The Impact of High Levels of Compensatory Exercise on Treatment Outcomes in Threshold and Subthreshold Bulimia Nervosa
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Assessments
2.2.1. ED-Related Clinical Variables and Compensatory Exercise
2.2.2. Psychometric Assessments
2.2.3. Treatment and Outcome Measurements
2.3. Statistical Analysis
3. Results
3.1. Description of the Sample
3.2. Baseline Comparisons between Groups of Compensatory Exercise Levels
3.3. Comparisons Regarding Therapy Outcomes between the Groups
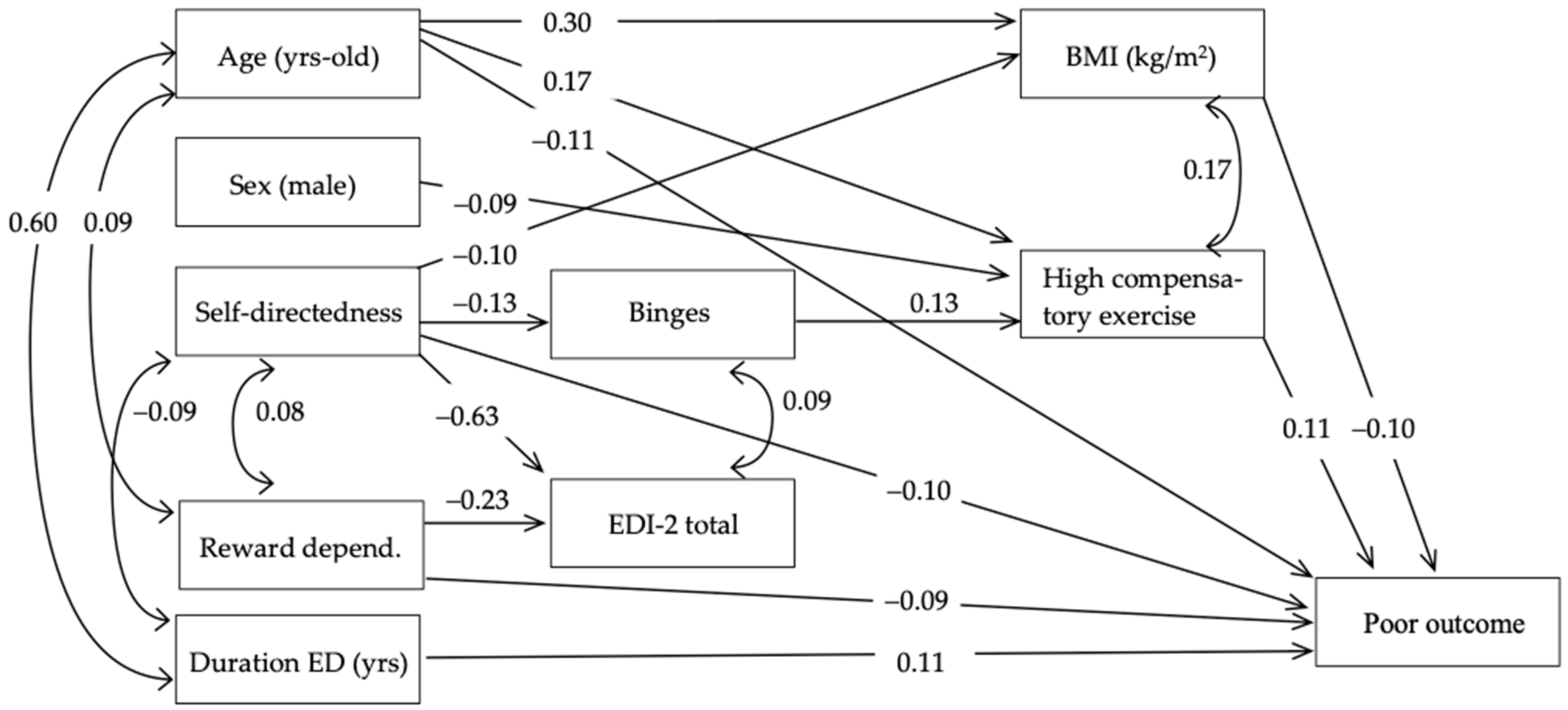
3.4. Path Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Arlington, TX, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- Stice, E.; Marti, C.N.; Rohde, P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J. Abnorm. Psychol. 2013, 122, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Kruger, D. Bulimia nervosa: Easy to hide but essential to recognize. J. Am. Acad. Physician Assist. 2008, 21, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Chapa, D.A.N.; Bohrer, B.K.; Forbush, K.T. Is the diagnostic threshold for bulimia nervosa clinically meaningful? Eat. Behav. 2018, 28, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Raevuori, A.; Suokas, J.; Haukka, J.; Gissler, M.; Linna, M.; Grainger, M.; Suvisaari, J. Highly increased risk of type 2 diabetes in patients with binge eating disorder and bulimia nervosa. Int. J. Eat. Disord. 2015, 48, 555–562. [Google Scholar] [CrossRef]
- Westmoreland, P.; Krantz, M.J.; Mehler, P.S. Medical Complications of Anorexia Nervosa and Bulimia. Am. J. Med. 2016, 129, 30–37. [Google Scholar] [CrossRef]
- Tith, R.M.; Paradis, G.; Potter, B.J.; Low, N.; Healy-Profitós, J.; He, S.; Auger, N.; Tith, R.M.; Paradis, G.; Potter, B.J.; et al. Association of Bulimia Nervosa With Long-term Risk of Cardiovascular Disease and Mortality Among Women. JAMA Psychiatry 2020, 77, 44. [Google Scholar] [CrossRef] [PubMed]
- Ulfvebrand, S.; Birgegård, A.; Norring, C.; Högdahl, L.; von Hausswolff-Juhlin, Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015, 230, 294–299. [Google Scholar] [CrossRef]
- Mustelin, L.; Latvala, A.; Raevuori, A.; Rose, R.J.; Kaprio, J.; Keski-Rahkonen, A. Risky drinking behaviors among women with eating disorders—A longitudinal community-based study. Int. J. Eat. Disord. 2016, 49, 563–571. [Google Scholar] [CrossRef]
- Treasure, J.; Duarte, T.A.; Schmidt, U. Eating disorders. Lancet 2020, 395, 899–911. [Google Scholar] [CrossRef]
- Keel, P.K.; Mitchell, J.E.; Miller, K.B.; Davis, T.L.; Crow, S.J. Long-term Outcome of Bulimia Nervosa. Arch. Gen. Psychiatry 1999, 56, 63. [Google Scholar] [CrossRef]
- Fernández-Aranda, F.; Turón Gil, V.J. Trastornos de la Alimentación: Guía Básica de Tratamiento en Anorexia y Bulimia; Masson: Barcelona, Spain, 1998; ISBN 8445807463. [Google Scholar]
