Calcium- and Sodium-Rich Food Intake among Koreans with and without Metabolic Syndrome: Cross-Sectional Analysis of the Korean Genome and Epidemiology Study
Abstract
1. Introduction
2. Materials and Methods
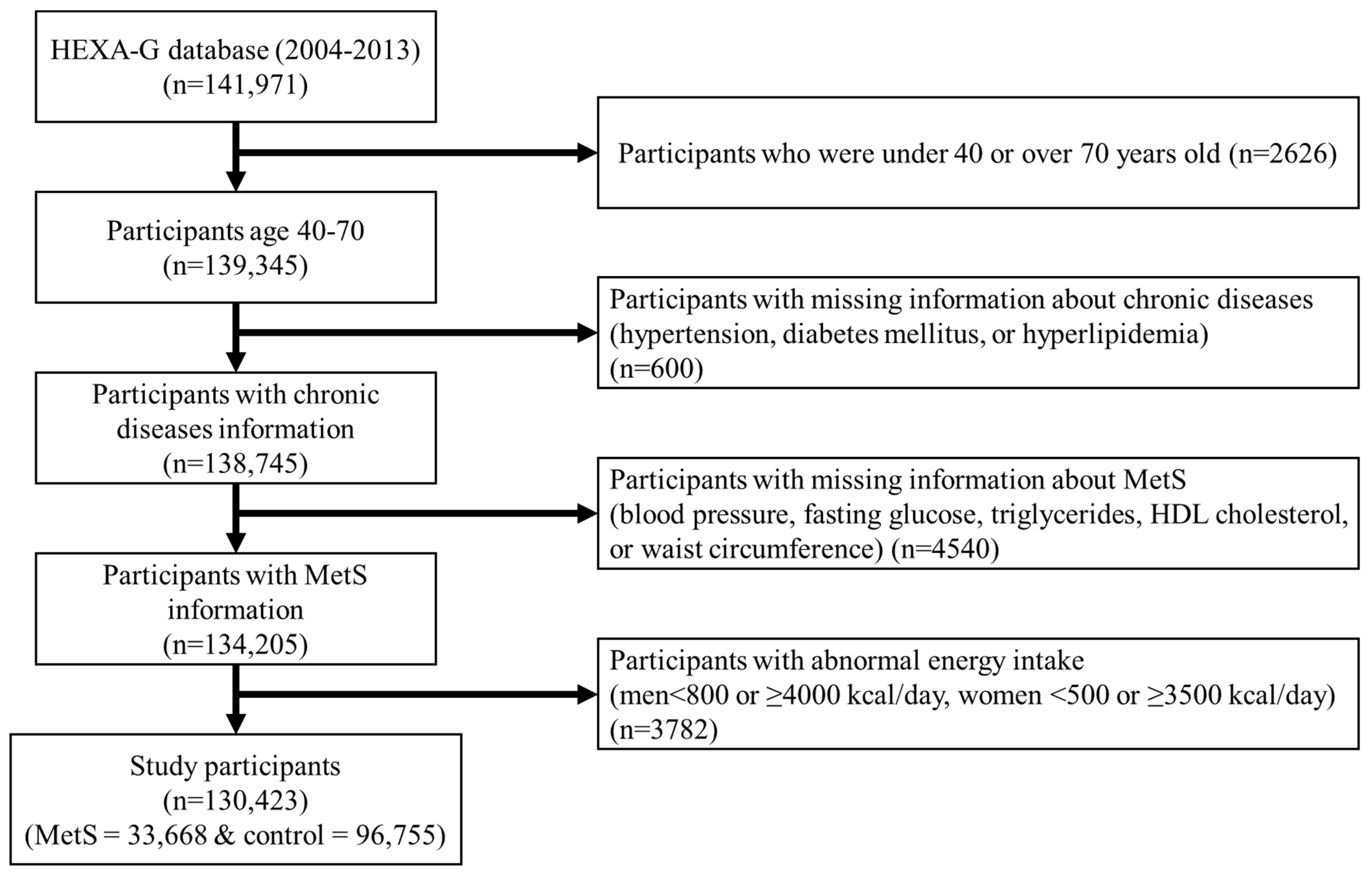
2.1. Study Population
2.2. Dietary Consumption Assessment
2.3. Definition of Metabolic Syndrome
2.4. Covariation Variables
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grundy, S.M.; Brewer, H.B., Jr.; Cleeman, J.I.; Smith, S.C., Jr.; Lenfant, C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004, 109, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Noubiap, J.J.; Nansseu, J.R.; Lontchi-Yimagou, E.; Nkeck, J.R.; Nyaga, U.F.; Ngouo, A.T.; Tounouga, D.N.; Tianyi, F.L.; Foka, A.J.; Ndoadoumgue, A.L.; et al. Geographic distribution of metabolic syndrome and its components in the general adult population: A meta-analysis of global data from 28 million individuals. Diabetes Res. Clin. Pract. 2022, 188, 109924. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Kang, D.R.; Kim, J.Y.; Koh, K.K. Metabolic Syndrome Fact Sheet 2021: Executive Report. Cardiometab. Syndr. J. 2021, 1, 125–134. [Google Scholar] [CrossRef]
- Arruda, A.P.; Hotamisligil, G.S. Calcium Homeostasis and Organelle Function in the Pathogenesis of Obesity and Diabetes. Cell Metab. 2015, 22, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; He, J. Health effects of sodium and potassium in humans. Curr. Opin. Lipidol. 2014, 25, 75–79. [Google Scholar] [CrossRef]
- Zemel, M.B.; Shi, H.; Greer, B.; Dirienzo, D.; Zemel, P.C. Regulation of adiposity by dietary calcium. FASEB J. 2000, 14, 1132–1138. [Google Scholar] [CrossRef]
- van Meijl, L.E.; Vrolix, R.; Mensink, R.P. Dairy product consumption and the metabolic syndrome. Nutr. Res. Rev. 2008, 21, 148–157. [Google Scholar] [CrossRef]
- Chen, J.; Gu, D.; Huang, J.; Rao, D.C.; Jaquish, C.E.; Hixson, J.E.; Chen, C.S.; Chen, J.; Lu, F.; Hu, D.; et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: A dietary intervention study. Lancet 2009, 373, 829–835. [Google Scholar] [CrossRef]
- Oberleithner, H.; Riethmuller, C.; Schillers, H.; MacGregor, G.A.; de Wardener, H.E.; Hausberg, M. Plasma sodium stiffens vascular endothelium and reduces nitric oxide release. Proc. Natl. Acad. Sci. USA 2007, 104, 16281–16286. [Google Scholar] [CrossRef]
- Shin, S.K.; Kim, M.K.; Lee, Y.H.; Shin, D.H.; Shin, M.H.; Chun, B.Y.; Choi, B.Y. The cross-sectional relationship between dietary calcium intake and metabolic syndrome among men and women aged 40 or older in rural areas of Korea. Nutr. Res. Pract. 2015, 9, 328–335. [Google Scholar] [CrossRef]
