Beyond the Tropics: Unraveling the Complex Relationship between Sun Exposure, Dietary Intake, and Vitamin D Deficiency in Coastal Malaysians
Abstract
1. Introduction
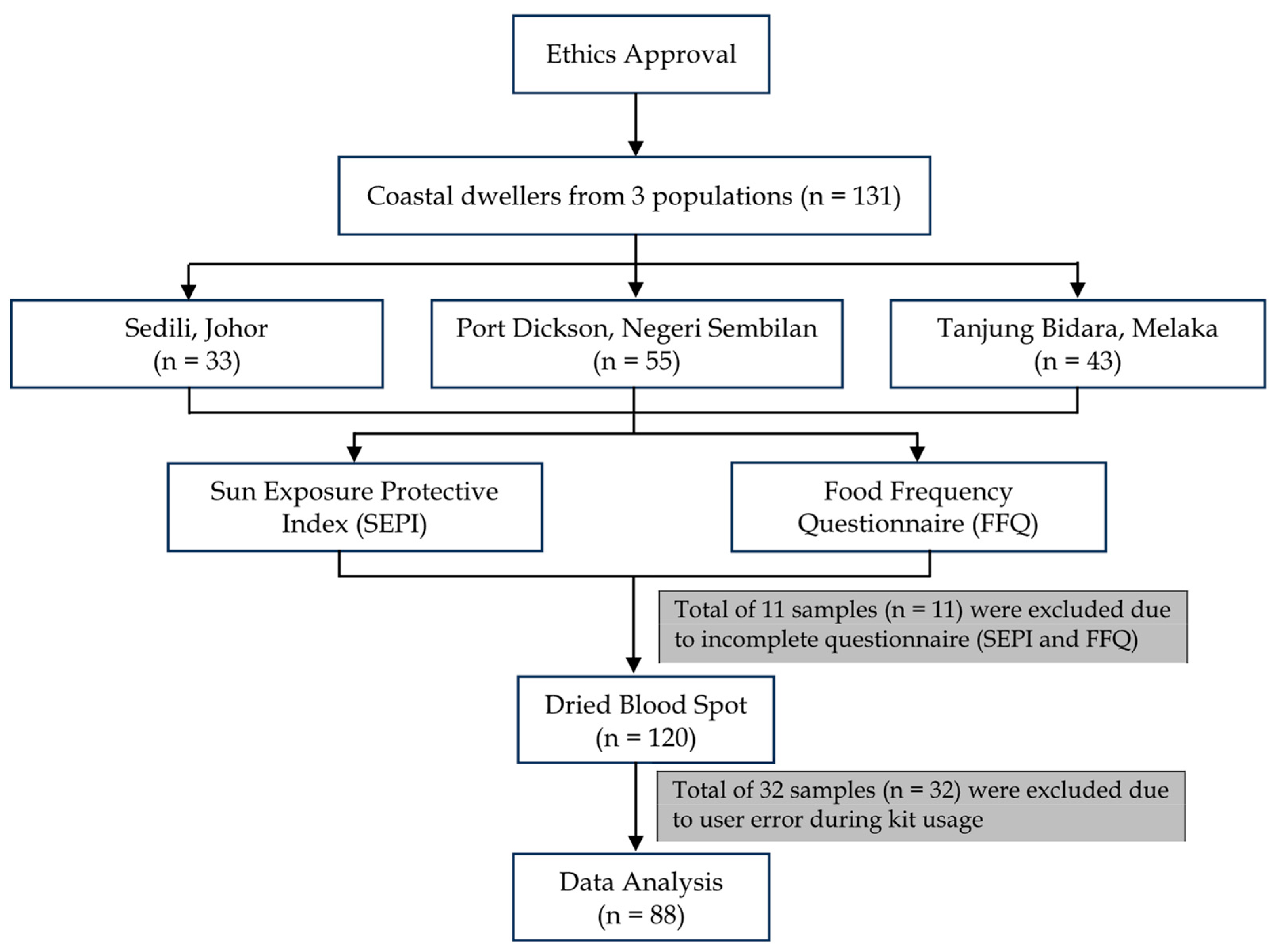
2. Methodology
2.1. Research Design
2.1.1. Subject Recruitment
2.1.2. Biochemical Analysis of DBS
2.1.3. Questionnaire
2.2. Data Collection
2.2.1. DBS and Data Processing
2.2.2. The 25-OH Vitamin D3 Status Using DBS
2.3. Statistical Analysis
3. Results and Discussion
3.1. Sociodemographic Profile
3.2. SEPI Score
