Shift Work, Shifted Diets: An Observational Follow-Up Study on Diet Quality and Sustainability among Healthcare Workers on Night Shifts
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Data Collection Tools
2.3. Instruments to Evaluate Diet Quality and Sustainability
2.4. Physical Activity Assessment
2.5. Statistical Analysis
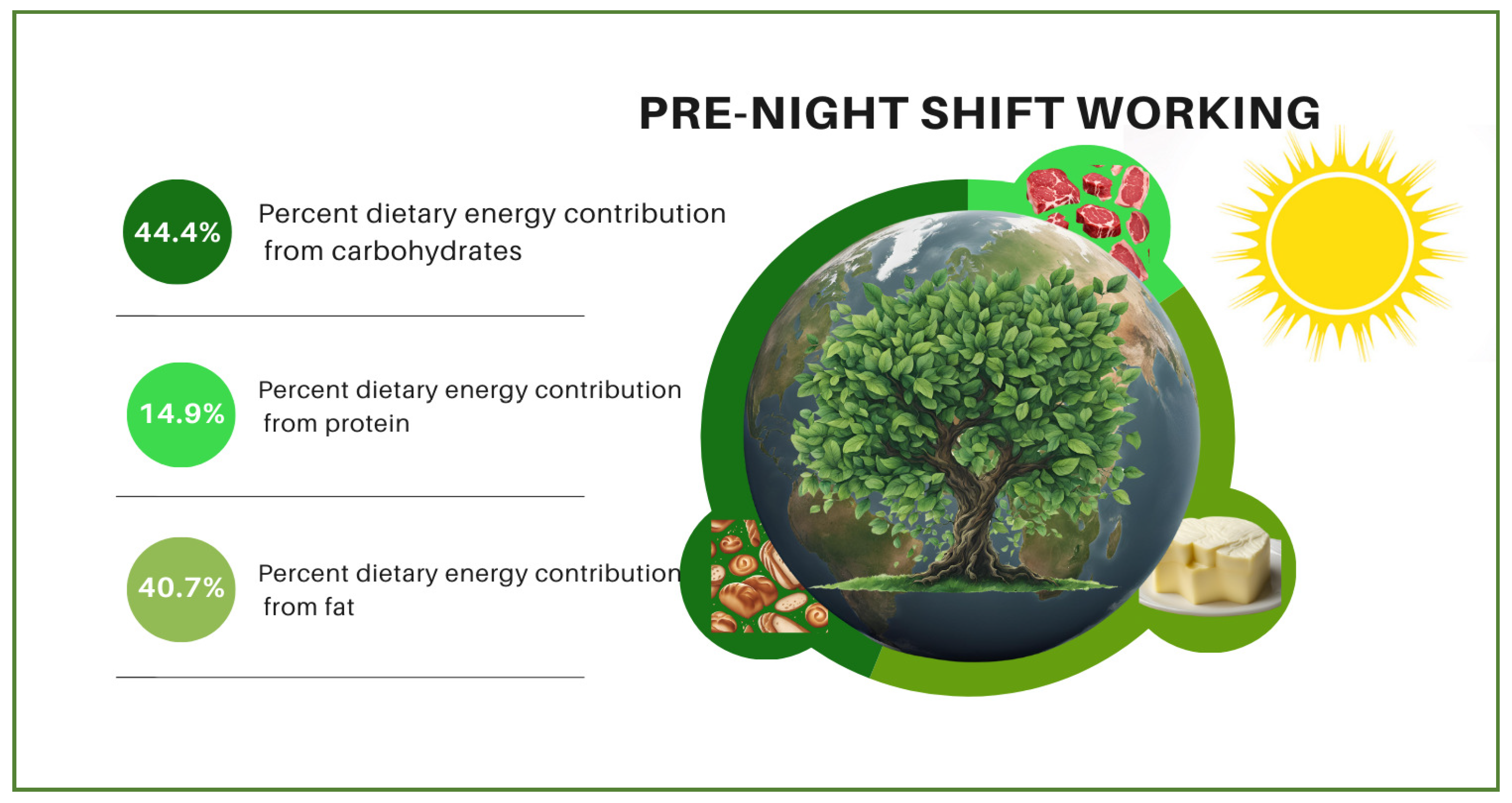
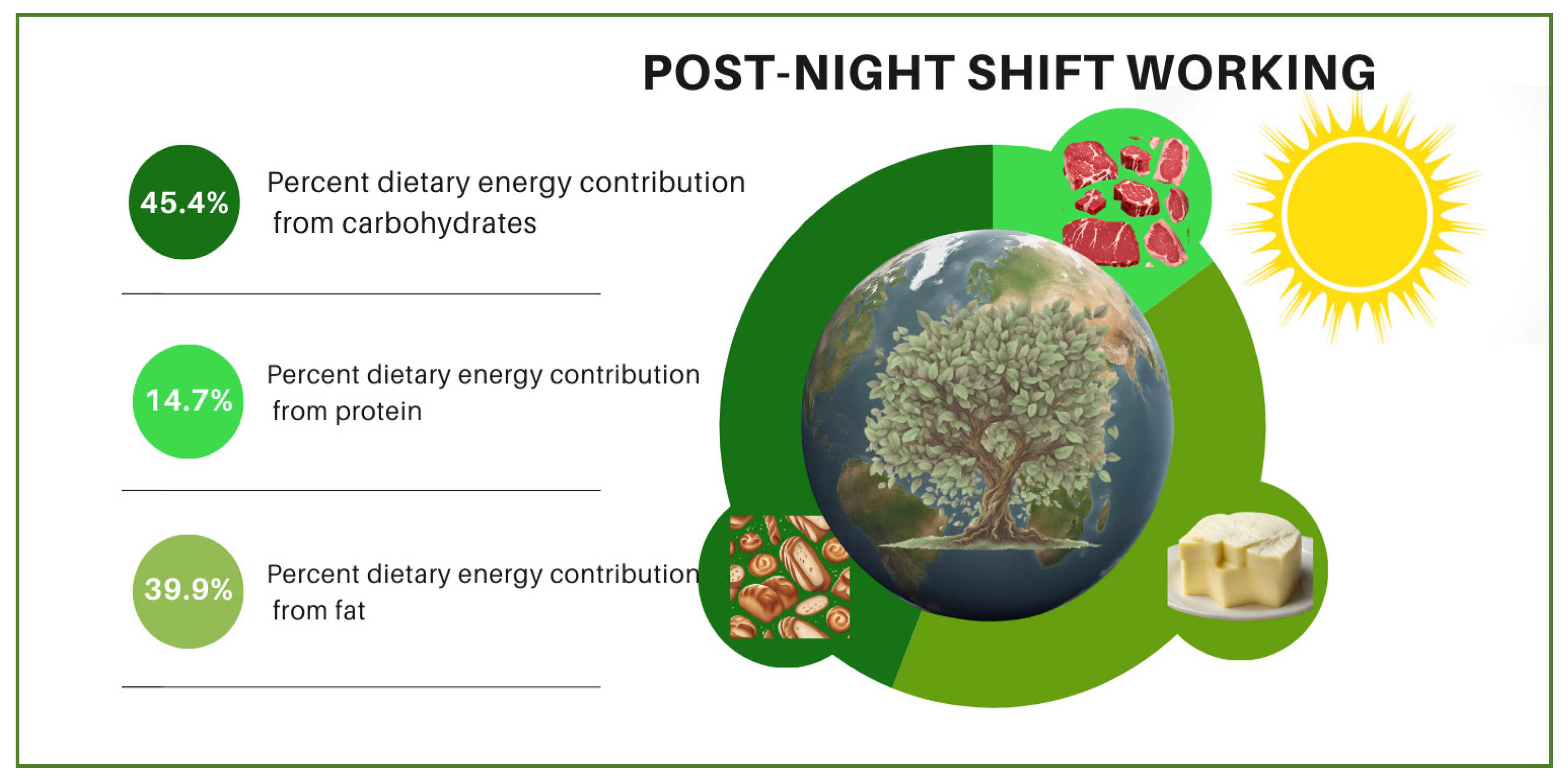
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Labor Force Statistics from the Current Population Survey. Work Schedules (Flexible and Shift Schedules). 2018. Available online: https://www.bls.gov/cps/lfcharacteristics.htm#schedules (accessed on 8 June 2024).