- Bruscato, N.M.; da Costa Vieira, J.L.; do Nascimento, N.M.R.; Canto, M.E.P.; Stobbe, J.C.; Gottlieb, M.G.; Wagner, M.B.; Dalacorte, R.R. Dietary intake is not associated to the metabolic syndrome in elderly women. N. Am. J. Med. Sci. 2010, 2, 182–188. [Google Scholar] [PubMed]
- Chen, G.C.; Szeto, I.M.; Chen, L.H.; Han, S.F.; Li, Y.J.; van Hekezen, R.; Qin, L.Q. Dairy products consumption and metabolic syndrome in adults: Systematic review and meta-analysis of observational studies. Sci. Rep. 2015, 5, 14606. [Google Scholar] [CrossRef]
- Balk, E.; Adam, G.; Langberg, V.; Earley, A.; Clark, P.; Ebeling, P.; Mithal, A.; Rizzoli, R.; Zerbini, C.; Pierroz, D. Global dietary calcium intake among adults: A systematic review. Osteoporos. Int. 2017, 28, 3315–3324. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R., 3rd; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Li, J.; Macgregor, G.A. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013, 346, f1325. [Google Scholar] [CrossRef]
- Park, H.R.; Jeong, G.O.; Lee, S.L.; Kim, J.Y.; Kang, S.A.; Park, K.Y.; Ryou, H.J. Workers intake too much salt from dishes of eating out and food service cafeterias; direct chemical analysis of sodium content. Nutr. Res. Pract. 2009, 3, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Powles, J.; Fahimi, S.; Micha, R.; Khatibzadeh, S.; Shi, P.; Ezzati, M.; Engell, R.E.; Lim, S.S.; Danaei, G.; Mozaffarian, D.; et al. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013, 3, e003733. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.D.; Shin, A.; Kim, J. Dietary patterns of Korean adults and the prevalence of metabolic syndrome: A cross-sectional study. PLoS ONE 2014, 9, e111593. [Google Scholar] [CrossRef]
- Song, Y.; Joung, H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 456–462. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, Y.M.; Shin, M.H.; Koh, S.B.; Chang Kim, H.; Kim, M.K. Empirically identified dietary patterns and metabolic syndrome risk in a prospective cohort study: The Cardiovascular Disease Association Study. Clin. Nutr. 2022, 41, 2156–2162. [Google Scholar] [CrossRef]
- Rhee, M.Y.; Kim, J.H.; Kim, Y.S.; Chung, J.W.; Bae, J.H.; Nah, D.Y.; Kim, Y.K.; Lee, M.M.; Lim, C.Y.; Byun, J.E.; et al. High sodium intake in women with metabolic syndrome. Korean Circ. J. 2014, 44, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.Y.; Kim, M.K.; Lee, M.; Kim, Y.O. Macronutrient composition and sodium intake of diet are associated with risk of metabolic syndrome and hypertension in Korean women. PLoS ONE 2013, 8, e78088. [Google Scholar] [CrossRef] [PubMed]
