Treatment Effects of Natural Products on Inflammatory Bowel Disease In Vivo and Their Mechanisms: Based on Animal Experiments
Abstract
1. Introduction
2. Pathogenesis of IBD and Current Therapeutic Agents
2.1. The Pathogenesis of IBD
2.1.1. Genetic Factors
2.1.2. Environmental Factors
2.1.3. Dietary Factors
2.1.4. Other Factors
2.2. IBD Treatment Drugs and Therapeutic Methods
2.2.1. Amino Salicylic Acid Agents
2.2.2. Corticosteroids
2.2.3. Immunomodulators
2.2.4. Biological Agents
2.2.5. Stem Cell Transplantation
2.2.6. Fecal Microbiota Transplantation (FMT)
2.2.7. Helminth Therapy
2.2.8. Surgery
3. NPs with IBD Therapeutic Activity
3.1. Flavonoids
3.2. Terpenoids
3.3. Glycosides
3.4. Polyphenols
3.5. Quinones
3.6. Alkaloids
3.7. Coumarins
3.8. Polysaccharides
3.9. Natural Proteins and Active Peptides
4. Major Pathways of Action of NPs in the Treatment of IBD
4.1. Improvement of IBD Pathology Symptoms
4.2. Regulation of Intestinal Microbiota
4.3. Protects the Intestinal Barrier Function
4.4. Reduces Inflammatory Response
4.5. Improves Oxidative Stress
4.6. Regulation of Immunity
4.7. Regulation of Key Signaling Pathways
4.7.1. NF-κB Signaling Pathway
4.7.2. MAPK Signaling Pathway
4.7.3. JAK/STAT Signaling Pathway
4.7.4. PI3K and TLRs
4.7.5. NLRP3 Inflammatory Vesicles
4.7.6. PPARγ
5. Conclusions and Prospect
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ramos, G.P.; Papadakis, K.A. Mechanisms of Disease: Inflammatory Bowel Diseases. Mayo Clin. Proc. 2019, 94, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Aniwan, S.; Park, S.H.; Loftus, E.V., Jr. Epidemiology, Natural History, and Risk Stratification of Crohn’s Disease. Gastroenterol. Clin. 2017, 46, 463–480. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef] [PubMed]
- Mirkov, M.U.; Verstockt, B.; Cleynen, I. Genetics of inflammatory bowel disease: Beyond NOD2. Lancet Gastroenterol. Hepatol. 2017, 2, 224–234. [Google Scholar] [CrossRef]
- Shouval, D.S.; Rufo, P.A. The Role of Environmental Factors in the Pathogenesis of Inflammatory Bowel Diseases: A Review. JAMA Pediatr. 2017, 171, 999–1005. [Google Scholar] [CrossRef]
- Nishida, A.; Inoue, R.; Inatomi, O.; Bamba, S.; Naito, Y.; Andoh, A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin. J. Gastroenterol. 2018, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xavier, R.J.; Podolsky, D.K. Unravelling the pathogenesis of inflammatory bowel disease. Nature 2007, 448, 427–434. [Google Scholar] [CrossRef]
- Cader, M.Z.; Kaser, A. Recent advances in inflammatory bowel disease: Mucosal immune cells in intestinal inflammation. Gut 2013, 62, 1653. [Google Scholar] [CrossRef]
- Abraham, B.P.; Ahmed, T.; Ali, T. Inflammatory Bowel Disease: Pathophysiology and Current Therapeutic Approaches. In Gastrointestinal Pharmacology; Greenwood-Van Meerveld, B., Ed.; Springer International Publishing: Cham, Switzerland, 2017; Volume 239, pp. 115–146. [Google Scholar]
- Bai, R.; Jie, X.; Yao, C.; Xie, Y. Discovery of small-molecule candidates against inflammatory bowel disease. Eur. J. Med. Chem. 2020, 185, 111805. [Google Scholar] [CrossRef]
- Volk, N.; Siegel, C.A. Defining Failure of Medical Therapy for Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2019, 25, 74–77. [Google Scholar] [CrossRef]
- Kane, S.; Huo, D.; Aikens, J.; Hanauer, S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. Am. J. Med. 2003, 114, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Kornbluth, A.; Sachar, D.B. Ulcerative Colitis Practice Guidelines in Adults: American College of Gastroenterology, Practice Parameters Committee. Am. J. Gastroenterol. 2010, 105, 501–523. [Google Scholar]
- Ribeiro, D.; Proenca, C.; Rocha, S.; Lima, J.L.F.C.; Carvalho, F.; Fernandes, E.; Freitas, M. Immunomodulatory Effects of Flavonoids in the Prophylaxis and Treatment of Inflammatory Bowel Diseases: A Comprehensive Review. Curr. Med. Chem. 2018, 25, 3374–3412. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; Liu, Z.; Zhong, Z.; Wang, L.; Zhuo, X.; Li, J.; Jiang, X.; Ye, X.-Y.; Xie, T.; Bai, R. Natural terpenoids with anti-inflammatory activities: Potential leads for anti-inflammatory drug discovery. Bioorg. Chem. 2022, 124, 105817. [Google Scholar] [CrossRef]
- Dong, J.-Y.; Xia, K.-J.; Liang, W.; Liu, L.-L.; Yang, F.; Fang, X.-S.; Xiong, Y.-J.; Wang, L.; Zhou, Z.-J.; Li, C.-Y.; et al. Ginsenoside Rb1 alleviates colitis in mice via activation of endoplasmic reticulum-resident E3 ubiquitin ligase Hrd1 signaling pathway. Acta Pharmacol. Sin. 2021, 42, 1461–1471. [Google Scholar] [PubMed]
- Caban, M.; Lewandowska, U. Polyphenols and the potential mechanisms of their therapeutic benefits against inflammatory bowel diseases. J. Funct. Foods 2022, 95, 105181. [Google Scholar] [CrossRef]
- Hua, Y.; Liu, R.; Lu, M.; Guan, X.; Zhuang, S.; Tian, Y.; Zhang, Z.; Cui, L. Juglone regulates gut microbiota and Th17/Treg balance in DSS-induced ulcerative colitis. Int. Immunopharmacol. 2021, 97, 107683. [Google Scholar] [CrossRef]
- Li, C.; Wang, J.; Ma, R.; Li, L.; Wu, W.; Cai, D.; Lu, Q. Natural-derived alkaloids exhibit great potential in the treatment of ulcerative colitis. Pharmacol. Res. 2022, 175, 105972. [Google Scholar] [CrossRef]
- Di Stasi, L.C. Coumarin Derivatives in Inflammatory Bowel Disease. Molecules 2021, 26, 422. [Google Scholar] [CrossRef]
- Yuan, D.; Li, C.; Huang, Q.; Fu, X.; Dong, H. Current advances in the anti-inflammatory effects and mechanisms of natural polysaccharides. Crit. Rev. Food Sci. Nutr. 2022. [Google Scholar] [CrossRef]
- Ma, Y.; Yan, W.; Ding, S.; Fei, Y.; Liu, G.; Fang, J. Effects of Bioactive Peptide on Inflammatory Bowel Disease, Focus on Signal Transduction and Intestinal Microbiota. Curr. Pharm. Des. 2018, 24, 2782–2788. [Google Scholar] [CrossRef]
- Yeshi, K.; Ruscher, R.; Hunter, L.; Daly, N.L.; Loukas, A.; Wangchuk, P. Revisiting Inflammatory Bowel Disease: Pathology, Treatments, Challenges and Emerging Therapeutics Including Drug Leads from Natural Products. J. Clin. Med. 2020, 9, 1273. [Google Scholar] [CrossRef]
- Khor, B.; Gardet, A.; Xavier, R.J. Genetics and pathogenesis of inflammatory bowel disease. Nature 2011, 474, 307–317. [Google Scholar] [CrossRef]
- Jostins, L.; Ripke, S.; Weersma, R.K.; Duerr, R.H.; McGovern, D.P.; Hui, K.Y.; Lee, J.C.; Philip Schumm, L.; Sharma, Y.; Anderson, C.A.; et al. Host–microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 2012, 491, 119–124. [Google Scholar] [CrossRef]
- Park, S.C.; Jeen, Y.T. Genetic Studies of Inflammatory Bowel Disease-Focusing on Asian Patients. Cells 2019, 8, 404. [Google Scholar] [CrossRef]
- Anderson, C.A.; Boucher, G.; Lees, C.W.; Franke, A.; D’Amato, M.; Taylor, K.D.; Lee, J.C.; Goyette, P.; Imielinski, M.; Latiano, A.; et al. Meta-analysis identifies 29 additional ulcerative colitis risk loci, increasing the number of confirmed associations to 47. Nat. Genet. 2011, 43, 246–252. [Google Scholar] [CrossRef]
- Franke, A.; McGovern, D.P.B.; Barrett, J.C.; Wang, K.; Radford-Smith, G.L.; Ahmad, T.; Lees, C.W.; Balschun, T.; Lee, J.; Roberts, R.; et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat. Genet. 2010, 42, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Kakuta, Y.; Naito, T.; Kinouchi, Y.; Masamune, A. Current Status and Future Prospects of Inflammatory Bowel Disease Genetics. Digestion 2022, 104, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Huang, E.S.; Ananthakrishnan, A.N.; Higuchi, L.; Richter, J.M.; Fuchs, C.S.; Chan, A.T. Geographical variation and incidence of inflammatory bowel disease among US women. Gut 2012, 61, 1686. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Goulart, R.d.A.; Gasparini, R.G. Associations between inflammatory bowel diseases and vitamin D. Crit. Rev. Food Sci. Nutr. 2019, 59, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Maeda, S.S.; Saraiva, G.L.; Hayashi, L.F.; Cendoroglo, M.S.; Ramos, L.R.; Corrêa, M.d.P.; Henrique de Mesquita, C.; Lazaretti-Castro, M. Seasonal variation in the serum 25-hydroxyvitamin D levels of young and elderly active and inactive adults in São Paulo, Brazil. Derm.-Endocrinol. 2013, 5, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Timm, S.; Svanes, C.; Janson, C.; Sigsgaard, T.; Johannessen, A.; Gislason, T.; Jogi, R.; Omenaas, E.; Forsberg, B.; Torén, K.; et al. Place of upbringing in early childhood as related to inflammatory bowel diseases in adulthood: A population-based cohort study in Northern Europe. Eur. J. Epidemiol. 2014, 29, 429–437. [Google Scholar] [CrossRef] [PubMed]
