Patterns of Dietary Supplement Use during the COVID-19 Pandemic in Poland: Focus on Vitamin D and Magnesium
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Ethical Approval
2.3. Study Questionnaire
2.4. Statistical Analysis
3. Results
3.1. Population Characteristics
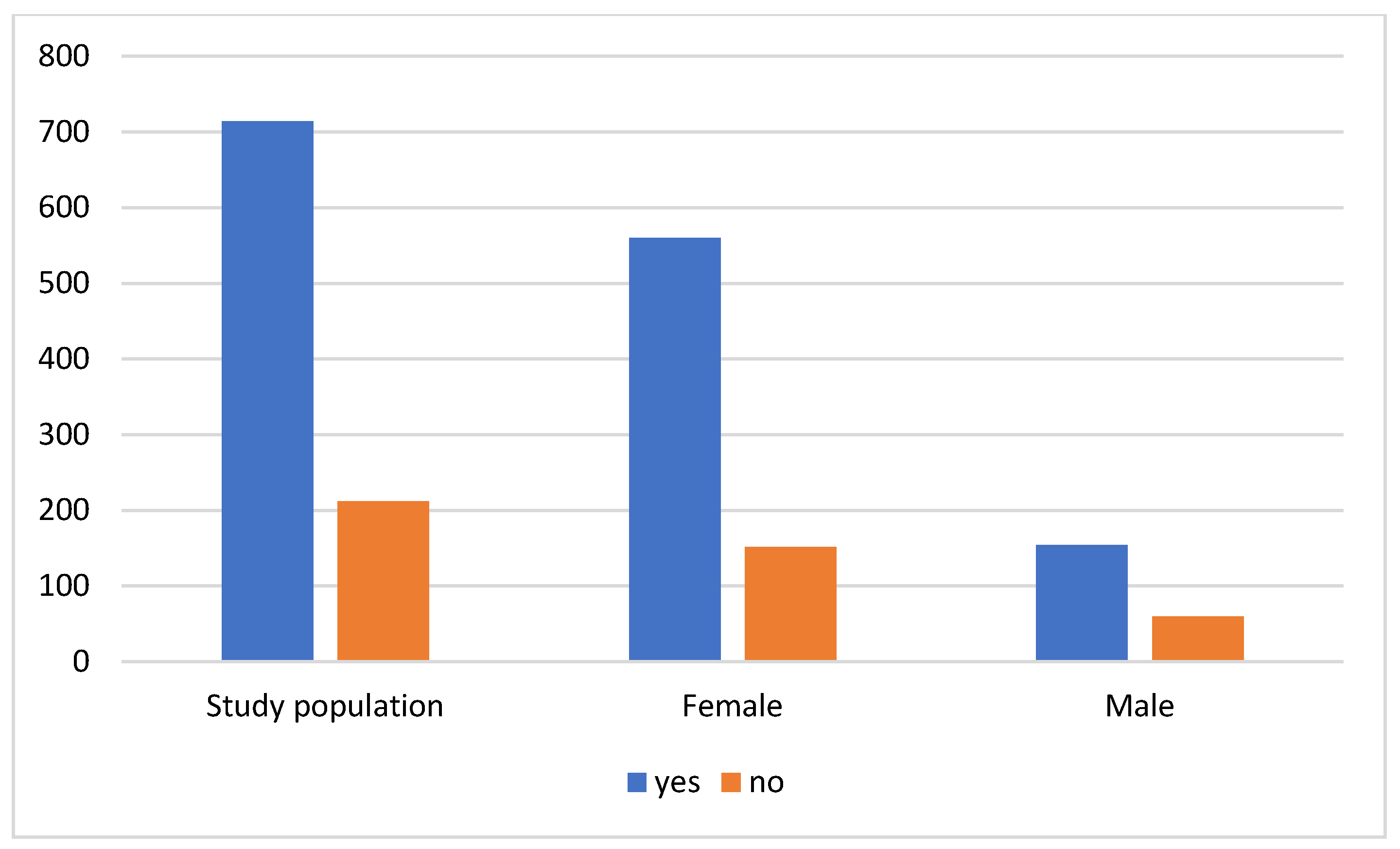
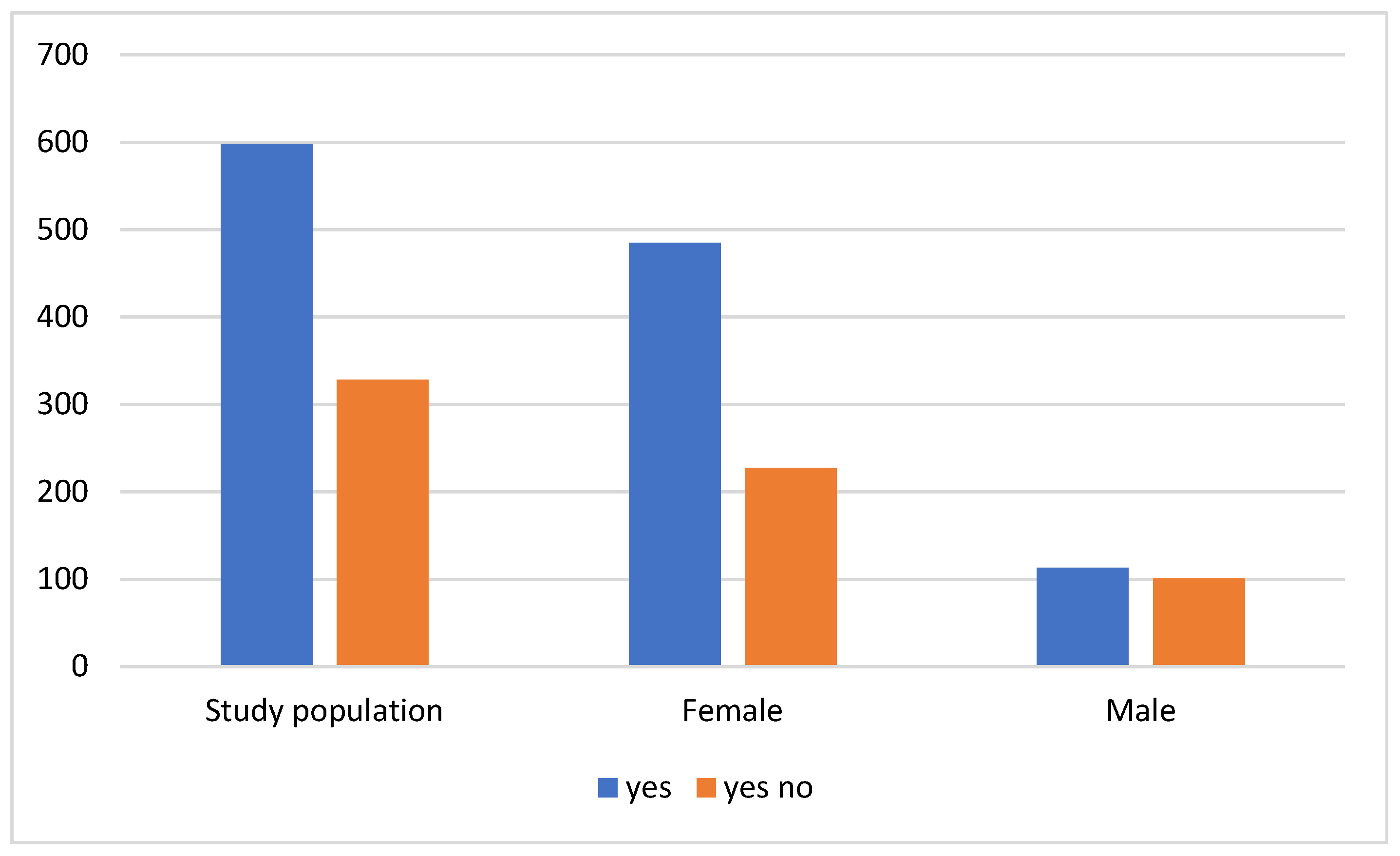
3.2. Taking Dietary Supplements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jęśkowiak, I.; Wiatrak, B.; Grosman-Dziewiszek, P.; Szeląg, A. The Incidence and Severity of Post-Vaccination Reactions after Vaccination against COVID-19. Vaccines 2021, 9, 502. [Google Scholar] [CrossRef] [PubMed]
- Tsang, H.F.; Chan, L.W.C.; Cho, W.C.S.; Yu, A.C.S.; Yim, A.K.Y.; Chan, A.K.C.; Ng, L.P.W.; Wong, Y.K.E.; Pei, X.M.; Li, M.J.W.; et al. An update on COVID-19 pandemic: The epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev. Anti-Infect. Ther. 2021, 19, 877–888. [Google Scholar] [CrossRef]
- Grosman-Dziewiszek, P.; Wiatrak, B.; Jęśkowiak, I.; Szeląg, A. Patients’ Habits and the Role of Pharmacists and Telemedicine as Elements of a Modern Health Care System during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 4211. [Google Scholar] [CrossRef]
- Kilis-Pstrusinska, K.; Akutko, K.; Braksator, J.; Dancewicz, A.; Grosman-Dziewiszek, P.; Jamer, T.; Juszczyńska, K.; Konikowska, K.; Koruba, M.; Pupek, M.; et al. Kidney Dysfunction and Its Progression in Patients Hospitalized Duo to COVID-19: Contribution to the Clinical Course and Outcomes. J. Clin. Med. 2021, 10, 5522. [Google Scholar] [CrossRef]
- Fitero, A.; Bungau, S.G.; Tit, D.M.; Endres, L.; Khan, S.A.; Bungau, A.F.; Romanul, I.; Vesa, C.M.; Radu, A.F.; Tarce, A.G.; et al. Comorbidities, Associated Diseases, and Risk Assessment in COVID-19-A Systematic Review. Int. J. Clin. Pract. 2022, 2022, 1571826. [Google Scholar] [CrossRef]
- Szkudlarek, D.; Gębarowski, T.; Hauzer, N.; Wiatrak, B. The Concept of Health Debt Incurred during the COVID-19 Pandemic on the Example of Basal Cell Skin Cancer Diagnosis in Lower Silesia. J. Clin. Med. 2024, 13, 4923. [Google Scholar] [CrossRef]
- Staszuk, A.; Wiatrak, B.; Tadeusiewicz, R.; Karuga-Kuźniewska, E.; Rybak, Z. Telerehabilitation approach for patients with hand impairment. Acta Bioeng. Biomech. 2016, 18, 55–62. [Google Scholar] [PubMed]