- Noh, H.-M.; Park, S.-Y.; Lee, H.-S.; Oh, H.-Y.; Paek, Y.J.; Song, H.J.; Park, K.H. Association between high blood pressure and intakes of sodium and potassium among Korean adults: Korean National Health and Nutrition Examination Survey, 2007–2012. J. Acad. Nutr. Diet. 2015, 115, 1950–1957. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.W.; Lim, Y.-H.; Kim, M.K.; Shin, J.; Lee, Y.-H.; Shin, D.H.; Shin, M.-H.; Choi, B.Y. Prospective associations between total, animal, and vegetable calcium intake and metabolic syndrome in adults aged 40 years and older. Clin. Nutr. 2020, 39, 2282–2291. [Google Scholar] [CrossRef] [PubMed]
- Cho, G.J.; Park, H.T.; Shin, J.H.; Hur, J.Y.; Kim, Y.T.; Kim, S.H.; Lee, K.W.; Kim, T. Calcium intake is inversely associated with metabolic syndrome in postmenopausal women: Korea National Health and Nutrition Survey, 2001 and 2005. Menopause 2009, 16, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Health Examinees Study, G. The Health Examinees (HEXA) study: Rationale, study design and baseline characteristics. Asian Pac. J. Cancer Prev. 2015, 16, 1591–1597. [Google Scholar] [CrossRef]
- Kim, Y.; Han, B.G.; Ko, G.E.S.g. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, 1350. [Google Scholar] [CrossRef]
- Ahn, Y.; Lee, J.E.; Paik, H.Y.; Lee, H.K.; Jo, I.; Kimm, K. Development of a semi-quantitative food frequency questionnaire based on dietary data from the Korea National Health and Nutrition Examination Survey. Nutr. Sci. 2003, 6, 173–184. [Google Scholar]
- Ahn, Y.; Lee, J.-E.; Cho, N.-H.; Shin, C.; Park, C.; Oh, B.-S.; Kimm, K. Validation and calibration of semi-quantitative food frequency questionnaire: With participants of the Korean Health and Genome Study. Korean J. Community Nutr. 2004, 9, 173–182. [Google Scholar]
- Ahn, Y.; Kwon, E.; Shim, J.E.; Park, M.K.; Joo, Y.; Kimm, K.; Park, C.; Kim, D.H. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007, 61, 1435–1441. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (US); Expert Panel on Detection, and Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef]
- Han, Y.; Kwon, S.O.; Lee, S.A. Distribution and Exposure Prevalence of Carbohydrate-based Food Intake among Obese Korean Adults Based on the Health Examinees (HEXA) Study. Korean J. Community Nutr. 2017, 22, 159–170. [Google Scholar] [CrossRef]
- Han, D.; Fang, X.; Su, D.; Huang, L.; He, M.; Zhao, D.; Zou, Y.; Zhang, R. Dietary Calcium Intake and the Risk of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Sci. Rep. 2019, 9, 19046. [Google Scholar] [CrossRef] [PubMed]
