Eating Spicy Food, Dietary Approaches to Stop Hypertension (DASH) Score, and Their Interaction on Incident Stroke in Southwestern Chinese Aged 30–79: A Prospective Cohort Study
Abstract
1. Introduction
2. Methods
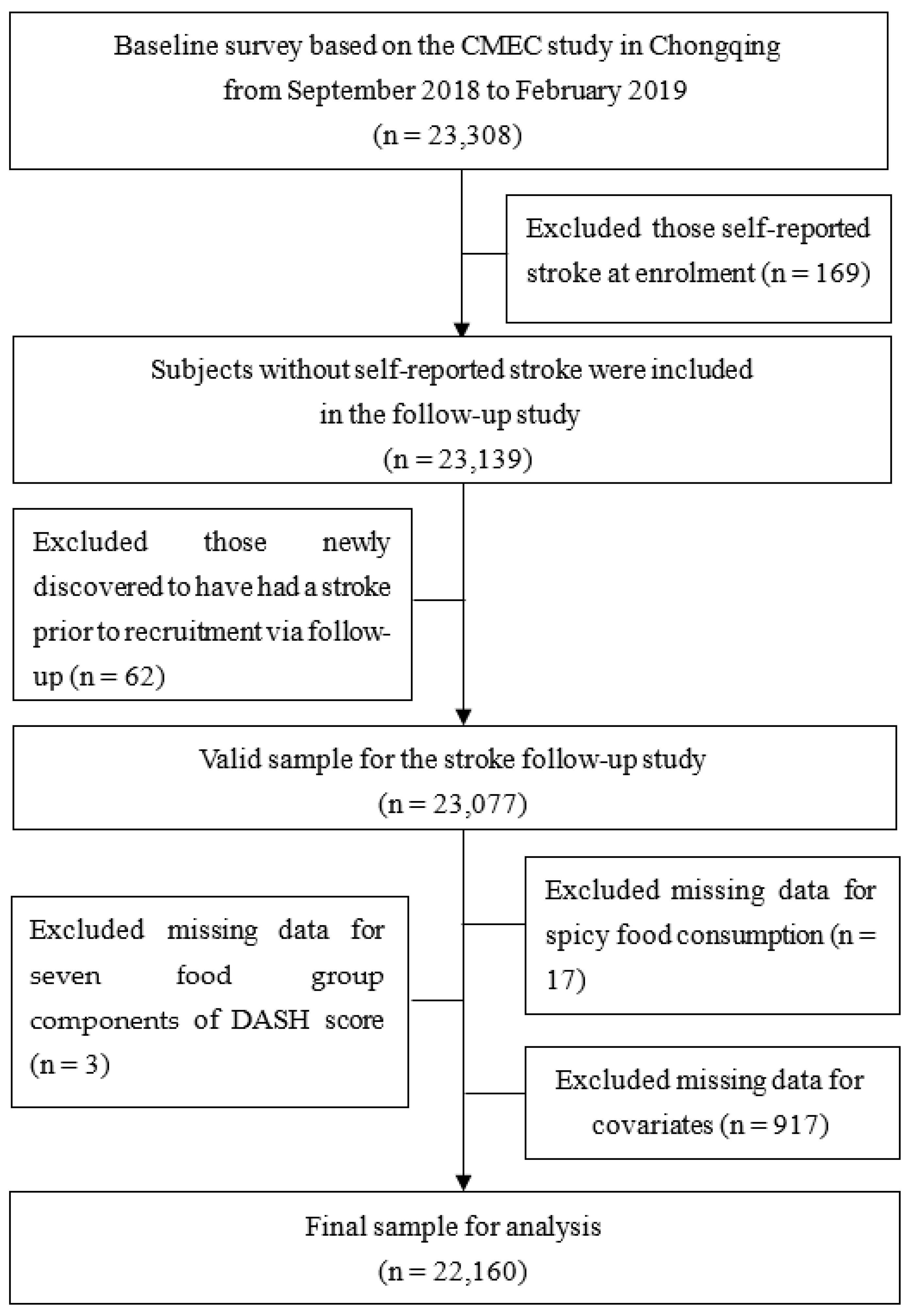
2.1. Study Population
2.2. Follow-Up and Outcome Assessment
2.3. Assessment of Spicy Food Consumption and DASH Score
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
3.1. General Characteristics
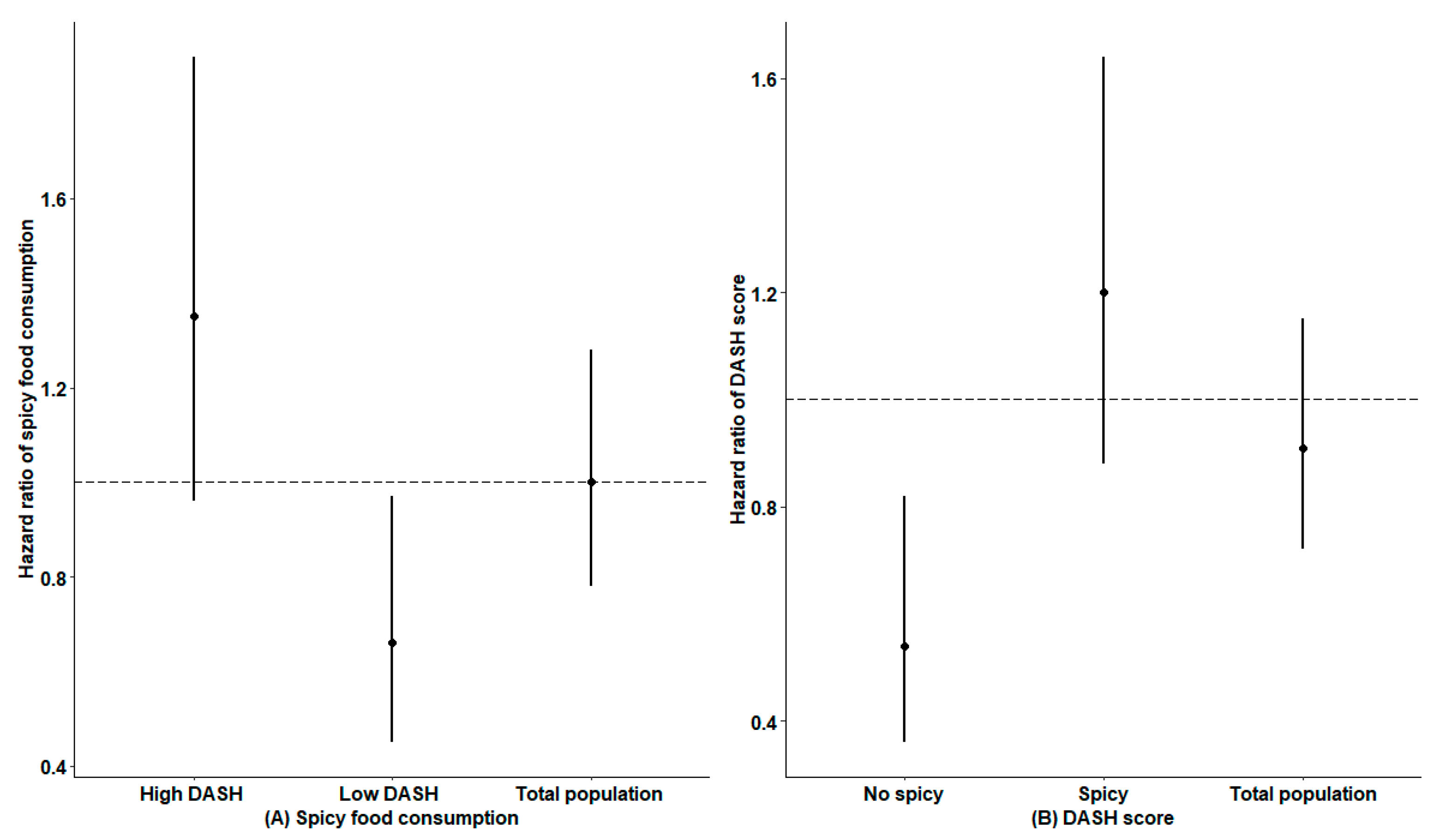
3.2. Independent Effect of Spicy Food Consumption and DASH Score
3.3. Interaction Effect of Spicy Food Consumption and DASH Score on Stroke Incidence
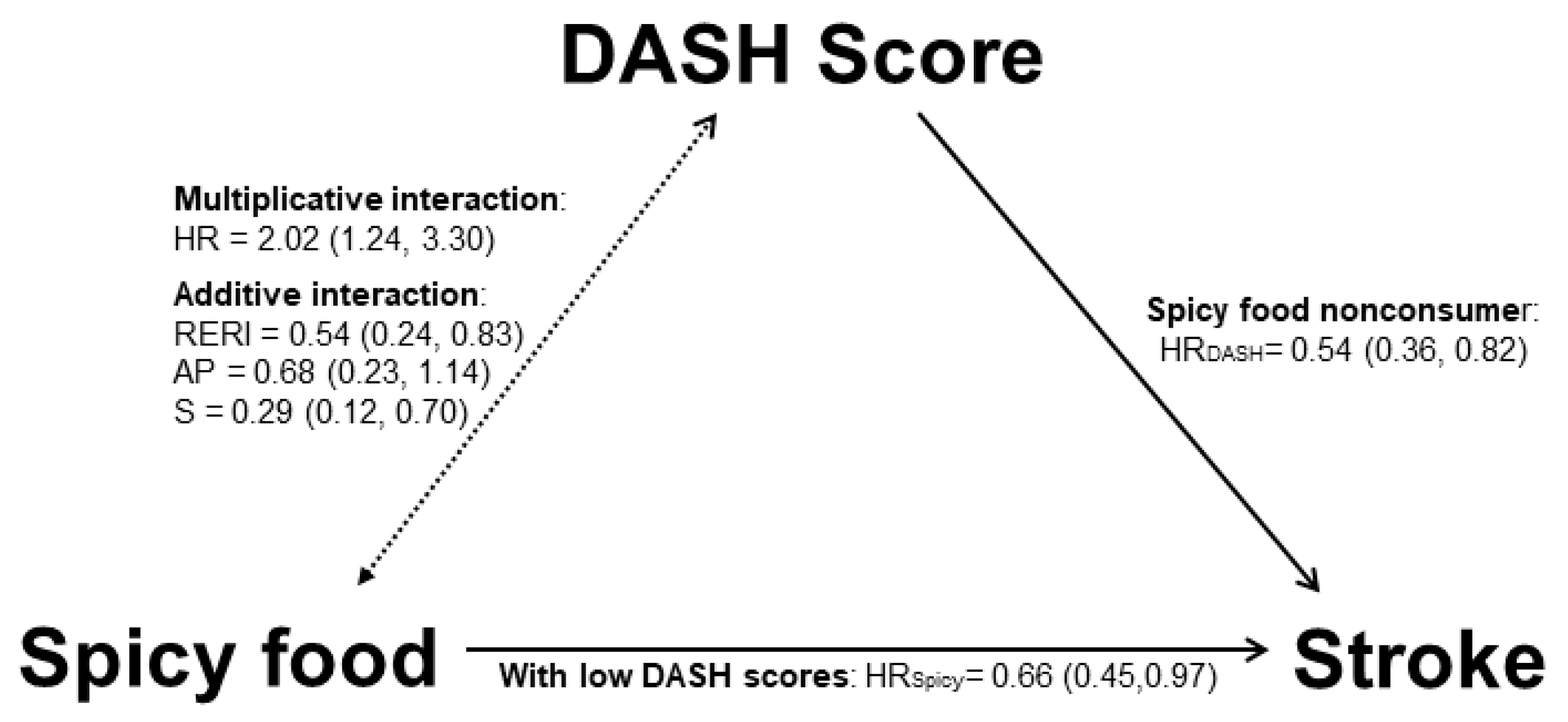
3.4. Summary of Main Results
4. Discussion
4.1. Spicy Food May Be an Effective Nutritional Strategy for Preventing Stroke
4.2. A Higher DASH Score Plays a Beneficial Role in Incident Stroke
4.3. A Negative Interaction May Exist between Spicy Food Consumption and DASH Score
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef]
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Ma, Q.; Li, R.; Wang, L.; Yin, P.; Wang, Y.; Yan, C.; Ren, Y.; Qian, Z.; Vaughn, M.G.; McMillin, S.E.; et al. Temporal trend and attributable risk factors of stroke burden in China, 1990-2019: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2021, 6, e897–e906. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.; Qin, Z.; Lv, X.; Dai, Y.; Ciren, Z.; Yangla, Y.; Zeng, P.; Ma, Y.; Li, X.; Wang, L.; et al. Dietary patterns and cardiometabolic risks in diverse less-developed ethnic minority regions: Results from the China Multi-Ethnic Cohort (CMEC) Study. Lancet Reg. Health West. Pac. 2021, 15, 100252. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelić, D.; Kahleová, H.; Salas-Salvadó, J.; Kendall, C.W.; Sievenpiper, J.L. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [PubMed]