- Wade, T.D. Recent Research on Bulimia Nervosa. Psychiatr. Clin. N. Am. 2019, 42, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Crow, S.J. Pharmacologic Treatment of Eating Disorders. Psychiatr. Clin. N. Am. 2019, 42, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Muratore, A.F.; Attia, E. Psychopharmacologic Management of Eating Disorders. Curr. Psychiatry Rep. 2022, 24, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Steinhausen, H.-C.; Weber, C.S.P. The Outcome of Bulimia Nervosa: Findings From One-Quarter Century of Research. Am. J. Psychiatry 2009, 166, 1331–1341. [Google Scholar] [CrossRef]
- Gull, W. ANOREXIA NERVOSA. Lancet 1888, 131, 516–517. [Google Scholar] [CrossRef][Green Version]
- Wons, O.; Lampe, E.; Patarinski, A.G.; Schaumberg, K.; Juarascio, A. Change in adaptive and maladaptive exercise and objective physical activity throughout CBT for individuals with eating disorders. Eat. Weight Disord. 2023, 28, 40. [Google Scholar] [CrossRef] [PubMed]
- Holland, L.A.; Brown, T.A.; Keel, P.K. Defining features of unhealthy exercise associated with disordered eating and eating disorder diagnoses. Psychol. Sport Exerc. 2014, 15, 116–123. [Google Scholar] [CrossRef]
- Martin, S.J.; Schell, S.E.; Srivastav, A.; Racine, S.E. Dimensions of unhealthy exercise and their associations with restrictive eating and binge eating. Eat. Behav. 2020, 39, 101436. [Google Scholar] [CrossRef]
- Waxman, S.E. A systematic review of impulsivity in eating disorders. Eur. Eat. Disord. Rev. 2009, 17, 408–425. [Google Scholar] [CrossRef]
- Solenberger, S.E. Exercise and eating disorders. Eat. Behav. 2001, 2, 151–168. [Google Scholar] [CrossRef]
- Smith, A.R.; Fink, E.L.; Anestis, M.D.; Ribeiro, J.D.; Gordon, K.H.; Davis, H.; Keel, P.K.; Bardone-Cone, A.M.; Peterson, C.B.; Klein, M.H.; et al. Exercise caution: Over-exercise is associated with suicidality among individuals with disordered eating. Psychiatry Res. 2013, 206, 246–255. [Google Scholar] [CrossRef]
- Lampe, E.W.; Hill, N.G.; Schleyer, B.; Giannone, A.; Juarascio, A.S.; Manasse, S.M. Subtypes of exercise are differentially associated with baseline eating disorder pathology and treatment outcome among individuals with bulimia nervosa. Int. J. Eat. Disord. 2024, 57, 363–375. [Google Scholar] [CrossRef] [PubMed]
- Salkind, N. Structured Clinical Interview for DSM-IV. In Encyclopedia of Measurement and Statistics; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2007; pp. 1–94. [Google Scholar]
- Davis, C. Eating Disorders and Hyperactivity: A Psychobiological Perspective. Can. J. Psychiatry 1997, 42, 168–175. [Google Scholar] [CrossRef]
- Davis, C.; Fox, J. Excessive exercise and weight preoccupation in women. Addict. Behav. 1993, 18, 201–211. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Guidelines on Physical Activity and Sedentary Behaviour. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 23 June 2024).