- Griffin, G.; Hewison, M.; Hopkin, J.; Kenny, R.; Quinton, R.; Rhodes, J.; Subramanian, S.; Thickett, D. Vitamin D and COVID-19: Evidence and recommendations for supplementation. R. Soc. Open Sci. 2020, 7, 201912. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 2011, 14, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Soininen, S.; Eloranta, A.M.; Schwab, U.; Lakka, T.A. Sources of vitamin D and determinants of serum 25-hydroxyvitamin D in Finnish adolescents. Eur. J. Nutr. 2023, 62, 1011–1025. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ikonen, H.; Lumme, J.; Seppälä, J.; Pesonen, P.; Piltonen, T.; Järvelin, M.R.; Herzig, K.H.; Miettunen, J.; Niinimäki, M.; Palaniswamy, S.; et al. The determinants and longitudinal changes in vitamin D status in middle-age: A Northern Finland Birth Cohort 1966 study. Eur. J. Nutr. 2021, 60, 4541–4553. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manoy, P.; Yuktanandana, P.; Tanavalee, A.; Anomasiri, W.; Ngarmukos, S.; Tanpowpong, T.; Honsawek, S. Vitamin D Supplementation Improves Quality of Life and Physical Performance in Osteoarthritis Patients. Nutrients 2017, 9, 799. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Cock, H.R.; Brex, P.; Giovannoni, G. Vitamin D supplementation. Pract. Neurol. 2018, 18, 35–42. [Google Scholar] [CrossRef]
- Muñoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Martineau, A.R.; Jolliffe, D.A.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; Goodall, E.C.; et al. Vitamin D supplementation to prevent acute respiratory infections: Individual participant data meta-analysis. Health Technol. Assess. 2019, 23, 1–44. [Google Scholar] [CrossRef]
- Weydert, J.A. Vitamin D in Children’s Health. Children 2014, 1, 208–226. [Google Scholar] [CrossRef]
- Chang, S.W.; Lee, H.C. Vitamin D and health—The missing vitamin in humans. Pediatr. Neonatol. 2019, 60, 237–244. [Google Scholar] [CrossRef]
- Eyles, D.W.; Burne, T.H.; McGrath, J.J. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front. Neuroendocrinol. 2013, 34, 47–64. [Google Scholar] [CrossRef]
- Del Pozo de la Calle, S.; Alonso Ledesma, I.; Nuñez, O.; Castelló Pastor, A.; Lope Carvajal, V.; Fernández de Larrea Baz, N.; Pérez-Gómez, B.; Pollán, M.; Ruiz Moreno, E. Composition and Nutritional Quality of the Diet in Spanish Households during the First Wave of the COVID-19 Pandemic. Nutrients 2021, 13, 1443. [Google Scholar] [CrossRef]
