Comprehensive Care and Education Can Improve Nutritional and Growth Outcomes in Children with Persistent Cow’s Milk, Egg, or Peanut Allergies: A Five-Year Follow-Up Study of Nutritional Status
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Blood Sampling
2.3. Statistical Analysis
3. Results
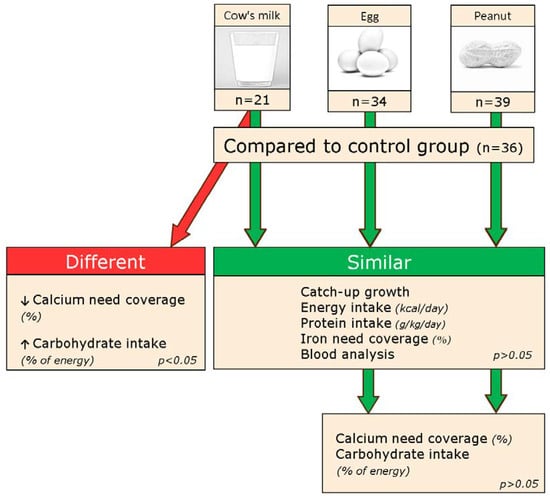
3.1. Growth and Nutritional Status in Children with Cow’s Milk Allergy
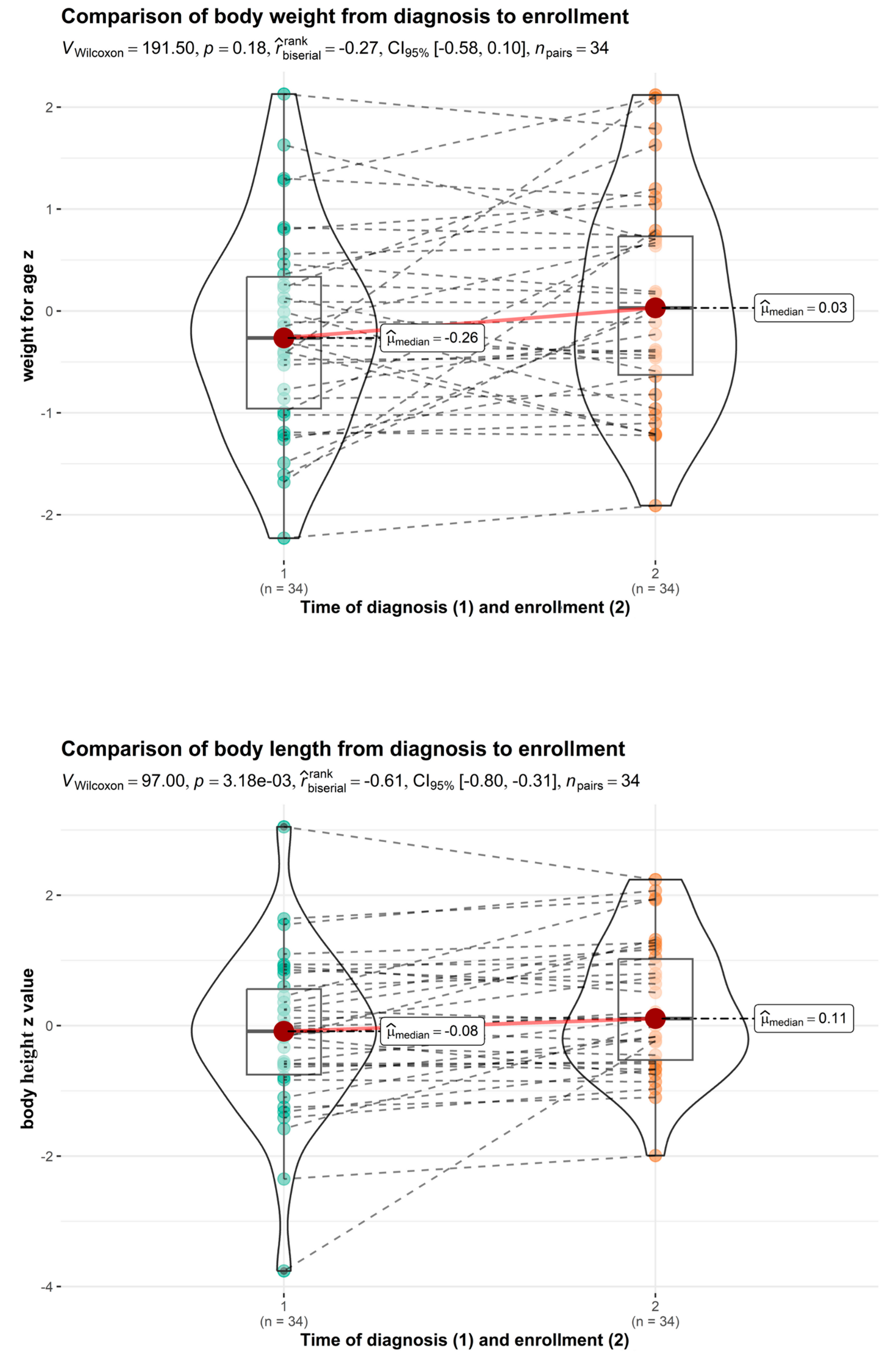
3.2. Growth and Nutritional Status in Children with Egg Allergy
3.3. Growth and Nutritional Status in Children with Peanut Allergy
3.4. Laboratory Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beck, C.; Koplin, J.; Dharmage, S.; Wake, M.; Gurrin, L.; McWilliam, V.; Tang, M.; Sun, C.; Foskey, R.; Allen, K.J.; et al. Persistent Food Allergy and Food Allergy Coexistent with Eczema Is Associated with Reduced Growth in the First 4 Years of Life. J. Allergy Clin. Immunol. Pract. 2016, 4, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Flammarion, S.; Santos, C.; Guimber, D.; Jouannic, L.; Thumerelle, C.; Gottrand, F.; Deschildre, A. Diet and nutritional status of children with food allergies. Pediatr. Allergy Immunol. 2011, 22, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.; De Koker, C.; Dziubak, R.; Godwin, H.; Dominguez-Ortega, G.; Chebar Lozinsky, A.; Skrapac, A.K.; Gholmie, Y.; Reeve, K.; Shah, N. The impact of the elimination diet on growth and nutrient intake in children with food protein-induced gastrointestinal allergies. Clin. Transl. Allergy 2016, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Lynn, C.; Jean Hine, R.; Parkes, J.G. Food allergies in children affect nutrient intake and growth. J. Am. Diet. Assoc. 2002, 102, 1648–1651. [Google Scholar] [CrossRef]
- Prescott, S.L.; Pawankar, R.; Allen, K.J.; Campbell, D.E.; Sinn, J.K.; Fiocchi, A.; Ebisawa, M.; Sampson, H.A.; Beyer, K.; Lee, B.-W. A global survey of changing patterns of food allergy burden in children. World Allergy Organ. J. 2013, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Groetch, M.; Wang, J. Growth and Nutritional Concerns in Children with Food Allergy. Curr. Opin. Allergy Clin. Immunol. 2013, 13, 275–279. [Google Scholar] [CrossRef]
- D’Auria, E.; Abrahams, M.; Zuccotti, G.V.; Venter, C. Personalized Nutrition Approach in Food Allergy: Is It Prime Time Yet? Nutrients 2019, 11, 359. [Google Scholar] [CrossRef] [PubMed]