- van der Sloot, K.W.J.; Weersma, R.K.; Alizadeh, B.Z.; Dijkstra, G. Identification of Environmental Risk Factors Associated with the Development of Inflammatory Bowel Disease. J. Crohn’s Colitis 2020, 14, 1662–1671. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Bernstein, C.N. Environmental risk factors for inflammatory bowel disease. United Eur. Gastroenterol. J. 2022, 10, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Adolph, T.E.; Zhang, J. Diet fuelling inflammatory bowel diseases: Preclinical and clinical concepts. Gut 2022, 71, 2574. [Google Scholar] [CrossRef]
- Khalili, H.; Chan, S.S.M.; Lochhead, P.; Ananthakrishnan, A.N.; Hart, A.R.; Chan, A.T. The role of diet in the aetiopathogenesis of inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 525–535. [Google Scholar] [CrossRef]
- Sasson, A.N.; Ananthakrishnan, A.N.; Raman, M. Diet in Treatment of Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2021, 19, 425–435.e3. [Google Scholar] [CrossRef]
- Godala, M.; Gaszyńska, E.; Zatorski, H.; Małecka-Wojciesko, E. Dietary Interventions in Inflammatory Bowel Disease. Nutrients 2022, 14, 4261. [Google Scholar] [CrossRef]
- Gao, Q.; Bi, P.; Luo, D.; Guan, Y.; Zeng, W.; Xiang, H.; Mi, Q.; Yang, G.; Li, X.; Yang, B. Nicotine-induced autophagy via AMPK/mTOR pathway exerts protective effect in colitis mouse model. Chem.-Biol. Interact. 2020, 317, 108943. [Google Scholar] [CrossRef]
- Qazi, T.; Farraye, F.A. Sleep and Inflammatory Bowel Disease: An Important Bi-Directional Relationship. Inflamm. Bowel Dis. 2019, 25, 843–852. [Google Scholar] [CrossRef]
- Peppas, S.; Pansieri, C.; Piovani, D.; Danese, S.; Peyrin-Biroulet, L.; Tsantes, A.G.; Brunetta, E.; Tsantes, A.E.; Bonovas, S. The Brain-Gut Axis: Psychological Functioning and Inflammatory Bowel Diseases. J. Clin. Med. 2021, 10, 377. [Google Scholar] [CrossRef] [PubMed]
- Hashash, J.G.; Binion, D.G. Exercise and Inflammatory Bowel Disease: Insights into Etiopathogenesis and Modification of Clinical Course. Gastroenterol. Clin. North Am. 2017, 46, 895–905. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Örtqvist, A.K.; Cao, Y.; Simon, T.G.; Roelstraete, B.; Song, M.; Joshi, A.D.; Staller, K.; Chan, A.T.; Khalili, H.; et al. Antibiotic use and the development of inflammatory bowel disease: A national case-control study in Sweden. Lancet Gastroenterol. Hepatol. 2020, 5, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Sokol, H. Antibiotics: A trigger for inflammatory bowel disease? Lancet Gastroenterol. Hepatol. 2020, 5, 956–957. [Google Scholar] [CrossRef]
- Chung, W.-S.; Chung, S.; Hsu, C.-Y.; Lin, C.-L. Risk of Inflammatory Bowel Disease Following Appendectomy in Adulthood. Front. Med. 2021, 8, 661752. [Google Scholar] [CrossRef]
- Bjarnason, I.; Macpherson, A.J. Delivery, safety and efficacy of 5-aminosalicylate preparations. Inflammopharmacology 1993, 2, 277–287. [Google Scholar] [CrossRef]
- Dorrington, A.M.; Selinger, C.P.; Parkes, G.C.; Smith, M.; Pollok, R.C.; Raine, T. The Historical Role and Contemporary Use of Corticosteroids in Inflammatory Bowel Disease. J. Crohn’s Colitis 2020, 14, 1316–1329. [Google Scholar] [CrossRef]
- Dubois-Camacho, K.; Ottum, P.A.; Franco-Muñoz, D.; De la Fuente, M.; Torres-Riquelme, A.; Díaz-Jiménez, D.; Olivares-Morales, M.; Astudillo, G.; Quera, R.; Hermoso, M.A. Glucocorticosteroid therapy in inflammatory bowel diseases: From clinical practice to molecular biology. World J. Gastroenterol. 2017, 23, 6628. [Google Scholar] [CrossRef]
- Kim, K.-U.; Kim, J.; Kim, W.-H.; Min, H.; Choi, C.H. Treatments of inflammatory bowel disease toward personalized medicine. Arch. Pharmacal Res. 2021, 44, 293–309. [Google Scholar] [CrossRef]
- Sattler, L.; Hanauer, S.B.; Malter, L. Immunomodulatory Agents for Treatment of Patients with Inflammatory Bowel Disease (Review safety of anti-TNF, Anti-Integrin, Anti IL-12/23, JAK Inhibition, Sphingosine 1-Phosphate Receptor Modulator, Azathioprine/6-MP and Methotrexate). Curr. Gastroenterol. Rep. 2021, 23, 30. [Google Scholar] [CrossRef]
- Cai, Z.; Wang, S.; Li, J. Treatment of Inflammatory Bowel Disease: A Comprehensive Review. Front. Med. 2021, 8, 765474. [Google Scholar] [CrossRef]
- Tominaga, K.; Sugaya, T.; Tanaka, T.; Kanazawa, M.; Iijima, M.; Irisawa, A. Thiopurines: Recent Topics and Their Role in the Treatment of Inflammatory Bowel Diseases. Front. Pharmacol. 2021, 11, 582291. [Google Scholar] [CrossRef]
- Herfarth, H.H. Methotrexate for Inflammatory Bowel Diseases—New Developments. Dig. Dis. 2016, 34, 140–146. [Google Scholar] [CrossRef]
- Tedesco, D.; Haragsim, L. Cyclosporine: A Review. J. Transplant. 2012, 2012, 230386. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Michalowski, C.B.; Beloqui, A. Oral Delivery of Biologics in Inflammatory Bowel Disease Treatment. Front. Bioeng. Biotechnol. 2021, 9, 675194. [Google Scholar] [CrossRef]
- Queiroz, N.S.F.; Regueiro, M. Safety considerations with biologics and new inflammatory bowel disease therapies. Curr. Opin. Gastroenterol. 2020, 36, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Rakowsky, S.; Papamichael, K.; Cheifetz, A.S. Choosing the right biologic for complications of inflammatory bowel disease. Expert Rev. Gastroenterol. Hepatol. 2022, 16, 235–249. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.-M.; Yuan, S.; Meng, H.; Hou, X.-T.; Li, J.; Xue, J.-C.; Li, Y.; Wang, Q.; Nan, J.-X.; Jin, X.-J.; et al. Stem Cell-Based Therapies for Inflammatory Bowel Disease. Int. J. Mol. Sci. 2022, 23, 8494. [Google Scholar] [CrossRef] [PubMed]
- Kotlarz, D.; Beier, R.; Murugan, D.; Diestelhorst, J.; Jensen, O.; Boztug, K.; Pfeifer, D.; Kreipe, H.; Pfister, E.D.; Baumann, U.; et al. Loss of Interleukin-10 Signaling and Infantile Inflammatory Bowel Disease: Implications for Diagnosis and Therapy. Gastroenterology 2012, 143, 347–355. [Google Scholar] [CrossRef]
- Pan, X.-H.; Li, Q.-Q.; Zhu, X.-Q.; Li, Z.-A.; Cai, X.-M.; Pang, R.-Q.; Ruan, G.-P. Mechanism and therapeutic effect of umbilical cord mesenchymal stem cells in inflammatory bowel disease. Sci. Rep. 2019, 9, 17646. [Google Scholar] [CrossRef]
- Wei, H.; Liu, X.; Ouyang, C.; Zhang, J.; Chen, S.; Lu, F.; Chen, L. Complications Following Stem Cell Therapy in Inflammatory Bowel Disease. Curr. Stem Cell Res. Ther. 2017, 12, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Lalu, M.M.; McIntyre, L.; Pugliese, C.; Fergusson, D.; Winston, B.W.; Marshall, J.C.; Granton, J.; Stewart, D.J. Safety of Cell Therapy with Mesenchymal Stromal Cells (SafeCell): A Systematic Review and Meta-Analysis of Clinical Trials. PLoS ONE 2012, 7, e47559. [Google Scholar] [CrossRef] [PubMed]
- Gough, E.; Shaikh, H.; Manges, A.R. Systematic Review of Intestinal Microbiota Transplantation (Fecal Bacteriotherapy) for Recurrent Clostridium difficile Infection. Clin. Infect. Dis. 2011, 53, 994–1002. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Harstall, C.; Louie, T.; Veldhuyzen van Zanten, S.; Dieleman, L.A. Systematic review: Faecal transplantation for the treatment of Clostridium difficile-associated disease. Aliment. Pharmacol. Ther. 2012, 35, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Colman, R.J.; Rubin, D.T. Fecal microbiota transplantation as therapy for inflammatory bowel disease: A systematic review and meta-analysis. J. Crohn’s Colitis 2014, 8, 1569–1581. [Google Scholar] [CrossRef]
- Weingarden, A.R.; Vaughn, B.P. Intestinal microbiota, fecal microbiota transplantation, and inflammatory bowel disease. Gut Microbes 2017, 8, 238–252. [Google Scholar] [CrossRef]
- Büning, J.; Homann, N.; von Smolinski, D.; Borcherding, F.; Noack, F.; Stolte, M.; Kohl, M.; Lehnert, H.; Ludwig, D. Helminths as governors of inflammatory bowel disease. Gut 2008, 57, 1182. [Google Scholar] [CrossRef]
- Summers, R.W.; Elliott, D.E.; Qadir, K.; Urban, J.F.; Thompson, R.; Weinstock, J.V. Trichuris suis seems to be safe and possibly effective in the treatment of inflammatory bowel disease. Am. J. Gastroenterol. 2003, 98, 2034–2041. [Google Scholar] [CrossRef]
- Hunter, M.M.; McKay, D.M. Helminths as therapeutic agents for inflammatory bowel disease. Aliment. Pharmacol. Ther. 2004, 19, 167–177. [Google Scholar] [CrossRef]