- Kočovská, E.; Gaughran, F.; Krivoy, A.; Meier, U.C. Vitamin-D Deficiency As a Potential Environmental Risk Factor in Multiple Sclerosis, Schizophrenia, and Autism. Front. Psychiatry 2017, 8, 47. [Google Scholar] [CrossRef]
- Sailike, B.; Onzhanova, Z.; Akbay, B.; Tokay, T.; Molnár, F. Vitamin D in Central Nervous System: Implications for Neurological Disorders. Int. J. Mol. Sci. 2024, 25, 7809. [Google Scholar] [CrossRef] [PubMed]
- Wassif, G.A.; Alrehely, M.S.; Alharbi, D.M.; Aljohani, A.A. The Impact of Vitamin D on Neuropsychiatric Disorders. Cureus 2023, 15, e47716. [Google Scholar] [CrossRef] [PubMed]
- Ohaegbulam, K.C.; Swalih, M.; Patel, P.; Smith, M.A.; Perrin, R. Vitamin D Supplementation in COVID-19 Patients: A Clinical Case Series. Am. J. Ther. 2020, 27, e485–e490. [Google Scholar] [CrossRef]
- Bouillon, R.; Manousaki, D.; Rosen, C.; Trajanoska, K.; Rivadeneira, F.; Richards, J.B. The health effects of vitamin D supplementation: Evidence from human studies. Nature reviews. Endocrinology 2022, 18, 96–110. [Google Scholar] [CrossRef]
- Benskin, L.L. A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency. Front. Public Health 2020, 8, 513. [Google Scholar] [CrossRef]
- Vyas, N.; Kurian, S.J.; Bagchi, D.; Manu, M.K.; Saravu, K.; Unnikrishnan, M.K.; Mukhopadhyay, C.; Rao, M.; Miraj, S.S. Vitamin D in Prevention and Treatment of COVID-19: Current Perspective and Future Prospects. J. Am. Coll. Nutr. 2021, 40, 632–645. [Google Scholar] [CrossRef]
- Žmitek, K.; Hribar, M.; Lavriša, Ž.; Hristov, H.; Kušar, A.; Pravst, I. Socio-Demographic and Knowledge-Related Determinants of Vitamin D Supplementation in the Context of the COVID-19 Pandemic: Assessment of an Educational Intervention. Front. Nutr. 2021, 8, 648450. [Google Scholar] [CrossRef]
- Tekin, C.S.; Kılıç, Z. Impact of COVID-19 pandemic on health-promoting lifestyle behaviors: A cross-sectional study. J. Acute Dis. 2023, 12, 10–17. [Google Scholar] [CrossRef]
- Khalesi, S.; Vandelanotte, C.; Thwaite, T.; Russell, A.M.T.; Dawson, D.; Williams, S.L. Awareness and Attitudes of Gut Health, Probiotics and Prebiotics in Australian Adults. J. Diet. Suppl. 2021, 18, 418–432. [Google Scholar] [CrossRef] [PubMed]