3.2.1. Sun Habits and Sun Protection Behaviour (SEPI Part 1)
3.2.2. Readiness to Increase Sun Protection (SEPI Part 2)
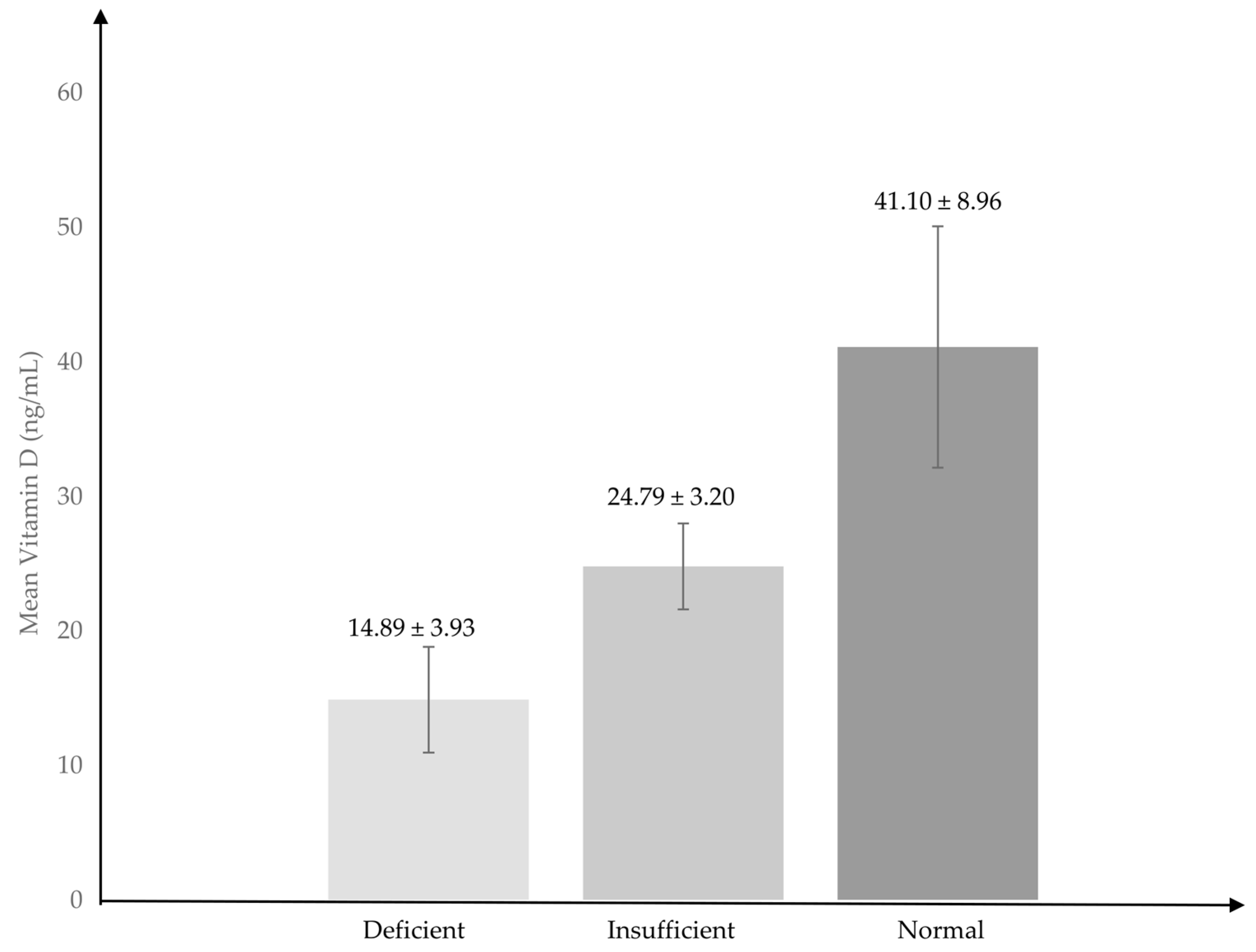
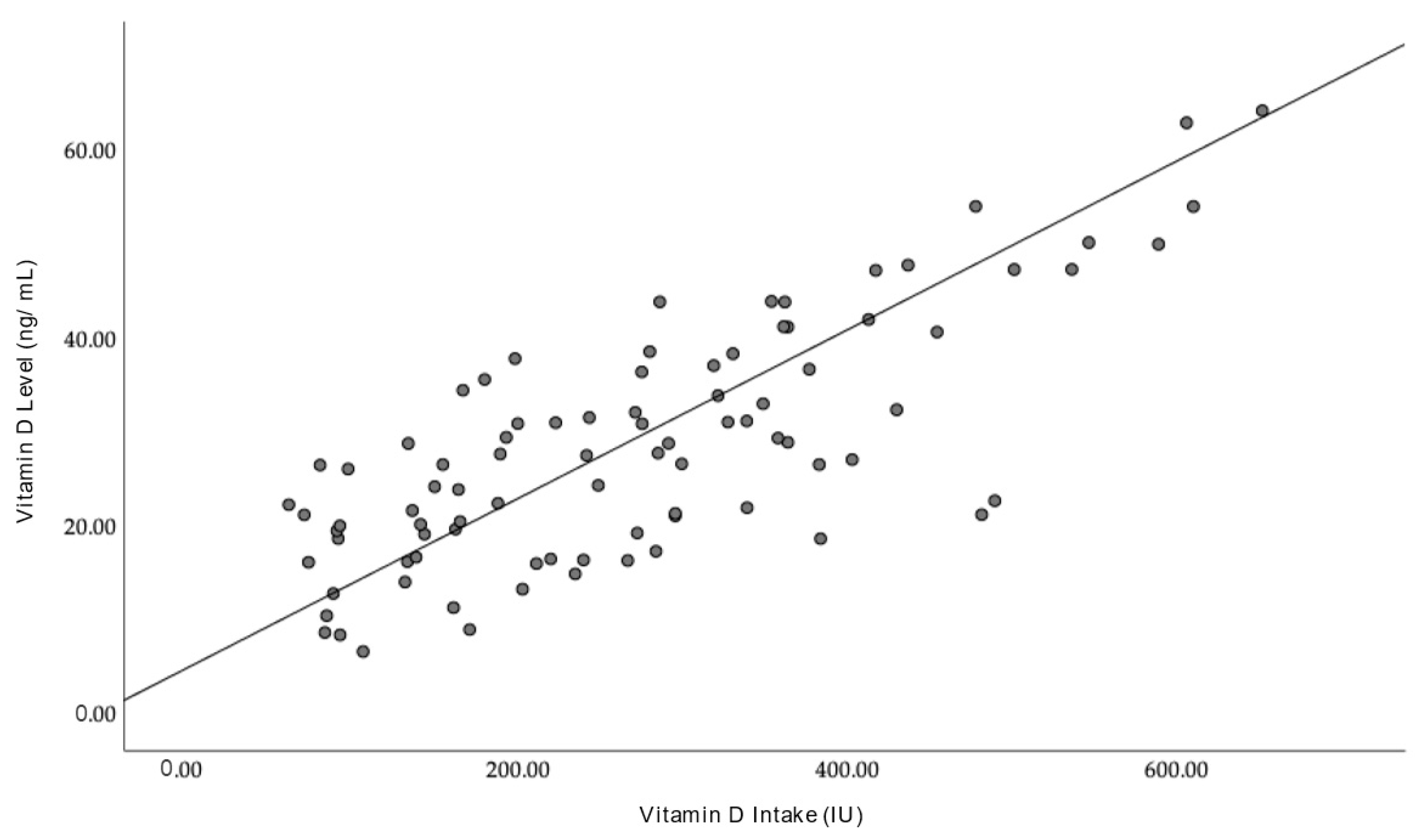
3.3. Vitamin D Levels
3.4. Discussion
SEPI Questionnaire
4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sizar, O.; Khare, S.; Goyal, A.; Givler, A. Vitamin D Deficiency; National Library of Medicine: Bethesda, MD, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532266/ (accessed on 18 July 2023).
- Isa, Z.M.; Mohd Nordin, N.R.; Mahmud, M.H.; Hashim, S. An Update on Vitamin D Deficiency Status in Malaysia. Nutrients 2022, 14, 567. [Google Scholar] [CrossRef] [PubMed]
- Saffian, S.M.; Jamil, N.A.; Tahir, N.A.M.; Hatah, E. Vitamin D Insufficiency is High in Malaysia: A Systematic Review and Meta-Analysis of Studies on Vitamin D Status in Malaysia; Research Square: Durham, NC, USA, 2021; Available online: https://assets.researchsquare.com/files/rs-833384/v1/8a127337-f3a7-4645-bdf6-fb6c89abd669.pdf?c=1631888409 (accessed on 1 August 2023).