- Bemelman, W.A.; S-ECCO Collaborators. Evolving Role of IBD Surgery. J. Crohn’s Colitis 2018, 12, 1005–1007. [Google Scholar] [CrossRef]
- Kühn, F.; Klar, E. Surgical Principles in the Treatment of Ulcerative Colitis. Visc. Med. 2015, 31, 246–250. [Google Scholar] [CrossRef] [PubMed]
- Salaritabar, A.; Darvishi, B.; Hadjiakhoondi, F.; Manayi, A.; Sureda, A.; Nabavi, S.F.; Fitzpatrick, L.R.; Nabavi, S.M.; Bishayee, A. Therapeutic potential of flavonoids in inflammatory bowel disease: A comprehensive review. World J. Gastroenterol. 2017, 23, 5097–5114. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Gao, M.; Kang, G.; Huang, H. The Potential Role of Phytonutrients Flavonoids Influencing Gut Microbiota in the Prophylaxis and Treatment of Inflammatory Bowel Disease. Front. Nutr. 2021, 8, 798038. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Li, Y.; Liu, M.; Yu, H.; Chen, Q.; Chen, Y.; Ruan, J.; Ding, Z.; Zhang, Y.; Wang, T. Citrus aurantium L. and Its Flavonoids Regulate TNBS-Induced Inflammatory Bowel Disease through Anti-Inflammation and Suppressing Isolated Jejunum Contraction. Int. J. Mol. Sci. 2018, 19, 3057. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Yan, Y.; Wan, P.; Chen, D.; Ding, Y.; Ran, L.; Mi, J.; Lu, L.; Zhang, Z.; Li, X.; et al. Gut microbiota modulation and anti-inflammatory properties of anthocyanins from the fruits of Lycium ruthenicum Murray in dextran sodium sulfate-induced colitis in mice. Free Radic. Biol. Med. 2019, 136, 96–108. [Google Scholar] [CrossRef]
- Kim, S.-E.; Kawaguchi, K.; Hayashi, H.; Furusho, K.; Maruyama, M. Remission Effects of Dietary Soybean Isoflavones on DSS-Induced Murine Colitis and an LPS-Activated Macrophage Cell Line. Nutrients 2019, 11, 1746. [Google Scholar] [CrossRef]
- Li, M.; Weigmann, B. A Novel Pathway of Flavonoids Protecting against Inflammatory Bowel Disease: Modulating Enteroendocrine System. Metabolites 2022, 12, 31. [Google Scholar] [CrossRef]
- Sangaraju, R.; Nalban, N.; Alavala, S.; Rajendran, V.; Jerald, M.K.; Sistla, R. Protective effect of galangin against dextran sulfate sodium (DSS)-induced ulcerative colitis in Balb/c mice. Inflamm. Res. 2019, 68, 691–704. [Google Scholar] [CrossRef]
- Gerges, S.H.; Tolba, M.F.; Elsherbiny, D.A.; El-Demerdash, E. The natural flavonoid galangin ameliorates dextran sulphate sodium–induced ulcerative colitis in mice: Effect on Toll-like receptor 4, inflammation and oxidative stress. Basic Clin. Pharmacol. Toxicol. 2020, 127, 10–20. [Google Scholar] [CrossRef]
- Hu, L.; Wu, C.; Zhang, Z.; Liu, M.; Maruthi Prasad, E.; Chen, Y.; Wang, K. Pinocembrin Protects Against Dextran Sulfate Sodium-Induced Rats Colitis by Ameliorating Inflammation, Improving Barrier Function and Modulating Gut Microbiota. Front. Physiol. 2019, 10, 908. [Google Scholar] [CrossRef]
- Liu, Q.; Zuo, R.; Wang, K.; Nong, F.-F.; Fu, Y.-J.; Huang, S.-W.; Pan, Z.-F.; Zhang, Y.; Luo, X.; Deng, X.-L.; et al. Oroxindin inhibits macrophage NLRP3 inflammasome activation in DSS-induced ulcerative colitis in mice via suppressing TXNIP-dependent NF-κB pathway. Acta Pharmacol. Sin. 2020, 41, 771–781. [Google Scholar] [CrossRef]
- Qu, X.; Li, Q.; Song, Y.; Xue, A.; Liu, Y.; Qi, D.; Dong, H. Potential of myricetin to restore the immune balance in dextran sulfate sodium-induced acute murine ulcerative colitis. J. Pharm. Pharmacol. 2020, 72, 92–100. [Google Scholar] [CrossRef]
- Tan, Y.; Zheng, C. Effects of Alpinetin on Intestinal Barrier Function, Inflammation and Oxidative Stress in Dextran Sulfate Sodium-Induced Ulcerative Colitis Mice. Am. J. Med. Sci. 2018, 355, 377–386. [Google Scholar] [CrossRef]
- Yu, Z.; Yue, B.; Ding, L.; Luo, X.; Ren, Y.; Zhang, J.; Mani, S.; Wang, Z.; Dou, W. Activation of PXR by Alpinetin Contributes to Abrogate Chemically Induced Inflammatory Bowel Disease. Front. Pharmacol. 2020, 11, 474. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Bhandari, R.; Li, C.; Shu, P.; Shaikh, I.I. Pectolinarigenin Suppresses LPS-Induced Inflammatory Response in Macrophages and Attenuates DSS-Induced Colitis by Modulating the NF-κB/Nrf2 Signaling Pathway. Inflammation 2022, 45, 2529–2543. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Yin, G.; Lu, Z.; Xie, P.; Zhou, H.; Liu, J.; Yu, L. Casticin prevents DSS induced ulcerative colitis in mice through inhibitions of NF-κB pathway and ROS signaling. Phytother. Res. 2018, 32, 1770–1783. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Shen, L.; Li, Y.; Li, Y.; Yu, S.; Wang, S. Hyperoside attenuates dextran sulfate sodium-induced colitis in mice possibly via activation of the Nrf2 signalling pathway. J. Inflamm. 2017, 14, 25. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Li, S.; Cao, H.; Shen, P.; Liu, J.; Fu, Y.; Cao, Y.; Zhang, N. The protective role of phloretin against dextran sulfate sodium-induced ulcerative colitis in mice. Food Funct. 2019, 10, 422–431. [Google Scholar] [CrossRef]
- Wu, Q.; Xie, S.; Zhu, Y.; Chen, J.; Tian, J.; Xiong, S.; Wu, C.; Ye, Y.; Peng, Y. Wogonin Strengthens the Therapeutic Effects of Mesenchymal Stem Cells in DSS-Induced Colitis via Promoting IL-10 Production. Oxidative Med. Cell. Longev. 2021, 2021, 5527935. [Google Scholar] [CrossRef]
- Zhou, Y.; Dou, F.; Song, H.; Liu, T. Anti-ulcerative effects of wogonin on ulcerative colitis induced by dextran sulfate sodium via Nrf2/TLR4/NF-κB signaling pathway in BALB/c mice. Environ. Toxicol. 2022, 37, 954–963. [Google Scholar] [CrossRef]
- Elhennawy, M.G.; Abdelaleem, E.A.; Zaki, A.A.; Mohamed, W.R. Cinnamaldehyde and hesperetin attenuate TNBS-induced ulcerative colitis in rats through modulation of the JAk2/STAT3/SOCS3 pathway. J. Biochem. Mol. Toxicol. 2021, 35, e22730. [Google Scholar] [CrossRef]
- Qu, S.-L.; Chen, L.; Wen, X.-S.; Zuo, J.-P.; Wang, X.-Y.; Lu, Z.-J.; Yang, Y.-F. Suppression of Th17 cell differentiation via sphingosine-1-phosphate receptor 2 by cinnamaldehyde can ameliorate ulcerative colitis. Biomed. Pharmacother. 2021, 134, 111116. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, H.; Lv, Q.; Zhong, C.; Cui, Y.; He, L.; Zhang, C.; Yu, J. Tiliroside Ameliorates Ulcerative Colitis by Restoring the M1/M2 Macrophage Balance via the HIF-1α/glycolysis Pathway. Front. Immunol. 2021, 12, 649463. [Google Scholar] [CrossRef] [PubMed]
- Lv, Q.; Xing, Y.; Liu, Y.; Chen, Q.; Xu, J.; Hu, L.; Zhang, Y. Didymin switches M1-like toward M2-like macrophage to ameliorate ulcerative colitis via fatty acid oxidation. Pharmacol. Res. 2021, 169, 105613. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.-H.; Liu, J.-Y.; Yin, J.-B. Eriodictyol attenuates TNBS-induced ulcerative colitis through repressing TLR4/NF-kB signaling pathway in rats. Kaohsiung J. Med. Sci. 2021, 37, 812–818. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Shen, L.; Li, H.; Peng, H. Eriodictyol attenuates dextran sodium sulphate-induced colitis in mice by regulating the sonic hedgehog signalling pathway. Pharm. Biol. 2021, 59, 972–983. [Google Scholar] [CrossRef]
- Li, X.-X.; Chen, S.-G.; Yue, G.G.-L.; Kwok, H.-F.; Lee, J.K.-M.; Zheng, T.; Shaw, P.-C.; Simmonds, M.S.J.; Lau, C.B.-S. Natural flavone tricin exerted anti-inflammatory activity in macrophage via NF-κB pathway and ameliorated acute colitis in mice. Phytomedicine 2021, 90, 153625. [Google Scholar] [CrossRef]
- Yue, B.; Ren, J.; Yu, Z.; Luo, X.; Ren, Y.; Zhang, J.; Mani, S.; Wang, Z.; Dou, W. Pinocembrin alleviates ulcerative colitis in mice via regulating gut microbiota, suppressing TLR4/MD2/NF-κB pathway and promoting intestinal barrier. Biosci. Rep. 2020, 40, BSR20200986. [Google Scholar] [CrossRef]
- Peng, L.; Gao, X.; Nie, L.; Xie, J.; Dai, T.; Shi, C.; Tao, L.; Wang, Y.; Tian, Y.; Sheng, J. Astragalin Attenuates Dextran Sulfate Sodium (DSS)-Induced Acute Experimental Colitis by Alleviating Gut Microbiota Dysbiosis and Inhibiting NF-κB Activation in Mice. Front. Immunol. 2020, 11, 2058. [Google Scholar] [CrossRef]
- Qu, Y.; Li, X.; Xu, F.; Zhao, S.; Wu, X.; Wang, Y.; Xie, J. Kaempferol Alleviates Murine Experimental Colitis by Restoring Gut Microbiota and Inhibiting the LPS-TLR4-NF-κB Axis. Front. Immunol. 2021, 12, 679897. [Google Scholar] [CrossRef]
- Ren, J.; Yue, B.; Wang, H.; Zhang, B.; Luo, X.; Yu, Z.; Zhang, J.; Ren, Y.; Mani, S.; Wang, Z.; et al. Acacetin Ameliorates Experimental Colitis in Mice via Inhibiting Macrophage Inflammatory Response and Regulating the Composition of Gut Microbiota. Front. Physiol. 2021, 11, 577237. [Google Scholar] [CrossRef] [PubMed]