- Poluektova, V.B.; Sankova, M.V.; Volchkova, E.V.; Larina, S.N.; Maloletneva, N.V.; Shabalina, O.Y.; Lisova, P.A.; Rochlina, D.A.; Darvina, O.V. The possibility of predicting the COVID-19 severity by clinical-laboratory criteria taking into account the SARS-CoV-2 strain: An analytical review. Epidemiol. Infect. Dis. 2024, 29, 192–203. [Google Scholar] [CrossRef]
- Durden, W.; Ezaldin, S.; Amos, J.; Kemper, S.; Campbell, J. Rise in Serum 25-Hydroxyvitamin D Levels during the COVID-19 Pandemic. Nutrients 2024, 16, 2449. [Google Scholar] [CrossRef] [PubMed]
- Nekoukar, Z.; Manouchehri, A.; Zakariaei, Z. Accidental vitamin D3 overdose in a young man. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. J. Int. Vitaminol. Nutr. 2024, 94, 82–85. [Google Scholar] [CrossRef]
- Alshahrani, F.; Aljohani, N. Vitamin D: Deficiency, sufficiency and toxicity. Nutrients 2013, 5, 3605–3616. [Google Scholar] [CrossRef]
- Galior, K.; Grebe, S.; Singh, R. Development of Vitamin D Toxicity from Overcorrection of Vitamin D Deficiency: A Review of Case Reports. Nutrients 2018, 10, 953. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D supplementation guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef]
- Mercola, J.; Grant, W.B.; Wagner, C.L. Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients 2020, 12, 3361. [Google Scholar] [CrossRef] [PubMed]
- Govender, N.; Khaliq, O.P.; Moodley, J.; Naicker, T. Insulin resistance in COVID-19 and diabetes. Prim. Care Diabetes 2021, 15, 629–634. [Google Scholar] [CrossRef]
- Wang, P.; Song, M.; Eliassen, A.H.; Wang, M.; Fung, T.T.; Clinton, S.K.; Rimm, E.B.; Hu, F.B.; Willett, W.C.; Tabung, F.K.; et al. Optimal dietary patterns for prevention of chronic disease. Nat. Med. 2023, 29, 719–728. [Google Scholar] [CrossRef]
- Xiang, Q.; Xu, H.; Zhan, J.; Lu, S.; Li, S.; Wang, Y.; Wang, Y.; He, J.; Ni, Y.; Li, L.; et al. Association between the Triglyceride-Glucose Index and Vitamin D Status in Type 2 Diabetes Mellitus. Nutrients 2023, 15, 639. [Google Scholar] [CrossRef]
- Trapani, V.; Rosanoff, A.; Baniasadi, S.; Barbagallo, M.; Castiglioni, S.; Guerrero-Romero, F.; Iotti, S.; Mazur, A.; Micke, O.; Pourdowlat, G.; et al. The relevance of magnesium homeostasis in COVID-19. Eur. J. Nutr. 2022, 61, 625–636. [Google Scholar] [CrossRef]