- Talaei, M.; Koh, W.P.; Yuan, J.M.; van Dam, R.M. DASH Dietary Pattern, Mediation by Mineral Intakes, and the Risk of Coronary Artery Disease and Stroke Mortality. J. Am. Heart Assoc. 2019, 8, e011054. [Google Scholar] [CrossRef] [PubMed]
- Soltani, S.; Arablou, T.; Jayedi, A.; Salehi-Abargouei, A. Adherence to the dietary approaches to stop hypertension (DASH) diet in relation to all-cause and cause-specific mortality: A systematic review and dose-response meta-analysis of prospective cohort studies. Nutr. J. 2020, 19, 37. [Google Scholar] [CrossRef] [PubMed]
- Mertens, E.; Markey, O.; Geleijnse, J.M.; Lovegrove, J.A.; Givens, D.I. Adherence to a healthy diet in relation to cardiovascular incidence and risk markers: Evidence from the Caerphilly Prospective Study. Eur. J. Nutr. 2018, 57, 1245–1258. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Fan, S.; Wu, Y.; Zhou, D.; Zhao, R.; Liu, M.; Song, Y. Adherence to the dietary approaches to stop hypertension diet and risk of stroke: A meta-analysis of prospective studies. Medicine 2018, 97, e12450. [Google Scholar] [CrossRef]
- Ao, Z.; Huang, Z.; Liu, H. Spicy Food and Chili Peppers and Multiple Health Outcomes: Umbrella Review. Mol. Nutr. Food Res. 2022, 66, e2200167. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Mohsenpour, M.A.; Nouri, M.; Faghih, S.; Liew, D.; Mazidi, M. Association of Spicy Chilli Food Consumption With Cardiovascular and All-Cause Mortality: A Meta-Analysis of Prospective Cohort Studies. Angiology 2021, 72, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Li, Y.; Yang, K.; Zhang, L.; Xue, Y.; Yu, S.; Liu, X.; Tu, R.; Qiao, D.; Luo, Z.; et al. Associations of spicy food flavour and intake frequency with blood lipid levels and risk of abnormal serum lipid levels in Chinese rural population: A cross-sectional study. Public Health Nutr 2021, 24, 6201–6210. [Google Scholar] [CrossRef] [PubMed]
- Batiha, G.E.; Alqahtani, A.; Ojo, O.A.; Shaheen, H.M.; Wasef, L.; Elzeiny, M.; Ismail, M.; Shalaby, M.; Murata, T.; Zaragoza-Bastida, A.; et al. Biological Properties, Bioactive Constituents, and Pharmacokinetics of Some Capsicum spp. and Capsaicinoids. Int. J. Mol. Sci. 2020, 21, 5179. [Google Scholar] [CrossRef] [PubMed]