- Wacker, M.; Holick, M.F. Sunlight and vitamin D: A global perspective for health. Dermato-Endocrinology 2013, 5, 51–108. [Google Scholar] [CrossRef]
- Krassilnikovva, M.; Ostrow, K.; Bader, A.; Heeger, P.; Mehrotra, A. Low Dietary Intake of Vitamin D and Vitamin D Deficiency in Hemodialysis Patients. J. Nephrol. Ther. 2014, 4, 166. [Google Scholar] [CrossRef] [PubMed]
- Vici, G.; Camilletti, D.; Polzonetti, V. Possible role of vitamin D in celiac disease onset. Nutrients 2020, 12, 1051. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N. Vitamin D and inflammatory bowel disease. Gastroenterol. Hepatol. 2016, 12, 513–515. [Google Scholar]
- Thomson, G.J.H.; Mountford, C.; Thompson, N. OC-027Use of Buccal Vitamin D Supplementation in Patients with Short Bowel Syndrome. Gut 2016, 65 (Suppl. S1), A16–A17. [Google Scholar] [CrossRef]
- Wan, J.; Yuan, J.; Li, X.; Bao, Y.; Hou, Y.; Li, Z.; Tan, S.C.; Low, T.Y.; Chu, Y. Association between serum vitamin D levels and venous thromboembolism (VTE): A systematic review and meta-analysis of observational studies. Complement. Ther. Med. 2020, 54, 102579. [Google Scholar] [CrossRef]
- Manappallil, R.G.; Krishnan, R.; Veetil, P.P.; Nambiar, H.; Karadan, U.; Anil, R.; Josephine, B. Hypocalcemic Seizure Due to Vitamin D Deficiency. Indian J. Crit. Care Med. 2020, 24, 882–884. [Google Scholar] [CrossRef]
- Lips, P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: Consequences for bone loss and fractures and therapeutic implications. Endocr. Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef]
- Cashman, K.D. Vitamin D in childhood and adolescence. Postgrad. Med. J. 2007, 83, 230–235. [Google Scholar] [CrossRef]
- Poh, B.K.; Ng, B.K.; Siti Haslinda, M.D.; Nik Shanita, S.; Wong, J.E.; Budin, S.B.; Ruzita, A.T.; Ng, L.O.; Khouw, I.; Norimah, A.K. Nutritional status and dietary intakes of children aged 6 months to 12 years: Findings of the nutrition survey of malaysian children (SEANUTS Malaysia). Br. J. Nutr. 2013, 110 (Suppl. S3), S21–S35. [Google Scholar] [CrossRef] [PubMed]
- Al-Sadat, N.; Majid, H.A.; Sim, P.Y.; Su, T.T.; Dahlui, M.; Bakar, M.F.A.; Dzaki, N.; Norbaya, S.; Murray, L.; Cantwell, M.M.; et al. Vitamin D deficiency in Malaysian adolescents aged 13 years: Findings from the Malaysian Health and Adolescents Longitudinal Research Team study (MyHeARTs). BMJ J. 2016, 6, e010689. [Google Scholar] [CrossRef] [PubMed]
- Bruce, S.J.; Rochat, B.; Béguin, A.; Pesse, B.; Guessous, I.; Boulat, O.; Henry, H. Analysis and quantification of vitamin D metabolites in serum by ultra-performance liquid chromatography coupled to tandem mass spectrometry and high-resolution mass spectrometry–a method comparison and validation. Rapid Commun. Mass Spectrom. 2013, 27, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Corran, P.H.; Cook, J.; Lynch, C.; Leendertse, H.; Manjurano, A.; Griffin, J.; Cox, J.; Abeku, T.; Bousema, T.; Ghani, A.C.; et al. Dried blood spots as a source of anti-malarial antibodies for epidemiological studies. Malar. J. 2008, 7, 195. [Google Scholar] [CrossRef] [PubMed]
