Association of Physical Activity with Phenotypic Age among Populations with Different Breakfast Habits
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Data Measurement
2.2.1. Definition of PhenoAge
2.2.2. Definition of Physical Activity
2.2.3. Eating Breakfast
2.2.4. Covariate Assessment
2.3. Statistical Analysis
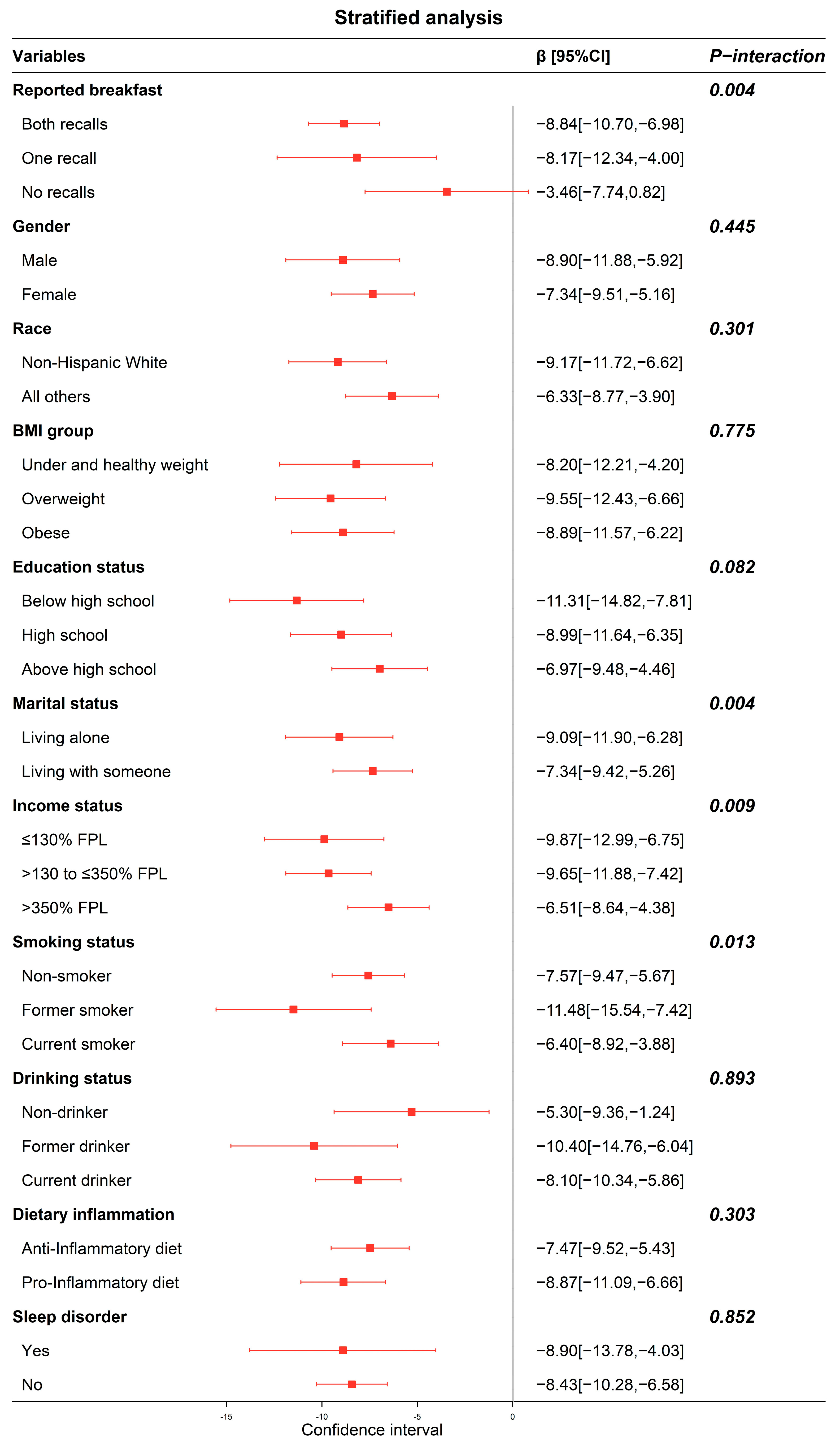
3. Results
4. Discussion
4.1. Study Strengths
4.2. Study Weaknesses
4.3. Future Research Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Serafini, M.M.; Catanzaro, M.; Rosini, M.; Racchi, M.; Lanni, C. Curcumin in Alzheimer’s disease: Can we think to new strategies and perspectives for this molecule? Pharmacol. Res. 2017, 124, 146–155. [Google Scholar] [CrossRef]
- Nations, T.U. World Social Report 2023; United Nations: New York, NY, USA, 2023. [Google Scholar]
- Liu, Z.; Kuo, P.-L.; Horvath, S.; Crimmins, E.; Ferrucci, L.; Levine, M. Correction: A new aging measure captures morbidity and mortality risk across diverse subpopulations from NHANES IV: A cohort study. PLoS Med. 2019, 16, e1002760. [Google Scholar] [CrossRef]
- Levine, M.E.; Lu, A.T.; Quach, A.; Chen, B.H.; Assimes, T.L.; Bandinelli, S.; Hou, L.; Baccarelli, A.A.; Stewart, J.D.; Li, Y.; et al. An epigenetic biomarker of aging for lifespan and healthspan. Aging 2018, 10, 573–591. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Pu, F.; Cao, X.; Li, X.; Sun, S.; Zhang, J.; Chen, C.; Han, L.; Yang, Y.; Wang, W.; et al. Does healthy lifestyle attenuate the detrimental effects of urinary polycyclic aromatic hydrocarbons on phenotypic aging? An analysis from NHANES 2001–2010. Ecotoxicol. Environ. Saf. 2022, 237, 113542. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-Y. Lifestyle Factors and Genetic Variants on 2 Biological Age Measures: Evidence from 94 443 Taiwan Biobank Participants. J. Gerontol. Ser. A 2022, 77, 1189–1198. [Google Scholar] [CrossRef] [PubMed]
- Peterman, J.E.; Loy, S.; Carlos, J.; Arena, R.; Kaminsky, L.A. Increasing physical activity in the community setting. Prog. Cardiovasc. Dis. 2021, 64, 27–32. [Google Scholar] [CrossRef]
- Carmona, J.J.; Michan, S. Biology of Healthy Aging and Longevity. Rev. Investig. Clin. 2016, 68, 7–16. [Google Scholar]