- Abron, J.D.; Singh, N.P.; Price, R.L.; Nagarkatti, M.; Nagarkatti, P.S.; Singh, U.P. Genistein induces macrophage polarization and systemic cytokine to ameliorate experimental colitis. PLoS ONE 2018, 13, e0199631. [Google Scholar] [CrossRef] [PubMed]
- Bai, D.; Sun, T.; Zhao, J.; Du, J.; Bu, X.; Cao, W.; Zhao, Y.; Lu, N. Oroxylin A maintains the colonic mucus barrier to reduce disease susceptibility by reconstituting a dietary fiber-deprived gut microbiota. Cancer Lett. 2021, 515, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhong, B.; Min, X.; Hou, Y.; Lin, L.; Wu, Q.; Shi, J.; Chen, X. Therapeutic potential of isobavachalcone, a natural flavonoid, in murine experimental colitis by inhibiting NF-κB p65. Phytother. Res. 2021, 35, 5861–5870. [Google Scholar] [CrossRef]
- Dou, W.; Zhang, J.; Sun, A.; Zhang, E.; Ding, L.; Mukherjee, S.; Wei, X.; Chou, G.; Wang, Z.-T.; Mani, S. Protective effect of naringenin against experimental colitis via suppression of Toll-like receptor 4/NF-κB signalling. Br. J. Nutr. 2013, 110, 599–608. [Google Scholar] [CrossRef]
- Hagenlocher, Y.; Gommeringer, S.; Held, A.; Feilhauer, K.; Köninger, J.; Bischoff, S.C.; Lorentz, A. Nobiletin acts anti-inflammatory on murine IL-10−/− colitis and human intestinal fibroblasts. Eur. J. Nutr. 2019, 58, 1391–1401. [Google Scholar] [CrossRef]
- Suga, N.; Murakami, A.; Arimitsu, H.; Nakamura, T.; Nakamura, Y.; Kato, Y. Luteolin suppresses 5-hydroxytryptamine elevation in stimulated RBL-2H3 cells and experimental colitis mice. J. Clin. Biochem. Nutr. 2021, 69, 20–27. [Google Scholar] [CrossRef]
- Li, Y.; Shen, L.; Luo, H. Luteolin ameliorates dextran sulfate sodium-induced colitis in mice possibly through activation of the Nrf2 signaling pathway. Int. Immunopharmacol. 2016, 40, 24–31. [Google Scholar] [CrossRef]
- Li, W.; Zhang, L.; Xu, Q.; Yang, W.; Zhao, J.; Ren, Y.; Yu, Z.; Ma, L. Taxifolin Alleviates DSS-Induced Ulcerative Colitis by Acting on Gut Microbiome to Produce Butyric Acid. Nutrients 2022, 14, 1069. [Google Scholar] [CrossRef]
- Zhang, H.; Zhuo, S.; Song, D.; Wang, L.; Gu, J.; Ma, J.; Gu, Y.; Ji, M.; Chen, M.; Guo, Y. Icariin Inhibits Intestinal Inflammation of DSS-Induced Colitis Mice Through Modulating Intestinal Flora Abundance and Modulating P-P65/P65 Molecule. Turk. J. Gastroenterol. 2021, 32, 382–392. [Google Scholar] [CrossRef]
- Li, Y.-Y.; Wang, X.-J.; Su, Y.-L.; Wang, Q.; Huang, S.-W.; Pan, Z.-F.; Chen, Y.-P.; Liang, J.-J.; Zhang, M.-L.; Xie, X.-Q.; et al. Baicalein ameliorates ulcerative colitis by improving intestinal epithelial barrier via AhR/IL-22 pathway in ILC3s. Acta Pharmacol. Sin. 2022, 43, 1495–1507. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Liu, J.; Shen, P.; Cai, J.; Han, Y.; Zhu, K.; Fu, Y.; Zhang, N.; Zhang, Z.; Cao, Y. Protective Effect of Naringin on DSS-Induced Ulcerative Colitis in Mice. J. Agric. Food Chem. 2018, 66, 13133–13140. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.-D.; Lee, J.-H.; Lee, Y.-M.; Kim, D.-K. Puerarin inhibits inflammation and oxidative stress in dextran sulfate sodium-induced colitis mice model. Biomed. Pharmacother. 2020, 124, 109847. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Lv, Q.; Miao, Y.-M.; Qiao, S.-M.; Dai, Y.; Wei, Z.-F. Cardamonin, a natural flavone, alleviates inflammatory bowel disease by the inhibition of NLRP3 inflammasome activation via an AhR/Nrf2/NQO1 pathway. Biochem. Pharmacol. 2018, 155, 494–509. [Google Scholar] [CrossRef] [PubMed]
- Gong, Z.; Zhao, S.; Zhou, J.; Yan, J.; Wang, L.; Du, X.; Li, H.; Chen, Y.; Cai, W.; Wu, J. Curcumin alleviates DSS-induced colitis via inhibiting NLRP3 inflammsome activation and IL-1β production. Mol. Immunol. 2018, 104, 11–19. [Google Scholar] [CrossRef]
- Xiao, Q.-P.; Zhong, Y.-B.; Kang, Z.-P.; Huang, J.-Q.; Fang, W.-Y.; Wei, S.-Y.; Long, J.; Li, S.-S.; Zhao, H.-M.; Liu, D.-Y. Curcumin regulates the homeostasis of Th17/Treg and improves the composition of gut microbiota in type 2 diabetic mice with colitis. Phytother. Res. 2022, 36, 1708–1723. [Google Scholar] [CrossRef]
- Ju, S.; Ge, Y.; Li, P.; Tian, X.; Wang, H.; Zheng, X.; Ju, S. Dietary quercetin ameliorates experimental colitis in mouse by remodeling the function of colonic macrophages via a heme oxygenase-1-dependent pathway. Cell Cycle 2018, 17, 53–63. [Google Scholar] [CrossRef]
- Shen, J.; Li, N.; Zhang, X. Daidzein Ameliorates Dextran Sulfate Sodium-Induced Experimental Colitis in Mice by Regulating NF-κB Signaling. J. Environ. Pathol. Toxicol. Oncol. 2019, 38, 29–39. [Google Scholar]
- Gan, Y.; Fu, Y.; Yang, L.; Chen, J.; Lei, H.; Liu, Q. Cyanidin-3-O-Glucoside and Cyanidin Protect Against Intestinal Barrier Damage and 2,4,6-Trinitrobenzenesulfonic Acid-Induced Colitis. J. Med. Food 2019, 23, 90–99. [Google Scholar] [CrossRef]
- Guo, G.; Shi, W.; Shi, F.; Gong, W.; Li, F.; Zhou, G.; She, J. Anti-inflammatory effects of eriocitrin against the dextran sulfate sodium–induced experimental colitis in murine model. J. Biochem. Mol. Toxicol. 2019, 33, e22400. [Google Scholar] [CrossRef]
- Guazelli, C.F.S.; Fattori, V.; Ferraz, C.R.; Borghi, S.M.; Casagrande, R.; Baracat, M.M.; Verri, W.A. Antioxidant and anti-inflammatory effects of hesperidin methyl chalcone in experimental ulcerative colitis. Chem.-Biol. Interact. 2021, 333, 109315. [Google Scholar] [CrossRef]
- Xu, B.; Huang, S.; Chen, Y.; Wang, Q.; Luo, S.; Li, Y.; Wang, X.; Chen, J.; Luo, X.; Zhou, L. Synergistic effect of combined treatment with baicalin and emodin on DSS-induced colitis in mouse. Phytother. Res. 2021, 35, 5708–5719. [Google Scholar] [CrossRef]
- Li, Z.; Lin, M.; Li, Y.; Shao, J.; Huang, R.; Qiu, Y.; Liu, Y.; Chen, L. Total flavonoids of Sophora flavescens and kurarinone ameliorated ulcerative colitis by regulating Th17/Treg cell homeostasis. J. Ethnopharmacol. 2022, 297, 115500. [Google Scholar] [CrossRef]
- Huang, B.; Wang, L.; Liu, M.; Wu, X.; Lu, Q.; Liu, R. The underlying mechanism of A-type procyanidins from peanut skin on DSS-induced ulcerative colitis mice by regulating gut microbiota and metabolism. J. Food Biochem. 2022, 46, e14103. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Liu, J.; Jin, R.; Yao, Y.; He, S.; Lei, M.; Peng, X. Linarin ameliorates dextran sulfate sodium-induced colitis in C57BL/6J mice via the improvement of intestinal barrier, suppression of inflammatory responses and modulation of gut microbiota. Food Funct. 2022, 13, 10574–10586. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liang, F.; Chen, Z.; Chen, Y.; Yuan, J.; Xiong, Q.; Hou, S.; Huang, S.; Liu, C.; Liang, J. Vitexin Protects against Dextran Sodium Sulfate-Induced Colitis in Mice and Its Potential Mechanisms. J. Agric. Food Chem. 2022, 70, 12041–12054. [Google Scholar] [CrossRef]
- Zhang, J.; Xu, X.; Li, N.; Cao, L.; Sun, Y.; Wang, J.; He, S.; Si, J.; Qing, D. Licoflavone B, an isoprene flavonoid derived from licorice residue, relieves dextran sodium sulfate-induced ulcerative colitis by rebuilding the gut barrier and regulating intestinal microflora. Eur. J. Pharmacol. 2022, 916, 174730. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Wang, S.; Ji, S. Trifolirhizin regulates the balance of Th17/Treg cells and inflammation in the ulcerative colitis mice through inhibiting the TXNIP-mediated activation of NLRP3 inflammasome. Clin. Exp. Pharmacol. Physiol. 2022, 49, 787–796. [Google Scholar] [CrossRef]
- Chao, L.; Zheng, P.; Xia, L.; Yong, Y.; Lu, G.; Tang, F.; Zhao, Z. Calycosin attenuates dextran sulfate sodium (DSS)-induced experimental colitis. Iran. J. Basic Med. Sci. 2017, 20, 1056–1062. [Google Scholar]
- Márquez-Flores, Y.K.; Villegas, I.; Cárdeno, A.; Rosillo, M.Á.; Alarcón-de-la-Lastra, C. Apigenin supplementation protects the development of dextran sulfate sodium-induced murine experimental colitis by inhibiting canonical and non-canonical inflammasome signaling pathways. J. Nutr. Biochem. 2016, 30, 143–152. [Google Scholar] [CrossRef]
- Yang, W.; Chen, X.; Li, Y.; Guo, S.; Wang, Z.; Yu, X. Advances in Pharmacological Activities of Terpenoids. Nat. Prod. Commun. 2020, 15, 1–13. [Google Scholar] [CrossRef]
- Guo, W.; Liu, W.; Jin, B.; Geng, J.; Li, J.; Ding, H.; Wu, X.; Xu, Q.; Sun, Y.; Gao, J. Asiatic acid ameliorates dextran sulfate sodium-induced murine experimental colitis via suppressing mitochondria-mediated NLRP3 inflammasome activation. Int. Immunopharmacol. 2015, 24, 232–238. [Google Scholar] [CrossRef] [PubMed]