- Barquín, D.; Ndarabu, A.; Carlos, S.; Fernández-Alonso, M.; Rubio-Garrido, M.; Makonda, B.; Holguín, Á.; Reina, G. HIV-1 diagnosis using dried blood spots from patients in Kinshasa, DRC: A tool to detect misdiagnosis and achieve World Health Organization 2030 Targets. Int. J. Infect. Dis. 2021, 111, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Mulla, H.; Kairamkonda, V.; Spooner, N.; Gade, S.; Della Pasqua, O.; Field, D.J.; Pandya, H.C. Dried blood spots and sparse sampling: A practical approach to estimating pharmacokinetic parameters of caffeine in preterm infants. Br. J. Clin. Pharmacol. 2013, 75, 805–813. [Google Scholar] [CrossRef]
- Moat, S.J.; George, R.S.; Carling, R.S. Use of dried blood spot specimens to monitor patients with inherited metabolic disorders. Int. J. Neonatal Screen. 2020, 6, 26. [Google Scholar] [CrossRef]
- Li, W.; Lee, M.S. Overview of the History and Applications of Dried Blood Samples. In Dried Blood Spots: Applications and Techniques; John Wiley & Sons: Hoboken, NJ, USA, 2014; pp. 5–6. [Google Scholar]
- Medizinische Labordiagnostika AG. 25-OH Vitamin D ELISA; EUROIMMUN: Lübeck, Germany, 2012; Available online: https://www.euroimmun.com/detail/news/euroimmun-25-oh-vitamin-d-elisa/ (accessed on 5 September 2022).
- Quah, S.W.; Abdul Majid, H.; Al-Sadat, N.; Yahya, A.; Su, T.T.; Jalaludin, M.Y. Risk factors of vitamin D deficiency among 15-year-old adolescents participating in the Malaysian Health and Adolescents Longitudinal Research Team Study (MyHeARTs). PLoS ONE 2018, 13, e0200736. [Google Scholar] [CrossRef]
- Isa, Z.M.; Shamsudin, K.; Bukhary, N.; Khor, G.L.; Mahdy, Z.; Haslinda, H.; Hana, N.; Ghazi, H. Development and Validation of a Food Frequency Questionnaire for Vitamin D intake among Urban Pregnant Women in Malays. Malays. J. Nutr. 2015, 21, 179–190. [Google Scholar]
- Christoph, S.; Cazzaniga, S.; Hunger, R.; Naldi, L.; Borradori, L.; Oberholzer, P. Ultraviolet radiation protection and skin cancer awareness in recreational athletes: A survey among participants in a running event. Swiss Med. Wkly. 2016, 146, w14297. [Google Scholar] [CrossRef]
- Reis-Mansur, M.C.; da Luz, B.G.; dos Santos, E.P. Consumer behavior, skin phototype, sunscreens, and tools for photoprotection: A Review. Cosmetics 2023, 10, 39. [Google Scholar] [CrossRef]
- McLeod, G.F.; Dhakal, B.; Reeder, A.I.; McGee, R. Sunburn paradoxes and the New Zealand population. J. Public Health 2019, 29, 387–392. [Google Scholar] [CrossRef]
- McLeod, G.F.; Reeder, A.I.; Gray, A.R.; McGee, R. Unintended Sunburn: A potential target for Sun Protection messages. J. Skin Cancer 2017, 2017, 6902942. [Google Scholar] [CrossRef]
- Autier, P. Sunscreen abuse for intentional sun exposure. Br. J. Dermatol. 2009, 161, 40–45. [Google Scholar] [CrossRef]
- Alli, S.; LeBeau, J.; Hasbani, A.; Lagacé, F.; Litvinov, I.V.; Peláez, S. Understanding the perceived relationship between sun exposure and melanoma in Atlantic canada: A consensual qualitative study highlighting a “sunscreen paradox”. Cancers 2023, 15, 4726. [Google Scholar] [CrossRef] [PubMed]
- Falk, M. Differences in sun exposure habits between self-reported skin type and ultraviolet sensitivity measured by phototest. Photodermatol. Photoimmunol. Photomed. 2011, 27, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Falk, M.; Anderson, C.D. Measuring sun exposure habits and sun protection behaviour using a comprehensive scoring instrument—An illustration of a possible model based on Likert scale scorings and on estimation of readiness to increase Sun Protection. Cancer Epidemiol. 2012, 36, e265–e269. [Google Scholar] [CrossRef]