- Fiorito, G.; Caini, S.; Palli, D.; Bendinelli, B.; Saieva, C.; Ermini, I.; Valentini, V.; Assedi, M.; Rizzolo, P.; Ambrogetti, D.; et al. DNA methylation-based biomarkers of aging were slowed down in a two-year diet and physical activity intervention trial: The DAMA study. Aging Cell 2021, 20, e13439. [Google Scholar] [CrossRef] [PubMed]
- Uzhova, I.; Fuster, V.; Fernandez-Ortiz, A.; Ordovas, J.M.; Sanz, J.; Fernandez-Friera, L.; Lopez-Melgar, B.; Mendiguren, J.M.; Ibanez, B.; Bueno, H.; et al. The Importance of Breakfast in Atherosclerosis Disease. J. Am. Coll. Cardiol. 2017, 70, 1833–1842. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Ard, J.; Baskin, M.L.; Chiuve, S.E.; Johnson, H.M.; Kris-Etherton, P.; Varady, K.; American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; et al. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation 2017, 135, E96–E121. [Google Scholar] [CrossRef]
- Barr, S.I.; DiFrancesco, L.; Fulgoni, V.L., III. Consumption of Breakfast and the Type of Breakfast Consumed Are Positively Associated with Nutrient Intakes and Adequacy of Canadian Adults. J. Nutr. 2013, 143, 86–92. [Google Scholar] [CrossRef]
- Deshmukh-Taskar, P.R.; Radcliffe, J.D.; Liu, Y.; Nicklas, T.A. Do Breakfast Skipping and Breakfast Type Affect Energy Intake, Nutrient Intake, Nutrient Adequacy, and Diet Quality in Young Adults? NHANES 1999–2002. J. Am. Coll. Nutr. 2010, 29, 407–418. [Google Scholar] [CrossRef]
- Monacelli, F.; Acquarone, E.; Giannotti, C.; Borghi, R.; Nencioni, A. Vitamin C, Aging and Alzheimer’s Disease. Nutrients 2017, 9, 670. [Google Scholar] [CrossRef]
- Maltais, M.; Boisvert-Vigneault, K.; Rolland, Y.; Vellas, B.; de Souto Barreto, P.; MAPT/DSA Study Group. Longitudinal associations of physical activity levels with morphological and functional changes related with aging: The MAPT study. Exp. Gerontol. 2019, 128, 110758. [Google Scholar] [CrossRef]
- Zakrzewski-Fruer, J.K.; Gillison, F.B.; Katzmarzyk, P.T.; Mire, E.F.; Broyles, S.T.; Champagne, C.M.; Chaput, J.P.; Denstel, K.D.; Fogelholm, M.; Hu, G.; et al. Association between breakfast frequency and physical activity and sedentary time: A cross-sectional study in children from 12 countries. BMC Public Health 2019, 19, 222. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. The Overview of National Health and Nutrition Examination Survey. Available online: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm (accessed on 18 October 2023).
