Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Inclusion Criteria
- RCTs evaluating the effects of IF on improving the cardiometabolic health of the ethnic Chinese population aged 18 years old or above, without restriction on the sex and health condition of the participants.
- Intervention with duration more than 3 weeks to capture the treatment effects of long-term duration only, with reference to a previous meta-analysis of RCTs that examined the efficacy of nutritional intervention on weight loss and body composition [14].
2.4. Exclusion Criteria
- Observational studies, review papers, comments, letters, news, notes, protocols, papers, or abstracts from conference proceedings.
- Studies without an abstract or full text in English or Simplified/Traditional Chinese.
- Studies without a control group.
2.5. Data Extraction
2.6. Quality and Risk-of-Bias Assessment
2.7. Outcomes
2.8. Statistical Analysis
3. Results
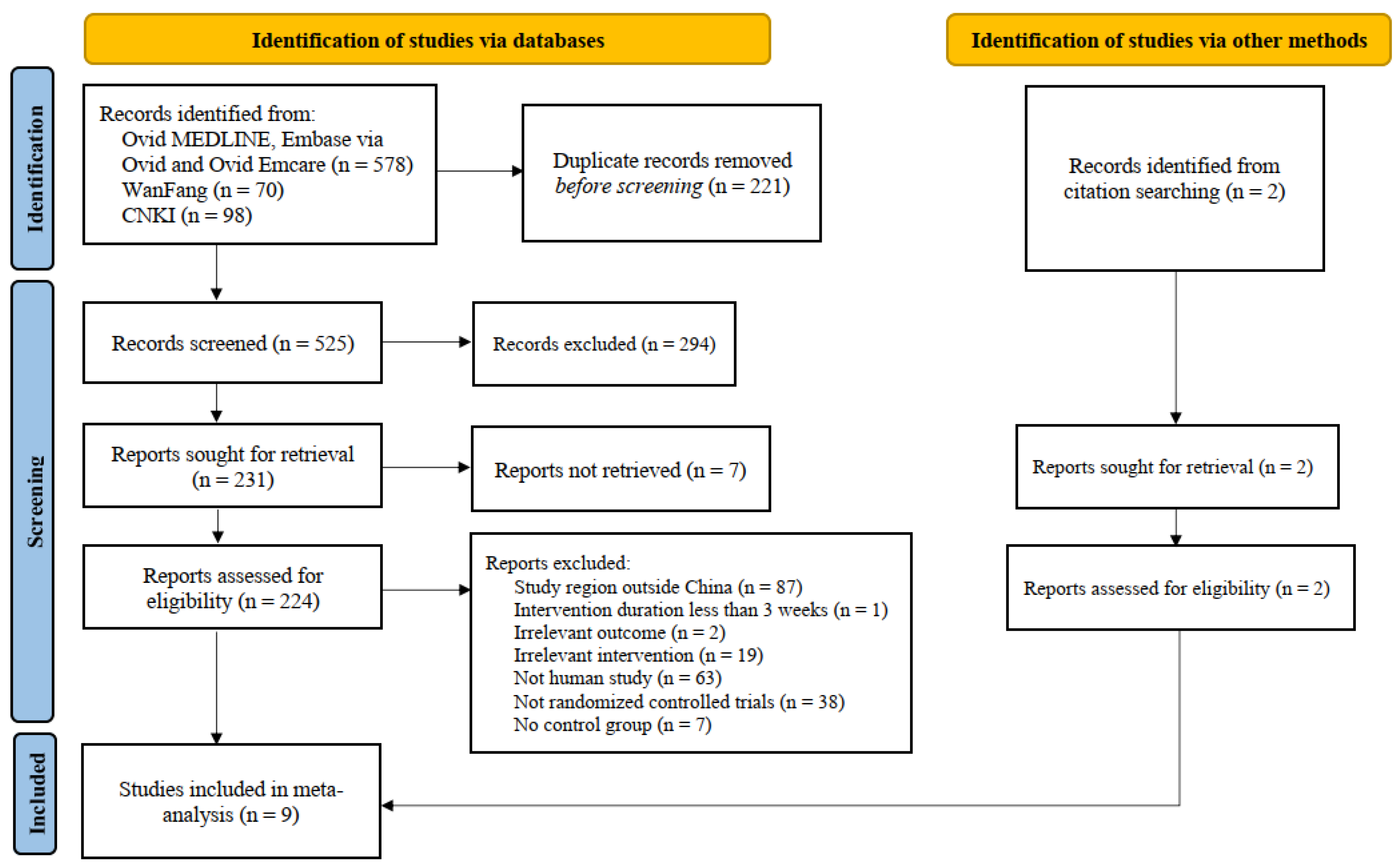
3.1. Study Selection
3.2. Study Characteristics
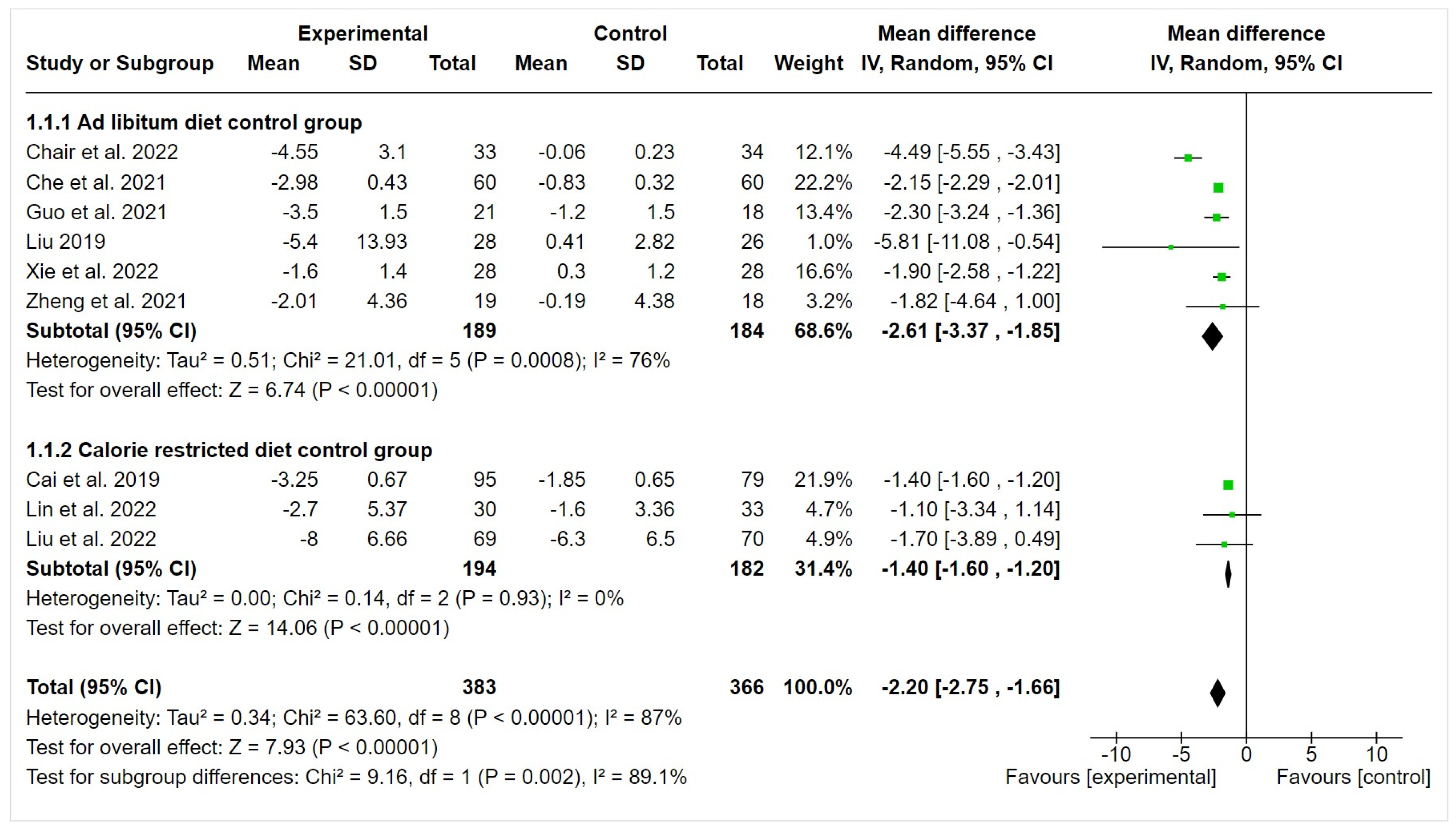
3.3. Effect on Anthropometric Measurement
3.4. Effect on Body Fat Composition
3.5. Effect on Blood Lipid Profile
3.6. Effect on Blood Glucose
3.7. Effect on Blood Pressure
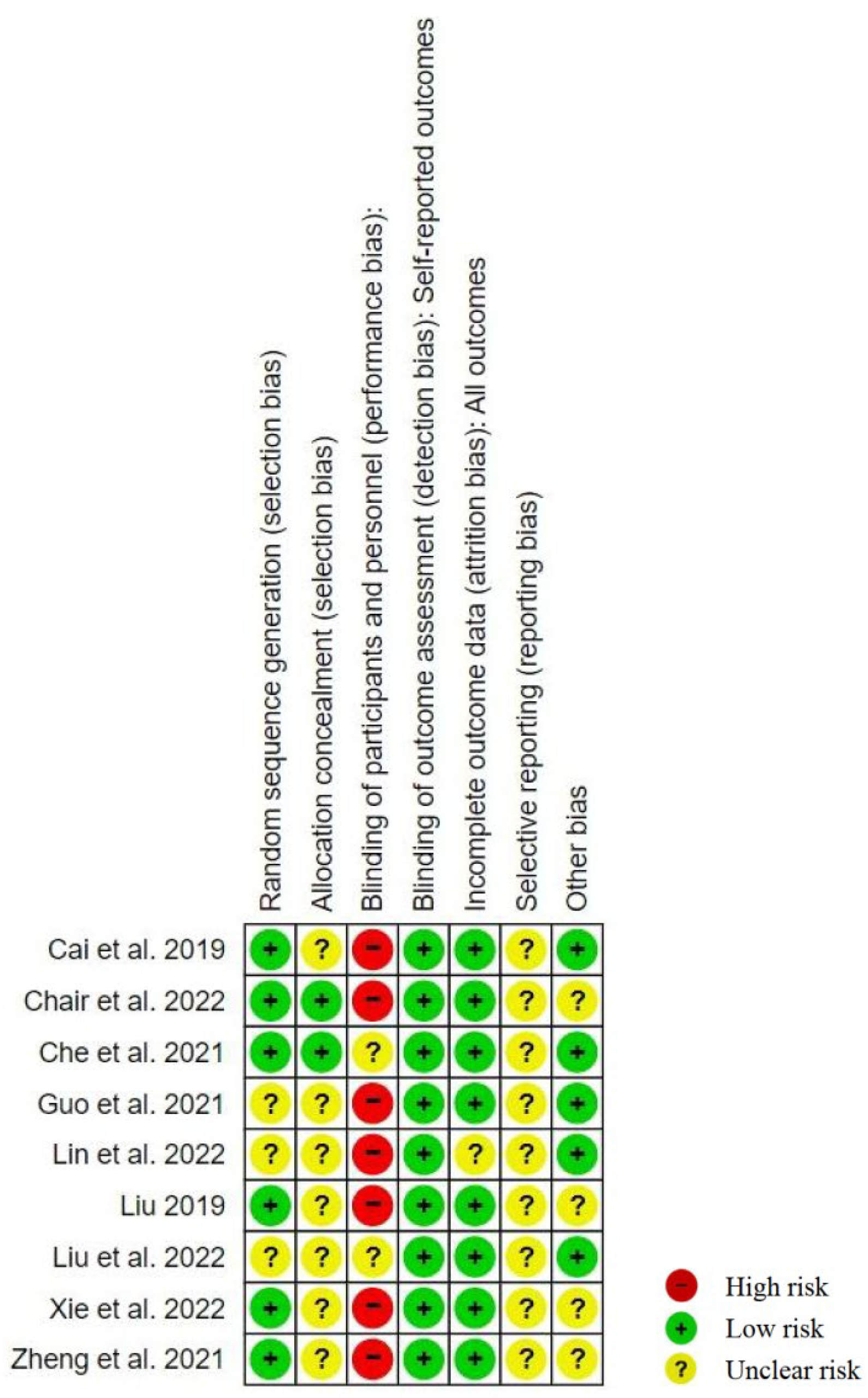
3.8. Risk-of-Bias Assessment
3.9. Safety
3.10. Sensitivity Analysis
4. Discussion
4.1. Summary of the Main Findings
4.2. Potential Mechanisms of Different IF Strategies
4.3. Additional Benefits of IF Compared with the Calorie-Restricted Diet
4.4. Adherence to IF Strategies in China
4.5. Adverse Events of IF in the Chinese Population
4.6. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, S.; Xi, B.; Yang, L.; Sun, J.; Zhao, M.; Bovet, P. Trends in the prevalence of overweight, obesity, and abdominal obesity among Chinese adults between 1993 and 2015. Int. J. Obes. 2021, 45, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Shen, Z.; Gu, W.; Lyu, Z.; Qi, X.; Mu, Y.; Ning, Y. Prevalence of obesity and associated complications in China: A cross-sectional, real-world study in 15.8 million adults. Diabetes Obes. Metab. 2023, 25, 3390–3399. [Google Scholar] [CrossRef]
- Hu, G. More vigorous efforts are needed to fight obesity, a serious public health problem in China. Obesity 2021, 29, 1580–1581. [Google Scholar] [CrossRef] [PubMed]
- Report on Cardiovascular Health and Diseases in China 2021: An Updated Summary. Biomed. Environ. Sci. 2022, 35, 573–603. [CrossRef]
- Pan, W.H.; Flegal, K.M.; Chang, H.Y.; Yeh, W.T.; Yeh, C.J.; Lee, W.C. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: Implications for definitions of overweight and obesity for Asians. Am. J. Clin. Nutr. 2004, 79, 31–39. [Google Scholar] [CrossRef]
