Polycyclic Aromatic Hydrocarbons and Pancreatic Cancer: An Analysis of the Blood Biomarker, r-1,t-2,3,c-4-Tetrahydroxy-1,2,3,4-tetrahydrophenanthrene and Selected Metabolism Gene SNPs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Society, A.C. Key Statistics for Pancreatic Cancer. 2022, pp. 5–6. Available online: https://www.cancer.org/content/dam/CRC/PDF/Public/8778.00.pdf (accessed on 15 August 2023).
- Aier, I.; Semwal, R.; Sharma, A.; Varadwaj, P.K. A Systematic Assessment of Statistics, Risk Factors, and Underlying Features Involved in Pancreatic Cancer. Cancer Epidemiol. 2019, 58, 104–110. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Gaduputi, V. Epidemiology of Pancreatic Cancer: Global Trends, Etiology and Risk Factors. World J. Oncol. 2019, 10, 10–27. [Google Scholar] [CrossRef]
- Society, A.C. Pancreatic Cancer Risk Factors. 2020, p. 2. Available online: https://www.cancer.org/cancer/pancreatic-cancer/causes-risks-prevention/risk-factors.html#:~:text=Smoking%20is%20one%20of%20the,be%20caused%20by%20cigarette%20smoking (accessed on 24 July 2023).
- Pandol, S.J.; Apte, M.V.; Wilson, J.S.; Gukovskaya, A.S.; Edderkaoui, M. The Burning Question: Why Is Smoking a Risk Factor for Pancreatic Cancer? Pancreatology 2012, 12, 344–349. [Google Scholar] [CrossRef]
- Pang, Y.; Holmes, M.V.; Guo, Y.; Yang, L.; Bian, Z.; Chen, Y.; Iona, A.; Millwood, I.Y.; Bragg, F.; Chen, J.; et al. Smoking, Alcohol, and Diet in Relation to Risk of Pancreatic Cancer in China: A Prospective Study of 0.5 Million People. Cancer Med. 2018, 7, 229–239. [Google Scholar] [CrossRef]
- Taunk, P.; Hecht, E.; Stolzenberg-Solomon, R. Are Meat and Heme Iron Intake Associated with Pancreatic Cancer? Results from the NIH-AARP Diet and Health Cohort. Int. J. Cancer 2016, 138, 2172–2189. [Google Scholar] [CrossRef]
- CDC Polycyclic Aromatic Carbon (PAH) Factsheet. 2017. Available online: https://www.cdc.gov/biomonitoring/PAHs_FactSheet.html (accessed on 5 September 2023).
- Anderson, K.E.; Kadlubar, F.F.; Kulldorff, M.; Harnack, L.; Gross, M.; Lang, N.P.; Barber, C.; Rothman, N.; Sinha, R. Dietary Intake of Heterocyclic Amines and Benzo(a)Pyrene: Associations with Pancreatic Cancer. Cancer Epidemiol. Biomark. Prev. 2005, 14, 2261–2265. [Google Scholar] [CrossRef]
- Anderson, K.E.; Sinha, R.; Kulldorff, M.; Gross, M.; Lang, N.P.; Barber, C.; Harnack, L.; DiMagno, E.; Bliss, R.; Kadlubar, F.F. Meat Intake and Cooking Techniques: Associations with Pancreatic Cancer. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2002, 506–507, 225–231. [Google Scholar] [CrossRef]
- Anderson, K.E.; Mongin, S.J.; Sinha, R.; Stolzenberg-Solomon, R.; Gross, M.D.; Ziegler, R.G.; Mabie, J.E.; Risch, A.; Kazin, S.S.; Church, T.R. Pancreatic Cancer Risk: Associations with Meat-Derived Carcinogen Intake in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) Cohort. Mol. Carcinog. 2012, 51, 128–137. [Google Scholar] [CrossRef]