- Han, W.M.; Apornpong, T.; Gatechompol, S.; Ubolyam, S.; Chattranukulchai, P.; Wattanachanya, L.; Siwamogsatham, S.; Kerr, S.J.; Erlandson, K.M.; Avihingsanon, A. Association of Phenotypic Aging Marker with comorbidities, frailty and inflammatory markers in people living with HIV. BMC Geriatr. 2022, 22, 1010. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Physical Activity for Everyone (Online); Centers for Disease Control and Prevention: Atlanta, GA, USA. Available online: http://www.cdc.gov/physicalactivity/everyone/glossary/index.html (accessed on 18 October 2023).
- Armstrong, T.; Bull, F. Development of the World Health Organization Global Physical Activity Questionnaire (GPAQ). J. Public Health 2006, 14, 66–70. [Google Scholar] [CrossRef]
- Feng, Q.; Yang, Z.; May, M.; Tsoi, K.K.; Ingle, S.; Lee, E.K.; Wong, S.Y.; Kim, J.H. The role of body mass index in the association between dietary sodium intake and blood pressure: A mediation analysis with NHANES. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3335–3344. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Wang, X.; Wang, L.; Hu, W.; Yang, Y.; Yao, N.; Li, J.; Xie, Z.; Guo, R.; Wang, Y.; et al. The Mediating Role of Dietary Inflammatory Index in the Association between Eating Breakfast and Obesity: A Cross-Sectional Study. Nutrients 2022, 14, 4378. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey 2005–2006 Data Documentation, Codebook, and Frequencies. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2005-2006/DR1TOT_D.htm (accessed on 18 October 2023).
- Shivappa, N.; Steck, S.E.; Hurley, T.G.; Hussey, J.R.; Hebert, J.R. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014, 17, 1689–1696. [Google Scholar] [CrossRef]
- Kim, H.S.; Sohn, C.; Kwon, M.; Na, W.; Shivappa, N.; Hebert, J.R.; Kim, M.K. Positive Association between Dietary Inflammatory Index and the Risk of Osteoporosis: Results from the KoGES_Health Examinee (HEXA) Cohort Study. Nutrients 2018, 10, 1999. [Google Scholar] [CrossRef]
- Di Giosia, P.; Stamerra, C.A.; Giorgini, P.; Jamialahamdi, T.; Butler, A.E.; Sahebkar, A. The role of nutrition in inflammaging. Ageing Res. Rev. 2022, 77, 101596. [Google Scholar] [CrossRef]
- Tsereteli, N.; Vallat, R.; Fernandez-Tajes, J.; Delahanty, L.M.; Ordovas, J.M.; Drew, D.A.; Valdes, A.M.; Segata, N.; Chan, A.T.; Wolf, J.; et al. Impact of insufficient sleep on dysregulated blood glucose control under standardised meal conditions. Diabetologia 2022, 65, 356–365. [Google Scholar] [CrossRef] [PubMed]
- Pengpid, S.; Peltzer, K. Skipping Breakfast and Its Association with Health Risk Behaviour and Mental Health Among University Students in 28 Countries. Diabetes Metab. Syndr. Obes. 2020, 13, 2889–2897. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Stubbs, B.; Smith, L.; Hallgren, M.; Firth, J.; Herring, M.P.; Probst, M.; Koyanagi, A. Physical activity and sleep problems in 38 low- and middle-income countries. Sleep Med. 2018, 48, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Kase, B.E.; Liu, J.; Wirth, M.D.; Shivappa, N.; Hebert, J.R. Associations between dietary inflammatory index and sleep problems among adults in the United States, NHANES 2005–2016. Sleep Health 2021, 7, 273–280. [Google Scholar] [CrossRef]
- Davis, J.A.; Mohebbi, M.; Collier, F.; Loughman, A.; Staudacher, H.; Shivappa, N.; Hebert, J.R.; Pasco, J.A.; Jacka, F.N. The role of diet quality and dietary patterns in predicting muscle mass and function in men over a 15-year period. Osteoporos. Int. 2021, 32, 2193–2203. [Google Scholar] [CrossRef] [PubMed]
- Physical Status: The Use and Interpretation of Anthropometry: Report of a WHO Expert Committee; WHO Technical Report Series No. 854; WHO: Geneva, Switzerland, 1995; pp. 312–344.