- Rijk, M.G.; Vries, H.H.M.; Mars, M.; Feskens, E.J.M.; Boesveldt, S. Dietary taste patterns and diet quality of female nurses around the night shift. Eur. J. Nutr. 2024, 63, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Berent, D.; Skoneczny, M.; Macander, M.; Wojnar, M. The association among health behaviors, shift work and chronic morbidity: A cross-sectional study on nurses working in full-time positions. J. Public Health Res. 2022, 11, 2099. [Google Scholar] [CrossRef] [PubMed]
- Mazurek Melnyk, B.; Pavan Hsieh, A.; Tan, A.; Teall, A.M.; Weberg, D.; Jun, J.; Gawlik, K.; Hoying, J. Associations among nurses’ mental/physical health, lifestyle behaviors, shift length, and workplace wellness support during COVID-19: Important implications for health care systems. Nurs. Adm. Q. 2022, 46, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Shaw, E.; Dorrian, J.; Coates, A.M.; Leung, G.K.W.; Davis, R.; Rosbotham, E.; Warnock, R.; Huggins, C.E.; Bonham, M.P. Temporal pattern of eating in night shift workers. Chronobiol. Int. 2019, 36, 1613.e52. [Google Scholar] [CrossRef]
- Flanagan, A.; Lowson, E.; Arber, S.; Griffin, B.A.; Skene, D.J. Dietary patterns of nurses on rotational shifts are marked by redistribution of energy into the nightshift. Nutrients 2020, 12, 1053. [Google Scholar] [CrossRef] [PubMed]
- Pepłońska, B.; Nowak, P.; Trafalska, E. The association between night shift work and nutrition patterns among nurses: A literature review. Medycyna Pracy 2019, 70, 363–376. [Google Scholar] [CrossRef] [PubMed]
- Rangel, T.L.; Bindler, T.S.R.; Roney, J.K.; Penders, R.A.; Faulkner, R.; Miller, L.; Sperry, M.; James, L.; Wilson, M.L. Exercise, diet, and sleep habits of nurses working full-time during the COVID-19 pandemic: An observational study. Appl. Nurs. Res. 2023, 69, 151665. [Google Scholar] [CrossRef]
- Farías, R.; Sepúlveda, A.; Chamorro, R. Impact of shift work on the eating pattern, physical activity and daytime sleepiness among chilean healthcare workers. Saf. Health Work. 2020, 11, 367–371. [Google Scholar] [CrossRef]
- Frank, S.M.; Jaacks, L.M.; Adair, L.S.; Avery, C.L.; Meyer, K.; Rose, D.; Taillie, L.S. Adherence to the Planetary Health Diet Index and correlation with nutrients of public health concern: An analysis of NHANES 2003–2018. Am. J. Clin. Nutr. 2024, 119, 384–392. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Fact Sheets. A Healthy Lifestyle-WHO Recommendations. 2010. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 8 June 2024).
- Merdol, T.K. Standart Yemek Tarifeleri, 1st ed.; Hatipoğlu Yayınevi: Ankara, Türkiye, 2011; pp. 10–200. [Google Scholar]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Cacau, L.T.; Carli, E.; de Carvalho, A.M.; Lotufo, P.A.; Moreno, L.A.; Bensenor, I.M.; Marchioni, D.M. Development and validation of an index based on EAT-Lancet recommendations: The planetary health diet index. Nutrients 2021, 13, 1698. [Google Scholar] [CrossRef]
- Marshall, A.L.; Smith, B.J.; Bauman, A.E.; Kaur, S. Reliability and validity of a brief physical activity assessment for use by family doctors. Br. J. Sports Med. 2005, 39, 294–297. [Google Scholar] [CrossRef]
- Suyoto, P.S.T.; de Rijk, M.G.; de Vries, J.H.; Feskens, E.J.M. The effect of meal glycemic index and meal frequency on glycemic control and variability in female nurses working night shifts: A two-arm randomized cross-over trial. J. Nutr. 2024, 154, 69–78. [Google Scholar] [CrossRef]
- Chellappa, S.L.; Qian, J.; Vujovic, N.; Morris, C.J.; Nedeltcheva, A.; Nguyen, H.; Rahman, N.; Heng, S.W.; Kelly, L.; Kerlin-Monteiro, K.; et al. Daytime eating prevents internal circadian misalignment and glucose intolerance in night work. Sci. Adv. 2022, 7, eabg9910. [Google Scholar] [CrossRef]