- Wilhelmi de Toledo, F.; Grundler, F.; Sirtori, C.R.; Ruscica, M. Unravelling the health effects of fasting: A long road from obesity treatment to healthy life span increase and improved cognition. Ann. Med. 2020, 52, 147–161. [Google Scholar] [CrossRef]
- Anton, S.D.; Moehl, K.; Donahoo, W.T.; Marosi, K.; Lee, S.A.; Mainous, A.G.; Leeuwenburgh, C.; Mattson, M.P. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting: Flipping the Metabolic Switch. Obesity 2018, 26, 254–268. [Google Scholar] [CrossRef]
- De Cabo, R.; Mattson, M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N. Engl. J. Med. 2019, 381, 2541–2551. [Google Scholar] [CrossRef]
- Yang, F.; Liu, C.; Liu, X.; Pan, X.; Li, X.; Tian, L.; Sun, J.; Yang, S.; Zhao, R.; An, N.; et al. Effect of Epidemic Intermittent Fasting on Cardiometabolic Risk Factors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Nutr. 2021, 8, 669325. [Google Scholar] [CrossRef]
- Tang, R.; Wang, J.; Zhang, W.; Fu, W.; Zhuo, L.; Yang, J.; Wang, Q.; Kun, Y. Eating window and eating habits of adults in China: A cross-sectional study. Heliyon 2023, 9, e17233. [Google Scholar] [CrossRef]
- Kant, A.K. Eating patterns of US adults: Meals, snacks, and time of eating. Physiol. Behav. 2018, 193, 270–278. [Google Scholar] [CrossRef]
- Liu, D.; Huang, Y.; Huang, C.; Yang, S.; Wei, X.; Zhang, P.; Guo, D.; Lin, J.; Xu, B.; Li, C.; et al. Calorie Restriction with or without Time-Restricted Eating in Weight Loss. N. Engl. J. Med. 2022, 386, 1495–1504. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Talenezhad, N.; Mohammadi, M.; Ramezani-Jolfaie, N.; Mozaffari-Khosravi, H.; Salehi-Abargouei, A. Effects of l-carnitine supplementation on weight loss and body composition: A systematic review and meta-analysis of 37 randomized controlled clinical trials with dose-response analysis. Clin. Nutr. ESPEN 2020, 37, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3; Cochrane: Oxford, UK, 2022; Available online: https://training.cochrane.org/handbook (accessed on 17 July 2023).
- Wong, J.; Chan, K.Y.; Lo, K. Sodium-glucose co-transporter 2 inhibitors on weight change and cardiometabolic profiles in individuals with overweight or obesity and without diabetes: A meta-analysis. Obes. Rev. 2021, 22, e13336. [Google Scholar] [CrossRef]
- Cai, H.; Qin, Y.L.; Shi, Z.Y.; Chen, J.H.; Zeng, M.J.; Zhou, W.; Chen, R.Q.; Chen, Z.Y. Effects of alternate-day fasting on body weight and dyslipidaemia in patients with non-alcoholic fatty liver disease: A randomised controlled trial. BMC Gastroenterol. 2019, 19, 219. [Google Scholar] [CrossRef]