- Sun, M.; Wang, L.; Wang, X.; Tong, L.; Fang, J.; Wang, Y.; Yang, Y.; Li, B. Interaction between sleep quality and dietary inflammation on frailty: NHANES 2005–2008. Food Funct. 2023, 14, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Eke, P.I.; Dye, B.A.; Wei, L.; Slade, G.D.; Thornton-Evans, G.O.; Borgnakke, W.S.; Taylor, G.W.; Page, R.C.; Beck, J.D.; Genco, R.J. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J. Periodontol. 2015, 86, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Fakhouri, T.H.; Carroll, M.D.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Adults, by Household Income and Education—United States, 2011–2014. MMWR-Morb. Mortal. Wkly. Rep. 2017, 66, 1369–1373. [Google Scholar] [CrossRef]
- Chang, H.-J.; Lin, K.-R.; Lin, M.-T.; Chang, J.-L. Associations Between Lifestyle Factors and Reduced Kidney Function in US Older Adults: NHANES 1999–2016. Int. J. Public Health 2021, 66, 1603966. [Google Scholar] [CrossRef]
- Lumley, T. Analysis of Complex Survey Samples. J. Stat. Softw. 2004, 9, 1–19. [Google Scholar] [CrossRef]
- Gordon, M.; Lumley, T. Forestplot: Advanced Forest Plot Using ‘Grid’ Graphics. Available online: http://CRAN.R-project.org/package=forestplot (accessed on 18 October 2023).
- Balan, E.; Decottignies, A.; Deldicque, L. Physical Activity and Nutrition: Two Promising Strategies for Telomere Maintenance? Nutrients 2018, 10, 1942. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, E.; Morales-Pison, S.; Urbina, F.; Solari, A. Aging Hallmarks and the Role of Oxidative Stress. Antioxidants 2023, 12, 651. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Xu, X. Dose- and Intensity-Response Associations Between Leisure-Time Physical Activity and Markers of Inflammation and Oxidative Stress in Older Adults. J. Aging Phys. Act. 2022, 30, 950–962. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.J.; Sartini, C.; Welsh, P.; Sattar, N.; Ash, S.; Lennon, L.T.; Wannamethee, S.G.; Lee, I.-M.; Whincup, P.H.; Jefferis, B.J. Physical Activity, Sedentary Behavior, and Inflammatory and Hemostatic Markers in Men. Med. Sci. Sports Exerc. 2017, 49, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Bird, L. Exercise lowers leptin and leukocytosis. Nat. Rev. Immunol. 2020, 20, 2–3. [Google Scholar] [CrossRef]
- Duglan, D.; Lamia, K.A. Clocking In, Working Out: Circadian Regulation of Exercise Physiology. Trends Endocrinol. Metab. 2019, 30, 347–356. [Google Scholar] [CrossRef]
- Campisi, J.; Kapahi, P.; Lithgow, G.J.; Melov, S.; Newman, J.C.; Verdin, E. From discoveries in ageing research to therapeutics for healthy ageing. Nature 2019, 571, 183–192. [Google Scholar] [CrossRef]
- Nas, A.; Mirza, N.; Haegele, F.; Kahlhofer, J.; Keller, J.; Rising, R.; Kufer, T.A.; Bosy-Westphal, A. Impact of breakfast skipping compared with dinner skipping on regulation of energy balance and metabolic risk. Am. J. Clin. Nutr. 2017, 105, 1351–1361. [Google Scholar] [CrossRef]
- Rong, S.; Snetselaar, L.G.; Xu, G.; Sun, Y.; Liu, B.; Wallace, R.B.; Bao, W. Association of Skipping Breakfast With Cardiovascular and All-Cause Mortality. J. Am. Coll. Cardiol. 2019, 73, 2025–2032. [Google Scholar] [CrossRef] [PubMed]