- Reid, I.R.; Mason, B.; Horne, A.; Ames, R.; Clearwater, J.; Bava, U.; Orr-Walker, B.; Wu, F.; Evans, M.C.; Gamble, G.D. Effects of calcium supplementation on serum lipid concentrations in normal older women: A randomized controlled trial. Am. J. Med. 2002, 112, 343–347. [Google Scholar] [CrossRef]
- Shin, H.; Yoon, Y.S.; Lee, Y.; Kim, C.I.; Oh, S.W. Dairy product intake is inversely associated with metabolic syndrome in Korean adults: Anseong and Ansan cohort of the Korean Genome and Epidemiology Study. J. Korean Med. Sci. 2013, 28, 1482–1488. [Google Scholar] [CrossRef]
- Kim, D.; Kim, J. Dairy consumption is associated with a lower incidence of the metabolic syndrome in middle-aged and older Korean adults: The Korean Genome and Epidemiology Study (KoGES). Br. J. Nutr. 2017, 117, 148–160. [Google Scholar] [CrossRef]
- Zemel, M.B.; Thompson, W.; Milstead, A.; Morris, K.; Campbell, P. Calcium and dairy acceleration of weight and fat loss during energy restriction in obese adults. Obes. Res. 2004, 12, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Dennis, E.J.; Kang, M.; Han, S.N. Relation between Beverage Consumption Pattern and Metabolic Syndrome among Healthy Korean Adults. Korean J. Community Nutr. 2017, 22, 441–455. [Google Scholar] [CrossRef]
- Woo, H.W.; Kim, M.K.; Lee, Y.H.; Shin, D.H.; Shin, M.H.; Choi, B.Y. Habitual consumption of soy protein and isoflavones and risk of metabolic syndrome in adults ≥ 40 years old: A prospective analysis of the Korean Multi-Rural Communities Cohort Study (MRCohort). Eur. J. Nutr. 2019, 58, 2835–2850. [Google Scholar] [CrossRef]
- Marventano, S.; Salomone, F.; Godos, J.; Pluchinotta, F.; Del Rio, D.; Mistretta, A.; Grosso, G. Coffee and tea consumption in relation with non-alcoholic fatty liver and metabolic syndrome: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2016, 35, 1269–1281. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Cho, S.; Jacobs, D.R., Jr.; Park, K. Instant coffee consumption may be associated with higher risk of metabolic syndrome in Korean adults. Diabetes Res. Clin. Pract. 2014, 106, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Ding, J.; Zhang, Y. Relationship between Egg Consumption and Metabolic Syndrome. A Meta-Analysis of Observational Studies. J. Nutr. Health Aging 2022, 26, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Mennen, L.I.; Lafay, L.; Feskens, E.J.; Novak, M.; Lépinay, P.; Balkau, B. Possible protective effect of bread and dairy products on the risk of the metabolic syndrome. Nutr. Res. 2000, 20, 335–347. [Google Scholar] [CrossRef]
- Weaver, C.M.; Heaney, R.P.; Martin, B.R.; Fitzsimmons, M.L. Human calcium absorption from whole-wheat products. J. Nutr. 1991, 121, 1769–1775. [Google Scholar] [CrossRef]