- de Santana Souza, M.T.; Teixeira, D.F.; de Oliveira, J.P.; Oliveira, A.S.; Quintans-Júnior, L.J.; Correa, C.B.; Camargo, E.A. Protective effect of carvacrol on acetic acid-induced colitis. Biomed. Pharmacother. 2017, 96, 313–319. [Google Scholar] [CrossRef]
- Rapa, S.F.; Waltenberger, B.; Di Paola, R.; Adesso, S.; Siracusa, R.; Peritore, A.F.; D’Amico, R.; Autore, G.; Cuzzocrea, S.; Stuppner, H.; et al. Plumericin prevents intestinal inflammation and oxidative stress in vitro and in vivo. FASEB J. 2020, 34, 1576–1590. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Wu, X.; Wu, Q.; Lu, Y.; Shi, J.; Chen, X. Dihydrotanshinone I, a natural product, ameliorates DSS-induced experimental ulcerative colitis in mice. Toxicol. Appl. Pharmacol. 2018, 344, 35–45. [Google Scholar] [CrossRef]
- Bento, A.F.; Marcon, R.; Dutra, R.C.; Claudino, R.F.; Cola, M.; Pereira Leite, D.F.; Calixto, J.B. β-Caryophyllene Inhibits Dextran Sulfate Sodium-Induced Colitis in Mice through CB2 Receptor Activation and PPARγ Pathway. Am. J. Pathol. 2011, 178, 1153–1166. [Google Scholar] [CrossRef]
- Matos, I.; Bento, A.F.; Marcon, R.; Claudino, R.F.; Calixto, J.B. Preventive and therapeutic oral administration of the pentacyclic triterpene α,β-amyrin ameliorates dextran sulfate sodium-induced colitis in mice: The relevance of cannabinoid system. Mol. Immunol. 2013, 54, 482–492. [Google Scholar] [CrossRef]
- Zhang, X.; Xu, F.; Liu, L.; Feng, L.; Wu, X.; Shen, Y.; Sun, Y.; Wu, X.; Xu, Q. (+)-Borneol improves the efficacy of edaravone against DSS-induced colitis by promoting M2 macrophages polarization via JAK2-STAT3 signaling pathway. Int. Immunopharmacol. 2017, 53, 1–10. [Google Scholar] [CrossRef]
- Trivedi, P.P.; Jena, G.B. Mechanistic insight into beta-carotene-mediated protection against ulcerative colitis-associated local and systemic damage in mice. Eur. J. Nutr. 2015, 54, 639–652. [Google Scholar] [CrossRef]
- De Fazio, L.; Spisni, E.; Cavazza, E.; Strillacci, A.; Candela, M.; Centanni, M.; Ricci, C.; Rizzello, F.; Campieri, M.; Valerii, M.C. Dietary geraniol by oral or enema administration strongly reduces dysbiosis and systemic inflammation in dextran sulfate sodium-treated mice. Front. Pharmacol. 2016, 7, 38. [Google Scholar] [CrossRef]
- Soubh, A.A.; Abdallah, D.M.; El-Abhar, H.S. Geraniol ameliorates TNBS-induced colitis: Involvement of Wnt/β-catenin, p38MAPK, NFκB, and PPARγ signaling pathways. Life Sci. 2015, 136, 142–150. [Google Scholar] [CrossRef]
- Liu, C.; Dunkin, D.; Lai, J.; Song, Y.; Ceballos, C.; Benkov, K.; Li, X.-M. Anti-inflammatory Effects of Ganoderma lucidum Triterpenoid in Human Crohn’s Disease Associated with Downregulation of NF-κB Signaling. Inflamm. Bowel Dis. 2015, 21, 1918–1925. [Google Scholar] [CrossRef]
- D’Alessio, P.A.; Ostan, R.; Bisson, J.-F.; Schulzke, J.D.; Ursini, M.V.; Béné, M.C. Oral administration of d-Limonene controls inflammation in rat colitis and displays anti-inflammatory properties as diet supplementation in humans. Life Sci. 2013, 92, 1151–1156. [Google Scholar] [CrossRef]
- Yu, L.; Yan, J.; Sun, Z. D-limonene exhibits anti-inflammatory and antioxidant properties in an ulcerative colitis rat model via regulation of iNOS, COX-2, PGE2 and ERK signaling pathways. Mol. Med. Rep. 2017, 15, 2339–2346. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi-Pirbaluti, M.; Motaghi, E.; Bozorgi, H. The effect of menthol on acute experimental colitis in rats. Eur. J. Pharmacol. 2017, 805, 101–107. [Google Scholar] [CrossRef] [PubMed]
- González-Ramírez, A.E.; González-Trujano, M.E.; Orozco-Suárez, S.A.; Alvarado-Vásquez, N.; López-Muñoz, F.J. Nerol alleviates pathologic markers in the oxazolone-induced colitis model. Eur. J. Pharmacol. 2016, 776, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Kang, G.-D.; Lim, S.; Kim, D.-H. Oleanolic acid ameliorates dextran sodium sulfate-induced colitis in mice by restoring the balance of Th17/Treg cells and inhibiting NF-κB signaling pathway. Int. Immunopharmacol. 2015, 29, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Uemura, T.; Yashiro, T.; Oda, R.; Shioya, N.; Nakajima, T.; Hachisu, M.; Kobayashi, S.; Nishiyama, C.; Arimura, G.-I. Intestinal Anti-Inflammatory Activity of Perillaldehyde. J. Agric. Food Chem. 2018, 66, 3443–3448. [Google Scholar] [CrossRef] [PubMed]
- Chamanara, M.; Abdollahi, A.; Rezayat, S.M.; Ghazi-Khansari, M.; Dehpour, A.; Nassireslami, E.; Rashidian, A. Thymol reduces acetic acid-induced inflammatory response through inhibition of NF-kB signaling pathway in rat colon tissue. Inflammopharmacology 2019, 27, 1275–1283. [Google Scholar] [CrossRef]
- Ren, Y.; Yue, B.; Ren, G.; Yu, Z.; Luo, X.; Sun, A.; Zhang, J.; Han, M.; Wang, Z.; Dou, W. Activation of PXR by alantolactone ameliorates DSS-induced experimental colitis via suppressing NF-κB signaling pathway. Sci. Rep. 2019, 9, 16636. [Google Scholar] [CrossRef]
- El-Sherbiny, M.; Eisa, N.H.; Abo El-Magd, N.F.; Elsherbiny, N.M.; Said, E.; Khodir, A.E. Anti-inflammatory/anti-apoptotic impact of betulin attenuates experimentally induced ulcerative colitis: An insight into TLR4/NF-kB/caspase signalling modulation. Environ. Toxicol. Pharmacol. 2021, 88, 103750. [Google Scholar] [CrossRef] [PubMed]
- El-Akabawy, G.; El-Sherif, N.M. Zeaxanthin exerts protective effects on acetic acid-induced colitis in rats via modulation of pro-inflammatory cytokines and oxidative stress. Biomed. Pharmacother. 2019, 111, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Wang, G.; Wu, S.; Li, C. Protective Effect of D-Carvone against Dextran Sulfate Sodium Induced Ulcerative Colitis in Balb/c Mice and LPS Induced RAW Cells via the Inhibition of COX-2 and TNF-&alpha. J. Environ. Pathol. Toxicol. Oncol. 2020, 39, 235–245. [Google Scholar] [PubMed]
- Li, M.; Guo, W.; Dong, Y.; Wang, W.; Tian, C.; Zhang, Z.; Yu, T.; Zhou, H.; Gui, Y.; Xue, K.; et al. Beneficial Effects of Celastrol on Immune Balance by Modulating Gut Microbiota in Experimental Ulcerative Colitis Mice. Genom. Proteom. Bioinform. 2022, 20, 288–303. [Google Scholar] [CrossRef]
- Yun, X.; Fang, Y.; Lv, C.; Qiao, S.; Tao, Y.; Dai, Y.; Xia, Y. Inhibition of the activation of γδT17 cells through PPARγ–PTEN/Akt/GSK3β/NFAT pathway contributes to the anti-colitis effect of madecassic acid. Cell Death Dis. 2020, 11, 752. [Google Scholar] [CrossRef]
- Raj, V.; Venkataraman, B.; Almarzooqi, S.; Chandran, S.; Ojha, S.K.; Attoub, S.; Adrian, T.E.; Subramanya, S.B. Nerolidol Mitigates Colonic Inflammation: An Experimental Study Using both In Vivo and In Vitro Models. Nutrients 2020, 12, 2032. [Google Scholar] [CrossRef]
- Almarzooqi, S.; Venkataraman, B.; Raj, V.; Alkuwaiti, S.A.; Das, K.M.; Collin, P.D.; Adrian, T.E.; Subramanya, S.B. β-Myrcene Mitigates Colon Inflammation by Inhibiting MAP Kinase and NF-κB Signaling Pathways. Molecules 2022, 27, 8744. [Google Scholar] [CrossRef]
- Amen, Y.; Elsbaey, M.; Othman, A.; Sallam, M.; Shimizu, K. Naturally Occurring Chromone Glycosides: Sources, Bioactivities, and Spectroscopic Features. Molecules 2021, 26, 7646. [Google Scholar] [CrossRef]
- Škubník, J.; Pavlíčková, V.; Rimpelová, S. Cardiac Glycosides as Immune System Modulators. Biomolecules 2021, 11, 659. [Google Scholar] [CrossRef]
- Li, J.; Ren, S.; Li, M.; Bi, J.; Yang, G.; Li, E. Paeoniflorin protects against dextran sulfate sodium (DSS)-induced colitis in mice through inhibition of inflammation and eosinophil infiltration. Int. Immunopharmacol. 2021, 97, 107667. [Google Scholar] [CrossRef]
- Li, H.; Shen, L.; Lv, T.; Wang, R.; Zhang, N.; Peng, H.; Diao, W. Salidroside attenuates dextran sulfate sodium-induced colitis in mice via SIRT1/FoxOs signaling pathway. Eur. J. Pharmacol. 2019, 861, 172591. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Fu, Y.; Xu, B.; Liu, C.; Wang, Q.; Luo, S.; Nong, F.; Wang, X.; Huang, S.; Chen, J.; et al. Wogonoside alleviates colitis by improving intestinal epithelial barrier function via the MLCK/pMLC2 pathway. Phytomedicine 2020, 68, 153179. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Ren, J.; Gu, G.; Wang, G.; Gong, W.; Wu, X.; Ren, H.; Hong, Z.; Li, J. Hesperidin Protects Against Intestinal Inflammation by Restoring Intestinal Barrier Function and Up-Regulating Treg Cells. Mol. Nutr. Food Res. 2019, 63, 1800975. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.-C.; Lee, D.-Y.; Hsu, J.-T.; Cheng, C.-F.; Lan, J.-L.; Chiu, S.-C.; Cho, D.-Y.; Hsu, J.-L. Evaluations and Mechanistic Interrogation of Natural Products Isolated from Paeonia suffruticosa for the Treatment of Inflammatory Bowel Disease. Front. Pharmacol. 2021, 12, 696158. [Google Scholar] [CrossRef]