- Li, D.; Day, R.S.; Bondy, M.L.; Sinha, R.; Nguyen, N.T.; Evans, D.B.; Abbruzzese, J.L.; Hassan, M.M. Dietary Mutagen Exposure and Risk of Pancreatic Cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 655–661. [Google Scholar] [CrossRef]
- Stolzenberg-Solomon, R.Z.; Cross, A.J.; Silverman, D.T.; Schairer, C.; Thompson, F.E.; Kipnis, V.; Subar, A.F.; Hollenbeck, A.; Schatzkin, A.; Sinha, R. Meat and Meat-Mutagen Intake and Pancreatic Cancer Risk in the NIH-AARP Cohort. Cancer Epidemiol. Biomark. Prev. 2007, 16, 2664–2675. [Google Scholar] [CrossRef]
- Zhong, Y.; Carmella, S.G.; Hochalter, J.B.; Balbo, S.; Hecht, S.S. Analysis of R-7,t-8,9,c-10-Tetrahydroxy-7,8,9,10-Tetrahydrobenzo[a]Pyrene in Human Urine: A Biomarker for Directly Assessing Carcinogenic Polycyclic Aromatic Hydrocarbon Exposure plus Metabolic Activation. Chem. Res. Toxicol. 2011, 24, 73–80. [Google Scholar] [CrossRef]
- Luo, K.; Hochalter, J.B.; Carmella, S.G.; Hecht, S.S. Quantitation of Phenanthrene Dihydrodiols in the Urine of Smokers and Non-Smokers by Gas Chromatography-Negative Ion Chemical Ionization-Tandem Mass Spectrometry. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2020, 1141, 122023. [Google Scholar] [CrossRef]
- Jansen, R.J.; Robinson, D.P.; Frank, R.D.; Stolzenberg-Solomon, R.Z.; Bamlet, W.R.; Oberg, A.L.; Rabe, K.G.; Olson, J.E.; Petersen, G.M.; Sinha, R.; et al. Meat-Related Mutagens and Pancreatic Cancer: Null Results from a Clinic-Based Case–Control Study. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1336–1339. [Google Scholar] [CrossRef][Green Version]
- Carmella, S.G.; Ming, X.; Olvera, N.; Brookmeyer, C.; Yoder, A.; Hecht, S.S. High Throughput Liquid and Gas Chromatography-Tandem Mass Spectrometry Assays for Tobacco-Specific Nitrosamine and Polycyclic Aromatic Hydrocarbon Metabolites Associated with Lung Cancer in Smokers. Chem. Res. Toxicol. 2013, 26, 1209–1217. [Google Scholar] [CrossRef]
- Petersen, G.M.; Amundadottir, L.; Fuchs, C.S.; Kraft, P.; Stolzenberg-Solomon, R.Z.; Jacobs, K.B.; Arslan, A.A.; Bueno-de-Mesquita, H.B.; Gallinger, S.; Gross, M.; et al. A Genome-Wide Association Study Identifies Pancreatic Cancer Susceptibility Loci on Chromosomes 13q22.1, 1q32.1 and 5p15.33. Nat. Genet. 2010, 42, 224–228. [Google Scholar] [CrossRef]
- Subar, A.F.; Thompson, F.E.; Kipnis, V.; Midthune, D.; Hurwitz, P.; McNutt, S.; McIntosh, A.; Rosenfeld, S. Comparative Validation of the Block, Willett, and National Cancer Institute Food Frequency Questionnaires: The Eating at America′s Table Study. Am. J. Epidemiol. 2001, 154, 1089–1099. [Google Scholar] [CrossRef]
- R Program. Available online: https://www.w3resource.com/r-programming-exercises/basic/r-programming-basic-exercise-3.php (accessed on 15 August 2023).
