Factors Influencing Duration of Breastfeeding: Insights from a Prospective Study of Maternal Health Literacy and Obstetric Practices
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Study Area
2.3. Inclusion and Exclusion Criteria
2.4. Sample Size
2.5. Baseline Variables
- Sociodemographic variables: maternal age, country of origin (Spain/foreign), level of education (primary to secondary school/university), employment status (professional to employee/unemployed/student), civil status (married/others), economic status (<EUR 1000 per month/>EUR 1000 per month), and financial status (bad–regular/good–very good).
- Health-literacy-related variables: HLS-EU-Q16, which assesses the population’s HL through a Likert scale with 16 items according to “very easy (1 point)”, “easy (1 point)”, “difficult (0 points)”, and “very difficult (0 points)”. This unifactorial scale exhibits good internal consistency, with a McDonald’s omega value of 0.982 in the Spanish population [22]. Level of HL: adequate (>12 points) or inadequate (≤12 points) (Supplementary Table S1).
- Obstetric–neonatal variables: gestational age at birth, parity (nulliparous/multiparous), type of onset of labour (spontaneous or elective Caesarean section/induced), type of rupture of membranes (spontaneous/artificial), group B streptococcus status (positive/negative), intrapartum antibiotic use (yes/no), intrapartum analgesia (inhalatory/local/epidural/none), Kristeller manoeuvre (yes/no), completion of birth (spontaneous vaginal/instrumental (vacuum, spatulas, forceps)/Caesarean section), episiotomy (yes/no), perineal condition following birth (intact/grade 1/grade 2/grade 3/grade 4) [23], newborn gender (female/male), newborn weight (grams), early skin-to-skin contact [(within 30 min and lasting for at least 2 continuous hours) (yes/no/with father)], early start of breastfeeding (within 2 h/after more than 2 h), drinking allowed during labour (yes/no), accompaniment of maternal choice allowed (yes/no), mobilization allowed during labour (yes/no), and positioning at the moment of birth (vertical/lying down—lithotomy position/lateral decubitus).