- Augustin, L.S.A.; Kendall, C.W.C.; Jenkins, D.J.A.; Willett, W.C.; Astrup, A.; Barclay, A.W.; Björck, I.; Brand-Miller, J.C.; Brighenti, F.; Buyken, A.E.; et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr. Metab. Cardiovasc. Dis. 2015, 25, 795–815. [Google Scholar] [CrossRef] [PubMed]
- Heath, G.; Dorrian, J.; Coates, A. Associations between shift type, sleep, mood, and diet in a group of shift working nurses. Scand. J. Work Environ. Health 2019, 45, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Hannemann, J.; Laing, A.; Middleton, B.; Schwedhelm, E.; Marx, N.; Federici, M.; Kastner, M.; Skene, D.J.; Böger, R. Effect of oral melatonin treatment on insulin resistance and diurnal blood pressure variability in night shift workers. A double-blind, randomized, placebo-controlled study. Pharmacol. Res. 2024, 199, 107011. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.; Holzhausen, E.A.; Mun, Y. Risk of prostate cancer with increasing years of night shift work: A two-stage dose-response meta-analysis with duration of night shift work as exposure dose. Heliyon 2024, 10, e29080. [Google Scholar] [CrossRef]
- Habib Rodrigues, G.; de Sousa Duarte, A.; Garrido, A.L.F.; Santana, P.T.; Pellegrino, P.; Nogueira, L.F.R.; Crispim, C.A.; Cipolla-Neto, J.; de Castro Moreno, C.R.; Marqueze, E.C. A putative association between food intake, meal timing and sleep parameters among overweight nursing professionals working night shifts. Sleep Epidemiol. 2022, 2, 100040. [Google Scholar] [CrossRef]
- Chen, Y.; Lauren, S.; Chang, B.P.; Shechter, A. Objective food intake in night and day shift workers: A laboratory study. Clocks Sleep 2019, 1, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Kosmadopoulos, A.; Kervezee, L.; Boudreau, P.; Gonzales-Aste, F.; Vujovic, N.; Scheer, F.A.J.L.; Boivin, D.B. Effects of shift work on the eating behavior of police officers on patrol. Nutrients 2020, 12, 999. [Google Scholar] [CrossRef] [PubMed]
- Jansen, E.C.; Stern, D.; Monge, A.; O’Brien, L.M.; Lajous, M.; Peterson, K.E.; López-Ridaura, R. Healthier dietary patterns are associated with better sleep quality among mid-life Mexican women. J. Clin. Sleep Med. 2020, 16, 1321–1330. [Google Scholar] [CrossRef] [PubMed]
- Crispim, C.A.; Zalcman, I.; Dáttilo, M.; Padilha, H.G.; Tufik, S.; de Mello, M.T. Relação entre sono e obesidade: Uma revisão da literature. Arq. Bras. Endocrinol. Metab. 2007, 51, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Schiavo-Cardozo, D.; Lima, M.M.O.; Parej, J.C.; Geloneze, B. Appetite-regulating hormones from the upper gut: Disrupted control of xenin and ghrelin in night workers. Clin. Endocrinol. 2013, 79, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Balieiro, L.C.; Rossato, L.T.; Waterhouse, J.; Paim, S.L.; Mota, M.C.; Crispim, C.A. Nutritional status and eating habits of bus drivers during the day and night. Chronobiol. Int. 2014, 31, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, E.S.; Canuto, R.; Henn, R.L.; Olinto, B.A.; Macagnan, J.B.A.; Pattussi, M.P.; Busnello, F.M.; Olinto, M.T.A. Alteração no comportamento alimentar de trabalhadores de turnos de um frigorífico do sul do Brasil. Ciência Saúde Coletiva 2015, 20, 2401–2410. [Google Scholar] [CrossRef]
- Mota, M.C.; De-Souza, D.A.; Crispim, C.A. Dietary patterns, metabolic markers and subjective sleep measures in resident physicians. Chronobiol. Int. 2013, 30, 1032–1041. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Bioversity International. Sustainable Diets and Biodiversity: Directions and Solutions for Policy, Research and Action. Available online: http://www.fao.org/3/i3004e/i3004e.pdf (accessed on 27 June 2024).