- Farshchi, H.R.; Taylor, M.A.; Macdonald, I.A. Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am. J. Clin. Nutr. 2005, 81, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Klop, B.; Proctor, S.D.; Mamo, J.C.; Botham, K.M.; Castro Cabezas, M. Understanding postprandial inflammation and its relationship to lifestyle behaviour and metabolic diseases. Int. J. Vasc. Med. 2012, 2012, 947417. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The Influence of Meal Frequency and Timing on Health in Humans: The Role of Fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef]
- Smith, H.A.; Betts, J.A. Nutrient timing and metabolic regulation. J. Physiol. 2022, 600, 1299–1312. [Google Scholar] [CrossRef]
- Deshmukh-Taskar, P.; Nicklas, T.A.; Radcliffe, J.D.; O’Neil, C.E.; Liu, Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults: The National Health and Nutrition Examination Survey (NHANES): 1999–2006. Public Health Nutr. 2013, 16, 2073–2082. [Google Scholar] [CrossRef]
- Mattson, M.P. Hormesis defined. Ageing Res. Rev. 2008, 7, 1–7. [Google Scholar] [CrossRef]
- Calabrese, E.J. Hormesis: Path and Progression to Significance. Int. J. Mol. Sci. 2018, 19, 2871. [Google Scholar] [CrossRef] [PubMed]
- Radak, Z.; Chung, H.Y.; Koltai, E.; Taylor, A.W.; Goto, S. Exercise, oxidative stress and hormesis. Ageing Res. Rev. 2008, 7, 34–42. [Google Scholar] [CrossRef]
- Ji, L.L.; Kang, C.; Zhang, Y. Exercise-induced hormesis and skeletal muscle health. Free Radic. Biol. Med. 2016, 98, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Santoro, A.; Martucci, M.; Conte, M.; Capri, M.; Franceschi, C.; Salvioli, S. Inflammaging, hormesis and the rationale for anti-aging strategies. Ageing Res. Rev. 2020, 64, 101142. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Mehdi, M.M. Oxidative stress, inflammation and hormesis: The role of dietary and lifestyle modifications on aging. Neurochem. Int. 2023, 164, 105490. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total (N = 3719) | Reported Breakfast in | F/χ2 | p | ||
|---|---|---|---|---|---|---|
| Both Recalls (N = 2940) | One Recall (N = 584) | No Recalls (N = 195) | ||||
| PhenoAge, years | 42.09(0.65) | 44.48(0.80) | 35.57(1.07) | 30.63(1.78) | 74.548 | <0.001 |
| PhenoAgeAccel, years | −5.53(0.17) | −5.64(0.21) | −5.32(0.28) | −4.87(0.56) | 2.676 | 0.069 |
| Physical activity | 1.137 | 0.566 | ||||
| Inactive | 1508(35.1) | 1205(35.5) | 228(33.8) | 75(34.0) | ||
| Active | 2211(64.9) | 1735(64.5) | 356(66.2) | 120(66.0) | ||
| Age, years | 47.62(0.57) | 50.12(0.71) | 40.89(0.91) | 35.50(1.58) | 119.795 | <0.001 |
| Gender | 21.978 | <0.001 | ||||
| Male | 1806(48.3) | 1383(46.4) | 299(52.4) | 124(59.6) | ||
| Female | 1913(51.7) | 1557(53.6) | 285(47.6) | 71(40.4) | ||
| Race | 19.291 | <0.001 | ||||
| Non-Hispanic White | 1969(73.7) | 1608(75.5) | 262(66.3) | 99(71.6) | ||
| All others | 1750(26.3) | 1332(24.5) | 322(33.7) | 96(28.4) | ||
| BMI, kg/m2 | 28.76(0.13) | 28.70(0.17) | 28.89(0.33) | 29.19(0.54) | 1.357 | 0.258 |
| BMI group | 6.540 | 0.162 | ||||
| Under and healthy weight | 1046(30.6) | 817(30.4) | 177(32.9) | 52(26.1) | ||
| Overweight | 1291(33.4) | 1045(34.2) | 176(29.0) | 70(35.8) | ||
| Obese | 1382(36.0) | 1078(35.4) | 231(38.1) | 73(38.1) | ||
| Education status | 16.130 | 0.003 | ||||
| Below high school | 1003(18.2) | 793(17.8) | 158(19.8) | 52(18.9) | ||