- Park, S.; Kim, K.; Lee, B.-K.; Ahn, J. A healthy diet rich in calcium and vitamin C is inversely associated with metabolic syndrome risk in Korean adults from the KNHANES 2013–2017. Nutrients 2021, 13, 1312. [Google Scholar] [CrossRef] [PubMed]
- Soltani, S.; Kolahdouz Mohammadi, R.; Shab-Bidar, S.; Vafa, M.; Salehi-Abargouei, A. Sodium status and the metabolic syndrome: A systematic review and meta-analysis of observational studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 196–206. [Google Scholar] [CrossRef]
- Won, J.C.; Hong, J.W.; Noh, J.H.; Kim, D.-J. Association between estimated 24-h urinary sodium excretion and metabolic syndrome in Korean adults: The 2009 to 2011 Korea National Health and Nutrition Examination Survey. Medicine 2016, 95, e3153. [Google Scholar] [CrossRef]
- Baudrand, R.; Campino, C.; Carvajal, C.; Olivieri, O.; Guidi, G.; Faccini, G.; Vöhringer, P.; Cerda, J.; Owen, G.; Kalergis, A. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin. Endocrinol. 2014, 80, 677–684. [Google Scholar] [CrossRef]
- Charles, P. Calcium absorption and calcium bioavailability. J. Intern. Med. 1992, 231, 161–168. [Google Scholar] [CrossRef]
- Jurek, A.M.; Greenland, S.; Maldonado, G.; Church, T.R. Proper interpretation of non-differential misclassification effects: Expectations vs observations. Int. J. Epidemiol. 2005, 34, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Ahn, Y.; Park, S.-J.; Kwack, H.-k.; Kim, M.K.; Ko, K.-P.; Kim, S.S. Rice-eating pattern and the risk of metabolic syndrome especially waist circumference in Korean Genome and Epidemiology Study (KoGES). BMC Public Health 2013, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Liu, M. A Positive Causal Relationship between Noodle Intake and Metabolic Syndrome: A Two-Sample Mendelian Randomization Study. Nutrients 2023, 15, 2091. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.-H.; Park, M.-S.; Kim, J.A.; Lim, J.-A. Associations between excessive sodium intake and smoking and alcohol intake among Korean men: KNHANES V. Int. J. Environ. Res. Public Health 2015, 12, 15540–15549. [Google Scholar] [CrossRef]
- Dalmasso, C.; Amigone, J.L.; Vivas, L. Serotonergic system involvement in the inhibitory action of estrogen on induced sodium appetite in female rats. Physiol. Behav. 2011, 104, 398–407. [Google Scholar] [CrossRef]
- Greenberg, A. Diuretic complications. Am. J. Med. Sci. 2000, 319, 10–24. [Google Scholar] [CrossRef]
| Men (n = 43,850) | Women (n = 86,573) | |||||||
|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | |
| Calcium Intake | ||||||||