- AlGhamdi, K.M.; AlAklabi, A.S.; AlQahtani, A.Z. Knowledge, attitudes and practices of the general public toward Sun Exposure and protection: A national survey in Saudi Arabia. Saudi Pharm. J. 2016, 24, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Adams, G.J.; Goldstein, E.K.; Goldstein, B.G.; Jarman, K.L.; Goldstein, A.O. Attitudes and behaviors that impact skin cancer risk among men. Int. J. Environ. Res. Public Health 2021, 18, 9989. [Google Scholar] [CrossRef]
- Abroms, L.; Jorgensen, C.M.; Southwell, B.G.; Geller, A.C.; Emmons, K.M. Gender differences in young adults’ beliefs about sunscreen use. Health Educ. Behav. 2003, 30, 29–43. [Google Scholar] [CrossRef]
- Martin, A.; Liu, J.; Thatiparthi, A.; Ge, S.; Wu, J.J. An evaluation of shade-seeking and long-sleeved shirt use in Asian Americans. J. Am. Acad. Dermatol. 2022, 86, 927–929. [Google Scholar] [CrossRef]
- Biswas, A.; Harbin, S.; Irvin, E.; Johnston, H.; Begum, M.; Tiong, M.; Apedaile, D.; Koehoorn, M.; Smith, P. Sex and gender differences in occupational hazard exposures: A scoping review of the recent literature. Curr. Environ. Health Rep. 2021, 8, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.P.; Chien, A.L. Sun Protective Clothing and sun avoidance: The most critical components of photoprotection in patients with melanoma. Dermatol. Surg. 2020, 47, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Shih, J.; Tran, A.; Mullane, A.; Thomas, C.; Aydin, N.; Misra, S. Gender-based differences and barriers in skin protection behaviors in melanoma survivors. J. Skin Cancer 2016, 2016, 3874572. [Google Scholar] [CrossRef] [PubMed]
- Rajaretnam, A.; Abdalqader, M.; Ghazi, H.; Hasan, D.T.; Fuad, M. Knowledge regarding vitamin D among private university students in Malaysia. Ann. Nutr. Disord. Ther. 2014, 1, 1008. [Google Scholar]
- Jamil, N.A.; Shahudin, N.N.; Abdul Aziz, N.S.; Jia Qi, C.; Wan Aminuddin, W.A.; Mat Ludin, A.F.; Chin, K.-Y.; Abd Manaf, Z.; Mat Daud, N. Knowledge, attitude and practice related to vitamin D and its relationship with vitamin D status among Malay female office workers. Int. J. Environ. Res. Public Health 2019, 16, 4735. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, B.; Augustine, L.; Nair, K. Sun exposure as a strategy for acquiring vitamin D in developing countries of Tropical Region: Challenges & Way Forward. Indian J. Med. Res. 2021, 154, 423. [Google Scholar]
- Husna, K.; Widajanti, N.; Sumarmi, S.; Firdaus, H. Hubungan Antara Skor paparan Matahari Dan ASUPAN vitamin D Dengan Kadar 25(oh)d serum pada wanita usia lanjut. J. Penyakit Dalam Indones. 2021, 8, 63. [Google Scholar] [CrossRef]
- Al Anouti, F.; Thomas, J.; Abdel-Wareth, L.; Rajah, J.; Grant, W.B.; Haq, A. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermato-Endocrinology 2011, 3, 235–239. [Google Scholar] [CrossRef]
- Shuib, N.E.; Muniandy, D. Sun Protection Awareness among Schoolchildren in Malaysia; International Atomic Energy Agency: Vienna, Austria, 2018; Available online: https://inis.iaea.org/collection/NCLCollectionStore/_Public/51/073/51073888.pdf (accessed on 26 November 2023).