- Dai, Q.; Zhu, X.; Manson, J.E.; Song, Y.; Li, X.; Franke, A.A.; Costello, R.B.; Rosanoff, A.; Nian, H.; Fan, L.; et al. Magnesium status and supplementation influence vitamin D status and metabolism: Results from a randomized trial. Am. J. Clin. Nutr. 2018, 108, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- Nasser, R.; Naffaa, M.E.; Mashiach, T.; Azzam, Z.S.; Braun, E. The association between serum magnesium levels and community-acquired pneumonia 30-day mortality. BMC Infect. Dis. 2018, 18, 698. [Google Scholar] [CrossRef] [PubMed]
- Chinni, V.; El-Khoury, J.; Perera, M.; Bellomo, R.; Jones, D.; Bolton, D.; Ischia, J.; Patel, O. Zinc supplementation as an adjunct therapy for COVID-19: Challenges and opportunities. Br. J. Clin. Pharmacol. 2021, 87, 3737–3746. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Patel, D.; Bittel, B.; Wolski, K.; Wang, Q.; Kumar, A.; Il’Giovine, Z.J.; Mehra, R.; McWilliams, C.; Nissen, S.E.; et al. Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs. Usual Care on Symptom Length and Reduction among Ambulatory Patients with SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e210369. [Google Scholar] [CrossRef]
- Read, S.A.; Obeid, S.; Ahlenstiel, C.; Ahlenstiel, G. The Role of Zinc in Antiviral Immunity. Adv. Nutr. 2019, 10, 696–710. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Kubota, Y.; Chernov, M.; Kasuya, H. Potential role of zinc supplementation in prophylaxis and treatment of COVID-19. Med. Hypotheses 2020, 144, 109848. [Google Scholar] [CrossRef]
- James, P.T.; Ali, Z.; Armitage, A.E.; Bonell, A.; Cerami, C.; Drakesmith, H.; Jobe, M.; Jones, K.S.; Liew, Z.; Moore, S.E.; et al. The Role of Nutrition in COVID-19 Susceptibility and Severity of Disease: A Systematic Review. J. Nutr. 2021, 151, 1854–1878. [Google Scholar] [CrossRef] [PubMed]
- Galmés, S.; Serra, F.; Palou, A. Current State of Evidence: Influence of Nutritional and Nutrigenetic Factors on Immunity in the COVID-19 Pandemic Framework. Nutrients 2020, 12, 2738. [Google Scholar] [CrossRef]
- Habib, H.M.; Ibrahim, S.; Zaim, A.; Ibrahim, W.H. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed. Pharmacother. Biomed. Pharmacother. 2021, 136, 111228. [Google Scholar] [CrossRef]
- Taneri, P.E.; Gómez-Ochoa, S.A.; Llanaj, E.; Raguindin, P.F.; Rojas, L.Z.; Roa-Díaz, Z.M.; Salvador, D.; Groothof, D., Jr.; Minder, B.; Kopp-Heim, D.; et al. Anemia and iron metabolism in COVID-19: A systematic review and meta-analysis. Eur. J. Epidemiol. 2020, 35, 763–773. [Google Scholar] [CrossRef]