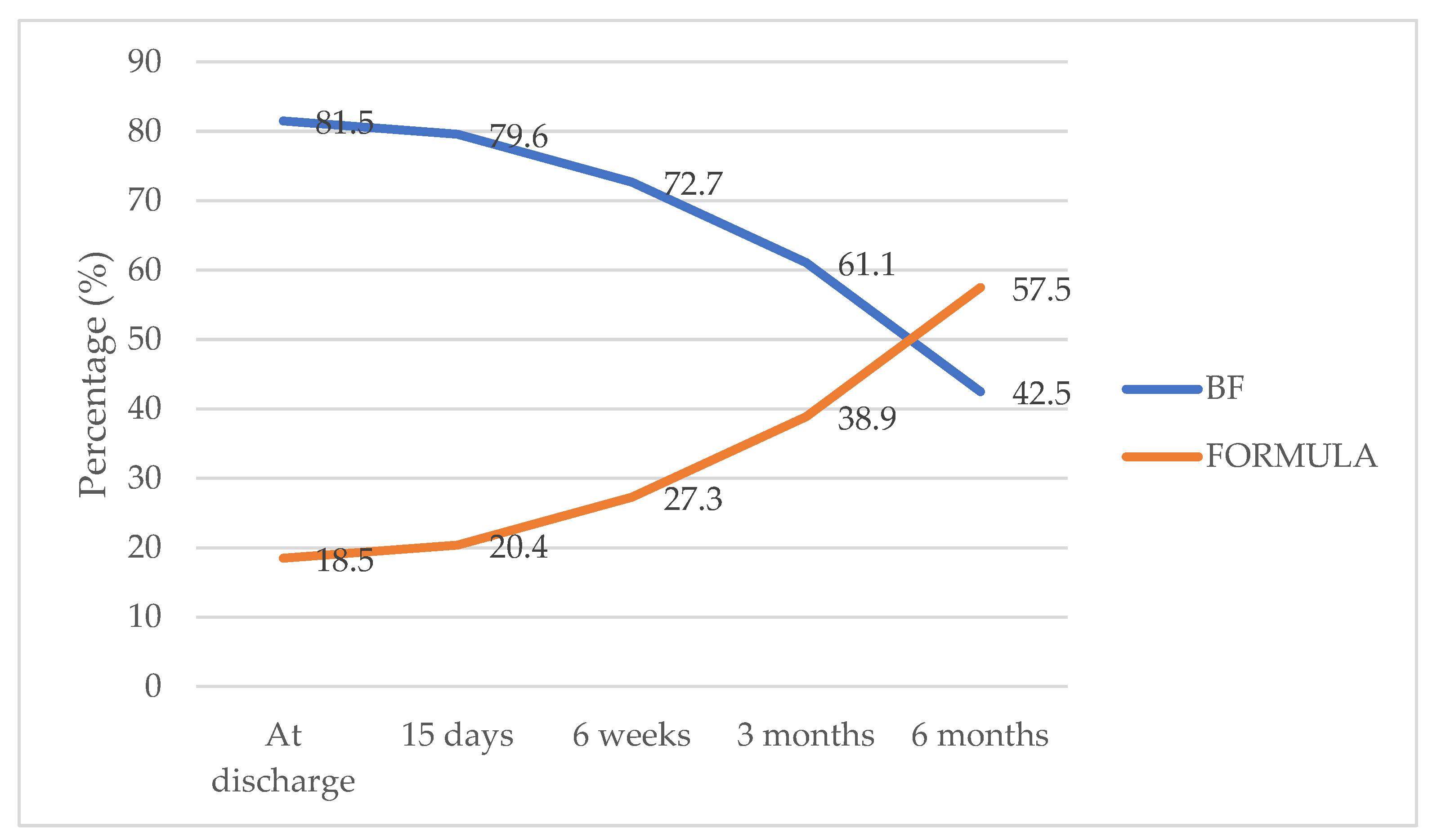
- Response variable: type of nursing (BF/supplementary feeding (SF)/mixed feeding (MF)) at 6 months postpartum, assessing the newborn and infant feeding practices. The response variable “Suspension of BF at 6 months” (yes/no) considered whether the infant was receiving SF (“yes”) or continued with BF or MF (“no”) at 6 months.
- Variables related to previous breastfeeding education: information/training in breastfeeding (none/previous information received from relatives; friends; or health professionals, such as midwives, pediatric nurses, obstetricians, and paediatricians); consultation of texts; participation in birth preparation groups, nursing groups, or postpartum groups; and the use of digital tools.
2.6. Data Collection
2.7. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Louis-Jacques, A.F.; Stuebe, A.M. Enabling Breastfeeding to Support Lifelong Health for Mother and Child. Obstet. Gynecol. Clin. N. Am. 2020, 47, 363–381. [Google Scholar] [CrossRef]
- Linde, K.; Lehnig, F.; Nagl, M.; Kersting, A. The association between breastfeeding and attachment: A systematic review. Midwifery 2020, 81, 102592. [Google Scholar] [CrossRef]
- World Health Organization (WHO); United Nations Children’s Fund (UNICEF). Protecting, Promoting and Supporting Breast-Feeding: The Special Role of Maternity Services/a Joint WHO/UNICEF Statement; World Health Organization: Geneva, Switzerland, 1989. [Google Scholar]
- World Health Organization; European Health Information Gateway. % of Infants Breastfed at Age 6 Months. Available online: https://gateway.euro.who.int/en/indicators/hfa_616-7260-of-infants-breastfed-at-age-6-months/#id=19721 (accessed on 23 January 2024).
- Instituto Nacional de Estadística (INE). Tipo de Lactancia Según Sexo y Clase Social Basada en la Ocupación de la Persona de Referencia. Población de 6 Meses a 4 Años. Encuesta Nacional de Salud España. Available online: https://www.ine.es/jaxi/Tabla.htm?path=/t15/p419/a2017/p06/l0/&file=06001.px&L=0 (accessed on 10 December 2023).