- Fardet, A.; Rock, E. How to protect both health and food system sustainability? A holistic ‘global health’-based approach via the 3V rule proposal. Public Health Nutr. 2020, 23, 3028–3044. [Google Scholar] [CrossRef]
- Steenson, S.; Buttriss, J.L. The challenges of defining a healthy and ‘sustainable’ diet. Nutr. Bull. 2020, 45, 206–222. [Google Scholar] [CrossRef]
- Meltzer, H.M.; Brantsaeter, A.L.; Trolle, E.; Eneroth, H.; Fogelholm, M.; Ydersbond, T.A.; Birgisdottir, B.E. Environmental sustainability perspectives of the nordic diet. Nutrients 2019, 11, 2248. [Google Scholar] [CrossRef]
- Chaves, D.B.R.; Costa, A.G.S.; Oliveira, A.R.S.; Olivera, T.C.; Araujo, T.L.; Lopes, M.V.O. Risk factors to high blood pressure: Inquiry with bus drivers and collectors. Rev. Enferm. 2008, 16, 370–376. [Google Scholar]
- Cavagioni, L.C. Cardiovascular Risk Profile Observed in Professional Truck Drivers Who Work on Highway BR116 within the Area of the State of São Paulo—Régis Bittencourt. Master’s Thesis, Nursing School, University of São Paulo, São Paulo, Brazil, 2008. [Google Scholar]
- Seffen, A.E.; Dohle, S. What motivates German consumers to reduce their meat consumption? Identifying relevant beliefs. Appetite 2023, 187, 106593. [Google Scholar] [CrossRef] [PubMed]
- Tobler, C.; Visschers, V.H.M.; Siegrist, M. Eating green Consumers’ willingness to adopt ecological food consumption behaviors. Appetite 2011, 57, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Judge, M.; Wilson, M.S. A dual-process motivational model of attitudes towards vegetarians and vegans. Eur. J. Soc. Psychol. 2019, 49, 169–178. [Google Scholar] [CrossRef]
- McHill, A.W.; Hull, J.T.; Klerman, E.B. Chronic circadian disruption and sleep restriction influence subjective hunger, appetite, and food preference. Nutrients 2022, 14, 1800. [Google Scholar] [CrossRef]
- Spiegel, K.; Tasali, E.; Penev, P.; Van Cauter, E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann. Intern. Med. 2004, 141, 846–850. [Google Scholar] [CrossRef]

| Variables | Percentages n (%) | Total PHDI Score (Mean ± SD) | Total HEI-2020 Score (Mean ± SD) | ||||
|---|---|---|---|---|---|---|---|
| Pre-Night-Shift | During Night Shift | Post-Night-Shift | Pre-Night-Shift | During Night Shift | Post-Night-Shift | ||
| Gender | |||||||
| Female | 327 (72.7) | 51.9 ± 13.4 a | 48.2 ± 13.8 b | 50.8 ± 14.9 a | 46.6 ± 9.4 a | 43.8 ± 8.8 b | 44.6 ± 10.2 b |
| F = 10,730.176; p < 0.001; η2 = 0.971 | F = 8034.557; p < 0.001; η2 = 0.985 | ||||||
| Male | 123 (27.3) | 51.9 ± 13.3 a | 48.8 ± 11.7 b | 50.8 ± 14.9 a,b | 44.7 ± 8.4 | 44.6 ± 8.6 | 45.0 ± 8.9 |
| F = 5049.914; p < 0.001; η2 = 0.976 | F = 18,506.432; p = 0.170; η2 = 0.014 | ||||||
| Age group (years) | |||||||
| 20–25 | 122 (27.1) | 49.3 ± 14.1 a | 45.5 ± 12.9 b | 46.2 ± 14.5 a,b | 45.6 ± 9.6 a | 43.4 ± 8.4 b | 42.7 ± 9.9 b |