- Garner, D.M. Eating Disorder Inventory-2; professional manual; Psychological Assessment Resources: Lutz, FL, USA, 1991. [Google Scholar]
- Garner, D.M. EDI 2: Inventario de Trastornos de la Conducta Alimentaria; TEA Ediciones: Madrid, Spain, 1998; Volume 267, ISBN 84-7174-536-4. [Google Scholar]
- Cloninger, C.R. The Temperament and Character Inventory-Revised; Center for Psychobiology of Personality: Sant Louis, MO, USA, 1999. [Google Scholar]
- Gutiérrez-Zotes, J.A.; Bayón, C.; Montserrat, C.; Valero, J.; Labad, A.; Cloninger, C.R.; Fernández-Aranda, F. Temperament and Character Inventory Revised (TCI-R). Standardization and normative data in a general population sample. Actas Españolas Psiquiatr. 2004, 32, 8–15. [Google Scholar]
- Derogatis, L.R.; Unger, R. SCL-90-R: Symptom Checklist-90-Revised: Administration, Scoring and Procedures Manual; Clinical Psychometric Research: Baltimore, MD, USA, 1996. [Google Scholar]
- González de Rivera, J.; De las Cuevas, C.; Rodríguez Abuín, M.; Rodríguez Pulido, F. SCL-90-R, Symptom Cheklist 90 Revised, Spanish Adaptation; TEA: Madrid, Sapin, 2002. [Google Scholar]
- Agüera, Z.; Sánchez, I.; Granero, R.; Riesco, N.; Steward, T.; Martín-Romera, V.; Jiménez-Murcia, S.; Romero, X.; Caroleo, M.; Segura-García, C.; et al. Short-Term Treatment Outcomes and Dropout Risk in Men and Women with Eating Disorders. Eur. Eat. Disord. Rev. 2017, 25, 293–301. [Google Scholar] [CrossRef]
- Agüera, Z.; Riesco, N.; Jiménez-Murcia, S.; Islam, M.A.; Granero, R.; Vicente, E.; Peñas-Lledó, E.; Arcelus, J.; Sánchez, I.; Menchon, J.M.; et al. Cognitive behaviour therapy response and dropout rate across purging and nonpurging bulimia nervosa and binge eating disorder: DSM-5 implications. BMC Psychiatry 2013, 13, 285. [Google Scholar] [CrossRef]
- Finner, H.; Gontscharuk, V. Controlling the Familywise Error Rate with Plug-in Estimator for the Proportion of True Null Hypotheses. J. R. Stat. Soc. Ser. B Stat. Methodol. 2009, 71, 1031–1048. [Google Scholar] [CrossRef]
- Jenkins, D.G.; Quintana-Ascencio, P.F. A solution to minimum sample size for regressions. PLoS ONE 2020, 15, e0229345. [Google Scholar] [CrossRef] [PubMed]
- Maxwell, S.E. Sample size and multiple regression analysis. Psychol. Methods 2000, 5, 434–458. [Google Scholar] [CrossRef]
- Meyer, C.; Taranis, L.; Goodwin, H.; Haycraft, E. Compulsive exercise and eating disorders. Eur. Eat. Disord. Rev. 2011, 19, 174–189. