | 37% | 62.2% | 58.3% | 52.5% |
| Administration staff | 24.5% | 41.3% * | 27% | 13.9% | 12.5% |
| Professors and researchers | 23.9% | 21.7% | 10.8% | 27.8% | 35% † |
| Living situation | |||||
| With family | 64.2% | 67.4% | 70.3% | 55.6% | 62.5% |
| With friends | 25.2% | 21.7% | 21.6% | 30.6% | 27.5% |
| Residential college | 0.6% | 0 | 0 | 0 | 2.5% |
| Own home | 10% | 10.9% | 8.1% | 13.9% | 7.5% |
| Area of knowledge | |||||
| Health Science | 13.8% | 10.9% | 18.9% | 11.1% | 15% |
| Other | 86.2% | 89.1% | 81.1% | 88.9% | 85% |
| Toxic habits | |||||
| Smoking | 5.7% | 2.2% | 8.1% | 5.6% | 7.5% |
| Alcohol drinking | 72.3% | 69.6% | 73% | 72.2% | 75% |
| Health conditions | |||||
| HBP | 5.7% | 6.5% | 5.4% | 5.6% | 5% |
| Dyslipidemia | 8.8% | 13% | 8.1% | 5.6% | 7.5% |
| Arthritis | 6.9% | 8.7% | 16.2% | 0 | 2.5% |
| No conditions | 67.3% | 65.2% | 64.9% | 75% | 65% |
| Medas-14 Questionnaire | |||||
| Predimed Score mean (SD) | 6.73 (1.9) | 6.61 (1.8) | 6.49 (2.0) | 6.78 (2.2) | 7.1 (1.8) |
| Low adherence | 29.6% | 32.6% | 35.1% | 30.6% | 20% |
| Medium adherence | 62.3% | 65.2% | 54.1% | 54.1% | 70% |
| High adherence | 8.2% | 2.2% | 10.8% | 11.1% | 10% |
| Total Sample | VC | FB | IG | Control | |
|---|---|---|---|---|---|
| Medas-14 Questionnaire | |||||
| Pre-intervention mean (SD) | 6.73 (1.9) | 6.61 (1.8) | 6.49 (2.0) | 6.78 (2.2) | 7.10 (1.8) |
| Post-intervention mean (SD) | 7.62 (1.9) | 7.75 (1.9) | 7,11 (1.3) | 7.40 (3.0) | 7.75 (1.9) |
| Item 3 Vegetable intake (>2 servings/day; 200 g) | |||||
| V intake pre-intervention | 24.5% | 17.4% | 21.6% | 27.8% | 32.5% |
| V intake post-intervention | 38.3% | 72.7% * | 33.3% | 40% | 40% |
| Item 4 Fruit intake (3 or more servings/day; 100–150 g) | |||||
| F intake pre-intervention | 23.3% | 23.9% | 24.3% | 19.4% | 25% |
| F intake post-intervention | 31.7% | 45.5% | 22.2% | 20% | 25% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carreño Enciso, L.; de Mateo Silleras, B.; de la Cruz Marcos, S.; Redondo del Río, P. Social Media for Nutrition Education—A Randomized Controlled Trial to Promote Fruit and Vegetable Intake in a University Setting: “The University of Valladolid Community Eats Healthy” Study. Nutrients 2024, 16, 1308. https://doi.org/10.3390/nu16091308
Carreño Enciso L, de Mateo Silleras B, de la Cruz Marcos S, Redondo del Río P. Social Media for Nutrition Education—A Randomized Controlled Trial to Promote Fruit and Vegetable Intake in a University Setting: “The University of Valladolid Community Eats Healthy” Study. Nutrients. 2024; 16(9):1308. https://doi.org/10.3390/nu16091308
Chicago/Turabian StyleCarreño Enciso, Laura, Beatriz de Mateo Silleras, Sandra de la Cruz Marcos, and Paz Redondo del Río. 2024. "Social Media for Nutrition Education—A Randomized Controlled Trial to Promote Fruit and Vegetable Intake in a University Setting: “The University of Valladolid Community Eats Healthy” Study" Nutrients 16, no. 9: 1308. https://doi.org/10.3390/nu16091308
APA StyleCarreño Enciso, L., de Mateo Silleras, B., de la Cruz Marcos, S., & Redondo del Río, P. (2024). Social Media for Nutrition Education—A Randomized Controlled Trial to Promote Fruit and Vegetable Intake in a University Setting: “The University of Valladolid Community Eats Healthy” Study. Nutrients, 16(9), 1308. https://doi.org/10.3390/nu16091308