- Chair, S.Y.; Cai, H.; Cao, X.; Qin, Y.; Cheng, H.Y.; Ng, M.T. Intermittent Fasting in Weight Loss and Cardiometabolic Risk Reduction: A Randomized Controlled Trial. J. Nurs. Res. 2022, 30, e185. [Google Scholar] [CrossRef] [PubMed]
- Che, T.; Yan, C.; Tian, D.; Zhang, X.; Liu, X.; Wu, Z. Time-restricted feeding improves blood glucose and insulin sensitivity in overweight patients with type 2 diabetes: A randomised controlled trial. Nutr. Metab. 2021, 18, 88. [Google Scholar] [CrossRef]
- Guo, Y.; Luo, S.; Ye, Y.; Yin, S.; Fan, J.; Xia, M. Intermittent Fasting Improves Cardiometabolic Risk Factors and Alters Gut Microbiota in Metabolic Syndrome Patients. J. Clin. Endocrinol. Metab. 2021, 106, 64–79. [Google Scholar] [CrossRef]
- Lin, Y.J.; Wang, Y.T.; Chan, L.C.; Chu, N.F. Effect of time-restricted feeding on body composition and cardio-metabolic risk in middle-aged women in Taiwan. Nutrition 2022, 93, 111504. [Google Scholar] [CrossRef]
- Liu, D. The Effects of Intermittent Fasting with Appropriate amount of Exercise on Overweight and Obese People: A randomized Controlled Trial. Master’s Thesis, Nanchang University, Nanchang, China, 2019. [Google Scholar]
- Xie, Z.; Sun, Y.; Ye, Y.; Hu, D.; Zhang, H.; He, Z.; Zhao, H.; Yang, H.; Mao, Y. Randomized controlled trial for time-restricted eating in healthy volunteers without obesity. Nat. Commun. 2022, 13, 1003. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Liu, J.; Jiang, Y.; Pang, R.; Yang, X.; Liu, H.; Lin, N.; Li, Y.; Xiong, D.; Chen, X.; et al. Safety of Every-Other-Day Fasting in the Treatment of Spinal Cord Injury: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2021, 100, 1184–1189. [Google Scholar] [CrossRef] [PubMed]
- Yin, C.; Li, Z.; Xiang, Y.; Peng, H.; Yang, P.; Yuan, S.; Zhang, X.; Wu, Y.; Huang, M.; Li, J. Effect of Intermittent Fasting on Non-Alcoholic Fatty Liver Disease: Systematic Review and Meta-Analysis. Front. Nutr. 2021, 8, 709683. [Google Scholar] [CrossRef]
- Liu, J.; Yi, P.; Liu, F. The Effect of Early Time-Restricted Eating vs Later Time-Restricted Eating on Weight Loss and Metabolic Health. J. Clin. Endocrinol. Metab. 2023, 108, 1824–1834. [Google Scholar] [CrossRef] [PubMed]
- Antoni, R.; Johnston, K.L.; Collins, A.L.; Robertson, M.D. Intermittent v. continuous energy restriction: Differential effects on postprandial glucose and lipid metabolism following matched weight loss in overweight/obese participants. Br. J. Nutr. 2018, 119, 507–516. [Google Scholar] [CrossRef]
- Cienfuegos, S.; Gabel, K.; Kalam, F.; Ezpeleta, M.; Wiseman, E.; Pavlou, V.; Lin, S.; Oliveira, M.L.; Varady, K.A. Effects of 4- and 6-h Time-Restricted Feeding on Weight and Cardiometabolic Health: A Randomized Controlled Trial in Adults with Obesity. Cell. Metab. 2020, 32, 366–378.e363. [Google Scholar] [CrossRef] [PubMed]