| F = 3830.169; p < 0.001; η2 = 0.969 | F = 6830.632; p < 0.001; η2 = 0.983 | ||||||
| 26–30 | 188 (41.8) | 52.5 ± 13.2 a | 49.7 ± 13.1 b | 51.7 ± 14.9 a,b | 45.9 ± 9.1 a,b | 44.4 ± 8.6 b | 46.1 ± 9.9 a |
| F = 6845.947; p < 0.001; η2 = 0.973 | F = 10,859.282; p < 0.001; η2 = 0.983 | ||||||
| 31–40 | 140 (31.1) | 53.4 ± 12.8 a | 48.9 ± 13.5 b | 52.9 ± 14.5 a | 46.7 ± 8.8 a | 44.1 ± 9.4 b | 44.7 ± 9.6 b |
| F = 5937.575; p < 0.001; η2 = 0.977 | F = 9026.722; p < 0.001; η2 = 0.985 | ||||||
| BMI (kg/m2) | |||||||
| Normal weight | 288 (64.0) | 51.5 ± 13.3 a | 48.4 ± 13.3 b | 51.2 ± 15.4 a | 46.3 ± 9.5 a | 44.5 ± 8.5 b | 45.2 ± 9.9 a |
| F = 4.642; p = 0.010; η2 = 0.016 | F = 3.407; p = 0.034; η2 = 0.012 | ||||||
| Overweight | 135 (30.0) | 51.7 ± 13.2 a | 47.8 ± 13.5 b | 49.4 ± 13.9 b | 45.1 ± 8.4 a | 43.4 ± 9.2 b | 43.7 ± 9.8 b |
| F = 3.057; p = 0.049; η2 = 0.022 | F = 1.549; p = 0.011; η2 = 0.011 | ||||||
| Obese | 27 (6.0) | 56.8 ± 13.7 | 50.5 ± 11.6 | 50.4 ± 13.7 | 48.8 ± 8.8 | 43.8 ± 9.3 | 45.5 ± 10.1 |
| F = 2.631; p = 0.082; η2 = 0.092 | F = 2.147; p = 0.127; η2 = 0.076 | ||||||
| Marital status | |||||||
| Married | 200 (44.4) | 53.1 ± 12.8 a | 49.4 ± 12.9 b | 51.7 ± 14.6 a,b | 46.7 ± 8.6 a | 44.6 ± 9.2 b | 45.6 ± 9.7 a,b |
| F = 8042.590; p < 0.001; η2 = 0.976 | F = 13,786.891; p < 0.001; η2 = 0.986 | ||||||
| Single | 250 (55.6) | 50.9 ± 13.8 a | 47.5 ± 13.5 b | 49.7 ± 15.1 b | 45.6 ± 9.6 a | 43.6 ± 8.4 b | 44.1 ± 9.9 a,b |
| F = 7959.767; p < 0.001; η2 = 0.970 | F = 13,266.537; p < 0.001; η2 = 0.982 | ||||||
| Job title | |||||||
| Nurse | 267 (59.3) | 50.2 ± 13.5 a | 46.6 ± 12.9 b | 49.1 ± 15.6 b | 46.5 ± 9.0 a | 44.7 ± 8.6 b | 44.6 ± 10.3 b |
| F = 8425.803; p < 0.001; η2 = 0.969 | F = 14,954.402; p < 0.001; η2 = 0.983 | ||||||
| Doctor | 36 (8.0) | 50.5 ± 13.2 a | 46.3 ± 12.9 b | 52.6 ± 14 a | 45.6 ± 9.6 a | 44.9 ± 7.7 b | 48.9 ± 9.6 a |
| F = 1694.439; p < 0.001; η2 = 0.980 | F = 2088.182; p < 0.001; η2 = 0.984 | ||||||
| Emergency medical technician | 100 (22.2) | 54.5 ± 12.8 a | 49.7 ± 12.4 b | 51.6 ± 12.4 a,b | 45.4 ± 9.4 a | 42.1 ± 8.4 b | 44.1 ± 9.4 a,b |
| F = 4620.098; p < 0.001; η2 = 0.979 | F = 7232.001; p < 0.001; η2 = 0.987 | ||||||
| Ambulance care technician | 47 (10.4) | 57.0 ± 12.1 | 56.5 ± 14.2 | 55.6 ± 14.7 | 45.7 ± 9.2 | 43.8 ± 10.5 | 43.9 ± 7.9 |
| F = 2685.913; p = 0.881; η2 = 0.003 | F = 2789.670; p = 0.489; η2 = 0.015 | ||||||
| Sleeping during night shift | |||||||
| Not sleeping | 118 (26.2) | 47.1 ± 11.9 a | 43.9 ± 13.4 b | 46.3 ± 13.3 a,b | 44.9 ± 8.6 a | 42.8 ± 7.6 b | 43.4 ± 9.3 a,b |
| F = 4145.019; p < 0.001; η2 = 0.973 | F = 8357.545; p < 0.001; η2 = 0.986 | ||||||
| 0–2 h sleep | 332 (73.8) | 53.6 ± 13.4 a | 49.9 ± 13.4 b | 52.1 ± 15.1 a | 46.5 ± 9.3 a | 44.5 ± 9.1 b | 45.2 ± 10.1 a,b |