- Olatunji, T.L.; Afolayan, A.J. The suitability of chili pepper (Capsicum annuum L.) for alleviating human micronutrient dietary deficiencies: A review. Food Sci. Nutr. 2018, 6, 2239–2251. [Google Scholar] [CrossRef] [PubMed]
- Amini, M.R.; Sheikhhossein, F.; Bazshahi, E.; Hajiaqaei, M.; Shafie, A.; Shahinfar, H.; Azizi, N.; Eghbaljoo Gharehgheshlaghi, H.; Naghshi, S.; Fathipour, R.B.; et al. The effects of capsinoids and fermented red pepper paste supplementation on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. 2021, 40, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Kelava, L.; Nemeth, D.; Hegyi, P.; Keringer, P.; Kovacs, D.K.; Balasko, M.; Solymar, M.; Pakai, E.; Rumbus, Z.; Garami, A. Dietary supplementation of transient receptor potential vanilloid-1 channel agonists reduces serum total cholesterol level: A meta-analysis of controlled human trials. Crit. Rev. Food Sci. Nutr. 2022, 62, 7025–7035. [Google Scholar] [CrossRef]
- Shi, Z.; Riley, M.; Brown, A.; Page, A. Chilli intake is inversely associated with hypertension among adults. Clin. Nutr. ESPEN 2018, 23, 67–72. [Google Scholar] [CrossRef]
- Jang, H.H.; Lee, J.; Lee, S.H.; Lee, Y.M. Effects of Capsicum annuum supplementation on the components of metabolic syndrome: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 20912. [Google Scholar] [CrossRef]
- Sanati, S.; Razavi, B.M.; Hosseinzadeh, H. A review of the effects of Capsicum annuum L. and its constituent, capsaicin, in metabolic syndrome. Iran. J. Basic Med. Sci. 2018, 21, 439–448. [Google Scholar] [CrossRef]
- Yang, X.; Tang, W.; Mao, D.; Liu, X.; Qian, W.; Dai, Y.; Chen, L.; Ding, X. Spicy food consumption is associated with abdominal obesity among Chinese Han population aged 30-79 years in the Sichuan Basin: A population-based cross-sectional study. BMC Public Health 2022, 22, 1881. [Google Scholar] [CrossRef] [PubMed]