- Skypala, I.; McKenzie, R. Nutritional Issues in Food Allergy. Clin. Rev. Allergy Immunol. 2019, 57, 166–178. [Google Scholar] [CrossRef]
- Venter, C.; Laitinen, K.; Vlieg-Boerstra, B. Nutritional Aspects in Diagnosis and Management of Food Hypersensitivity—The Dietitians Role. J. Allergy 2012, 2012, 269376. [Google Scholar] [CrossRef]
- Corica, D.; Aversa, T.; Caminiti, L.; Lombardo, F.; Wasniewska, M.; Pajno, G.B. Nutrition and Avoidance Diets in Children with Food Allergy. Front. Pediatr. 2020, 8, 518. [Google Scholar] [CrossRef]
- Mazzocchi, A.; Venter, C.; Maslin, K.; Agostoni, C. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients 2017, 9, 850. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.; De Koker, C.; Dziubak, R.; Venter, C.; Dominguez-Ortega, G.; Cutts, R.; Yerlett, N.; Skrapak, A.K.; Fox, A.T.; Shah, N. Malnutrition in children with food allergies in the UK. J. Hum. Nutr. Diet. 2014, 27, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Sova, C.; Feuling, M.B.; Baumler, M.; Gleason, L.; Tam, J.S.; Zafra, H.; Goday, P.S. A systematic review of nutrient intake and growth in children with multiple IgE-mediated food allergies. Nutr. Clin. Pract. 2013, 28, 669–675. [Google Scholar] [CrossRef]
- Kim, J.; Kwon, J.; Noh, G.; Lee, S.S. The effects of nutritional status in subjects with atopic dermatitis. J. Nutr. Res. Pract. 2013, 7, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Canani, R.B.; Leone, L.; D’Auria, E.; Riva, E.; Nocerino, R.; Ruotolo, S.; Terrin, G.; Cosenza, L.; Di Costanzo, M.; Passariello, A.; et al. The Effects of Dietary Counseling on Children with Food Allergy: A Prospective, Multicenter Intervention Study. J. Acad. Nutr. Diet. 2014, 114, 1432–1439. [Google Scholar] [CrossRef] [PubMed]
- Dupont, C.; Hol, J.; Nieuwenhuis, E.E.S. An extensively hydrolyzed casein–based formula for infants with cows’ milk protein allergy: Tolerance/hypo-allergenicity and growth catch up. Br. J. Nutr. 2015, 113, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.A.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Firke, S. Janitor: Simple Tools for Examining and Cleaning Dirty Data, R Package Version 2.2.0. 2022. Available online: https://cran.r-project.org/web/packages/janitor/index.html (accessed on 5 February 2023).