- Gabel, K.; Kroeger, C.M.; Trepanowski, J.F.; Hoddy, K.K.; Cienfuegos, S.; Kalam, F.; Varady, K.A. Differential Effects of Alternate-Day Fasting Versus Daily Calorie Restriction on Insulin Resistance. Obesity 2019, 27, 1443–1450. [Google Scholar] [CrossRef]
- Sutton, E.F.; Beyl, R.; Early, K.S.; Cefalu, W.T.; Ravussin, E.; Peterson, C.M. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018, 27, 1212–1221.e1213. [Google Scholar] [CrossRef]
- Ferrannini, E. Is insulin resistance the cause of the metabolic syndrome? Ann. Med. 2006, 38, 42–51. [Google Scholar] [CrossRef]
- Albosta, M.; Bakke, J. Intermittent fasting: Is there a role in the treatment of diabetes? A review of the literature and guide for primary care physicians. Clin. Diabetes Endocrinol. 2021, 7, 3. [Google Scholar] [CrossRef]
- Rui, L. Energy metabolism in the liver. Compr. Physiol. 2014, 4, 177–197. [Google Scholar] [CrossRef]
- Santos, H.O.; Macedo, R.C.O. Impact of intermittent fasting on the lipid profile: Assessment associated with diet and weight loss. Clin. Nutr. ESPEN 2018, 24, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Harris, L.; Hamilton, S.; Azevedo, L.B.; Olajide, J.; De Brún, C.; Waller, G.; Whittaker, V.; Sharp, T.; Lean, M.; Hankey, C.; et al. Intermittent fasting interventions for treatment of overweight and obesity in adults: A systematic review and meta-analysis. JBI Database System. Rev. Implement. Rep. 2018, 16, 507–547. [Google Scholar] [CrossRef] [PubMed]
- Morales-Suarez-Varela, M.; Collado Sánchez, E.; Peraita-Costa, I.; Llopis-Morales, A.; Soriano, J.M. Intermittent Fasting and the Possible Benefits in Obesity, Diabetes, and Multiple Sclerosis: A Systematic Review of Randomized Clinical Trials. Nutrients 2021, 13, 3179. [Google Scholar] [CrossRef]
- Park, J.; Seo, Y.G.; Paek, Y.J.; Song, H.J.; Park, K.H.; Noh, H.M. Effect of alternate-day fasting on obesity and cardiometabolic risk: A systematic review and meta-analysis. Metabolism 2020, 111, 154336. [Google Scholar] [CrossRef]
- Khanna, D.; Peltzer, C.; Kahar, P.; Parmar, M.S. Body Mass Index (BMI): A Screening Tool Analysis. Cureus 2022, 14, e22119. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, C.; Wang, H.; Ma, Z.; Liu, D.; Guan, X.; Liu, Y.; Fu, Y.; Cui, M.; Dong, J. Intermittent Fasting versus Continuous Calorie Restriction: Which Is Better for Weight Loss? Nutrients 2022, 14, 1781. [Google Scholar] [CrossRef]
- Varkaneh Kord, H.; Tinsley, G.M.; Santos, H.O.; Zand, H.; Nazary, A.; Fatahi, S.; Mokhtari, Z.; Salehi-Sahlabadi, A.; Tan, S.C.; Rahmani, J.; et al. The influence of fasting and energy-restricted diets on leptin and adiponectin levels in humans: A systematic review and meta-analysis. Clin. Nutr. 2021, 40, 1811–1821. [Google Scholar] [CrossRef]