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Jiménez-Murcia, S.; Álvarez-Moya, E.M.; Granero, R.; Vallejo, J.; Bulik, C.M. Impulse control disorders in eating disorders: Clinical and therapeutic implications. Compr. Psychiatry 2006, 47, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.B.; Thuras, P.; Ackard, D.M.; Mitchell, J.E.; Berg, K.; Sandager, N.; Wonderlich, S.A.; Pederson, M.W.; Crow, S.J. Personality dimensions in bulimia nervosa, binge eating disorder, and obesity. Compr. Psychiatry 2010, 51, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Joffe, R.T.; Bagby, R.M.; Levitt, A.J.; Regan, J.J.; Parker, J.D.A. The Tridimensional Personality Questionnaire in major depression. Am. J. Psychiatry 1993, 150, 959–960. [Google Scholar] [CrossRef]
- Cloninger, C.R. A New Conceptual Paradigm from Genetics and Psychobiology for the Science of Mental Health. Aust. N. Z. J. Psychiatry 1999, 33, 174–186. [Google Scholar] [CrossRef]
- Agüera, Z.; Krug, I.; Sánchez, I.; Granero, R.; Penelo, E.; Peñas-Lledó, E.; Jiménez-Murcia, S.; Menchón, J.M.; Fernández-Aranda, F. Personality Changes in Bulimia Nervosa after a Cognitive Behaviour Therapy. Eur. Eat. Disord. Rev. 2012, 20, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Klump, K.L.; Strober, M.; Bulik, C.M.; Thornton, L.; Johnson, C.; Devlin, B.; Fichter, M.M.; Halmi, K.A.; Kaplan, A.S.; Woodside, D.B.; et al. Personality characteristics of women before and after recovery from an eating disorder. Psychol. Med. 2004, 34, 1407–1418. [Google Scholar] [CrossRef] [PubMed]
- Grandi, S.; Clementi, C.; Guidi, J.; Benassi, M.; Tossani, E. Personality characteristics and psychological distress associated with primary exercise dependence: An exploratory study. Psychiatry Res. 2011, 189, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Atiye, M.; Miettunen, J.; Raevuori-Helkamaa, A. A meta-analysis of temperament in eating disorders. Eur. Eat. Disord. Rev. 2015, 23, 139–146. [Google Scholar] [CrossRef]
- Shroff, H.; Reba, L.; Thornton, L.M.; Tozzi, F.; Klump, K.L.; Berrettini, W.H.; Brandt, H.; Crawford, S.; Crow, S.; Fichter, M.M.; et al. Features associated with excessive exercise in women with eating disorders. Int. J. Eat. Disord. 2006, 39, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Calugi, S.; Marchesini, G. Compulsive exercise to control shape or weight in eating disorders: Prevalence, associated features, and treatment outcome. Compr. Psychiatry 2008, 49, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, S.G.; Lydecker, J.A.; Grilo, C.M. Associations between physical activity and eating-disorder psychopathology among individuals categorised with binge-eating disorder and bulimia nervosa. Int. J. Clin. Pract. 2019, 73, e13401. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003, 41, 509–528. [Google Scholar] [CrossRef]
- Fassino, S.; Abbate-Daga, G.; Pierò, A.; Leombruni, P.; Rovera, G.G. Dropout from Brief Psychotherapy within a Combination Treatment in Bulimia nervosa: Role of Personality and Anger. Psychother. Psychosom. 2003, 72, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Fassino, S.; Pierò, A.; Tomba, E.; Abbate-Daga, G. Factors associated with dropout from treatment for eating disorders: A comprehensive literature review. BMC Psychiatry 2009, 9, 67. [Google Scholar] [CrossRef] [PubMed]