| High school | 880(23.4) | 667(21.9) | 146(25.2) | 67(36.1) | ||
| Above high school | 1836(58.4) | 1480(60.3) | 280(55.0) | 76(45.0) | ||
| Marital status | 37.107 | <0.001 | ||||
| Living alone | 1442(36.9) | 1069(34.0) | 270(43.8) | 103(53.5) | ||
| Living with someone | 2277(63.1) | 1871(66.0) | 314(56.2) | 92(46.5) | ||
| Income status | 54.803 | <0.001 | ||||
| ≤130% FPL | 1122(20.5) | 809(17.4) | 230(30.0) | 83(31.5) | ||
| >130 to ≤350% FPL | 1437(35.6) | 1158(36.3) | 203(31.7) | 76(38.0) | ||
| >350% FPL | 1160(43.9) | 973(46.3) | 151(38.3) | 36(30.5) | ||
| Smoking status | 104.174 | <0.001 | ||||
| Non-smoker | 2001(54.3) | 1620(55.7) | 292(49.6) | 89(50.4) | ||
| Former smoker | 989(26.8) | 834(29.1) | 128(22.5) | 27(10.3) | ||
| Current smoker | 729(18.9) | 486(15.2) | 164(27.9) | 79(39.3) | ||
| Drinking status | 17.223 | 0.002 | ||||
| Non-drinker | 480(10.3) | 411(11.4) | 56(7.1) | 13(5.4) | ||
| Former drinker | 552(12.3) | 439(13.0) | 88(10.6) | 25(9.1) | ||
| Current drinker | 2687(77.4) | 2090(75.6) | 440(82.3) | 157(85.5) | ||
| DII | −0.10(0.09) | −0.35(0.07) | 0.38(0.15) | 1.74(0.29) | 101.671 | <0.001 |
| Dietary inflammation | 119.751 | <0.001 | ||||
| Anti-Inflammatory | 1791(53.8) | 1543(58.9) | 209(43.5) | 39(20.2) | ||
| Pro-Inflammatory | 1928(46.2) | 1397(41.1) | 375(56.5) | 156(79.8) | ||
| Energy, kcal | 2119.99(19.50) | 2116.63(19.18) | 2203.81(68.86) | 1937.37(67.81) | 1.009 | 0.365 |
| Sleep disorder | 1.039 | 0.595 | ||||
| Yes | 275(7.1) | 224(7.4) | 38(5.6) | 13(6.9) | ||
| No | 3444(92.9) | 2716(92.6) | 546(94.4) | 182(93.1) | ||
| Model 1 a | Model 2 b | Model 3 c | ||||
|---|---|---|---|---|---|---|
| β [95%CI] | p | β [95%CI] | p | β [95%CI] | p | |
| Physical activity (reference = Inactive) | −10.39 [−12.45, −8.33] | <0.001 | −10.03 [−12.13, −7.92] | <0.001 | −8.36 [−10.09, −6.62] | <0.001 |
| Reported breakfast (reference = Both recalls) | — | — | — | — | — | — |
| One recall | −8.73 [−11.17, −6.29] | <0.001 | −7.98 [−10.50, −5.47] | <0.001 | −6.02 [−8.03, −4.01] | <0.001 |
| No recalls | −13.69 [−17.98, −9.41] | <0.001 | −13.72 [−18.01, −9.42] | <0.001 | −11.40 [−15.53, −7.26] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Z.; Li, J.; Xu, Y.; Guo, R.; Wang, F.; Liu, Y.; Wang, S.; Dong, Y.; Li, B. Association of Physical Activity with Phenotypic Age among Populations with Different Breakfast Habits. Nutrients 2024, 16, 575. https://doi.org/10.3390/nu16050575
Wu Z, Li J, Xu Y, Guo R, Wang F, Liu Y, Wang S, Dong Y, Li B. Association of Physical Activity with Phenotypic Age among Populations with Different Breakfast Habits. Nutrients. 2024; 16(5):575. https://doi.org/10.3390/nu16050575
Chicago/Turabian StyleWu, Zibo, Jing Li, Yang Xu, Ruirui Guo, Fengdan Wang, Yan Liu, Sizhe Wang, Yibo Dong, and Bo Li. 2024. "Association of Physical Activity with Phenotypic Age among Populations with Different Breakfast Habits" Nutrients 16, no. 5: 575. https://doi.org/10.3390/nu16050575
APA StyleWu, Z., Li, J., Xu, Y., Guo, R., Wang, F., Liu, Y., Wang, S., Dong, Y., & Li, B. (2024). Association of Physical Activity with Phenotypic Age among Populations with Different Breakfast Habits. Nutrients, 16(5), 575. https://doi.org/10.3390/nu16050575