- Mendes, M.M.; Hart, K.H.; Botelho, P.B.; Lanham-New, S.A. Vitamin D status in the tropics: Is sunlight exposure the main determinant? Nutr. Bull. 2018, 43, 428–434. [Google Scholar] [CrossRef]
- Watson, M.; Holman, D.M.; Maguire-Eisen, M. Ultraviolet radiation exposure and its impact on Skin cancer risk. Semin. Oncol. Nurs. 2016, 32, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.E. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens Sci. Clin. Prac. 2011, 37, 246–249. [Google Scholar] [CrossRef] [PubMed]
| Frequency | Percentage (%) | |
|---|---|---|
| Gender | ||
| Male | 31 | 35.2 |
| Female | 57 | 64.8 |
| Total | 88 | 100.0 |
| Age | ||
| 18–24 | 5 | 5.7 |
| 25–34 | 12 | 13.6 |
| 35–44 | 19 | 21.6 |
| 45–54 | 14 | 15.9 |
| 55–64 | 23 | 26.1 |
| 65–74 | 13 | 14.8 |
| 75–84 | 0 | 0.00 |
| 85–94 | 2 | 2.30 |
| Total | 88 | 100.0 |
| Occupation | ||
| Administrative | 1 | 1.1 |
| Agriculture and fisheries | 4 | 4.5 |
| Cleaning services | 5 | 5.7 |
| Construction | 2 | 2.3 |
| Driver | 1 | 1.1 |
| Educator | 7 | 8.0 |
| Entrepreneur | 14 | 15.9 |
| Hospitality | 5 | 5.7 |
| Housewife | 21 | 23.9 |
| Manufacturing | 1 | 1.1 |
| Office job | 4 | 4.5 |
| Retired | 18 | 20.5 |
| Shop assistant | 2 | 2.3 |
| Unemployed | 3 | 3.4 |
| Total | 88 | 100.0 |
| Frequency | Percentage (%) | |
|---|---|---|
| Skin Tone | ||
| 1.00—Light, pale white | 5 | 5.7 |
| 2.00—Fair, white | 21 | 23.9 |
| 3.00—Medium to olive | 25 | 28.4 |
| 4.00—Olive | 22 | 25.0 |
| 5.00—Brown | 15 | 17.0 |
| 6.00—Dark brown to black | 0 | 0.0 |
| Total | 88 | 100.0 |
| Time Spent in the Sun | ||
| Early morning | 50 | 39.4% |
| Mid morning | 27 | 21.3% |
| Early afternoon | 15 | 11.8% |
| Late afternoon | 35 | 27.6% |
| Intentional Tanning | Occasions with Sunburn | Time Spent in the Midday Sun | Sun Vacation Abroad | Sunscreen Use | Protective Clothing Use | Protective Headwear Use | Staying in the Shade | Total Score | |
|---|---|---|---|---|---|---|---|---|---|
| Skin Type 1 (n = 5) | |||||||||
| Mean | 0.00 | 0.40 | 0.40 | 0.60 | 2.40 | 1.00 | 3.80 | 1.20 | 9.80 |
| Median | 0 | 0 | 0 | 0 | 3 | 0 | 4 | 0 | 11 |
| Skin Type 2 (n = 21) | |||||||||
| Mean | 0.33 | 0.14 | 0.67 | 0.38 | 1.76 | 0.57 | 3.14 | 0.90 | 7.90 |
| Median | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 1 | 7 |
| Skin Type 3 (n = 25) | |||||||||
| Mean | 0.24 | 0.20 | 0.88 | 0.16 | 2.92 | 0.80 | 2.44 | 0.92 | 8.56 |
| Median | 0 | 0 | 0 | 0 | 4 | 0 | 4 | 0 | 8 |
| Skin Type 4 (n = 22) | |||||||||
| Mean | 0.45 | 0.27 | 0.91 | 0.09 | 3.18 | 1.23 | 1.55 | 0.73 | 8.41 |
| Median | 0 | 0 | 0 | 0 | 4 | 0 | 1 | 0 | 8 |
| Skin Type 5 (n = 15) | |||||||||
| Mean | 0.00 | 0.00 | 1.47 | 0.27 | 4.00 | 2.27 | 1.67 | 1.07 | 10.73 |
| Median | 0 | 0 | 0 | 0 | 4 | 2 | 2 | 0 | 10 |
| p-value | 0.379 | 0.170 | 0.610 | 0.292 | 0.001 * | 0.005 * | 0.006 * | 0.924 | 0.070 |
| Intentional Tanning | Occasions with Sunburn | Time Spent in the Midday Sun | Sun Vacation Abroad | Sunscreen Use | Protective Clothing Use | Protective Headwear Use | Staying in the Shade | Total Score | |
|---|---|---|---|---|---|---|---|---|---|