- Pham-Scottez, A.; Huas, C.; Perez-Diaz, F.; Nordon, C.; Divac, S.; Dardennes, R.; Speranza, M.; Rouillon, F. Why do people with eating disorders drop out from inpatient treatment?: The role of personality factors. J. Nerv. Ment. Dis. 2012, 200, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.; Davis-Becker, K.; Fischer, S. An exploration of the influence of thinness expectancies and eating pathology on compensatory exercise. Eat. Behav. 2014, 15, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Melissa, R.; Lama, M.; Laurence, K.; Sylvie, B.; Jeanne, D.; Odile, V.; Nathalie, G. Physical Activity in Eating Disorders: A Systematic Review. Nutrients 2020, 12, 183. [Google Scholar] [CrossRef]
- Ashdown-Franks, G.; Firth, J.; Carney, R.; Carvalho, A.F.; Hallgren, M.; Koyanagi, A.; Rosenbaum, S.; Schuch, F.B.; Smith, L.; Solmi, M.; et al. Exercise as Medicine for Mental and Substance Use Disorders: A Meta-review of the Benefits for Neuropsychiatric and Cognitive Outcomes. Sport. Med. 2020, 50, 151–170. [Google Scholar] [CrossRef]
- Vancampfort, D.; Vanderlinden, J.; De Hert, M.; Soundy, A.; Adámkova, M.; Skjaerven, L.H.; Catalán-Matamoros, D.; Lundvik Gyllensten, A.; Gómez-Conesa, A.; Probst, M. A systematic review of physical therapy interventions for patients with anorexia and bulemia nervosa. Disabil. Rehabil. 2014, 36, 628–634. [Google Scholar] [CrossRef]
- Raisi, A.; Zerbini, V.; Piva, T.; Belvederi Murri, M.; Menegatti, E.; Caruso, L.; Masotti, S.; Grazzi, G.; Mazzoni, G.; Mandini, S. Treating Binge Eating Disorder With Physical Exercise: A Systematic Review and Meta-analysis. J. Nutr. Educ. Behav. 2023, 55, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Bakland, M.; Rosenvinge, J.H.; Wynn, R.; Sørlie, V.; Sundgot-Borgen, J.; Fostervold Mathisen, T.; Hanssen, T.A.; Jensen, F.; Innjord, K.; Pettersen, G. A new treatment for eating disorders combining physical exercise and dietary therapy (the PED-t): Experiences from patients who dropped out. Int. J. Qual. Stud. Health Well-Being 2020, 15, 1731994. [Google Scholar] [CrossRef] [PubMed]
- Paslakis, G.; Fauck, V.; Röder, K.; Rauh, E.; Rauh, M.; Erim, Y. Virtual reality jogging as a novel exposure paradigm for the acute urge to be physically active in patients with eating disorders: Implications for treatment. Int. J. Eat. Disord. 2017, 50, 1243–1246. [Google Scholar] [CrossRef] [PubMed]
- Lampe, E.W.; Trainor, C.; Presseller, E.K.; Michael, M.L.; Payne-Reichert, A.; Juarascio, A.S.; Manasse, S.M. Characterizing reasons for exercise in binge-spectrum eating disorders. Eat. Behav. 2021, 43, 101558. [Google Scholar] [CrossRef] [PubMed]