- Williamson, D.A.; Bray, G.A.; Ryan, D.H. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity 2015, 23, 2319–2320. [Google Scholar] [CrossRef]
- Zhou, B.F. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases-report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed. Environ. Sci. 2002, 15, 245–252. [Google Scholar]
- Khan, S.U.; Michos, E.D. Cardiovascular mortality after intensive LDL-Cholesterol lowering: Does baseline LDL-Cholesterol really matter? Am. J. Prev. Cardiol. 2020, 1, 100013. [Google Scholar] [CrossRef]
- Meng, H.; Zhu, L.; Kord-Varkaneh, H.; Santos, H.O.; Tinsley, G.M.; Fu, P. Effects of intermittent fasting and energy-restricted diets on lipid profile: A systematic review and meta-analysis. Nutrition 2020, 77, 110801. [Google Scholar] [CrossRef]
- Aksungar, F.B.; Sarıkaya, M.; Coskun, A.; Serteser, M.; Unsal, I. Comparison of Intermittent Fasting Versus Caloric Restriction in Obese Subjects: A Two Year Follow-Up. J. Nutr. Health Aging 2017, 21, 681–685. [Google Scholar] [CrossRef]
- Stekovic, S.; Hofer, S.J.; Tripolt, N.; Aon, M.A.; Royer, P.; Pein, L.; Stadler, J.T.; Pendl, T.; Prietl, B.; Url, J.; et al. Alternate Day Fasting Improves Physiological and Molecular Markers of Aging in Healthy, Non-obese Humans. Cell Metab. 2019, 30, 462–476.e466. [Google Scholar] [CrossRef]
- Harvie, M.N.; Pegington, M.; Mattson, M.P.; Frystyk, J.; Dillon, B.; Evans, G.; Cuzick, J.; Jebb, S.A.; Martin, B.; Cutler, R.G.; et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: A randomized trial in young overweight women. Int. J. Obes. 2011, 35, 714–727. [Google Scholar] [CrossRef]
- Patterson, R.E.; Sears, D.D. Metabolic Effects of Intermittent Fasting. Annu. Rev. Nutr. 2017, 37, 371–393. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.Y.; Desmet, L.; Depoortere, I. Time-restricted eating for chronodisruption-related chronic diseases. Acta Physiol. 2023, 239, e14027. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wei, R.; Pan, Q.; Guo, L. Beneficial effect of time-restricted eating on blood pressure: A systematic meta-analysis and meta-regression analysis. Nutr. Metab. 2022, 19, 77. [Google Scholar] [CrossRef] [PubMed]
- Wilhelmi de Toledo, F.; Grundler, F.; Bergouignan, A.; Drinda, S.; Michalsen, A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS ONE 2019, 14, e0209353. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.A.; Sandesara, P.B.; Dhindsa, D.S.; Mehta, A.; Arneson, L.C.; Dollar, A.L.; Taub, P.R.; Sperling, L.S. Intermittent Fasting: A Heart Healthy Dietary Pattern? Am. J. Med. 2020, 133, 901–907. [Google Scholar] [CrossRef]