- Zheng, J.; Guinter, M.A.; Merchant, A.T.; Wirth, M.D.; Zhang, J.; Stolzenberg-Solomon, R.Z.; Steck, S.E. Dietary Patterns and Risk of Pancreatic Cancer: A Systematic Review. Nutr Rev. 2017, 75, 883–908. [Google Scholar] [CrossRef]
- Huxley, R.; Ansary-Moghaddam, A.; González, A.B.D.; Barzi, F.; Woodward, M. Type-II Diabetes and Pancreatic Cancer: A Meta-Analysis of 36 Studies. Br. J. Cancer 2005, 92, 2076–2083. [Google Scholar] [CrossRef]
- Li, D. Diabetes and Pancreatic Cancer. Mol. Carcinog. 2012, 51, 64–74. [Google Scholar] [CrossRef]
- Bogovski, P.; Bogovski, S. Special Report Animal Species in Whichn-Nitroso Compounds Induce Cancer. Int. J. Cancer 1981, 27, 471–474. [Google Scholar] [CrossRef]
- Aschebrook-Kilfoy, B.; Cross, A.J.; Stolzenberg-Solomon, R.Z.; Schatzkin, A.; Hollenbeck, A.R.; Sinha, R.; Ward, M.H. Pancreatic Cancer and Exposure to Dietary Nitrate and Nitrite in the NIH-AARP Diet and Health Study. Am. J. Epidemiol. 2011, 174, 305–315. [Google Scholar] [CrossRef]
- Xie, L.; Mo, M.; Jia, H.-X.; Liang, F.; Yuan, J.; Zhu, J. Association between Dietary Nitrate and Nitrite Intake and Site-Specific Cancer Risk: Evidence from Observational Studies. Oncotarget 2016, 7, 56915–56932. [Google Scholar] [CrossRef] [PubMed]
- Abasse, K.S.; Essien, E.E.; Abbas, M.; Yu, X.; Xie, W.; Sun, J.; Akter, L.; Cote, A. Association between Dietary Nitrate, Nitrite Intake, and Site-Specific Cancer Risk: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 666. [Google Scholar] [CrossRef]
- Puel, A.; Cypowyj, S.; Bustamante, J.; Wright, J.F.; Liu, L.; Lim, H.K.; Migaud, M.; Israel, L.; Chrabieh, M.; Audry, M.; et al. Chronic Mucocutaneous Candidiasis in Humans with Inborn Errors of Interleukin-17 Immunity. Science 2011, 332, 65–68. [Google Scholar] [CrossRef]
- Takeuchi, A.; Miyamoto, T.; Yamaji, K.; Masuho, Y.; Hayashi, M.; Hayashi, H.; Onozaki, K. A Human Erythrocyte-Derived Growth-Promoting Factor with a Wide Target Cell Spectrum: Identification as Catalase. Cancer Res. 1995, 55, 1586–1589. [Google Scholar]
- Stelzer, G.; Rosen, R.; Plaschkes, I.; Zimmerman, S.; Twik, M.; Fishilevich, S.; Iny Stein, T.; Nudel, R.; Lieder, I.; Mazor, Y.; et al. The GeneCards Suite: From Gene Data Mining to Disease Genome Sequence Analyses. Curr. Protoc. Bioinform. 2016, 54, 1.30.1–1.30.33. [Google Scholar] [CrossRef]