- Li, Q.; Shan, Q.; Sang, X.; Zhu, R.; Chen, X.; Cao, G. Total glycosides of peony protects against inflammatory bowel disease by regulating IL-23/IL-17 axis and Th17/Treg balance. Am. J. Chin. Med. 2019, 47, 177–201. [Google Scholar] [CrossRef]
- Kang, Z.; Zhonga, Y.; Wu, T.; Huang, J.; Zhao, H.; Liu, D. Ginsenoside from ginseng: A promising treatment for inflammatory bowel disease. Pharmacol. Rep. 2021, 73, 700–711. [Google Scholar] [CrossRef]
- Yang, N.; Liang, G.; Lin, J.; Zhang, S.; Lin, Q.; Ji, X.; Chen, H.; Li, N.; Jin, S. Ginsenoside Rd therapy improves histological and functional recovery in a rat model of inflammatory bowel disease. Phytother. Res. 2020, 34, 3019–3028. [Google Scholar] [CrossRef]
- Cheng, H.; Liu, J.; Zhang, D.; Wang, J.; Tan, Y.; Feng, W.; Peng, C. Ginsenoside Rg1 Alleviates Acute Ulcerative Colitis by Modulating Gut Microbiota and Microbial Tryptophan Metabolism. Front. Immunol. 2022, 13, 817600. [Google Scholar] [CrossRef]
- Chen, X.; Xu, T.; Lv, X.; Zhang, J.; Liu, S. Ginsenoside Rh2 alleviates ulcerative colitis by regulating the STAT3/miR-214 signaling pathway. J. Ethnopharmacol. 2021, 274, 113997. [Google Scholar] [CrossRef]
- Tian, M.; Ma, P.; Zhang, Y.; Mi, Y.; Fan, D. Ginsenoside Rk3 alleviated DSS-induced ulcerative colitis by protecting colon barrier and inhibiting NLRP3 inflammasome pathway. Int. Immunopharmacol. 2020, 85, 106645. [Google Scholar] [CrossRef]
- Wu, M.-M.; Wang, Q.-M.; Huang, B.-Y.; Mai, C.-T.; Wang, C.-L.; Wang, T.-T.; Zhang, X.-J. Dioscin ameliorates murine ulcerative colitis by regulating macrophage polarization. Pharmacol. Res. 2021, 172, 105796. [Google Scholar] [CrossRef]
- Ghattamaneni, N.K.R.; Sharma, A.; Panchal, S.K.; Brown, L. Pelargonidin 3-glucoside-enriched strawberry attenuates symptoms of DSS-induced inflammatory bowel disease and diet-induced metabolic syndrome in rats. Eur. J. Nutr. 2020, 59, 2905–2918. [Google Scholar] [CrossRef]
- He, X.; Liu, J.; Long, G.; Xia, X.-H.; Liu, M. 2,3,5,4′-Tetrahydroxystilbene-2-O-β-D-glucoside, a major bioactive component from Polygoni multiflori Radix (Heshouwu) suppresses DSS induced acute colitis in BALb/c mice by modulating gut microbiota. Biomed. Pharmacother. 2021, 137, 111420. [Google Scholar] [CrossRef]
- Zhang, J.; Dou, W.; Zhang, E.; Sun, A.; Ding, L.; Wei, X.; Chou, G.; Mani, S.; Wang, Z. Paeoniflorin abrogates DSS-induced colitis via a TLR4-dependent pathway. Am. J. Physiol.-Gastrointest. Liver Physiol. 2014, 306, 27–36. [Google Scholar] [CrossRef]
- Han, Q.; Deng, L.-R.; Zou, M.; Tang, H.-z.; Huang, C.-y.; Chen, F.-J.; Tomlinson, B.; Li, Y.-H. Anemoside B4 protects against chronic relapsing colitis in mice by modulating inflammatory response, colonic transcriptome and the gut microbiota. Phytomedicine 2022, 106, 154416. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.-T.; Wen, B.; Shen, X.-C.; Bian, Z.-X. Potential of Plant-sourced Phenols for Inflammatory Bowel Disease. Curr. Med. Chem. 2018, 25, 5191–5217. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wu, B.; Fu, W.; Reddivari, L. The Anti-inflammatory Effects of Dietary Anthocyanins against Ulcerative Colitis. Int. J. Mol. Sci. 2019, 20, 2588. [Google Scholar] [CrossRef] [PubMed]
- Direito, R.; Rocha, J.; Lima, A.; Gonçalves, M.M.; Duarte, M.P.; Mateus, V.; Sousa, C.; Fernandes, A.; Pinto, R.; Boavida Ferreira, R.; et al. Reduction of Inflammation and Colon Injury by a Spearmint Phenolic Extract in Experimental Bowel Disease in Mice. Medicines 2019, 6, 65. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yang, Q.; Mi, X.; Qiu, L.; Tao, X.; Zhang, Z.; Xia, J.; Wu, Q.; Wei, H. Ripened Pu-erh Tea Extract Promotes Gut Microbiota Resilience against Dextran Sulfate Sodium Induced Colitis. J. Agric. Food Chem. 2021, 69, 2190–2203. [Google Scholar] [CrossRef]
- Zhao, L.; Zhang, Y.; Liu, G.; Hao, S.; Wang, C.; Wang, Y. Black rice anthocyanin-rich extract and rosmarinic acid, alone and in combination, protect against DSS-induced colitis in mice. Food Funct. 2018, 9, 2796–2808. [Google Scholar] [CrossRef]
- Valero, M.S.; González, M.; Ramón-Gimenez, M.; Andrade, P.B.; Moreo, E.; Les, F.; Fernandes, F.; Gómez-Rincón, C.; Berzosa, C.; García de Jalón, J.A.; et al. Jasonia glutinosa (L.) DC.; a traditional herbal medicine, reduces inflammation, oxidative stress and protects the intestinal barrier in a murine model of colitis. Inflammopharmacology 2020, 28, 1717–1734. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Zheng, J.; Xu, F.; Xi, Y.; Chen, J.; Xu, X. Resveratrol Alleviates Dextran Sulfate Sodium-Induced Acute Ulcerative Colitis in Mice by Mediating PI3K/Akt/VEGFA Pathway. Front. Pharmacol. 2021, 12, 693982. [Google Scholar] [CrossRef]
- Pan, H.-H.; Zhou, X.-X.; Ma, Y.-Y.; Pan, W.-S.; Zhao, F.; Yu, M.-S.; Liu, J.-Q. Resveratrol alleviates intestinal mucosal barrier dysfunction in dextran sulfate sodium-induced colitis mice by enhancing autophagy. World J. Gastroenterol. 2020, 26, 4945. [Google Scholar] [CrossRef] [PubMed]
- Alrafas, H.R.; Busbee, P.B.; Nagarkatti, M.; Nagarkatti, P.S. Resveratrol modulates the gut microbiota to prevent murine colitis development through induction of Tregs and suppression of Th17 cells. J. Leukoc. Biol. 2019, 106, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Chen, D.; Zheng, P.; Yu, J.; He, J.; Mao, X.; Yu, B. The Bidirectional Interactions between Resveratrol and Gut Microbiota: An Insight into Oxidative Stress and Inflammatory Bowel Disease Therapy. BioMed Res. Int. 2019, 2019, 5403761. [Google Scholar] [CrossRef]
- Arya, V.S.; Kanthlal, S.K.; Linda, G. The role of dietary polyphenols in inflammatory bowel disease: A possible clue on the molecular mechanisms involved in the prevention of immune and inflammatory reactions. J. Food Biochem. 2020, 44, e13369. [Google Scholar] [CrossRef]
- Wu, Z.; Huang, S.; Li, T.; Li, N.; Han, D.; Zhang, B.; Xu, Z.Z.; Zhang, S.; Pang, J.; Wang, S.; et al. Gut microbiota from green tea polyphenol-dosed mice improves intestinal epithelial homeostasis and ameliorates experimental colitis. Microbiome 2021, 9, 184. [Google Scholar] [CrossRef]
- Pandurangan, A.K.; Mohebali, N.; Norhaizan, M.E.; Looi, C.Y. Gallic acid attenuates dextran sulfate sodium-induced experimental colitis in BALB/c mice. Drug Des. Dev. Ther. 2015, 9, 3923–3934. [Google Scholar] [CrossRef]
- Zhu, X.; Tian, X.; Yang, M.; Yu, Y.; Zhou, Y.; Gao, Y.; Zhang, L.; Li, Z.; Xiao, Y.; Moses, R.E.; et al. Procyanidin B2 Promotes Intestinal Injury Repair and Attenuates Colitis-Associated Tumorigenesis via Suppression of Oxidative Stress in Mice. Antioxid. Redox Signal. 2020, 35, 75–92. [Google Scholar] [CrossRef]
- Zhang, H.; Lang, W.; Liu, X.; Bai, J.; Jia, Q.; Shi, Q. Procyanidin A1 alleviates DSS-induced ulcerative colitis via regulating AMPK/mTOR/p70S6K-mediated autophagy. J. Physiol. Biochem. 2022, 78, 213–227. [Google Scholar] [CrossRef]
- Lv, T.; Shen, L.; Yang, L.; Diao, W.; Yang, Z.; Zhang, Y.; Yu, S.; Li, Y. Polydatin ameliorates dextran sulfate sodium-induced colitis by decreasing oxidative stress and apoptosis partially via Sonic hedgehog signaling pathway. Int. Immunopharmacol. 2018, 64, 256–263. [Google Scholar] [CrossRef]
- Gao, W.; Wang, C.; Yu, L.; Sheng, T.; Wu, Z.; Wang, X.; Zhang, D.; Lin, Y.; Gong, Y. Chlorogenic Acid Attenuates Dextran Sodium Sulfate-Induced Ulcerative Colitis in Mice through MAPK/ERK/JNK Pathway. BioMed Res. Int. 2019, 2019, 6769789. [Google Scholar] [CrossRef]
- Zeng, J.; Zhang, D.; Wan, X.; Bai, Y.; Yuan, C.; Wang, T.; Yuan, D.; Zhang, C.; Liu, C. Chlorogenic Acid Suppresses miR-155 and Ameliorates Ulcerative Colitis through the NF-κB/NLRP3 Inflammasome Pathway. Mol. Nutr. Food Res. 2020, 64, 2000452. [Google Scholar] [CrossRef]
- Güvenç, M.; Cellat, M.; Özkan, H.; Tekeli, İ.O.; Uyar, A.; Gökçek, İ.; İşler, C.T.; Yakan, A. Protective Effects of Tyrosol Against DSS-Induced Ulcerative Colitis in Rats. Inflammation 2019, 42, 1680–1691. [Google Scholar] [CrossRef]