- Luo, Q.; Ding, R.; Chen, L.; Bu, X.; Xiao, M.; Liu, X.; Wu, Y.; Xu, J.; Tang, W.; Qiu, J.; et al. The Association Between Spicy Food Intake and Risk of Hyperuricemia Among Chinese Adults. Front. Public Health 2022, 10, 919347. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Jiao, Y.; Mao, D.; Xu, J.; Tang, W.; Jiang, B. Epidemic characteristics of stroke mortality in Chongqing. Public Health Prev. Med. 2021, 32, 20–23. [Google Scholar]
- Zhao, X.; Hong, F.; Yin, J.; Tang, W.; Zhang, G.; Liang, X.; Li, J.; Cui, C.; Li, X.; China Multi-Ethnic Cohort Collaborative Group. Cohort Profile: The China Multi-Ethnic Cohort (CMEC) study. Int. J. Epidemiol. 2021, 50, 721–721l. [Google Scholar] [CrossRef]
- WHO. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Chan, W.C.; Millwood, I.Y.; Kartsonaki, C.; Du, H.; Guo, Y.; Chen, Y.; Bian, Z.; Walters, R.G.; Lv, J.; He, P.; et al. Spicy food consumption and risk of gastrointestinal-tract cancers: Findings from the China Kadoorie Biobank. Int. J. Epidemiol. 2021, 50, 199–211. [Google Scholar] [CrossRef]
- Chiu, S.; Bergeron, N.; Williams, P.T.; Bray, G.A.; Sutherland, B.; Krauss, R.M. Comparison of the DASH (Dietary Approaches to Stop Hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: A randomized controlled trial1–3. Am. J. Clin. Nutr. 2016, 103, 341–347. [Google Scholar] [CrossRef]
- Fung, T.T.; Chiuve, S.E.; McCullough, M.L.; Rexrode, K.M.; Logroscino, G.; Hu, F.B. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch. Intern. Med. 2008, 168, 713–720. [Google Scholar] [CrossRef]
- Ao, L.; Zhou, J.; Han, M.; Li, H.; Li, Y.; Pan, Y.; Chen, J.; Xie, X.; Jiang, Y.; Wei, J.; et al. The joint effects of physical activity and air pollution on type 2 diabetes in older adults. BMC Geriatr. 2022, 22, 472. [Google Scholar] [CrossRef]
- WS/T 428-2013; Criteria of Weight for Adults. Standard Press of China: Beijing, China, 2013.