| Total N = 478 | ||
|---|---|---|
| n | % | |
| Sex | ||
| Women | 440 | 92.1% |
| Men | 38 | 7.9% |
| Mean | SD | |
| Age (years) | 29.51 | 9.57 |
| Age of onset ED (years) | 19.54 | 7.85 |
| Duration of the ED (years) | 10.10 | 8.23 |
| BMI (kg/m2) | 25.50 | 6.48 |
| Binge episodes (number/week) | 5.58 | 5.60 |
| Purge episodes (number/week) | 5.37 | 7.18 |
| SCL-90R: global severity index (GSI) | 1.85 | 0.71 |
| SCL-90R: positive symptom total (PST) | 66.82 | 15.73 |
| SCL-90R: positive symptom distress index (PSDI) | 2.41 | 0.56 |
| EDI-2: Total score | 112.57 | 41.88 |
| TCI-R: Novelty seeking | 104.15 | 16.43 |
| TCI-R: Harm avoidance | 118.41 | 20.42 |
| TCI-R: Reward dependence | 101.18 | 15.31 |
| TCI-R: Persistence | 108.33 | 20.99 |
| TCI-R: Self-directedness | 111.71 | 19.89 |
| TCI-R: Cooperativeness | 132.33 | 15.53 |
| TCI-R: Self-transcendence | 65.29 | 14.69 |
| n | % | |
| Compensatory exercise level | ||
| High | 270 | 56.5% |
| Mild–moderate | 84 | 17.6% |
| Low | 124 | 25.9% |
| n | % | |
| Outcome | ||
| Dropout | 235 | 49.2% |
| Non-remission | 51 | 10.7% |
| Partial remission | 94 | 19.7% |
| Total remission | 98 | 20.5% |
| Outcome | ||
| Good | 192 | 40.2% |
| Poor | 286 | 59.8% |
| High N = 270 | Mild– Moderate N = 84 | Low N = 124 | High vs. Mild– Moderate | High vs. Low | Mild– Moderate vs. Low | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | p | |d| | p | |d| | p | |d| | |
| Age (years) | 31.03 | 9.87 | 27.79 | 9.10 | 27.37 | 8.67 | 0.006 * | 0.34 | 0.001 * | 0.39 | 0.756 | 0.05 |
| Age of onset ED (years) | 19.96 | 8.40 | 18.68 | 7.20 | 19.23 | 6.98 | 0.193 | 0.16 | 0.391 | 0.09 | 0.622 | 0.08 |
| Duration of the ED (years) | 11.25 | 8.47 | 9.08 | 7.34 | 8.26 | 7.89 | 0.032 * | 0.28 | 0.001 * | 0.37 | 0.480 | 0.11 |
| BMI (kg/m2) | 26.61 | 7.55 | 24.70 | 5.39 | 23.62 | 3.41 | 0.017 * | 0.29 | 0.001 * | 0.51 † | 0.227 | 0.24 |
| Binges (number/week) | 6.36 | 6.61 | 4.26 | 3.09 | 4.80 | 4.04 | 0.003 * | 0.41 | 0.010 * | 0.28 | 0.493 | 0.15 |
| Purges (number/week) | 5.70 | 7.96 | 5.99 | 7.29 | 4.21 | 4.85 | 0.751 | 0.04 | 0.055 | 0.23 | 0.079 | 0.29 |
| EDI-2: Drive for thinness | 15.67 | 4.66 | 15.85 | 4.28 | 16.52 | 4.49 | 0.759 | 0.04 | 0.084 | 0.19 | 0.292 | 0.15 |
| EDI-2: Body dissatisfaction | 18.74 | 7.29 | 17.04 | 7.43 | 17.55 | 7.82 | 0.068 | 0.23 | 0.141 | 0.16 | 0.627 | 0.07 |
| EDI-2: Interoceptive awareness | 13.10 | 6.88 | 11.17 | 7.09 | 13.44 | 7.33 | 0.028 * | 0.28 | 0.660 | 0.05 | 0.023 * | 0.31 |
| EDI-2: Bulimia | 10.36 | 4.86 | 9.25 | 4.76 | 9.20 | 5.31 | 0.073 | 0.23 | 0.032 * | 0.23 | 0.945 | 0.01 |
| EDI-2: Interpersonal distrust | 6.19 | 4.72 | 5.04 | 4.76 | 5.65 | 4.52 | 0.050 * | 0.24 | 0.287 | 0.12 | 0.357 | 0.13 |
| EDI-2: Ineffectiveness | 12.69 | 7.56 | 9.83 | 6.41 | 11.34 | 7.47 | 0.002 * | 0.41 | 0.091 | 0.18 | 0.148 | 0.22 |