- Ramiro González, M.D.; Ortiz Marrón, H.; Arana Cañedo-Argüelles, C.; Esparza Olcina, M.J.; Cortés Rico, O.; Terol Claramonte, M.; Ordobás Gavín, M. Prevalence of breastfeeding and factors associated with the start and duration of exclusive breastfeeding in the Community of Madrid among participants in the ELOIN. An. Pediatr. 2018, 89, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Cabedo, R.; Manresa, J.M.; Cambredó, M.V.; Montero, L.; Reyes, A.; Gol, R.; Falguera, G. Tipos de lactancia materna y factores que influyen en su abandono hasta los 6 meses. Estudio LACTEM. Matronas Profesión 2019, 20, 54–61. [Google Scholar]
- López de Aberasturi Ibáñez de Garayo, A.; Santos Ibáñez, N.; Ramos Castro, Y.; García Franco, M.; Artola Gutiérrez, C.; Arara Vidal, I. Prevalence and determinants of breastfeeding: The Zorrotzaurre study. Nutr. Hosp. 2020, 38, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Vila-Candel, R.; Mena-Tudela, D.; Franco-Antonio, C.; Quesada, J.A.; Soriano-Vidal, F.J. Effects of a mobile application on breastfeeding maintenance in the first 6 months after birth: Randomised controlled trial (COMLACT study). Midwifery 2024, 128, 103874. [Google Scholar] [CrossRef]
- Liu, C.; Wang, D.; Liu, C.; Jiang, J.; Wang, X.; Chen, H.; Ju, X.; Zhang, X. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam. Med. Community Health 2020, 8, e000351. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef]
- Kaufman, H.; Skipper, B.; Small, L.; Terry, T.; McGrew, M. Effect of literacy on breast-feeding outcomes. South. Med. J. 2001, 94, 293–296. [Google Scholar] [CrossRef]
- Stafford, J.D.; Goggins, E.R.; Lathrop, E.; Haddad, L.B. Health Literacy and Associated Outcomes in the Postpartum Period at Grady Memorial Hospital. Matern. Child Health J. 2021, 25, 599–605. [Google Scholar] [CrossRef]
- Stafford, J.D.; Lathrop, E.; Haddad, L. Health Literacy and Associated Outcomes in the Postpartum Period at Grady Memorial Hospital [2H]. Obstet. Gynecol. 2016, 127, 66S–67S. [Google Scholar] [CrossRef]
- Mirjalili, N.; Jaberi, A.A.; Jaberi, K.A.; Bonabi, T.N. The role of maternal health literacy in breastfeeding pattern. J. Nurs. Midwifery Sci. 2018, 5, 53–58. [Google Scholar] [CrossRef]
- Graus, T.M.; Brandstetter, S.; Seelbach-Göbel, B.; Melter, M.; Kabesch, M.; Apfelbacher, C.; Fill Malfertheiner, S.; Ambrosch, A.; Arndt, P.; Baessler, A.; et al. Breastfeeding behavior is not associated with health literacy: Evidence from the German KUNO-Kids birth cohort study. Arch. Gynecol. Obstet. 2021, 304, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Shannon, T.; O‘donnell, M.J.; Skinner, K. Breastfeeding in the 21st Century: Overcoming Barriers to Help Women and Infants. Nurs. Women’s Heal. 2007, 11, 568–575. [Google Scholar] [CrossRef] [PubMed]
- Bohren, M.A.; Hofmeyr, G.J.; Sakala, C.; Fukuzawa, R.K.; Cuthbert, A. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2017, 7, CD003766. [Google Scholar] [CrossRef] [PubMed]
- Finnie, S.; Peréz-Escamilla, R.; Buccini, G. Determinants of early breastfeeding initiation and exclusive breastfeeding in Colombia. Public Health Nutr. 2020, 23, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Sen, K.K.; Mallick, T.S.; Bari, W. Gender inequality in early initiation of breastfeeding in Bangladesh: A trend analysis. Int. Breastfeed. J. 2020, 15, 18. [Google Scholar] [CrossRef]