- Varady, K.A. Intermittent versus daily calorie restriction: Which diet regimen is more effective for weight loss? Obes. Rev. 2011, 12, e593–e601. [Google Scholar] [CrossRef] [PubMed]
- Elortegui Pascual, P.; Rolands, M.R.; Eldridge, A.L.; Kassis, A.; Mainardi, F.; Lê, K.A.; Karagounis, L.G.; Gut, P.; Varady, K.A. A meta-analysis comparing the effectiveness of alternate day fasting, the 5:2 diet, and time-restricted eating for weight loss. Obesity 2023, 31 (Suppl. S1), 9–21. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Gill, J.M.R.; Alazawi, W. Improving prevention strategies for cardiometabolic disease. Nat. Med. 2020, 26, 320–325. [Google Scholar] [CrossRef]
- Zhou, Y.; Wang, J.; Duan, Y.; Luo, X.; Wan, Z.; Luo, Y.; Li, Y.; Wang, Y.; Xie, J. Dietary diversity and determinants of young adults in central China: A cross-sectional study from 2015 to 2020. Front. Nutr. 2022, 9, 931107. [Google Scholar] [CrossRef]
- Parr, E.B.; Devlin, B.L.; Hawley, J.A. Perspective: Time-Restricted Eating-Integrating the What with the When. Adv. Nutr. 2022, 13, 699–711. [Google Scholar] [CrossRef]
- Grajower, M.M.; Horne, B.D. Clinical Management of Intermittent Fasting in Patients with Diabetes Mellitus. Nutrients 2019, 11, 873. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Ang, W.H.D.; Tan, Z.Y.A.; Ang, W.W.; Chan, K.S.; Lau, Y. Umbrella review of time-restricted eating on weight loss, fasting blood glucose, and lipid profile. Nutr. Rev. 2022, 81, 1180–1199. [Google Scholar] [CrossRef]
- Faris, M.A.; Jahrami, H.; BaHammam, A.; Kalaji, Z.; Madkour, M.; Hassanein, M. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on glucometabolic markers in healthy subjects. Diabetes Res. Clin. Pract. 2020, 165, 108226. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Alsibai, J.; Clark, C.C.T.; Faris, M.A.E. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur. J. Nutr. 2020, 59, 2291–2316. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Study Location | Follow-Up Period | Subject (n) | Comorbidities of Participants | IF Method | Comparator | Age ± SD | Gender (% of Male) | Baseline Weight ± SD (kg) | Weight Change (%) | Baseline BMI ± SD (kg/m2) | Other Outcomes | Reported Adverse Events | Compliance to IF |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cai et al., 2019 [17] | Changsha, Hunan Province | 12 weeks | 264 | Patients with non-alcoholic fatty liver dis | (i) 16:8 TRE (freely arranged) (n = 95) (ii) ADF (n = 90) | Consumed 80% of energy needs every day (n = 79) | Intervention: (i) TRE: 33.56 ± 6.23 (ii) ADF: 35.50 ± 4.42 Control group: 34.54 ± 6.96 | 33.0 | Intervention: (i) TRE: 74.98 ± 8.02 (ii) ADF: 75.32 ± 8.53 Control: 72.94 ± 8.00 | Intervention: (i) TRE: −4.4% (ii) ADF: −5.4% Control: −1.6% | Intervention: (i) TRE: 26.76 ± 1.59 (ii) ADF: 26.12 ± 2.21 Control: 26.34 ± 2.73 | WC, BFM, TC, HDL-C, LDL-C, TG, GLU | No severe adverse events | Intervention: 97.5% |