| EDI-2: Maturity fears | 8.93 | 5.85 | 7.57 | 5.47 | 7.74 | 5.64 | 0.059 | 0.24 | 0.057 | 0.21 | 0.833 | 0.03 |
| EDI-2: Perfectionism | 5.98 | 4.43 | 5.87 | 4.82 | 6.68 | 4.55 | 0.843 | 0.02 | 0.158 | 0.15 | 0.208 | 0.17 |
| EDI-2: Impulse regulation | 7.73 | 6.27 | 6.04 | 5.34 | 7.82 | 6.35 | 0.028 * | 0.29 | 0.885 | 0.02 | 0.040 * | 0.30 |
| EDI-2: Asceticism | 8.20 | 3.82 | 6.79 | 3.73 | 8.27 | 4.31 | 0.004 * | 0.37 | 0.862 | 0.02 | 0.008 * | 0.37 |
| EDI-2: Social insecurity | 8.63 | 5.27 | 7.35 | 5.33 | 7.77 | 5.00 | 0.049 * | 0.24 | 0.127 | 0.17 | 0.568 | 0.08 |
| EDI-2: Total score | 116.21 | 41.76 | 101.77 | 39.00 | 111.98 | 43.03 | 0.006 * | 0.36 | 0.349 | 0.10 | 0.084 | 0.25 |
| SCL-90R: Somatization | 1.99 | 0.91 | 1.69 | 0.88 | 1.73 | 0.86 | 0.007 * | 0.34 | 0.008 * | 0.29 | 0.728 | 0.05 |
| SCL-90R: Obsessive | 2.12 | 0.80 | 1.81 | 0.75 | 2.03 | 0.84 | 0.003 * | 0.39 | 0.308 | 0.11 | 0.058 | 0.27 |
| SCL-90R: Sensitivity | 2.23 | 0.90 | 1.86 | 0.86 | 2.18 | 0.86 | 0.001 * | 0.41 | 0.617 | 0.05 | 0.012 * | 0.37 |
| SCL-90R: Depressive | 2.43 | 0.87 | 2.05 | 0.89 | 2.30 | 0.86 | 0.001 * | 0.43 | 0.176 | 0.15 | 0.043 * | 0.28 |
| SCL-90R: Anxiety | 1.87 | 0.88 | 1.59 | 0.90 | 1.76 | 0.86 | 0.010 * | 0.32 | 0.228 | 0.13 | 0.178 | 0.19 |
| SCL-90R: Hostility | 1.57 | 1.03 | 1.19 | 0.87 | 1.41 | 0.91 | 0.002 * | 0.39 | 0.136 | 0.16 | 0.113 | 0.24 |
| SCL-90R: Phobic anxiety | 1.22 | 0.94 | 1.00 | 0.85 | 1.10 | 0.90 | 0.059 | 0.24 | 0.225 | 0.13 | 0.457 | 0.11 |
| SCL-90R: Paranoia | 1.55 | 0.87 | 1.36 | 0.81 | 1.55 | 0.80 | 0.074 | 0.22 | 0.978 | 0.00 | 0.109 | 0.24 |
| SCL-90R: Psychotic | 1.47 | 0.77 | 1.25 | 0.66 | 1.46 | 0.78 | 0.022 * | 0.30 | 0.926 | 0.01 | 0.050 * | 0.29 |
| SCL-90R: global severity index (GSI) | 1.93 | 0.71 | 1.64 | 0.71 | 1.82 | 0.69 | 0.001 * | 0.42 | 0.156 | 0.16 | 0.059 | 0.27 |
| SCL-90R: positive symptom total (PST) | 68.21 | 15.23 | 63.29 | 18.22 | 66.18 | 14.67 | 0.012 * | 0.29 | 0.232 | 0.14 | 0.192 | 0.17 |
| SCL-90R: positive symptom distress index (PSDI) | 2.47 | 0.55 | 2.21 | 0.54 | 2.41 | 0.55 | 0.001 * | 0.47 | 0.332 | 0.10 | 0.011 * | 0.36 |
| TCI-R: Novelty seeking | 103.46 | 17.25 | 104.48 | 14.86 | 105.42 | 15.64 | 0.621 | 0.06 | 0.273 | 0.12 | 0.685 | 0.06 |
| TCI-R: Harm avoidance | 121.68 | 20.29 | 116.74 | 20.41 | 112.44 | 19.36 | 0.049 * | 0.24 | 0.001 * | 0.47 | 0.130 | 0.22 |
| TCI-R: Reward dependence | 101.55 | 14.74 | 101.58 | 16.58 | 100.11 | 15.72 | 0.985 | 0.00 | 0.389 | 0.09 | 0.498 | 0.09 |
| TCI-R: Persistence | 106.00 | 21.98 | 106.73 | 19.49 | 114.49 | 18.57 | 0.780 | 0.03 | 0.001 * | 0.42 | 0.008 * | 0.41 |
| TCI-R: Self-directedness | 110.34 | 20.84 | 112.29 | 19.06 | 114.31 | 18.10 | 0.433 | 0.10 | 0.065 | 0.20 | 0.470 | 0.11 |