- Venturi, S.; Venturi, M. Iodine in evolution of salivary glands and in oral health. Nutr. Health 2009, 20, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Delange, F.; Bürgi, H. Iodine deficiency disorders in Europe. Bull. World Health Organ. 1989, 67, 317–325. [Google Scholar]
- Winder, M.; Kosztyła, Z.; Boral, A.; Kocełak, P.; Chudek, J. The Impact of Iodine Concentration Disorders on Health and Cancer. Nutrients 2022, 14, 2209. [Google Scholar] [CrossRef]
- Nawaz, M.; Ashraf, M.A.; Ali, M.A.; Shabbir, M.Z.; Shabbir, M.A.B.; Altaf, I.; Raza, S.; Rafique, S.; Hassan, S.; Sardar, N.; et al. Renessans Helps in Early Clearance of SARS-CoV-2: In-Vivo Activity of the Iodine Complex in Rhesus macaque. Life 2022, 12, 1424. [Google Scholar] [CrossRef]
- Ashraf, S.; Ashraf, S.; Ashraf, M.; Imran, M.A.; Kalsoom, L.; Siddiqui, U.N.; Farooq, I.; Ghufran, M.; Khokhar, R.A.; Akram, M.K.; et al. A quadruple blinded placebo controlled randomised trial to evaluate the effectiveness of an Iodine complex for patients with mild to moderate COVID-19 in Pakistan (I-COVID-PK): A structured summary of a study protocol for a randomised controlled trial. Trials 2021, 22, 127. [Google Scholar] [CrossRef]
- Djuricic, I.; Calder, P.C. Beneficial Outcomes of Omega-6 and Omega-3 Polyunsaturated Fatty Acids on Human Health: An Update for 2021. Nutrients 2021, 13, 2421. [Google Scholar] [CrossRef]
- Brunvoll, S.H.; Nygaard, A.B.; Ellingjord-Dale, M.; Holland, P.; Istre, M.S.; Kalleberg, K.T.; Søraas, C.L.; Holven, K.B.; Ulven, S.M.; Hjartåker, A.; et al. Prevention of covid-19 and other acute respiratory infections with cod liver oil supplementation, a low dose vitamin D supplement: Quadruple blinded, randomised placebo controlled trial. BMJ 2022, 378, e071245. [Google Scholar] [CrossRef]
- Fan, Y.; Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2021, 19, 55–71. [Google Scholar] [CrossRef]
- Bistrian, B.R. Parenteral Fish-Oil Emulsions in Critically Ill COVID-19 Emulsions. J. Parenter. Enter. Nutr. 2020, 44, 1168. [Google Scholar] [CrossRef]
- Bochenek, T.; Godman, B.; Lipowska, K.; Mikrut, K.; Zuziak, S.; Pedzisz, M.; Nowak, A.; Pilc, A. Over-the-counter medicine and dietary supplement consumption among academic youth in Poland. Expert Rev. Pharmacoeconomics Outcomes Res. 2016, 16, 199–205. [Google Scholar] [CrossRef]