| Female (n = 57) | |||||||||
| Mean | 0.14 | 0.09 | 0.63 | 0.23 | 2.21 | 0.32 | 2.71 | 0.93 | 7.27 |
| Median | 0 | 0 | 0 | 0 | 2 | 0 | 4 | 0 | 7 |
| Male (n = 31) | |||||||||
| Mean | 0.48 | 0.35 | 1.32 | 0.13 | 4.00 | 2.55 | 1.58 | 0.77 | 11.19 |
| Median | 0 | 0 | 0 | 0 | 4 | 2 | 1 | 0 | 11 |
| p-value | 0.445 | 0.465 | 0.159 | 0.501 | <0.001 *** | <0.001 *** | 0.03 | 0.463 | 0.001 *** |
| Giving Up Sunbathing | Sunscreen Use | Clothes for Sun Protection | Headwear for Sun Protection | Staying in the Shade | Total Score | |
|---|---|---|---|---|---|---|
| Skin Type 1 (n = 5) | ||||||
| Mean | 1.20 | 2.40 | 1.00 | 3.40 | 0.80 | 8.80 |
| Median | 0.00 | 3.00 | 0.00 | 4.00 | 0.00 | 8.00 |
| Skin Type 2 (n = 21) | ||||||
| Mean | 1.95 | 1.71 | 0.57 | 3.24 | 0.67 | 8.14 |
| Median | 1.00 | 0.00 | 0.00 | 4.00 | 0.00 | 8.00 |
| Skin Type 3 (n = 25) | ||||||
| Mean | 1.68 | 2.68 | 0.60 | 2.16 | 1.00 | 8.12 |
| Median | 0.00 | 4.00 | 0.00 | 4.00 | 0.00 | 8.00 |
| Skin Type 4 (n = 22) | ||||||
| Mean | 1.77 | 3.05 | 0.73 | 1.36 | 0.64 | 7.55 |
| Median | 0.00 | 4.00 | 0.00 | 0.00 | 0.00 | 8.00 |
| Skin Type 5 (n = 15) | ||||||
| Mean | 2.13 | 4.00 | 1.93 | 1.40 | 1.27 | 10.73 |
| Median | 4.00 | 4.00 | 2.00 | 1.00 | 0.00 | 10.00 |
| p-value | 0.884 | 0.002 * | 0.011 * | 0.006 * | 0.772 | 0.314 |
| Giving Up Sunbathing | Sunscreen Use | Clothes for Sun Protection | Headwear for Sun Protection | Staying in the Shade | Total Score | |
|---|---|---|---|---|---|---|
| Female (n = 57) | ||||||
| Mean | 1.75 | 2.16 | 0.26 | 2.72 | 0.81 | 7.70 |
| Median | 0.00 | 3.00 | 0.00 | 4.00 | 0.00 | 8.00 |
| Male (n = 31) | ||||||
| Mean | 1.94 | 3.84 | 2.00 | 1.13 | 0.97 | 9.87 |
| Median | 2.00 | 4.00 | 2.00 | 0.00 | 0.00 | 9.00 |
| p-value | 0.670 | <0.001 *** | <0.001 *** | <0.001 *** | 0.555 | 0.032 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gill, S.; Adenan, A.M.; Thomas, E.E.; Haleelur Rahman, A.; Rahim, N.B.A.; Ismail, N.A.S. Beyond the Tropics: Unraveling the Complex Relationship between Sun Exposure, Dietary Intake, and Vitamin D Deficiency in Coastal Malaysians. Nutrients 2024, 16, 830. https://doi.org/10.3390/nu16060830
Gill S, Adenan AM, Thomas EE, Haleelur Rahman A, Rahim NBA, Ismail NAS. Beyond the Tropics: Unraveling the Complex Relationship between Sun Exposure, Dietary Intake, and Vitamin D Deficiency in Coastal Malaysians. Nutrients. 2024; 16(6):830. https://doi.org/10.3390/nu16060830
Chicago/Turabian StyleGill, Shameena, Alia Maisara Adenan, Emillia Elza Thomas, Arifah Haleelur Rahman, Noor Baitee A. Rahim, and Noor Akmal Shareela Ismail. 2024. "Beyond the Tropics: Unraveling the Complex Relationship between Sun Exposure, Dietary Intake, and Vitamin D Deficiency in Coastal Malaysians" Nutrients 16, no. 6: 830. https://doi.org/10.3390/nu16060830
APA StyleGill, S., Adenan, A. M., Thomas, E. E., Haleelur Rahman, A., Rahim, N. B. A., & Ismail, N. A. S. (2024). Beyond the Tropics: Unraveling the Complex Relationship between Sun Exposure, Dietary Intake, and Vitamin D Deficiency in Coastal Malaysians. Nutrients, 16(6), 830. https://doi.org/10.3390/nu16060830