| Chair et al., 2022 [18] | Changsha, Hunan Province | 3 weeks | 101 | Overweight and obese individuals with prediabetes | (i) 16:8 TRE (freely arranged) (n = 33) (ii) ADF (n = 34) | Eating ad libitum (n = 34) | Intervention: (i) TRE: 36.06 ± 7.67 (ii) ADF: 34.68 ± 4.37 Control: 34.97 ± 6.23 | 36.7 | Intervention: (i) TRE: 74.98 ± 8.02 (ii) ADF: 75.78 ± 8.46 Control: 72.15 ± 8.47 | Intervention: (i) TRE: −6.1% (ii) ADF: −6.4% Control: −0.1% | Intervention: (i) TRE: 26.74 ± 1.58 (ii) ADF: 26.46 ± 2.36 Control: 26.47 ± 1.84 | WC, TC, HDL-C, LDL-C, TG, GLU | No severe adverse events | Not available |
| Che et al., 2021 [19] | Tianjin | 12 weeks | 120 | Overweight patients with type 2 diabetes | 14:10 TRE (08:00–18:00) (n = 60) | Eating ad libitum (n = 60) | Intervention: 48.21 ± 9.32 Control: 48.78 ± 9.56 | 54.2 | Intervention: 75.06 ± 4.42 Control: 74.68 ± 4.35 | Intervention: −4.0% Control: −1.1% | Intervention: 26.42 ± 1.96 Control: 26.08 ± 2.14 | TC, HDL-C, LDL-C, TG, FPG, HOMA-IR | No severe adverse events | Intervention: >6 days per week |
| Guo et al., 2021 [20] | Dongguan, Guangdong Province | 8 weeks | 39 | Patients with metabolic syndrome | 5:2 diet (n = 21) | Eating ad libitum (n = 18) | Intervention: 40.2 ± 5.7 Control: 42.7 ± 4.1 | 53.8 | Intervention: 77.8 ± 13.6 Control: 74.1 ± 8.6 | Intervention: −4.5% Control: −1.6% | Intervention: 28.0 ± 7.8 Control: 27.7 ± 2.3 | WC, BFM, TC, HDL-C, LDL-C, TG, GLU, HOMA-IR, SBP, DBP | No severe adverse events | Intervention: 91.3% Control: 78.3% |
| Lin et al., 2022 [21] | Taiwan | 8 weeks | 63 | Middle-aged perimenopausal women with BMI > 24 kg/m2 or WC > 80 cm | 16:8 TRE (10:00–18:00 or 12:00–20:00) (n = 30) | Daily low-calorie diet of 1400 kcal (n = 33) | Intervention: 50.1 ± 7.5 Control: 54.2 ± 7.9 | 0 | Intervention: 65.9 ± 9.7 Control: 65.8 ± 8.8 | Intervention: −4.1% Control: −2.4% | Intervention: 25.9 ± 3.7 Control: 25.7 ± 3.8 | WC, TC, HDL-C, LDL-C, TG, GLU, HOMA-IR, SBP, DBP | Not mentioned | Intervention: 84% |
| Liu, 2019 [22] | Nanchang, Jiangxi Province | 20 weeks | 54 | Overweight and obese people | 5:2 diet (n = 28) | Eating ad libitum with moderate exercise (n = 26) | Intervention: 43.04 ± 8.75 Control: 41.69 ± 8.56 | 31.5 | Intervention: 72.96 ± 10.94 Control: 72.59 ± 8.26 | Intervention: −7.4% Control: +0.6% | Intervention: 27.41 ± 2.52 Control: 27.94 ± 1.85 | WC, TC, HDL-C, LDL-C, TG, FPG, SBP, DBP | Decreased concentration, thirsty, dizziness, low blood sugar level, abdominal bloating, constipation, unstable emotion | Not available |