- Zeng, C.; Xiao, J.-H.; Chang, M.-J.; Wang, J.-L. Beneficial Effects of THSG on Acetic Acid-Induced Experimental Colitis: Involvement of Upregulation of PPAR-γ and Inhibition of the Nf-Κb Inflammatory Pathway. Molecules 2011, 16, 8552–8568. [Google Scholar] [CrossRef]
- Wang, K.; Yang, Q.; Ma, Q.; Wang, B.; Wan, Z.; Chen, M.; Wu, L. Protective Effects of Salvianolic Acid A against Dextran Sodium Sulfate-Induced Acute Colitis in Rats. Nutrients 2018, 10, 791. [Google Scholar] [CrossRef]
- Wu, X.; Wang, L.; Tang, L.; Wang, L.; Cao, S.; Wu, Q.; Zhang, Z.; Li, L. Salvianolic acid B alters the gut microbiota and mitigates colitis severity and associated inflammation. J. Funct. Foods 2018, 46, 312–319. [Google Scholar] [CrossRef]
- Gong, H.; He, Z.; Peng, A.; Zhang, X.; Cheng, B.; Sun, Y.; Zheng, L.; Huang, K. Effects of several quinones on insulin aggregation. Sci. Rep. 2014, 4, 5648. [Google Scholar] [CrossRef]
- Han, H.; Sun, W.; Feng, L.; Wen, Z.; Yang, M.; Ma, Y.; Fu, J.; Ma, X.; Xu, X.; Wang, Z.; et al. Differential relieving effects of shikonin and its derivatives on inflammation and mucosal barrier damage caused by ulcerative colitis. PeerJ 2021, 9, e10675. [Google Scholar] [CrossRef]
- Subramanya, S.B.; Venkataraman, B.; Raj, V.; Al Marzooqi, S.; Alhassani, A.; AlHassani, A.; Ahmed, K.J.; Attoub, S. Thymoquinone, a bioactive phytochemical alleviates colon inflammation through Nrf2/Keap1 system: An experimental study using both in vivo and in vitro model of colon inflammation. FASEB J. 2019, 33, 764.2. [Google Scholar] [CrossRef]
- Mahmoud, N.; Hegazy, M.-E.F.; Wadie, W.; Elbadawi, M.; Fleischer, E.; Klinger, A.; Bringmann, G.; Khayyal, M.T.; Efferth, T. Naphthoquinone derivatives as P-glycoprotein inducers in inflammatory bowel disease: 2D monolayers, 3D spheroids, and in vivo models. Pharmacol. Res. 2022, 179, 106233. [Google Scholar] [CrossRef] [PubMed]
- Pile, J.E.; Navalta, J.W.; Davis, C.D.; Sharma, N.C. Interventional Effects of Plumbagin on Experimental Ulcerative Colitis in Mice. J. Nat. Prod. 2013, 76, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Moreira, R.; Pereira, D.M.; Valentão, P.; Andrade, P.B. Pyrrolizidine Alkaloids: Chemistry, Pharmacology, Toxicology and Food Safety. Int. J. Mol. Sci. 2018, 19, 1668. [Google Scholar] [CrossRef]
- Peng, J.; Zheng, T.-T.; Li, X.; Liang, Y.; Wang, L.-J.; Huang, Y.-C.; Xiao, H.-T. Plant-Derived Alkaloids: The Promising Disease-Modifying Agents for Inflammatory Bowel Disease. Front. Pharmacol. 2019, 10, 351. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Fan, H.; Zhang, Z.; Jiang, F.; Li, M.; Zhou, H.; Guo, W.; Zhang, Z.; Kang, Z.; Gui, Y.; et al. Berberine ameliorates DSS-induced intestinal mucosal barrier dysfunction through microbiota-dependence and Wnt/β-catenin pathway. Int. J. Biol. Sci. 2022, 18, 1381–1397. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Fan, C.; Lu, H.; Feng, C.; He, P.; Yang, X.; Xiang, C.; Zuo, J.; Tang, W. Protective role of berberine on ulcerative colitis through modulating enteric glial cells–intestinal epithelial cells–immune cells interactions. Acta Pharm. Sin. B 2020, 10, 447–461. [Google Scholar] [CrossRef]
- Gupta, R.A.; Motiwala, M.N.; Dumore, N.G.; Danao, K.R.; Ganjare, A.B. Effect of piperine on inhibition of FFA induced TLR4 mediated inflammation and amelioration of acetic acid induced ulcerative colitis in mice. J. Ethnopharmacol. 2015, 164, 239–246. [Google Scholar] [CrossRef]
- Guo, G.; Shi, F.; Zhu, J.; Shao, Y.; Gong, W.; Zhou, G.; Wu, H.; She, J.; Shi, W. Piperine, a functional food alkaloid, exhibits inhibitory potential against TNBS-induced colitis via the inhibition of IκB-α/NF-κB and induces tight junction protein (claudin-1, occludin, and ZO-1) signaling pathway in experimental mice. Hum. Exp. Toxicol. 2019, 39, 477–491. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, K.; Qi, Z.; Chen, T.; Yu, W.; Jiang, Y.; Li, G.; Xiao, H. Therapeutic Mechanism and Effect of Camptothecin on Dextran Sodium Sulfate-Induced Ulcerative Colitis in Mice. J. Immunol. Res. 2021, 2021, 5556659. [Google Scholar] [CrossRef]
- Chen, Y.S.; Lian, Y.Z.; Chen, W.C.; Chang, C.C.; Tinkov, A.A.; Skalny, A.V.; Chao, J.C. Lycium barbarum Polysaccharides and Capsaicin Inhibit Oxidative Stress, Inflammatory Responses, and Pain Signaling in Rats with Dextran Sulfate Sodium-Induced Colitis. Int. J. Mol. Sci. 2022, 23, 2423. [Google Scholar] [CrossRef]
- Yan, X.; Lu, Q.-G.; Zeng, L.; Li, X.-H.; Liu, Y.; Du, X.-F.; Bai, G.-M. Synergistic protection of astragalus polysaccharides and matrine against ulcerative colitis and associated lung injury in rats. World J. Gastroenterol. 2020, 26, 55–69. [Google Scholar] [CrossRef]
- Yao, H.; Shi, Y.; Yuan, J.; Sa, R.; Chen, W.; Wan, X. Matrine protects against DSS-induced murine colitis by improving gut barrier integrity, inhibiting the PPAR-α signaling pathway, and modulating gut microbiota. Int. Immunopharmacol. 2021, 100, 108091. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, Y.; Zhao, Y.; Wu, W.; Meng, W.; Zhou, Y.; Qiu, Y.; Li, C. Protection against ulcerative colitis and colorectal cancer by evodiamine via anti-inflammatory effects. Mol. Med. Rep. 2022, 25, 188. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zhao, Q.; Huang, Q.; Li, Y.; Yu, J.; Zhang, R.; Liu, J.; Yan, P.; Xia, J.; Guo, L.; et al. Nuciferine Regulates Immune Function and Gut Microbiota in DSS-Induced Ulcerative Colitis. Front. Vet. Sci. 2022, 9, 939377. [Google Scholar] [CrossRef] [PubMed]
- Min, X.; Guo, Y.; Zhou, Y.; Chen, X. Protection against Dextran Sulfate Sodium-Induced Ulcerative Colitis in Mice by Neferine, A Natural Product from Nelumbo nucifera Gaertn. Cell J. 2020, 22, 523–531. [Google Scholar]
- Wu, X.; Guo, Y.; Min, X.; Pei, L.; Chen, X. Neferine, a bisbenzylisoquinoline alkaloid, ameliorates dextran sulfate sodium-induced ulcerative colitis. Am. J. Chin. Med. 2018, 46, 1263–1279. [Google Scholar] [CrossRef]
- Ruiz Castro, P.A.; Kogel, U.; Lo Sasso, G.; Phillips, B.W.; Sewer, A.; Titz, B.; Garcia, L.; Kondylis, A.; Guedj, E.; Peric, D.; et al. Anatabine ameliorates intestinal inflammation and reduces the production of pro-inflammatory factors in a dextran sulfate sodium mouse model of colitis. J. Inflamm. 2020, 17, 29. [Google Scholar] [CrossRef]
- Su, S.; Wang, X.; Xi, X.; Zhu, L.; Chen, Q.; Zhang, H.; Qin, Y.; Yang, B.; Che, N.; Cao, H.; et al. Phellodendrine promotes autophagy by regulating the AMPK/mTOR pathway and treats ulcerative colitis. J. Cell. Mol. Med. 2021, 25, 5707–5720. [Google Scholar] [CrossRef]
- de Carvalho, L.R.; de Brito, T.V.; Junior, J.S.D.C.; Júnior, G.J.D.; de Aguiar Magalhãres, D.; Sousa, S.G.; Silva, R.O.; da Silva, F.R.P.; Vasconcelos, D.F.P.; Véras, L.M.C.; et al. Epiisopiloturine, an imidazole alkaloid, reverses inflammation and lipid peroxidation parameters in the Crohn disease model induced by trinitrobenzenosulfonic acid in Wistar rats. Biomed. Pharmacother. 2018, 102, 278–285. [Google Scholar] [CrossRef]
- Jia, Q.; Zhang, H.; Su, Y.; Liu, X.; Bai, J.; Lang, W.; Shi, Q.; Feng, M. Strictosamide alleviates the inflammation in an acute ulcerative colitis (UC) model. J. Physiol. Biochem. 2021, 77, 283–294. [Google Scholar] [CrossRef]
- Tang, Q.; Zhang, W.; Zhang, C.; Guan, Y.; Ding, J.; Yuan, C.; Tan, C.; Gao, X.; Tan, S. Oxymatrine loaded nitric oxide-releasing liposomes for the treatment of ulcerative colitis. Int. J. Pharm. 2020, 586, 119617. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Duan, X.; Fan, H.; Xu, M.; Tang, Q.; Zhang, L.; Shou, Z.; Liu, X.; Zuo, D.; Yang, J.; et al. Oxymatrine protects against DSS-induced colitis via inhibiting the PI3K/AKT signaling pathway. Int. Immunopharmacol. 2017, 53, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.-M.; Zhu, Y.-B.; Li, H.-G.; Luan, S.-M.; Song, C.-Y.; Deng, X.; Chen, Y.-X. Protection of Sophocarpine on Colonic Barrier in DSS-induced Acute Colitis in Mice by Increasing Expression of HNF4α. Chin. Herb. Med. 2015, 7, 261–266. [Google Scholar] [CrossRef]
- Shepherd, C.; Giacomin, P.; Navarro, S.; Miller, C.; Loukas, A.; Wangchuk, P. A medicinal plant compound, capnoidine, prevents the onset of inflammation in a mouse model of colitis. J. Ethnopharmacol. 2018, 211, 17–28. [Google Scholar] [CrossRef]