- John, J.R.; Mistry, S.K.; Kebede, G.; Manohar, N.; Arora, A. Determinants of early initiation of breastfeeding in Ethiopia: A population-based study using the 2016 demographic and health survey data. BMC Pregnancy Childbirth 2019, 19, 69. [Google Scholar] [CrossRef]
- Nolasco, A.; Barona, C.; Tamayo-Fonseca, N.; Irles, M.Á.; Más, R.; Tuells, J.; Pereyra-Zamora, P. Alfabetización en salud: Propiedades psicométricas del cuestionario HLS-EU-Q16. Gac. Sanit. 2018, in press. [CrossRef]
- Alcaraz-Vidal, L.; Leon-Larios, F.; Robleda, G.; Vila-Candel, R. Exploring home births in Catalonia (Spain): A cross-sectional study of women’s experiences and influencing factors. J. Adv. Nurs. 2023, 1–16. [Google Scholar] [CrossRef]
- World Health Organization; UNICEF. Global Nutrion Target 2025. Breastfeeding Policy Brief; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Theurich, M.A.; Davanzo, R.; Busck-Rasmussen, M.; Díaz-Gómez, N.M.; Brennan, C.; Kylberg, E.; Bærug, A.; McHugh, L.; Weikert, C.; Abraham, K.; et al. Breastfeeding rates and programs in europe: A survey of 11 national breastfeeding committees and representatives. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 400–407. [Google Scholar] [CrossRef]
- Gaupšienė, A.; Vainauskaitė, A.; Baglajeva, J.; Stukas, R.; Ramašauskaitė, D.; Paliulytė, V.; Istomina, N. Associations between maternal health literacy, neonatal health and breastfeeding outcomes in the early postpartum period. Eur. J. Midwifery 2023, 7, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Estrela, M.; Semedo, G.; Roque, F.; Ferreira, P.L.; Herdeiro, M.T. Sociodemographic determinants of digital health literacy: A systematic review and meta-analysis. Int. J. Med. Inform. 2023, 177, 105124. [Google Scholar] [CrossRef]
- Vila-Candel, R.; Martínez-Arnau, F.M.; de la Cámara-de Las Heras, J.M.; Castro-Sánchez, E.; Pérez-Ros, P. Interventions to Improve Health among Reproductive-Age Women of Low Health Literacy: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 7405. [Google Scholar] [CrossRef] [PubMed]
- Vila-Candel, R.; Navarro-Illana, E.; Mena-Tudela, D.; Pérez-Ros, P.; Castro-Sánchez, E.; Soriano-Vidal, F.J.; Quesada, J.A. Influence of puerperal health literacy on tobacco use during pregnancy among spanish women: A transversal study. Int. J. Environ. Res. Public Health 2020, 17, 2910. [Google Scholar] [CrossRef] [PubMed]
- Valero-Chillerón, M.J.; Mena-Tudela, D.; Cervera-Gasch, Á.; González-Chordá, V.M.; Soriano-Vidal, F.J.; Quesada, J.A.; Castro-Sánchez, E.; Vila-Candel, R. Influence of Health Literacy on Maintenance of Exclusive Breastfeeding at 6 Months Postpartum: A Multicentre Study. Int. J. Environ. Res. Public Health 2022, 19, 5411. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sánchez, E.; Chang, P.W.S.; Vila-Candel, R.; Escobedo, A.A.; Holmes, A.H. Health literacy and infectious diseases: Why does it matter? Int. J. Infect. Dis. 2016, 43, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Valero-Chillerón, M.J.; Vila-Candel, R.; Mena-Tudela, D.; Soriano-Vidal, F.J.; González-Chordá, V.M.; Andreu-Pejo, L.; Antolí-Forner, A.; Durán-García, L.; Vicent-Ferrandis, M.; Andrés-Alegre, M.E.; et al. Development and Validation of the Breastfeeding Literacy Assessment Instrument (BLAI) for Obstetric Women. Int. J. Environ. Res. Public Health 2023, 20, 3808. [Google Scholar] [CrossRef] [PubMed]