- Xie, Y.; Cheng, J.; Tan, X. DT: A Wrapper of the JavaScript Library ‘DataTables’, R Package Version 0.27. 2022. Available online: https://cran.r-project.org/package=dt (accessed on 5 February 2023).
- Kuhn, M. Caret: Classification and Regression Training, R Package Version 6.0-93. 2022. Available online: https://cran.r-project.org/package=caret (accessed on 5 February 2023).
- Slowikowski, K. Ggrepel: Automatically Position Non-Overlapping Text Labels with ‘ggplot2’, R Package Version 0.9.2. 2022. Available online: https://cran.r-project.org/package=ggrepel (accessed on 5 February 2023).
- World Health Organization & UNICEF. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children; World Health Organization and UNICEF: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. Global Database on Child Growth and Malnutrition; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Primeau, M.N.; Kagan, R.; Joseph, L.; Lim, H.; Dufresne, C.; Duffy, C.; Prhcal, D.; Clarke, A. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin. Exp. Allergy 2000, 30, 1135–1143. [Google Scholar] [CrossRef]
- Dupont, C.; Chouraqui, J.-P.; Linglart, A.; Bocquet, A.; Darmaun, D.; Feillet, F.; Frelut, M.-L.; Girardet, J.-P.; Hankard, R.; Rozé, J.-C.; et al. Nutritional management of cow’s milk allergy in children: An update. Arch. Pediatr. 2018, 25, 236–243. [Google Scholar] [CrossRef]
- Robbins, K.A.; Wood, R.A.; Keet, C.A. Milk allergy is associated with decreased growth in US children. J. Allergy Clin. Immunol. 2014, 134, 1466–1468. [Google Scholar] [CrossRef]
- Mailhot, G.; Perrone, V.; Alos, N.; Dubois, J.; Delvin, E.; Paradis, L.; Roches, A.D. Cow’s Milk Allergy and Bone Mineral Density in Prepubertal Children. Pediatrics 2016, 137, e20151742. [Google Scholar] [CrossRef] [PubMed]
- Maslin, K.; Oliver, E.M.; Scally, K.S.; Atkinson, J.; Foote, K.; Venter, C.; Roberts, G.; Grimshaw, K.E.C. Nutritional adequacy of a cows’ milk exclusion diet in infancy. Clin. Transl. Allergy 2016, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Bahnson, H.T.; Radulovic, S.; Santos, A.F.; Brough, H.A.; Phippard, D.; Basting, M.; Feeney, M.; et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 2015, 372, 803–813. [Google Scholar] [CrossRef] [PubMed]
- Du Toit, G.; Sayre, P.H.; Roberts, G.; Sever, M.L.; Lawson, K.; Bahnson, H.T.; Brough, H.A.; Santos, A.F.; Harris, K.M.; Radulovic, S.; et al. Effect of avoidance on peanut allergy after early peanut consumption. N. Engl. J. Med. 2016, 374, 1435–1443. [Google Scholar] [CrossRef]



| All Participants (n = 130) | Cow’s Milk (n = 21) | Egg (n = 34) | Peanuts (n = 39) | Control Group (n = 36) |
|---|---|---|---|---|
| Age (years) at diagnosis (SD) | 1.58 (0.99) | 1.41 (1.12) | 2.88(2.11) | / |
| Age (years) at enrolment (SD) | 5.90 (3.06) | 6.24 (3.06) | 8.08 (2.99) | 8.03 (2.79) |
| Sex (male) | 14 (66.7%) | 20 (55%) | 25 (64%) | 18 (48.7%) |
| Body weight for age z at diagnosis | −0.254 (0.866) | −0.347 (0.838) | 0.183 (1.014) | / |
| Body height for age z at diagnosis | 0.252 (1.020) | −0.288 (1.073) | 0.229 (1.092) | / |
| Body weight for age z at enrolment | −0.02 (0.83) | 0.09 (1.03) | 0.47 (1.26) | 0.35 (0.97) |
| Body height for age z at enrolment | 0.34 (1.05) | 0.27 (1.01) | 0.58 (1.13) | 0.74 (1.04) |