- China Hypertension Prevention Guideline Revision Committee. Chinese Guidelines for the Prevention and Treatment of Hypertension (2018 Revision). Chin. J. Cardiol. 2019, 24, 24–56. [Google Scholar]
- Chinese Joint Committee on the Revision of Guidelines for Prevention and Treatment of Adult Dyslipidemia. Guidelines for prevention and treatment of dyslipidemia in Chinese adults (2016 version). Chin. Circ. J. 2016, 31, 937–953. [Google Scholar]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care 2017, 40, S11–S24. [Google Scholar] [CrossRef] [PubMed]
- Andersson, T.; Alfredsson, L.; Källberg, H.; Zdravkovic, S.; Ahlbom, A. Calculating measures of biological interaction. Eur. J. Epidemiol. 2005, 20, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; Ruggiero, E.; De Curtis, A.; Persichillo, M.; Tabolacci, C.; Facchiano, F.; Cerletti, C.; Donati, M.B.; et al. Chili Pepper Consumption and Mortality in Italian Adults. J. Am. Coll. Cardiol. 2019, 74, 3139–3149. [Google Scholar] [CrossRef] [PubMed]
- Chopan, M.; Littenberg, B. The Association of Hot Red Chili Pepper Consumption and Mortality: A Large Population-Based Cohort Study. PLoS ONE 2017, 12, e0169876. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Qi, L.; Yu, C.; Yang, L.; Guo, Y.; Chen, Y.; Bian, Z.; Sun, D.; Du, J.; Ge, P.; et al. Consumption of spicy foods and total and cause-specific mortality: Population based cohort study. BMJ 2015, 351, h3942. [Google Scholar] [CrossRef]
- Ma, Y.; He, F.J.; Sun, Q.; Yuan, C.; Kieneker, L.M.; Curhan, G.C.; MacGregor, G.A.; Bakker, S.J.L.; Campbell, N.R.C.; Wang, M.; et al. 24-Hour Urinary Sodium and Potassium Excretion and Cardiovascular Risk. N. Engl. J. Med. 2022, 386, 252–263. [Google Scholar] [CrossRef]
- Govindarajan, V.S.; Salzer, U.J. Capsicum—Production, technology, chemistry, and quality—Part II. Processed products, standards, world production and trade. Crit. Rev. Food Sci. Nutr. 1986, 23, 207–288. [Google Scholar] [CrossRef]
- Rosca, A.E.; Iesanu, M.I.; Zahiu, C.D.M.; Voiculescu, S.E.; Paslaru, A.C.; Zagrean, A.M. Capsaicin and Gut Microbiota in Health and Disease. Molecules 2020, 25, 5681. [Google Scholar] [CrossRef]
- Wang, S.; Cheng, L.; He, S.; Xie, D. Regional Pungency Degree in China and Its Correlation with Typical Climate Factors. J. Food Sci. 2019, 84, 31–37. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, M.; Li, C.; Wang, T.; Xu, Y.; Zhan, Z.; Dong, W.; Shen, Z.; Xu, M.; Lu, J.; et al. Dietary preferences and diabetic risk in China: A large-scale nationwide Internet data-based study. J. Diabetes 2020, 12, 270–278. [Google Scholar] [CrossRef]
- Azadbakht, L.; Mirmiran, P.; Esmaillzadeh, A.; Azizi, T.; Azizi, F. Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome. Diabetes Care 2005, 28, 2823–2831. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Cano, F.J.; Castell, M. Flavonoids, Inflammation and Immune System. Nutrients 2016, 8, 659. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.N. Associations of fats and carbohydrates with cardiovascular disease and mortality-PURE and simple? Lancet 2018, 391, 1676. [Google Scholar] [CrossRef] [PubMed]
- Castro-Barquero, S.; Ruiz-León, A.M.; Sierra-Pérez, M.; Estruch, R.; Casas, R. Dietary Strategies for Metabolic. Nutrients 2020, 12, 2983. [Google Scholar] [CrossRef] [PubMed]