- Berta, M.; Lindgren, H.; Christensson, K.; Mekonnen, S.; Adefris, M. Effect of maternal birth positions on duration of second stage of labor: Systematic review and meta-analysis. BMC Pregnancy Childbirth 2019, 19, 466. [Google Scholar] [CrossRef]
- Gupta, J.K.; Sood, A.; Hofmeyr, G.J.; Vogel, J.P. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database Syst. Rev. 2017, 2017, CD002006. [Google Scholar] [CrossRef]
- Jafari, E.; Mohebbi, P.; Mazloomzadeh, S. Factors related to women’s childbirth satisfaction in physiologic and routine childbirth groups. Iran. J. Nurs. Midwifery Res. 2017, 22, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Fan, H.S.L.; Fong, D.Y.T.; Lok, K.Y.W.; Tarrant, M. The Association Between Breastfeeding Self-Efficacy and Mode of Infant Feeding. Breastfeed. Med. 2022, 17, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Social Policy and Equality. Report on Attention to Delivery and Birth in the National Health System; Ministry of Health and Social Policy and Equality: Madrid, Spain, 2012. (In Spanish) [Google Scholar]
- Rydahl, E.; Eriksen, L.; Juhl, M. Effects of induction of labor prior to post-term in low-risk pregnancies: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 170–208. [Google Scholar] [CrossRef] [PubMed]
- Carlson, N.; Ellis, J.; Page, K.; Dunn Amore, A.; Phillippi, J. Review of Evidence-Based Methods for Successful Labor Induction. J. Midwifery Women’s Heal. 2021, 66, 459–469. [Google Scholar] [CrossRef]
- Froeliger, A.; Deneux-Tharaux, C.; Loussert, L.; Bouchghoul, H.; Madar, H.; Sentilhes, L. Prevalence and risk factors for postpartum depression 2 months after a vaginal delivery: A prospective multicenter study. Am. J. Obstet. Gynecol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Ponti, L.; Ghinassi, S.; Tani, F. Spontaneous and induced labor: Association with maternal well-being three months after childbirth. Psychol. Heal. Med. 2022, 27, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Slomian, J.; Honvo, G.; Emonts, P.; Reginster, J.Y.; Bruyère, O. Consequences of maternal postpartum depression: A systematic review of maternal and infant outcomes. Women’s Heal. 2019, 15, 1745506519844044. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Carrillo, G.H.; de Pablo, Á.L.L.; Arribas, S.M.; Ramiro-Cortijo, D. Association between maternal postpartum depression, stress, optimism, and breastfeeding pattern in the first six months. Int. J. Environ. Res. Public Health 2020, 17, 7153. [Google Scholar] [CrossRef]
- Vila-Candel, R.; Piquer-Martín, N.; Perdomo-Ugarte, N.; Quesada, J.A.; Escuriet, R.; Martin-Arribas, A. Indications of Induction and Caesarean Sections Performed Using the Robson Classification in a University Hospital in Spain from 2010 to 2021. Healthcare 2023, 11, 1521. [Google Scholar] [CrossRef]
- Turner, S.; McGann, B.; Brockway, M.M. A review of the disruption of breastfeeding supports in response to the COVID-19 pandemic in five Western countries and applications for clinical practice. Int. Breastfeed. J. 2022, 17, 38. [Google Scholar] [CrossRef]

| Early BF Abandonment in the Previous 6 Months | ||||||
|---|---|---|---|---|---|---|
| No n = 117 (42.5%) | Yes n = 158 (57.5%) | |||||
| n | % | n | % | p-Value * | ||
| Country of origin | Spain | 108 | 92.3 | 140 | 88.6 | 0.308 |
| Foreign | 9 | 7.7 | 18 | 11.4 | ||
| Education level | Primary to secondary school | 54 | 46.2 | 73 | 46.2 | 0.994 |
| University | 63 | 53.8 | 85 | 53.8 | ||