| Body mass index z at enrolment | −0.33 (0.68) | −0.12 (1.06) | 0.21 (1.37) | −0.12 (1.20) |
| Comorbidities | ||||
| Atopic dermatitis (n, %) | 7 (33%) | 14 (41.1%) | 15 (38.4%) | 5 (13.8%) |
| Asthma (n, %) | 6 (28.5%) | 8 (23.5%) | 12 (30.7%) | 4 (11.1%) |
| Hay fever (n, %) | 4 (19%) | 11 (32.3%) | 18 (46.1%) | 5 (13.8%) |
| Anaphylaxis (n, %) | 0 | 0 | 2 (0.05%) | 3 (8.3%) |
| Angioedema (n, %) | 0 | 4 (11.7%) | 12 (30.7%) | 2 (5.5%) |
| Dietary intake | ||||
| Coverage of energy needs (%) | 88.73 (22.97) | 86.40 (25.87) | 86.70 (22.86) | 89.59 (26.97) |
| Coverage of iron needs (%) | 77.39 (28.22) | 68.16 (25.87) | 71.76 (25.80) | 77.92 (38.82) |
| Coverage of calcium needs (%) | 44.86 (22.89) | 70.01 (32.10) | 65.21 (27.02) | 63.83 (25.69) |
| Protein intake (g/kg) | 2.31 (0.88) | 2.30 (0.91) | 2.17 (0.82) | 2.20 (0.89) |
| Fat intake (% daily energy) | 27.48 (4.61) | 31.09 (5.34) | 31.85 (5.37) | 30.30 (5.03) |
| Carbohydrate (% daily energy) | 53.65 (5.80) | 53.68 (6.66) | 51.97 (6.69) | 53.65 (5.80) |
| Vitamin D supplementation (n, %) | 21 (100%) | / | / | / |
| Calcium supplementation (n, %) | 19 (90%) | / | / | / |
| Calcium Need Coverage (%) | Control | Cow’s Milk | Total | p |
| Mean (SD) | 63.83 (25.69) | 44.86 (22.89) * | 7.26 (3.05) | 0.027 * |
| Median (Q1, Q3) | 61.91 (46.56, 74.55) | 45.60 (29.20, 53.50) * | 53.89 (38.10, 70.40) | |
| Min–Max | 13.89–124.67 | 17.55–118.83 | 13.89–124.67 | |
| Carbohydrate (% Energy Intake) | Control | Cow’s Milk | Total | p |
| Mean (SD) | 53.65 (5.80) | 57.76 (5.80) ** | 55.14 (6.09) | 0.048 ** |
| Median (Q1, Q3) | 61.91 (46.56, 74.55) | 57.00 (53.00, 63.00) | 54.00 (51.00, 58.00) | |
| Min–Max | 44.00–76.00 | 49.00–66.00 | 44.00–76.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poredoš, T.; Vesel Tajnšek, T.; Koren Jeverica, A.; Zajc Avramovič, M.; Markelj, G.; Emeršič, N.; Avčin, T. Comprehensive Care and Education Can Improve Nutritional and Growth Outcomes in Children with Persistent Cow’s Milk, Egg, or Peanut Allergies: A Five-Year Follow-Up Study of Nutritional Status. Nutrients 2024, 16, 48. https://doi.org/10.3390/nu16010048
Poredoš T, Vesel Tajnšek T, Koren Jeverica A, Zajc Avramovič M, Markelj G, Emeršič N, Avčin T. Comprehensive Care and Education Can Improve Nutritional and Growth Outcomes in Children with Persistent Cow’s Milk, Egg, or Peanut Allergies: A Five-Year Follow-Up Study of Nutritional Status. Nutrients. 2024; 16(1):48. https://doi.org/10.3390/nu16010048
Chicago/Turabian StylePoredoš, Tomaž, Tina Vesel Tajnšek, Anja Koren Jeverica, Mojca Zajc Avramovič, Gašper Markelj, Nina Emeršič, and Tadej Avčin. 2024. "Comprehensive Care and Education Can Improve Nutritional and Growth Outcomes in Children with Persistent Cow’s Milk, Egg, or Peanut Allergies: A Five-Year Follow-Up Study of Nutritional Status" Nutrients 16, no. 1: 48. https://doi.org/10.3390/nu16010048
APA StylePoredoš, T., Vesel Tajnšek, T., Koren Jeverica, A., Zajc Avramovič, M., Markelj, G., Emeršič, N., & Avčin, T. (2024). Comprehensive Care and Education Can Improve Nutritional and Growth Outcomes in Children with Persistent Cow’s Milk, Egg, or Peanut Allergies: A Five-Year Follow-Up Study of Nutritional Status. Nutrients, 16(1), 48. https://doi.org/10.3390/nu16010048