- Hébert, J.R.; Shivappa, N.; Wirth, M.D.; Hussey, J.R.; Hurley, T.G. Perspective: The Dietary Inflammatory Index (DII)-Lessons Learned, Improvements Made, and Future Directions. Adv. Nutr. 2019, 10, 185–195. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 22,160) | Spicy Food Consumption | DASH Score | ||||
|---|---|---|---|---|---|---|---|
| No (n = 5322) | Yes (n = 16,838) | p | Low (n = 6755) | High (n = 15,405) | p | ||
| Age (years) | 51.4 ± 11.7 | 54.7 ± 12.2 | 50.4 ± 11.4 | <0.01 | 52.6 ± 11.5 | 50.9 ± 11.8 | 0.03 |
| Age group (years) | <0.01 | <0.01 | |||||
| <60 | 16,198 (73.1%) | 3299 (62.0%) | 12,899 (76.6%) | 4741 (70.2%) | 11,457 (74.4%) | ||
| ≥60 | 5962 (26.9%) | 2023 (38.0%) | 3939 (23.4%) | 2014 (29.8%) | 3948 (25.6%) | ||
| Gender | <0.01 | <0.01 | |||||
| Male | 10,371 (46.8%) | 2354 (44.2%) | 8017 (47.6%) | 3811 (56.4%) | 6560 (42.6%) | ||
| Female | 11,789 (53.2%) | 2968 (55.8%) | 8821 (52.4%) | 2944 (43.6%) | 8845 (57.4%) | ||
| Education level | <0.01 | <0.01 | |||||
| Primary school and below | 7197 (32.5%) | 2303 (43.3%) | 4894 (29.1%) | 3194 (47.3%) | 4003 (26.0%) | ||
| Middle school | 7154 (32.3%) | 1609 (30.2%) | 5545 (32.9%) | 2062 (30.5%) | 5092 (33.1%) | ||
| High school | 4108 (18.5%) | 735 (13.8%) | 3373 (20.0%) | 818 (12.1%) | 3290 (21.4%) | ||
| College or university and above | 3701 (16.7%) | 675 (12.7%) | 3026 (18.0%) | 681 (10.1%) | 3020 (19.6%) | ||
| Smoking | <0.01 | <0.01 | |||||
| No | 16,220 (73.2%) | 4325 (81.3%) | 11,895 (70.6%) | 4513 (66.8%) | 11,707 (76.0%) | ||
| Yes | 5940 (26.8%) | 997 (18.7%) | 4943 (29.4%) | 2242 (33.2%) | 3698 (24.0%) | ||
| Drinking | <0.01 | <0.01 | |||||
| No | 10,115 (45.6%) | 3360 (63.1%) | 6755 (40.1%) | 3320 (49.1%) | 6795 (44.1%) | ||
| Yes | 12,045 (54.4%) | 1962 (36.9%) | 10,083 (59.9%) | 3435 (50.9%) | 8610 (55.9%) | ||
| Physical activity (METs h/day) | <0.01 | <0.01 | |||||
| <21.94 | 7260 (32.8%) | 2166 (40.7%) | 5094 (30.3%) | 2170 (32.1%) | 5090 (33.0%) | ||
| 21.94–35.55 | 7459 (33.7%) | 1544 (29.0%) | 5915 (35.1%) | 2014 (29.8%) | 5445 (35.3%) | ||
| >35.55 | 7441 (33.6%) | 1612 (30.3%) | 5829 (34.6%) | 2571 (38.1%) | 4870 (31.6%) | ||
| BMI (Body mass index, kg/m2) | <0.01 | <0.01 | |||||
| 18.5 ≤ BMI< 24.0 | 9476 (42.8%) | 2371 (44.6%) | 7105 (42.2%) | 2649 (39.2%) | 6827 (44.3%) | ||
| BMI < 18.5 | 338 (1.53%) | 87 (1.63%) | 251 (1.49%) | 93 (1.38%) | 245 (1.59%) | ||
| 24.0 ≤ BMI < 28 | 9107 (41.1%) | 2164 (40.7%) | 6943 (41.2%) | 2854 (42.3%) | 6253 (40.6%) | ||
| BMI ≥ 28 | 3239 (14.6%) | 700 (13.2%) | 2539 (15.1%) | 1159 (17.2%) | 2080 (13.5%) | ||
| Hypertension | <0.01 | <0.01 | |||||
| No | 14,422 (65.1%) | 3226 (60.6%) | 11,196 (66.5%) | 3979 (58.9%) | 10,443 (67.8%) | ||
| Yes | 7738 (34.9%) | 2096 (39.4%) | 5642 (33.5%) | 2776 (41.1%) | 4962 (32.2%) | ||
| Dyslipidemia | 0.02 | <0.01 | |||||
| No | 15,111 (68.2%) | 3697 (69.5%) | 11,414 (67.8%) | 4470 (66.2%) | 10,641 (69.1%) | ||
| Yes | 7049 (31.8%) | 1625 (30.5%) | 5424 (32.2%) | 2285 (33.8%) | 4764 (30.9%) | ||
| Diabetes | <0.01 | <0.01 | |||||
| No | 19,577 (88.3%) | 4613 (86.7%) | 14,964 (88.9%) | 5900 (87.3%) | 13,677 (88.8%) | ||
| Yes | 2583 (11.7%) | 709 (13.3%) | 1874 (11.1%) | 855 (12.7%) | 1728 (11.2%) | ||
| DASH score | <0.01 | - | |||||
| Low | 6755 (30.5%) | 2065 (38.8%) | 4690 (27.9%) | - | - | ||
| High | 15,405 (69.5%) | 3257 (61.2%) | 12,148 (72.1%) | - | - | ||
| Spicy food consumption | - | <0.01 | |||||
| No | 5322 (24.0%) | - | - | 2065 (30.6%) | 3257 (21.1%) | ||