| Liu et al., 2022 [12] | Guangzhou, Guangdong Province | 12 months | 139 | Patients with obesity | 16:8 TRE (08:00–16:00) (n = 69) | Daily calorie restriction by 75% (n = 70) | 31.9 ± 9.1 | 51.1 | 88.2 ± 11.6 | Intervention: −9.0% Control: −7.2% | Intervention: 31.8 ± 2.9 Control: 31.3 ± 2.6 | WC, BFM, TC, HDL-C, LDL-C, TG, GLU, SBP, DBP, HOMA–IR | No deaths or serious adverse events, occurrences of mild adverse events were similar in the two groups | Intervention: 84.0% Control: 83.8% |
| Xie et al., 2022 [23] | Beijing | 5 weeks | 82 | Healthy individuals without obesity | Early 16:8 TRE (06:00–15:00) (n = 28) Mid-day 16:8 TRE (11:00–20:00) (n = 26) | Eating ad libitum (n = 28) | Intervention: (i) eTRE: 28.68 ± 9.71 (ii) mTRE: 31.08 ± 8.44 Control: 33.57 ± 11.60 | 22.0 | Intervention: (i) eTRE: 61.1 ± 8.8 (ii) mTRE: 61.0 ± 11.7 Control: 61.2 ± 9.9 | Intervention: (i) eTRE: −2.6% (ii) mTRE: −0.3% Control: +0.5% | Intervention: (i) eTRE: 22.7 ± 3.1 (ii) mTRE: 21.4 ± 2.2 Control: 21.5 ± 2.9 | BFM, FPG, HOMA-IR | No severe adverse events | Intervention: 96.8% |
| Zheng et al., 2021 [24] | Chengdu, Sichuan Province | 8 weeks | 37 | Patients with spinal cord injury | ADF (n = 19) | Eating ad libitum (n = 18) | 35.76 ± 6.92 | 91.9 | Intervention: 61.06 ± 6.29 Control: 61.44 ± 5.29 | Intervention: −3.3% Control: −0.3% | Intervention: 21.88 ± 1.59 Control: 22.34 ± 1.88 | -- | Nausea, dysphoria, pulmonary infection, hypoglycemia, hunger, irritability | Not available |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheung, K.; Chan, V.; Chan, S.; Wong, M.M.H.; Chung, G.K.-K.; Cheng, W.-Y.; Lo, K.; Zeng, F. Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2024, 16, 357. https://doi.org/10.3390/nu16030357
Cheung K, Chan V, Chan S, Wong MMH, Chung GK-K, Cheng W-Y, Lo K, Zeng F. Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials. Nutrients. 2024; 16(3):357. https://doi.org/10.3390/nu16030357
Chicago/Turabian StyleCheung, Katy, Vicky Chan, Stephanie Chan, Martin Ming Him Wong, Gary Ka-Ki Chung, Wai-Yin Cheng, Kenneth Lo, and Fangfang Zeng. 2024. "Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials" Nutrients 16, no. 3: 357. https://doi.org/10.3390/nu16030357
APA StyleCheung, K., Chan, V., Chan, S., Wong, M. M. H., Chung, G. K.-K., Cheng, W.-Y., Lo, K., & Zeng, F. (2024). Effect of Intermittent Fasting on Cardiometabolic Health in the Chinese Population: A Meta-Analysis of Randomized Controlled Trials. Nutrients, 16(3), 357. https://doi.org/10.3390/nu16030357