- Wróbel, K.; Zastawna, B.; Milewska, A.J.; Marczak, M.; Kozłowski, R. Comparison between the American and the European Systems of Monitoring Adverse Effects of Dietary Supplements and Their Usefulness on the Polish Market. Int. J. Environ. Res. Public Health 2023, 20, 902. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Number of Participants [n] | Percent [%] |
|---|---|---|
| Gender | ||
| Female | 712 | 76.9 |
| Male | 214 | 23.1 |
| Education | ||
| Higher education | 552 | 59.6 |
| Student | 201 | 21.7 |
| Secondary education | 151 | 16.3 |
| Primary education | 6 | 0.6 |
| Vocation | 16 | 1.7 |
| Age groups | ||
| 18–30 | 398 | 43.0 |
| 31–40 | 185 | 20.0 |
| 41–50 | 136 | 14.7 |
| 51–60 | 97 | 10.5 |
| 61–70 | 87 | 9.4 |
| 71–80 | 15 | 1.6 |
| >80 | 8 | 0.9 |
| Gender [n] | ||
| Age groups | Female | Male |
| 18–30 | 314 | 84 |
| 31–40 | 145 | 40 |
| 41–50 | 105 | 31 |
| 51–60 | 73 | 24 |
| 61–70 | 61 | 26 |
| 71–80 | 7 | 8 |
| >80 | 7 | 1 |
| Supplements | Takes (YES) | Takes (NO) | p |
|---|---|---|---|
| Vitamin D | 598 | 328 | <0.001 |
| Vitamin C | 257 | 669 | 0.55 |
| Omega-3 | 158 | 768 | 0.35 |
| Multivitamin preparations | 132 | 795 | 0.54 |
| Magnesium | 623 | 303 | 0.02 |
| Zinc | 115 | 811 | 0.56 |
| Iron | 10 | 916 | 0.32 |
| Vitamin B | 28 | 898 | 0.26 |
| Iodine | 2 | 924 | 0.43 |
| Folic acid | 10 | 916 | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grosman-Dziewiszek, P.; Jęśkowiak-Kossakowska, I.; Szeląg, A.; Wiatrak, B. Patterns of Dietary Supplement Use during the COVID-19 Pandemic in Poland: Focus on Vitamin D and Magnesium. Nutrients 2024, 16, 3225. https://doi.org/10.3390/nu16193225
Grosman-Dziewiszek P, Jęśkowiak-Kossakowska I, Szeląg A, Wiatrak B. Patterns of Dietary Supplement Use during the COVID-19 Pandemic in Poland: Focus on Vitamin D and Magnesium. Nutrients. 2024; 16(19):3225. https://doi.org/10.3390/nu16193225
Chicago/Turabian StyleGrosman-Dziewiszek, Patrycja, Izabela Jęśkowiak-Kossakowska, Adam Szeląg, and Benita Wiatrak. 2024. "Patterns of Dietary Supplement Use during the COVID-19 Pandemic in Poland: Focus on Vitamin D and Magnesium" Nutrients 16, no. 19: 3225. https://doi.org/10.3390/nu16193225
APA StyleGrosman-Dziewiszek, P., Jęśkowiak-Kossakowska, I., Szeląg, A., & Wiatrak, B. (2024). Patterns of Dietary Supplement Use during the COVID-19 Pandemic in Poland: Focus on Vitamin D and Magnesium. Nutrients, 16(19), 3225. https://doi.org/10.3390/nu16193225