| F = 13,167.330; p < 0.001; η2 = 0.975 | F = 18,804.628; p < 0.001; η2 = 0.983 | ||||||
| Physical activity status | |||||||
| Inadequate | 170 (37.8) | 48.9 ± 13.1 a | 45.8 ± 12.5 b | 48.1 ± 15.3 a,b | 46.7 ± 8.8 | 45.7 ± 8.4 | 45.1 ± 9.9 |
| F = 10,383.005; p < 0.001; η2 = 0.974 | F = 9883.626; p = 0.189; η2 = 0.010 | ||||||
| Adequate | 280 (62.2) | 53.7 ± 13.2 a | 49.9 ± 13.5 b | 52.1 ± 14.4 a | 45.7 ± 9.3 a | 43.0 ± 8.9 b | 44.5 ± 9.9 a,b |
| F = 6230.596; p < 0.001; η2 = 0.974 | F = 16,912.648; p < 0.001; η2 = 0.984 | ||||||
| Indices and Their Components | F | p | η2 | |||
|---|---|---|---|---|---|---|
| HEI-2020 score | 46.1 ± 9.2 a | 44.0 ± 8.8 b | 44.7 ± 9.9 a | 6.277 | 0.002 | 0.014 |
| HEI-2020 components scores [] | ||||||
| Whole grains | 0.8 ± 2.5 a | 0.5 ± 1.9 b | 0.7 ± 2.3 b | 3.633 | 0.027 | 0.008 |
| Refined grains | 7.6 ± 2.9 | 7.2 ± 2.9 | 7.3 ± 3.3 | 2.676 | 0.069 | 0.006 |
| Seafood and plant proteins | 4.9 ± 0.7 a | 4.9 ± 0.5 a | 4.8 ± 0.9 b | 5.626 | 0.006 | 0.012 |
| Sodium | 9.4 ± 1.9 a | 6.7 ± 1.3 b | 9.4 ± 1.9 a | 4.428 | 0.014 | 0.010 |
| Dairy | 3.2 ± 2.1 | 3.1 ± 2.0 | 3.4 ± 2.7 | 1.895 | 0.153 | 0.004 |
| Greens and beans | 3.5 ± 1.7 a | 3.5 ± 1.6 a | 3.2 ± 1.8 b | 5.796 | 0.003 | 0.013 |
| Total vegetable | 3.2 ± 1.5 | 3.2 ± 1.4 | 3.1 ± 1.6 | 0.348 | 0.706 | 0.001 |
| Whole fruit | 3.5 ± 1.9 a | 2.1 ± 1.7 b | 2.4 ± 2.0 a | 6.568 | 0.001 | 0.014 |
| Total fruit | 1.7 ± 1.6 a | 1.3 ± 1.2 b | 1.7 ± 1.7 a | 10.502 | <0.001 | 0.023 |
| Added sugar | 4.9 ± 4.6 a | 4.1 ± 4.5 b | 4.6 ± 4.7 a | 4.662 | 0.010 | 0.010 |
| MUFA/PUFA ratio | 0.1 ± 0.6 b | 0.1 ± 0.5 b | 0.2 ± 1.3 a | 5.001 | 0.014 | 0.011 |
| Saturated fatty acids | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.4 | 1.000 | 0.318 | 0.002 |
| PHDI score [] | 51.9 ± 13.4 a | 48.3 ± 13.2 b | 50.6 ± 14.9 a | 8.208 | <0.001 | 0.018 |
| PHDI components scores [] | ||||||
| Red meat | 1.5 ± 3.5 a | 0.6 ± 2.3 b | 2.3 ± 4.1 c | 27.081 | <0.001 | 0.057 |
| Nuts and peanuts | 5.3 ± 4.2 a | 5.6 ± 4.2 a | 4.7 ± 4.4 b | 5.163 | 0.006 | 0.011 |
| Legumes | 3.2 ± 3.8 b | 3.5 ± 3.8 a | 2.7 ± 3.8 b | 4.332 | 0.013 | 0.010 |
| Chicken and substitutes | 7.7 ± 4.2 a | 6.6 ± 4.7 b | 8.0 ± 3.9 a | 13.943 | <0.001 | 0.030 |
| Fish and seafood | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.1 ± 0.1 | 0.640 | 0.491 | 0.001 |
| Eggs | 0.4 ± 1.5 a | 0.9 ± 2.4 b | 2.9 ± 3.7 a | 106.921 | <0.001 | 0.192 |
| Fruits | 6.9 ± 3.7 | 6.4 ± 3.6 | 6.4 ± 3.9 | 2.4560 | 0.086 | 0.005 |
| Vegetables | 6.7 ± 2.5 a | 8.7 ± 2.5 a | 8.3 ± 3.0 b | 3.469 | 0.033 | 0.008 |
| DGV/total ratio | 0.5 ± 0.3 | 0.4 ± 0.3 | 0.4 ± 0.3 | 0.056 | 0.944 | 0.000 |
| ReV/total ratio | 0.8 ± 0.3 a | 0.9 ± 0.3 b | 0.8 ± 0.4 b | 6.928 | 0.001 | 0.015 |
| Whole cereals | 0.7 ± 1.8 a | 0.4 ± 0.3 b | 0.6 ± 0.3 a,b | 3.633 | 0.027 | 0.008 |
| Tubers and potatoes | 0.3 ± 0.1 | 0.4 ± 0.1 | 0.5 ± 0.8 | 1.907 | 0.150 | 0.004 |