| Yes | 16,838 (76.0%) | - | - | 4690 (69.4%) | 12,148 (78.9%) | ||
| Family history of stroke-related diseases | <0.01 | <0.01 | |||||
| No | 11,834 (53.4%) | 3169 (59.5%) | 8665 (51.5%) | 3898 (57.7%) | 7936 (51.5%) | ||
| Yes | 10,326 (46.6%) | 2153 (40.5%) | 8173 (48.5%) | 2857 (42.3%) | 7469 (48.5%) | ||
| Variables | Number of Events/n | Incidence Density (1/100,000 Person-Years) | Crude Model | Model 1 | ||
|---|---|---|---|---|---|---|
| HR (95%CI) | p | HR (95%CI) | p | |||
| Total population | 312 */22,160 | 371.68 | ||||
| Spicy food consumption | ||||||
| No | 103/5322 | 515.68 | 1.00 | 1.00 | ||
| Yes | 209/16,838 | 326.72 | 0.64 (0.50, 0.80) | < 0.01 | 1.00 (0.78, 1.28) | 1.00 |
| DASH score | ||||||
| Low | 117/6755 | 459.40 | 1.00 | 1.00 | ||
| High | 195/15,405 | 333.48 | 0.73 (0.58, 0.92) | < 0.01 | 0.91 (0.72, 1.15) | 0.43 |
| Males a | 172/10,371 | 440.64 | ||||
| Spicy food consumption | ||||||
| No | 58/2354 | 664.64 | 1.00 | 1.00 | ||
| Yes | 114/8017 | 376.14 | 0.57 (0.41, 0.78) | < 0.01 | 0.90 (0.64, 1.25) | 0.52 |
| DASH score | ||||||
| Low | 72/3811 | 503.49 | 1.00 | 1.00 | ||
| High | 100/6560 | 404.30 | 0.81 (0.60, 1.09) | 0.16 | 0.89 (0.65, 1.23) | 0.48 |
| Females a | 140/11,789 | 311.75 | ||||
| Spicy food consumption | ||||||
| No | 45/2968 | 400.11 | 1.00 | 1.00 | ||
| Yes | 95/8821 | 282.22 | 0.71 (0.50, 1.01) | 0.05 | 1.13 (0.78, 1.63) | 0.52 |
| DASH score | ||||||
| Low | 45/2944 | 402.94 | 1.00 | 1.00 | ||
| High | 95/8845 | 281.56 | 0.70 (0.49, 1.00) | 0.05 | 0.95 (0.65, 1.37) | 0.78 |
| Age < 60 years b | 82/16,198 | 132.77 | ||||
| Spicy food consumption | ||||||
| No | 25/3299 | 199.84 | 1.00 | 1.00 | ||
| Yes | 57/12,899 | 115.73 | 0.58 (0.36, 0.93) | 0.02 | 0.67 (0.41, 1.09) | 0.11 |
| DASH score | ||||||
| Low | 34/4741 | 188.71 | 1.00 | 1.00 | ||
| High | 48/11,457 | 109.73 | 0.58 (0.38, 0.90) | 0.02 | 0.78 (0.49, 1.25) | 0.31 |
| Age ≥ 60 years b | 230/5962 | 1036.95 | ||||
| Spicy food consumption | ||||||
| No | 78/2023 | 1045.10 | 1.00 | 1.00 | ||
| Yes | 152/3939 | 1032.82 | 0.99 (0.76, 1.30) | 0.95 | 1.127 (0.849, 1.496) | 0.41 |
| DASH score | ||||||
| Low | 83/2014 | 1113.89 | 1.00 | 1.00 | ||
| High | 147/3948 | 998.03 | 0.90 (0.69, 1.18) | 0.44 | 0.96 (0.73, 1.27) | 0.79 |
| Variables | Number of Events/n | Incidence Density (1/100,000 Person-Years) | Crude Model | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|---|
| HR (95%CI) | p | HR (95%CI) | p | HR (95%CI) | p | |||
| Total population | 312/22,160 | 371.68 | ||||||
| Interaction * | 2.02 (1.24, 3.30) | <0.01 | ||||||
| Not spicy/Low DASH score | 57/2065 | 742.86 | 1.00 | 1.00 | - | - | ||
| Not spicy/High DASH score | 46/3257 | 373.97 | 0.51 (0.34, 0.75) | <0.01 | 0.58 (0.39, 0.86) | 0.01 | - | - |
| Spicy/Low DASH score | 60/4690 | 337.17 | 0.46 (0.32, 0.65) | <0.01 | 0.67 (0.46, 0.97) | 0.03 | - | - |
| Spicy/High DASH score | 149/12,148 | 322.69 | 0.44 (0.32, 0.59) | <0.01 | 0.78 (0.57, 1.08) | 0.14 | - | - |
| Males a | 172/10,371 | 440.64 | ||||||
| Interaction * | 1.99 (1.03, 3.85) | 0.04 | ||||||
| Not spicy/Low DASH score | 35/1088 | 874.71 | 1.00 | 1.00 | - | - | ||
| Not spicy/High DASH score | 23/1266 | 486.75 | 0.56 (0.33, 0.95) | 0.03 | 0.57 (0.33, 0.98) | 0.04 | - | - |
| Spicy/Low DASH score | 37/2723 | 359.26 | 0.41 (0.26, 0.66) | <0.01 | 0.62 (0.39, 1.01) | 0.05 | - | - |