| Civil status | Others | 37 | 31.6 | 55 | 34.8 | 0.994 |
| Married | 80 | 68.4 | 103 | 65.2 | ||
| Employment status | Unemployed or student | 38 | 32.5 | 59 | 37.3 | 0.994 |
| Employee or professional | 79 | 67.5 | 99 | 62.7 | ||
| Economic status | <EUR 1000/month | 50 | 42.7 | 74 | 46.8 | 0.499 |
| >EUR 1000/month | 67 | 57.3 | 84 | 53.2 | ||
| Financial stability level | Bad or medium | 51 | 43.6 | 83 | 52.5 | 0.142 |
| Good or very good | 66 | 56.4 | 75 | 47.5 | ||
| Desired type of breastfeeding | Exclusive | 110 | 94 | 138 | 87.3 | 0.177 |
| Mixed | 5 | 4.3 | 13 | 8.2 | ||
| Not desired yet | 2 | 1.7 | 7 | 4.4 | ||
| Previous breastfeeding information | No information | 4 | 3.4 | 10 | 6.3 | 0.093 |
| Family or friend | 21 | 17.9 | 47 | 29.7 | ||
| Healthcare professional | 34 | 29.1 | 36 | 22.8 | ||
| Books | 10 | 8.5 | 5 | 3.2 | ||
| Birth preparation | 19 | 16.2 | 18 | 11.4 | ||
| Breastfeeding group | 1 | 0.9 | 1 | 0.6 | ||
| Digital tools | 28 | 23.9 | 41 | 25.9 | ||
| Health literacy level by HLS-EU-16Q | Inadequate | 28 | 23.9 | 56 | 35.4 | 0.040 |
| Adequate | 89 | 76.1 | 102 | 64.6 | ||
| Parity | Nulliparous | 81 | 69.2 | 121 | 76.6 | 0.172 |
| Multiparous | 36 | 30.8 | 37 | 23.4 | ||
| Pregnancy risk | Low risk | 92 | 78.6 | 118 | 74.7 | 0.649 |
| Gestational diabetes | 9 | 7.7 | 16 | 10.1 | ||
| Hypothyroidism | 4 | 3.4 | 5 | 3.2 | ||
| Preeclampsia/hypertension | 2 | 1.7 | 2 | 1.3 | ||
| Infertility | 1 | 0.9 | 1 | 0.6 | ||
| Premature birth | 0 | 0 | 4 | 2.5 | ||
| Other gestational diseases | 8 | 6.8 | 8 | 5.1 | ||
| Chronic condition with medication | 1 | 0.9 | 4 | 2.5 | ||
| Onset of labour | Spontaneous or elective C-section | 95 | 81.2 | 100 | 63.3 | 0.014 |
| Induction | 22 | 18.8 | 58 | 36.7 | ||
| Type of rupture of membranes | Spontaneous | 83 | 70.9 | 89 | 56.3 | 0.013 |
| Artificial | 34 | 29.1 | 69 | 43.7 | ||
| Streptococcus Agalactie B | Negative | 96 | 82.1 | 129 | 81.6 | 0.931 |
| Positive | 21 | 17.9 | 29 | 18.4 | ||
| Intrapartum use of antibiotic | No | 98 | 83.8 | 126 | 79.7 | 0.397 |
| Yes | 19 | 16.2 | 32 | 20.3 | ||
| Type of analgesia | Inhalator | 0 | 0 | 0 | 0 | 0.420 |
| Local | 3 | 2.6 | 8 | 5.1 | ||
| Epidural | 92 | 78.6 | 123 | 77.8 | ||
| Without analgesia | 9 | 7.7 | 16 | 10.1 | ||
| Spinal | 13 | 11.1 | 11 | 7 | ||
| Kristeller manoeuvre | No | 103 | 88 | 145 | 91.8 | 0.303 |
| Yes | 14 | 12 | 13 | 8.2 | ||
| Drinking allowed during labour | No | 28 | 23.9 | 57 | 36.1 | 0.031 |
| Yes | 89 | 76.1 | 101 | 63.9 | ||
| Labour accompaniment | No | 8 | 6.8 | 6 | 3.8 | 0.257 |
| Yes | 109 | 93.2 | 152 | 96.2 | ||
| Mobilization allowed during labour | No | 27 | 23.1 | 57 | 36.3 | 0.019 |
| Yes | 90 | 76.9 | 100 | 63.7 | ||
| Positioning in birth (n = 218) | Vertical | 8 | 8.4 | 21 | 17.1 | 0.087 |
| Lithotomy | 61 | 64.2 | 81 | 65.9 | ||
| Lateral decubitus | 26 | 27.4 | 21 | 17.1 | ||
| Type of birth | Spontaneous vaginal | 66 | 56.4 | 90 | 57 | 0.443 |
| Instrumental vaginal | 30 | 25.6 | 32 | 20.3 | ||
| C-section | 21 | 17.9 | 36 | 22.8 | ||
| Type of instrumental birth | Vacuum | 26 | 86.7 | 24 | 75 | 0.472 |
| Spatulas | 2 | 6.7 | 5 | 15.6 | ||
| Forceps | 2 | 6.7 | 3 | 9.4 | ||
| Episiotomy | No | 68 | 70.8 | 81 | 66.4 | 0.484 |
| Yes | 28 | 29.2 | 41 | 33.6 | ||
| Perineum injury | Intact | 19 | 27.9 | 27 | 32.5 | 0.846 |
| Grade I | 28 | 41.2 | 29 | 34.9 | ||
| Grade II | 20 | 29.4 | 25 | 30.1 | ||