- Rouhani, M.H.; Salehi-Abargouei, A.; Surkan, P.J.; Azadbakht, L. Is There a Relationship between Red or Processed Meat Intake and Obesity? A Systematic Review and Meta-Analysis of Observational Studies. Obes. Rev. 2014, 15, 740–748. [Google Scholar] [CrossRef]
- Jiao, L.; de Gonzalez, A.B.; Hartge, P.; Pfeiffer, R.M.; Park, Y.; Freedman, D.M.; Gail, M.H.; Alavanja, M.C.R.; Albanes, D.; Freeman, L.E.B.; et al. Body Mass Index, Effect Modifiers, and Risk of Pancreatic Cancer: A Pooled Study of Seven Prospective Cohorts. Cancer Causes Control 2010, 21, 1305–1314. [Google Scholar] [CrossRef]
- Xu, M.; Jung, X.; Hines, O.J.; Eibl, G.; Chen, Y. Obesity and Pancreatic Cancer. Pancreas 2018, 47, 158–162. [Google Scholar] [CrossRef]
- Patel, Y.M.; Park, S.L.; Carmella, S.G.; Paiano, V.; Olvera, N.; Stram, D.O.; Haiman, C.A.; Le Marchand, L.; Hecht, S.S. Metabolites of the Polycyclic Aromatic Hydrocarbon Phenanthrene in the Urine of Cigarette Smokers from Five Ethnic Groups with Differing Risks for Lung Cancer. PLoS ONE 2016, 11, e0156203. [Google Scholar] [CrossRef]
| Control | Case | OR [95% CI] | p.overall | |
|---|---|---|---|---|
| N = 198 Mean (SD) or N(%) | N = 202 Mean (SD) or N(%) | |||
| PheT (fmol/mL) | 16.9 (11.1) | 21.5 (25.1) | 1.01 [1.00;1.03] | 0.018 |
| Smoked: | 0.847 | |||
| Never | 101 (51.0%) | 106 (52.5%) | Ref. | |
| Former | 97 (49.0%) | 96 (47.5%) | 0.94 [0.64;1.40] | |
| Sex: | 0.815 | |||
| Female | 82 (41.4%) | 87 (43.1%) | Ref. | |
| Male | 116 (58.6%) | 115 (56.9%) | 0.93 [0.63;1.39] | |
| Age | 68.0 (10.7) | 68.5 (10.4) | 1.01 [0.99;1.02] | 0.600 |
| BMI | 27.2 (4.67) | 28.4 (5.66) | 1.04 [1.00;1.09] | 0.029 |
| Pack_Years | 10.6 (17.4) | 9.65 (17.1) | 1.00 [0.99;1.01] | 0.581 |
| Type_2_Diabetes: | <0.001 | |||
| No | 180 (90.9%) | 144 (71.3%) | Ref. | |
| Yes | 18 (9.09%) | 58 (28.7%) | 4.03 [2.27;7.14] |
| Control | Case | OR [95% CI] | p.overall | |
|---|---|---|---|---|
| N = 188 Mean (SD) | N = 93 Mean (SD) | |||
| PheT (fmol/mL) | 10.3 (7.65) | 15.2 (19.9) | 1.03 [1.01;1.05] | 0.023 |
| Very_Well_Done_Red_Meat(g) | 6.80 (7.09) | 4.10 (4.09) | 0.91 [0.87;0.97] | <0.001 |
| Total_Nitrite | 0.08 (0.09) | 0.05 (0.06) | 0.00 [0.00;0.15] | 0.001 |