| Age (years, med, Q1, Q3) | 54 (47, 61) | 54 (47, 60) | 53 (46, 60) | 53 (46, 60) | 52 (47, 61) | 52 (47, 60) | 52 (46, 60) | 52 (46, 60) |
| Marital status (married, n, %) | 10,145 (93.0) | 10,288 (94.2) | 10,329 (94.5) | 10,398 (95.1) | 18,229 (84.6) | 18,724 (86.8) | 18,844 (87.4) | 19,042 (88.3) |
| Education (>12 year, n, %) | 3582 (33.2) | 3978 (36.7) | 4062 (37.6) | 4422 (40.8) | 3396 (15.9) | 4187 (19.6) | 4414 (20.6) | 4822 (22.6) |
| Employment (occupied, n, %) | 8489 (79.5) | 8742 (81.4) | 8839 (82.2) | 8810 (82.0) | 8276 (39.2) | 8464 (40.0) | 8566 (40.6) | 8156 (38.8) |
| Family income (≥3000 $/month, n, %) | 4380 (45.8) | 4769 (48.9) | 5052 (51.8) | 5066 (52.1) | 7284 (39.5) | 8236 (44.1) | 8393 (45.1) | 8592 (47.2) |
| Current smoker * | 3486 (31.9) | 3545 (32.4) | 3516 (32.1) | 3398 (31.1) | 574 (2.7) | 473 (2.2) | 486 (2.3) | 479 (2.2) |
| Current drinker * | 7815 (71.4) | 8115 (74.2) | 8011 (73.3) | 7948 (72.7) | 6318 (29.3) | 6745 (31.3) | 6674 (30.9) | 6680 (31.0) |
| Regular exercise * | 5581 (51.1) | 6029 (55.1) | 6410 (58.6) | 6980 (63.8) | 9356 (43.3) | 10,647 (49.3) | 11,420 (52.9) | 12,784 (59.2) |
| BMI (kg/m2, med, Q1, Q3) | 24.2 (22.5, 26.0) | 24.3 (22.6, 26.1) | 24.4 (22.6, 26.2) | 24.5 (22.8, 26.2) | 23.3 (22.5, 26.0) | 23.3 (22.6, 26.1) | 23.3 (22.6, 26.2) | 23.3 (22.8, 26.2) |
| Total energy intake (kcal/day, med, Q1, Q3) | 1466 (1296, 1644) | 1701 (1524, 1,914) | 1883 (1676, 2134) | 2220 (1928, 2593) | 1345 (1296, 1644) | 1574 (1524, 1914) | 1747 (1676, 2134) | 2060 (1928, 2593) |
| Family history Hypertension * | 2624 (23.9) | 2646 (24.1) | 2724 (24.9) | 2657 (24.2) | 6659 (30.8) | 7006 (32.4) | 7150 (33.0) | 6890 (31.8) |
| Family history Diabetes * | 1699 (15.5) | 1831 (16.7) | 1768 (16.1) | 1822 (16.6) | 4121 (19.0) | 4298 (19.9) | 4306 (19.9) | 4243 (19.6) |
| Family history Hyperlipidemia * | 86 (1.4) | 86 (1.4) | 91 (1.5) | 93 (1.5) | 324 (2.7) | 380 (3.1) | 385 (3.2) | 382 (3.3) |
| Sodium Intake | ||||||||
| Age (years, med, Q1, Q3) | 54 (48, 61) | 54 (47, 61) | 53 (47, 60) | 52 (46, 60) | 52 (48, 61) | 52 (47, 61) | 52 (47, 60) | 51 (46, 60) |
| Marital status (married, n, %) | 10,226 (93.6) | 10,272 (94.1) | 10,306 (94.3) | 10,356 (94.8) | 18,046 (83.8) | 18,638 (86.5) | 18,976 (88.0) | 19,179 (89.0) |
| Education (>12 year, n, %) | 4051 (37.4) | 4077 (37.6) | 3953 (36.5) | 3963 (36.7) | 3802 (17.8) | 4437 (20.7) | 4281 (20.0) | 4299 (20.2) |
| Employment (occupied, n, %) | 8518 (79.6) | 8612 (80.2) | 8815 (82.0) | 8935 (83.4) | 8077 (38.3) | 8481 (40.1) | 8445 (39.9) | 8459 (40.3) |
| Family income (≥3000 $/month, n, %) | 4759 (49.1) | 4918 (50.4) | 4840 (49.5) | 4750 (49.8) | 7639 (41.0) | 8563 (45.6) | 8287 (44.4) | 8016 (44.9) |