| TCI-R: Cooperativeness | 132.09 | 16.18 | 132.21 | 13.43 | 132.91 | 15.51 | 0.950 | 0.01 | 0.628 | 0.05 | 0.751 | 0.05 |
| TCI-R: Self-transcendence | 65.05 | 15.30 | 65.11 | 12.50 | 65.94 | 14.82 | 0.976 | 0.00 | 0.577 | 0.06 | 0.688 | 0.06 |
| High N = 270 | Mild– Moderate N = 84 | Low N = 124 | High vs. Mild– Moderate | High vs. Low | Mild– Moderate vs. Low | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | |C-V| | p | |C-V| | p | |C-V| | |
| Outcome | ||||||||||||
| Dropout | 144 | 53.3% | 41 | 48.8% | 50 | 40.3% | 0.824 | 0.051 | 0.115 | 0.123 | 0.629 | 0.091 |
| Non-remission | 28 | 10.4% | 8 | 9.5% | 15 | 12.1% | ||||||
| Partial remission | 48 | 17.8% | 16 | 19.0% | 30 | 24.2% | ||||||
| Total remission | 50 | 18.5% | 19 | 22.6% | 29 | 23.4% | ||||||
| Outcome | ||||||||||||
| Good | 98 | 36.3% | 35 | 41.7% | 59 | 47.6% | 0.375 | 0.047 | 0.034 * | 0.107 | 0.400 | 0.058 |
| Poor | 172 | 63.7% | 49 | 58.3% | 65 | 52.4% | ||||||
| Independent Variable (Predictor) | B | SE | p | OR | 95%CI OR | NR2 | H-L | |
|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | −0.038 | 0.015 | 0.011 | 0.962 | 0.934 | 0.991 | 0.060 | 0.147 |
| High compensatory exercise | 0.284 | 0.114 | 0.013 | 1.328 | 1.063 | 1.659 | ||
| TCI-R reward dependence | −0.013 | 0.006 | 0.047 | 0.988 | 0.975 | 1.000 | ||
| TCI-R self-directedness | −0.013 | 0.005 | 0.011 | 0.988 | 0.978 | 0.997 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camacho-Barcia, L.; Sánchez, I.; Ibáñez-Caparrós, A.; Ohsako, N.; Granero, R.; Artero, C.; Crespo, J.M.; Paslakis, G.; Jiménez-Murcia, S.; Fernández-Aranda, F. The Impact of High Levels of Compensatory Exercise on Treatment Outcomes in Threshold and Subthreshold Bulimia Nervosa. Nutrients 2024, 16, 2337. https://doi.org/10.3390/nu16142337
Camacho-Barcia L, Sánchez I, Ibáñez-Caparrós A, Ohsako N, Granero R, Artero C, Crespo JM, Paslakis G, Jiménez-Murcia S, Fernández-Aranda F. The Impact of High Levels of Compensatory Exercise on Treatment Outcomes in Threshold and Subthreshold Bulimia Nervosa. Nutrients. 2024; 16(14):2337. https://doi.org/10.3390/nu16142337
Chicago/Turabian StyleCamacho-Barcia, Lucía, Isabel Sánchez, Ana Ibáñez-Caparrós, Noriaki Ohsako, Roser Granero, Cristina Artero, José Manuel Crespo, Georgios Paslakis, Susana Jiménez-Murcia, and Fernando Fernández-Aranda. 2024. "The Impact of High Levels of Compensatory Exercise on Treatment Outcomes in Threshold and Subthreshold Bulimia Nervosa" Nutrients 16, no. 14: 2337. https://doi.org/10.3390/nu16142337
APA StyleCamacho-Barcia, L., Sánchez, I., Ibáñez-Caparrós, A., Ohsako, N., Granero, R., Artero, C., Crespo, J. M., Paslakis, G., Jiménez-Murcia, S., & Fernández-Aranda, F. (2024). The Impact of High Levels of Compensatory Exercise on Treatment Outcomes in Threshold and Subthreshold Bulimia Nervosa. Nutrients, 16(14), 2337. https://doi.org/10.3390/nu16142337