| Dairy | 2.7 ± 0.3 a | 2.9 ± 0.4 a | 2.3 ± 0.3 b | 4.613 | 0.010 | 0.010 |
| Vegetable oils | 3.9 ± 0.6 a | 3.2 ± 0.7 b | 3.1 ± 0.4 b | 6.853 | 0.001 | 0.015 |
| Animal fats | 5.1 ± 0.9 a | 4.6 ± 0.4 b | 5.7 ± 0.9 c | 7.822 | 0.001 | 0.017 |
| Added sugar | 4.3 ± 0.6 a | 3.4 ± 0.4 b | 4.1 ± 0.6 a | 5.706 | 0.003 | 0.013 |
| Variables | SS | df | MS | F | p | ηp2 |
|---|---|---|---|---|---|---|
| PHDI total scores | ||||||
| Night shift working | 2933.499 | 2 | 1466.750 | 8.208 | <0.001 | 0.018 |
| Night shift working * Gender | 16.190 | 2 | 8.095 | 0.045 | 0.956 | 0.000 |
| Night shift working * Age group | 513.499 | 4 | 128.375 | 0.717 | 0.580 | 0.003 |
| Night shift working * BMI group | 581.021 | 4 | 145.255 | 0.812 | 0.517 | 0.004 |
| Night shift working * Marital status | 5.662 | 2 | 2.831 | 0.016 | 0.984 | 0.000 |
| Night shift working * Job title | 777.763 | 6 | 129.627 | 0.724 | 0.630 | 0.005 |
| Night shift working * Sleeping | 20.722 | 2 | 10.361 | 0.058 | 0.944 | 0.000 |
| Night shift working * Physical activity | 33.696 | 2 | 16.848 | 0.094 | 0.910 | 0.000 |
| HEI-2020 total scores | ||||||
| Night shift working | 975.849 | 2 | 487.924 | 6.277 | 0.002 | 0.014 |
| Night shift working * Gender | 342.720 | 2 | 171.360 | 2.210 | 0.110 | 0.005 |
| Night shift working * Age group | 425.992 | 4 | 106.498 | 1.372 | 0.242 | 0.006 |
| Night shift working * BMI group | 142.162 | 4 | 35.541 | 0.456 | 0.768 | 0.002 |
| Night shift working * Marital status | 14.640 | 2 | 7.320 | 0.094 | 0.910 | 0.000 |
| Night shift working * Job title | 604.204 | 6 | 100.701 | 1.298 | 0.255 | 0.009 |
| Night shift working * Sleeping | 6.188 | 2 | 3.094 | 0.040 | 0.961 | 0.000 |
| Night shift working * Physical activity | 236.282 | 2 | 118.141 | 1.522 | 0.219 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navruz-Varlı, S.; Mortaş, H. Shift Work, Shifted Diets: An Observational Follow-Up Study on Diet Quality and Sustainability among Healthcare Workers on Night Shifts. Nutrients 2024, 16, 2404. https://doi.org/10.3390/nu16152404
Navruz-Varlı S, Mortaş H. Shift Work, Shifted Diets: An Observational Follow-Up Study on Diet Quality and Sustainability among Healthcare Workers on Night Shifts. Nutrients. 2024; 16(15):2404. https://doi.org/10.3390/nu16152404
Chicago/Turabian StyleNavruz-Varlı, Semra, and Hande Mortaş. 2024. "Shift Work, Shifted Diets: An Observational Follow-Up Study on Diet Quality and Sustainability among Healthcare Workers on Night Shifts" Nutrients 16, no. 15: 2404. https://doi.org/10.3390/nu16152404
APA StyleNavruz-Varlı, S., & Mortaş, H. (2024). Shift Work, Shifted Diets: An Observational Follow-Up Study on Diet Quality and Sustainability among Healthcare Workers on Night Shifts. Nutrients, 16(15), 2404. https://doi.org/10.3390/nu16152404