| Current smoker * | 3089 (28.2) | 3417 (31.2) | 3586 (32.8) | 3853 (35.2) | 503 (2.3) | 539 (2.5) | 464 (2.2) | 506 (2.4) |
| Current drinker * | 7580 (69.3) | 7976 (72.9) | 8112 (74.1) | 8221 (75.1) | 6206 (28.8) | 6742 (31.3) | 6618 (30.7) | 6851 (31.8) |
| Regular exercise * | 6146 (56.2) | 6174 (56.5) | 6255 (57.2) | 6425 (58.7) | 10,801 (50.0) | 10,925 (50.6) | 11,095 (51.4) | 11,386 (52.7) |
| BMI (kg/m2, med, Q1, Q3) | 24.2 (22.5, 26.0) | 24.3 (22.5, 26.0) | 24.3 (22.5, 26.1) | 24.6 (22.9, 26.3) | 23.2 (22.5, 26.0) | 23.2 (22.5, 26.0) | 23.4 (22.5, 26.1) | 23.5 (22.9, 26.3) |
| Total energy intake (kcal/day, med, Q1, Q3) | 1525 (1326, 1741) | 1713 (1485, 1990) | 1851 (1623, 2135) | 2138 (1839, 2535) | 1377 (1326, 1741) | 1581 (1485, 1990) | 1714 (1623, 2135) | 1977 (1839, 2535) |
| Family history Hypertension * | 2692 (24.6) | 2703 (24.7) | 2741 (25.0) | 2515 (22.9) | 7033 (32.5) | 7039 (32.5) | 6888 (31.8) | 6745 (31.2) |
| Family history Diabetes * | 1753 (16.0) | 1809 (16.5) | 1800 (16.4) | 1758 (16.0) | 4309 (19.9) | 4291 (19.8) | 4165 (19.2) | 4203 (19.4) |
| Family history Hyperlipidemia * | 98 (1.6) | 79 (1.2) | 95 (1.5) | 84 (1.5) | 383 (3.1) | 393 (3.1) | 334 (2.7) | 361 (3.4) |
| Men (n = 43,850) | Women (n = 86,573) | |||||
|---|---|---|---|---|---|---|
| Median Value (Q3–Q1) | ORIQR (95% CI) | Median Value (Q3–Q1) | ORIQR (95% CI) | |||
| MetS (n = 12,640) | Control (n = 31,210) | MetS (n = 21,028) | Control (n = 65,545) | |||
| Calcium (mg) | 378 (258) | 381 (268) | 0.94 (0.91–0.97) | 395 (282) | 413 (294) | 0.92 (0.90–0.94) |
| Dairy products (g/day) | 47 (137.3) | 59 (150.5) | 0.92 (0.88–0.95) | 69 (185.3) | 100 (175.0) | 0.90 (0.87–0.92) |
| Vegetables except for Kimchi and Korean-style pickles (g/day) | 105 (96.3) | 103 (97.6) | 0.99 (0.96–1.01) | 113 (105.3) | 115 (109.2) | 1.01 (0.99–1.02) |
| Kimchi (g/day) | 150 (138.1) | 150 (129.8) | 1.04 (1.02–1.07) | 125 (128.0) | 112 (119.3) | 1.05 (1.03–1.07) |
| Fishes except for salt-fermented fish (g/day) | 34 (35.0) | 32 (34.4) | 1.00 (0.98–1.02) | 30 (34.2) | 31 (34.2) | 0.99 (0.97–1.01) |
| Legumes (g/day) | 27 (33.1) | 26 (33.8) | 0.98 (0.96–1.00) | 23 (32.5) | 26 (34.0) | 0.99 (0.98–1.00) |
| Beverages except for coffee and green tea (g/day) | 26 (46.6) | 29 (50.1) | 0.98 (0.97–0.99) | 27 (43.3) | 33 (50.2) | 0.98 (0.97–0.99) |
| Seaweeds (g/day) | 1.4 (1.73) | 1.4 (1.63) | 1.01 (0.98–1.04) | 1.5 (2.32) | 1.5 (2.30) | 1.01 (0.99–1.02) |
| Eggs (g/day) | 11 (10.1) | 11 (9.6) | 0.99 (0.98–1.01) | 4 (9.5) | 11 (10.4) | 0.95 (0.94–0.96) |