| Fruits/Vegetables(servings) | 2.07 (1.14) | 2.46 (1.43) | 1.28 [1.05;1.55] | 0.022 |
| OR | Lower 95% CI | Upper 95% CI | p-Value | |
|---|---|---|---|---|
| Type_2_Diabetes | 6.26 | 2.83 | 14.46 | 9 × 10−6 |
| BMI | 1.04 | 0.97 | 1.11 | 0.025 |
| PheT | 1.01 | 0.99 | 1.03 | 0.232 |
| Very_Well_Done_Red_Meat(g) | 0.9 | 0.83 | 0.96 | 0.0019 |
| Fruits/Vegetables (servings) | 1.35 | 1.06 | 1.73 | 0.0155 |
| Total Nitrites | 0.01 | 0 | 0.81 | 0.0606 |
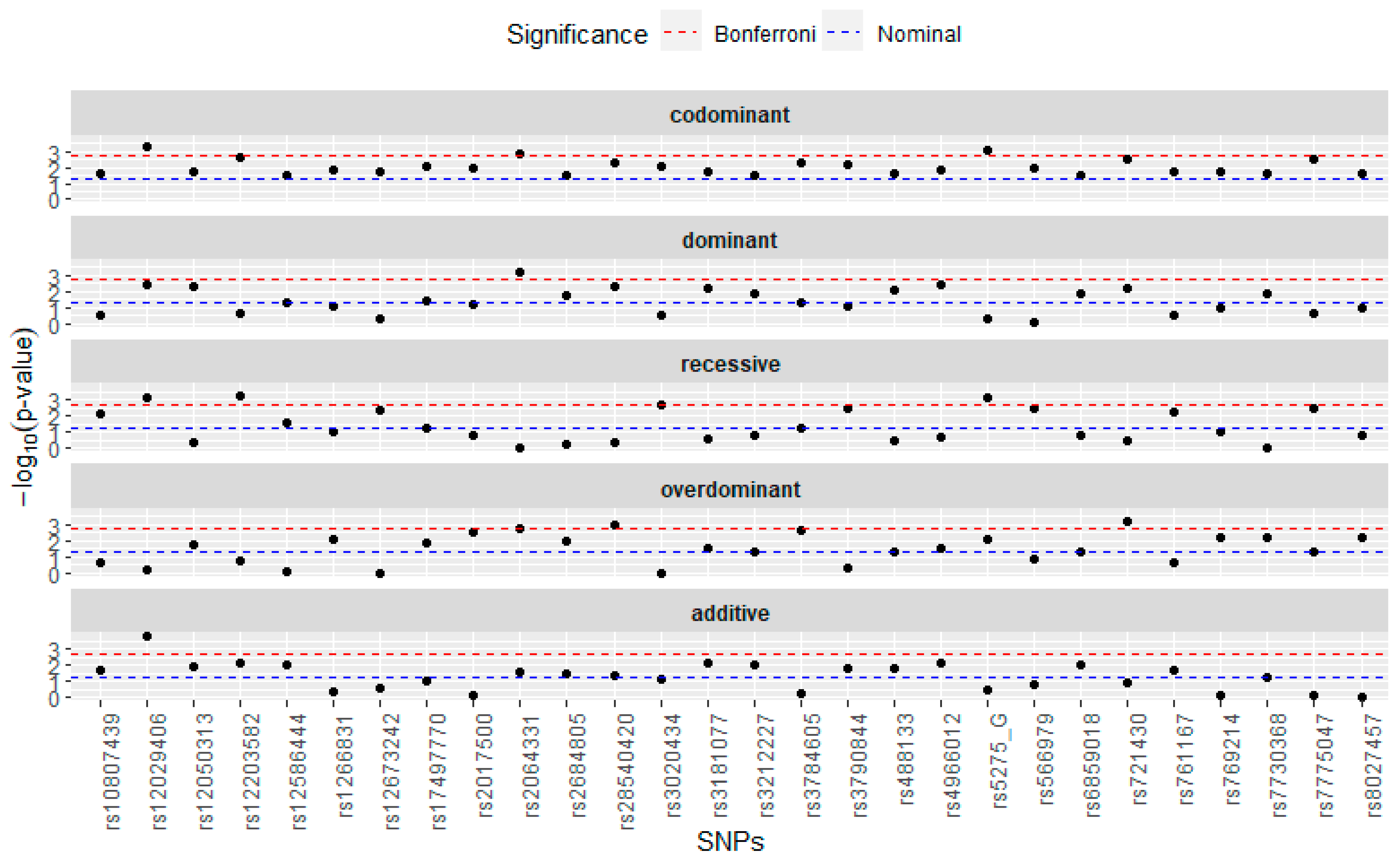
| Recessive (rs12203582) | 4.11 | 1.77 | 9.91 | 0.0012 |
| Recessive (rs566979) | 0.26 | 0.06 | 0.85 | 0.0421 |
| Overdominant (rs3784605) | 3.14 | 1.69 | 6.01 | 0.0004 |
| Overdominant (rs721430) | 0.39 | 0.19 | 0.76 | 0.0068 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, S.; Carlson, H.; Yoder, A.; Bamlet, W.R.; Oberg, A.L.; Petersen, G.M.; Carmella, S.G.; Hecht, S.S.; Jansen, R.J. Polycyclic Aromatic Hydrocarbons and Pancreatic Cancer: An Analysis of the Blood Biomarker, r-1,t-2,3,c-4-Tetrahydroxy-1,2,3,4-tetrahydrophenanthrene and Selected Metabolism Gene SNPs. Nutrients 2024, 16, 688. https://doi.org/10.3390/nu16050688
Nguyen S, Carlson H, Yoder A, Bamlet WR, Oberg AL, Petersen GM, Carmella SG, Hecht SS, Jansen RJ. Polycyclic Aromatic Hydrocarbons and Pancreatic Cancer: An Analysis of the Blood Biomarker, r-1,t-2,3,c-4-Tetrahydroxy-1,2,3,4-tetrahydrophenanthrene and Selected Metabolism Gene SNPs. Nutrients. 2024; 16(5):688. https://doi.org/10.3390/nu16050688
Chicago/Turabian StyleNguyen, Sierra, Heather Carlson, Andrea Yoder, William R. Bamlet, Ann L. Oberg, Gloria M. Petersen, Steven G. Carmella, Stephen S. Hecht, and Rick J. Jansen. 2024. "Polycyclic Aromatic Hydrocarbons and Pancreatic Cancer: An Analysis of the Blood Biomarker, r-1,t-2,3,c-4-Tetrahydroxy-1,2,3,4-tetrahydrophenanthrene and Selected Metabolism Gene SNPs" Nutrients 16, no. 5: 688. https://doi.org/10.3390/nu16050688
APA StyleNguyen, S., Carlson, H., Yoder, A., Bamlet, W. R., Oberg, A. L., Petersen, G. M., Carmella, S. G., Hecht, S. S., & Jansen, R. J. (2024). Polycyclic Aromatic Hydrocarbons and Pancreatic Cancer: An Analysis of the Blood Biomarker, r-1,t-2,3,c-4-Tetrahydroxy-1,2,3,4-tetrahydrophenanthrene and Selected Metabolism Gene SNPs. Nutrients, 16(5), 688. https://doi.org/10.3390/nu16050688