| Spicy/High DASH score | 77/5294 | 384.83 | 0.44 (0.30, 0.66) | <0.01 | 0.71 (0.46, 1.09) | 0.11 | - | - |
| Females a | 140/11,789 | 311.75 | ||||||
| Interaction * | 1.90 (0.89, 4.02) | 0.10 | ||||||
| Not spicy/Low DASH score | 22/977 | 599.17 | 1.00 | 1.00 | - | - | ||
| Not spicy/High DASH score | 23/1991 | 303.62 | 0.51 (0.28, 0.91) | 0.02 | 0.64 (0.35, 1.15) | 0.14 | - | - |
| Spicy/Low DASH score | 23/1967 | 306.83 | 0.51 (0.29, 0.92) | 0.03 | 0.76 (0.42, 1.37) | 0.35 | - | - |
| Spicy/High DASH score | 72/6854 | 275.17 | 0.46 (0.29, 0.74) | <0.01 | 0.91 (0.55, 1.51) | 0.72 | - | - |
| Age < 60 years b | 82/16,198 | 132.77 | ||||||
| Interaction * | 2.38 (0.88, 6.41) | 0.09 | ||||||
| Not spicy/Low DASH score | 16/1222 | 347.72 | - | - | ||||
| Not spicy/High DASH score | 9/2077 | 113.80 | 0.33 (0.15, 0.74) | 0.01 | 0.43 (0.19, 1.00) | 0.05 | - | - |
| Spicy/Low DASH score | 18/3519 | 134.18 | 0.39 (0.20, 0.76) | 0.01 | 0.43 (0.22, 0.86) | 0.02 | - | - |
| Spicy/High DASH score | 39/9380 | 108.83 | 0.32 (0.18, 0.56) | <0.01 | 0.44 (0.24, 0.83) | 0.01 | - | - |
| Age ≥ 60 years b | 230/5962 | 1036.95 | ||||||
| Interaction * | 1.89 (1.07, 3.34) | 0.03 | ||||||
| Not spicy/Low DASH score | 41/843 | 1334.78 | 1.00 | 1.00 | - | - | ||
| Not spicy/High DASH score | 37/1180 | 842.49 | 0.63 (0.41, 0.99) | 0.04 | 0.65 (0.41, 1.02) | 0.06 | - | - |
| Spicy/Low DASH score | 42/1171 | 958.98 | 0.72 (0.47, 1.11) | 0.14 | 0.77 (0.50, 1.20) | 0.25 | - | - |
| Spicy/High DASH score | 110/2768 | 1064.10 | 0.80 (0.56, 1.15) | 0.23 | 0.95 (0.65, 1.38) | 0.78 | - | - |
| RERI (95%CI) | AP (95%CI) | S (95%CI) | |
|---|---|---|---|
| Total population | 0.54 (0.24, 0.83) | 0.68 (0.23, 1.14) | 0.29 (0.12, 0.70) |
| Males | 0.52 (0.13, 0.90) | 0.73 (0.08, 1.38) | 0.36 (0.17, 0.78) |
| Females | 0.52 (0.02, 1.02) | 0.57 (−0.08, 1.22) | 0.14 (0.002, 12.65) |
| Age < 60 years | 0.58 (0.15, 1.00) | 1.33 (−0.11, 2.77) | 0.50 (0.34, 0.74) |
| Age ≥ 60 years | 0.51 (0.11, 0.90) | 0.54 (0.06, 1.02) | 0.10 (0.0003, 31.44) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, L.; Tang, W.; Wu, X.; Zhang, R.; Ding, R.; Liu, X.; Tang, X.; Wu, J.; Ding, X. Eating Spicy Food, Dietary Approaches to Stop Hypertension (DASH) Score, and Their Interaction on Incident Stroke in Southwestern Chinese Aged 30–79: A Prospective Cohort Study. Nutrients 2023, 15, 1222. https://doi.org/10.3390/nu15051222
Chen L, Tang W, Wu X, Zhang R, Ding R, Liu X, Tang X, Wu J, Ding X. Eating Spicy Food, Dietary Approaches to Stop Hypertension (DASH) Score, and Their Interaction on Incident Stroke in Southwestern Chinese Aged 30–79: A Prospective Cohort Study. Nutrients. 2023; 15(5):1222. https://doi.org/10.3390/nu15051222
Chicago/Turabian StyleChen, Liling, Wenge Tang, Xiaomin Wu, Rui Zhang, Rui Ding, Xin Liu, Xiaojun Tang, Jing Wu, and Xianbin Ding. 2023. "Eating Spicy Food, Dietary Approaches to Stop Hypertension (DASH) Score, and Their Interaction on Incident Stroke in Southwestern Chinese Aged 30–79: A Prospective Cohort Study" Nutrients 15, no. 5: 1222. https://doi.org/10.3390/nu15051222
APA StyleChen, L., Tang, W., Wu, X., Zhang, R., Ding, R., Liu, X., Tang, X., Wu, J., & Ding, X. (2023). Eating Spicy Food, Dietary Approaches to Stop Hypertension (DASH) Score, and Their Interaction on Incident Stroke in Southwestern Chinese Aged 30–79: A Prospective Cohort Study. Nutrients, 15(5), 1222. https://doi.org/10.3390/nu15051222