| Fermented pastes (g/day) | 4.5 (4.82) | 4.3 (4.82) | 1.04 (1.01–1.06) | 3.9 (4.61) | 3.2 (3.39) | 1.01 (0.99–1.03) |
| Breads (g/day) | 5.3 (13.58) | 6.0 (15.00) | 0.95 (0.94–0.97) | 4.2 (11.83) | 6.0 (17.08) | 0.94 (0.93–0.95) |
| Men (n = 43,850) | Women (n = 86,573) | |||||
|---|---|---|---|---|---|---|
| Median Value (Q3–Q1) | ORIQR (95% CI) | Median Value (Q3–Q1) | ORIQR (95% CI) | |||
| MetS (n = 12,640) | Control (n = 31,210) | MetS (n = 21,028) | Control (n = 65,545) | |||
| Sodium (mg) | 2532 (1739) | 2467 (1687) | 1.05 (1.02–1.08) | 2266 (1610) | 2224 (1580) | 1.03 (1.00–1.05) |
| Kimchi (g/day) | 150 (138.1) | 150 (129.8) | 1.04 (1.02–1.07) | 125 (128.0) | 112 (119.3) | 1.05 (1.03–1.07) |
| Fishes except for salt-fermented fish (g/day) | 34 (35.0) | 32 (34.4) | 1.00 (0.98–1.02) | 30 (34.2) | 31 (34.2) | 0.99 (0.97–1.01) |
| Noodles (g/day) | 44 (60.9) | 36 (56.6) | 1.07 (1.05–1.09) | |||
| Vegetables except for Kimchi and Korean-style pickles (g/day) | 113 (105.3) | 115 (109.2) | 1.01 (0.99–1.02) | |||
| p for Interaction | ||||||
|---|---|---|---|---|---|---|
| MetS/Control (%) | OR (95%CI) | |||||
| Low | High | Low | High | |||
| Men | 0.9563 | |||||
| High | 12.2/13.8 | 37.3/36.4 | Ref. | 1.15 (1.06–1.24) | ||
| Low | 36.2/36.8 | 14.3/13.0 | 1.14 (1.05–1.23) | 1.28 (1.17–1.40) | ||
| Women | 0.4853 | |||||
| High | 12.4/14.7 | 35.0/36.2 | Ref. | 1.11 (1.05–1.17) | ||
| Low | 36.6/35.6 | 16.0/13.5 | 1.18 (1.11–1.25) | 1.27 (1.18–1.35) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, B.; Kim, J.; Kim, Y.; Shin, J.; Lee, S.-A. Calcium- and Sodium-Rich Food Intake among Koreans with and without Metabolic Syndrome: Cross-Sectional Analysis of the Korean Genome and Epidemiology Study. Nutrients 2024, 16, 2439. https://doi.org/10.3390/nu16152439
Choi B, Kim J, Kim Y, Shin J, Lee S-A. Calcium- and Sodium-Rich Food Intake among Koreans with and without Metabolic Syndrome: Cross-Sectional Analysis of the Korean Genome and Epidemiology Study. Nutrients. 2024; 16(15):2439. https://doi.org/10.3390/nu16152439
Chicago/Turabian StyleChoi, Byeonggeun, Jiyoon Kim, Yeonjin Kim, Jiae Shin, and Sang-Ah Lee. 2024. "Calcium- and Sodium-Rich Food Intake among Koreans with and without Metabolic Syndrome: Cross-Sectional Analysis of the Korean Genome and Epidemiology Study" Nutrients 16, no. 15: 2439. https://doi.org/10.3390/nu16152439
APA StyleChoi, B., Kim, J., Kim, Y., Shin, J., & Lee, S.-A. (2024). Calcium- and Sodium-Rich Food Intake among Koreans with and without Metabolic Syndrome: Cross-Sectional Analysis of the Korean Genome and Epidemiology Study. Nutrients, 16(15), 2439. https://doi.org/10.3390/nu16152439