| Grade III | 1 | 1.5 | 2 | 2.4 | ||
| Sex of newborn | Female | 63 | 53.8 | 75 | 47.5 | 0.296 |
| Male | 54 | 46.2 | 83 | 52.5 | ||
| Early skin-to-skin contact | No | 2 | 1.7 | 7 | 4.4 | 0.288 |
| Yes | 108 | 92.3 | 137 | 86.7 | ||
| Companion | 7 | 6 | 14 | 8.9 | ||
| Breastfeeding initiation | <2 h | 90 | 76.9 | 109 | 69 | 0.146 |
| >2 h | 27 | 23.1 | 49 | 31 | ||
| Mean | Median | Log Rank (Mantel–Cox) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimation | SE | 95% Confidence Interval | Estimation | SE | Chi-Square | df | p-Value | ||
| Lower Limit | Upper Limit | ||||||||
| HL level | |||||||||
| Inadequate | 89.17 | 8.18 | 73.13 | 105.2 | 80 | 28.41 | 6.615 | 1 | 0.01 |
| Adequate | 116.44 | 5.07 | 106.5 | 126.38 | 132 | ||||
| Global | 108.11 | 4.38 | 99.52 | 116.7 | 123 | 7.77 | |||
| Onset of labour | |||||||||
| Spontaneous or elective C-section | 112.74 | 5.37 | 102.22 | 123.26 | 145 | 8.25 | 1 | 0.004 | |
| Induction | 96.83 | 7.33 | 82.45 | 111.2 | 110 | 11.72 | |||
| Global | 108.11 | 4.38 | 99.52 | 116.7 | 123 | 7.77 | |||
| Type of rupture of membranes | |||||||||
| Spontaneous | 111.27 | 5.75 | 100 | 122.53 | 140 | 3.979 | 1 | 0.046 | |
| Artificial | 102.83 | 6.67 | 89.77 | 115.9 | 114 | 8.46 | |||
| Global | 108.11 | 4.38 | 99.52 | 116.7 | 123 | 7.77 | |||
| Drinking allowed during labour | |||||||||
| No | 92.4 | 8.01 | 76.69 | 108.11 | 99 | 20.49 | 5.513 | 1 | 0.019 |
| Yes | 115.14 | 5.15 | 105.04 | 125.24 | 130 | ||||
| Global | 108.11 | 4.38 | 99.52 | 116.7 | 123 | 7.77 | |||
| Mobilization allowed during labour | |||||||||
| No | 91.42 | 8.06 | 75.63 | 107.2 | 98 | 20.62 | 6.833 | 1 | 0.009 |
| Yes | 115.43 | 5.16 | 105.31 | 125.54 | 132 | ||||
| Global | 108.07 | 4.4 | 99.44 | 116.69 | 123 | 8.01 | |||
| B | SD | Wald | df | p-Value | Exp(B) | |
|---|---|---|---|---|---|---|
| HL level | −0.384 | 0.168 | 5.257 | 1 | 0.022 | 0.681 |
| Mobilization allowed during labour | −0.392 | 0.167 | 5.537 | 1 | 0.019 | 0.676 |
| Type of onset of labour | 0.431 | 0.167 | 6.640 | 1 | 0.010 | 1.538 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vila-Candel, R.; Soriano-Vidal, F.J.; Franco-Antonio, C.; Garcia-Algar, O.; Andreu-Fernandez, V.; Mena-Tudela, D. Factors Influencing Duration of Breastfeeding: Insights from a Prospective Study of Maternal Health Literacy and Obstetric Practices. Nutrients 2024, 16, 690. https://doi.org/10.3390/nu16050690
Vila-Candel R, Soriano-Vidal FJ, Franco-Antonio C, Garcia-Algar O, Andreu-Fernandez V, Mena-Tudela D. Factors Influencing Duration of Breastfeeding: Insights from a Prospective Study of Maternal Health Literacy and Obstetric Practices. Nutrients. 2024; 16(5):690. https://doi.org/10.3390/nu16050690
Chicago/Turabian StyleVila-Candel, Rafael, Francisco Javier Soriano-Vidal, Cristina Franco-Antonio, Oscar Garcia-Algar, Vicente Andreu-Fernandez, and Desirée Mena-Tudela. 2024. "Factors Influencing Duration of Breastfeeding: Insights from a Prospective Study of Maternal Health Literacy and Obstetric Practices" Nutrients 16, no. 5: 690. https://doi.org/10.3390/nu16050690
APA StyleVila-Candel, R., Soriano-Vidal, F. J., Franco-Antonio, C., Garcia-Algar, O., Andreu-Fernandez, V., & Mena-Tudela, D. (2024). Factors Influencing Duration of Breastfeeding: Insights from a Prospective Study of Maternal Health Literacy and Obstetric Practices. Nutrients, 16(5), 690. https://doi.org/10.3390/nu16050690