- Li, C.; Ai, G.; Wang, Y.; Lu, Q.; Luo, C.; Tan, L.; Lin, G.; Liu, Y.; Li, Y.; Zeng, H.; et al. Oxyberberine, a novel gut microbiota-mediated metabolite of berberine, possesses superior anti-colitis effect: Impact on intestinal epithelial barrier, gut microbiota profile and TLR4-MyD88-NF-κB pathway. Pharmacol. Res. 2020, 152, 104603. [Google Scholar] [CrossRef]
- Fu, X.; Sun, F.; Wang, F.; Zhang, J.; Zheng, B.; Zhong, J.; Yue, T.; Zheng, X.; Xu, J.-F.; Wang, C.-Y. Aloperine Protects Mice against DSS-Induced Colitis by PP2A-Mediated PI3K/Akt/mTOR Signaling Suppression. Mediat. Inflamm. 2017, 2017, 5706152. [Google Scholar] [CrossRef]
- Yu, X.-T.; Xu, Y.-F.; Huang, Y.-F.; Qu, C.; Xu, L.-Q.; Su, Z.-R.; Zeng, H.-F.; Zheng, L.; Yi, T.-G.; Li, H.-L.; et al. Berberrubine attenuates mucosal lesions and inflammation in dextran sodium sulfate-induced colitis in mice. PLoS ONE 2018, 13, e0194069. [Google Scholar] [CrossRef]
- Zhou, Y.; Liu, H.; Song, J.; Cao, L.; Tang, L.; Qi, C. Sinomenine alleviates dextran sulfate sodium-induced colitis via the Nrf2/NQO-1 signaling pathway. Mol. Med. Rep. 2018, 18, 3691–3698. [Google Scholar] [CrossRef]
- Jiao, Y.-F.; Lu, M.; Zhao, Y.-P.; Liu, N.; Niu, Y.-T.; Niu, Y.; Zhou, R.; Yu, J.-Q. N-Methylcytisine Ameliorates Dextran-Sulfate-Sodium-Induced Colitis in Mice by Inhibiting the Inflammatory Response. Molecules 2018, 23, 510. [Google Scholar] [CrossRef]
- Chu, Y.; Zhu, Y.; Zhang, Y.; Liu, X.; Guo, Y.; Chang, L.; Yun, X.; Wei, Z.; Xia, Y.; Dai, Y. Tetrandrine attenuates intestinal epithelial barrier defects caused by colitis through promoting the expression of Occludin via the AhR-miR-429 pathway. FASEB J. 2021, 35, e21502. [Google Scholar] [CrossRef]
- Zhang, D.K.; Cheng, L.N.; Huang, X.L.; Shi, W.; Xiang, J.Y.; Gan, H.T. Tetrandrine ameliorates dextran-sulfate-sodium-induced colitis in mice through inhibition of nuclear factor -κB activation. Int. J. Color. Dis. 2009, 24, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Lv, Q.; Wang, K.; Qiao, S.-M.; Dai, Y.; Wei, Z.-F. Norisoboldine, a natural aryl hydrocarbon receptor agonist, alleviates TNBS-induced colitis in mice, by inhibiting the activation of NLRP3 inflammasome. Chin. J. Nat. Med. 2018, 16, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Dong, N.; Wu, B.; Mo, Z.; Xie, J.; Lu, Q. Dihydroberberine, an isoquinoline alkaloid, exhibits protective effect against dextran sulfate sodium-induced ulcerative colitis in mice. Phytomedicine 2021, 90, 153631. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-J.; Yuan, Z.-W.; Qu, C.; Yu, X.-T.; Huang, T.; Chen, P.V.; Su, Z.-R.; Dou, Y.-X.; Wu, J.-Z.; Zeng, H.-F.; et al. Palmatine ameliorated murine colitis by suppressing tryptophan metabolism and regulating gut microbiota. Pharmacol. Res. 2018, 137, 34–46. [Google Scholar] [CrossRef]
- Mai, C.-T.; Wu, M.-M.; Wang, C.-L.; Su, Z.-R.; Cheng, Y.-Y.; Zhang, X.-J. Palmatine attenuated dextran sulfate sodium (DSS)-induced colitis via promoting mitophagy-mediated NLRP3 inflammasome inactivation. Mol. Immunol. 2019, 105, 76–85. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, J.; Huang, Z.; Li, Y.; Liang, Y.; Luo, C.; Ni, C.; Xie, J.; Su, Z.; Chen, J.; et al. Coptisine ameliorates DSS-induced ulcerative colitis via improving intestinal barrier dysfunction and suppressing inflammatory response. Eur. J. Pharmacol. 2021, 896, 173912. [Google Scholar] [CrossRef]
- Niu, X.; Fan, T.; Li, W.; Huang, H.; Zhang, Y.; Xing, W. Protective effect of sanguinarine against acetic acid-induced ulcerative colitis in mice. Toxicol. Appl. Pharmacol. 2013, 267, 256–265. [Google Scholar] [CrossRef]
- Liu, F.; Yao, Y.; Lu, Z.; Zhang, Q.; Liu, C.; Zhu, C.; Lin, C. 5-Hydroxy-4-methoxycanthin-6-one alleviates dextran sodium sulfate-induced colitis in rats via regulation of metabolic profiling and suppression of NF-κB/p65 signaling pathway. Phytomedicine 2021, 82, 153438. [Google Scholar] [CrossRef]
- Rabelo Socca, E.A.; Luiz-Ferreira, A.; de Faria, F.M.; de Almeida, A.C.; Dunder, R.J.; Manzo, L.P.; Souza Brito, A.R.M. Inhibition of tumor necrosis factor-alpha and cyclooxigenase-2 by Isatin: A molecular mechanism of protection against TNBS-induced colitis in rats. Chem.-Biol. Interact. 2014, 209, 48–55. [Google Scholar] [CrossRef]
- Lucena, A.M.M.; Souza, C.R.M.; Jales, J.T.; Guedes, P.M.M.; De Miranda, G.E.C.; De Moura, A.M.A.; Araújo-Júnior, J.X.; Nascimento, G.J.; Scortecci, K.C.; Santos, B.V.O.; et al. The Bisindole Alkaloid Caulerpin, from Seaweeds of the Genus Caulerpa, Attenuated Colon Damage in Murine Colitis Model. Mar. Drugs 2018, 16, 318. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, L.; Wang, X.; Yu, L.; Wang, C.; Gong, Y. The combination of indirubin and isatin attenuates dextran sodium sulfate induced ulcerative colitis in mice. Biochem. Cell Biol. 2018, 96, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Guo, Y.; Wang, C.; Lin, Y.; Yu, L.; Sheng, T.; Wu, Z.; Gong, Y. Indirubin ameliorates dextran sulfate sodium-induced ulcerative colitis in mice through the inhibition of inflammation and the induction of Foxp3-expressing regulatory T cells. Acta Histochem. 2016, 118, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yan, T.; Sun, D.; Xie, C.; Wang, T.; Liu, X.; Wang, J.; Wang, Q.; Luo, Y.; Wang, P.; et al. Rutaecarpine inhibits KEAP1-NRF2 interaction to activate NRF2 and ameliorate dextran sulfate sodium-induced colitis. Free Radic. Biol. Med. 2020, 148, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Wu, H.; Hou, J.; Wang, J.; Wang, J.; Li, M.; Yao, X.; Gao, J.; Zhang, Q. Daurisoline alleviated experimental colitis in vivo and in vitro: Involvement of NF-κB and Wnt/β-Catenin pathway. Int. Immunopharmacol. 2022, 108, 108714. [Google Scholar] [CrossRef] [PubMed]
- Wangchuk, P.; Navarro, S.; Shepherd, C.; Keller, P.A.; Pyne, S.G.; Loukas, A. Diterpenoid alkaloids of Aconitum laciniatum and mitigation of inflammation by 14-O-acetylneoline in a murine model of ulcerative colitis. Sci. Rep. 2015, 5, 12845. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Qian, J.; Ju, X.; Bao, X.; Li, L.; Zheng, S.; Chen, X.; Xiao, Z.; Chen, X.; Zhu, W.; et al. Osthole Protects against Acute Lung Injury by Suppressing NF-κB-Dependent Inflammation. Mediat. Inflamm. 2018, 2018, 4934592. [Google Scholar] [CrossRef]
- Sun, W.; Cai, Y.; Zhang, X.-X.; Chen, H.; Lin, Y.-D.; Li, H. Osthole pretreatment alleviates TNBS-induced colitis in mice via both cAMP/PKA-dependent and independent pathways. Acta Pharmacol. Sin. 2017, 38, 1120–1128. [Google Scholar] [CrossRef]
- Fan, H.; Gao, Z.; Ji, K.; Li, X.; Wu, J.; Liu, Y.; Wang, X.; Liang, H.; Liu, Y.; Li, X.; et al. The in vitro and in vivo anti-inflammatory effect of osthole, the major natural coumarin from Cnidium monnieri (L.) Cuss, via the blocking of the activation of the NF-κB and MAPK/p38 pathways. Phytomedicine 2019, 58, 152864. [Google Scholar] [CrossRef]
- Abdel-Wahab, B.A.; Alkahtani, S.A.; Alqahtani, A.A.; Hassanein, E.H.M. Umbelliferone ameliorates ulcerative colitis induced by acetic acid via modulation of TLR4/NF-κB-p65/iNOS and SIRT1/PPARγ signaling pathways in rats. Environ. Sci. Pollut. Res. 2022, 29, 37644–37659. [Google Scholar] [CrossRef]
- Witaicenis, A.; de Oliveira, E.C.S.; Tanimoto, A.; Zorzella-Pezavento, S.F.G.; de Oliveira, S.L.; Sartori, A.; Di Stasi, L.C. 4-methylesculetin, a coumarin derivative, ameliorates dextran sulfate sodium-induced intestinal inflammation. Chem.-Biol. Interact. 2018, 280, 59–63. [Google Scholar] [CrossRef]
- Witaicenis, A.; Luchini, A.C.; Hiruma-Lima, C.A.; Felisbino, S.L.; Garrido-Mesa, N.; Utrilla, P.; Gálvez, J.; Di Stasi, L.C. Suppression of TNBS-induced colitis in rats by 4-methylesculetin, a natural coumarin: Comparison with prednisolone and sulphasalazine. Chem.-Biol. Interact. 2012, 195, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Ji, J.; Ge, X.; Chen, Y.; Zhu, B.; Wu, Q.; Zhang, J.; Shan, J.; Cheng, H.; Shi, L. Daphnetin ameliorates experimental colitis by modulating microbiota composition and Treg/Th17 balance. FASEB J. 2019, 33, 9308–9322. [Google Scholar] [CrossRef] [PubMed]
- Adakudugu, E.A.; Ameyaw, E.O.; Obese, E.; Biney, R.P.; Henneh, I.T.; Aidoo, D.B.; Oge, E.N.; Attah, I.Y.; Obiri, D.D. Protective effect of bergapten in acetic acid-induced colitis in rats. Heliyon 2020, 6, e04710. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Luo, Y. Imperatorin relieved ulcerative colitis by regulating the Nrf-2/ARE/HO-1 pathway in rats. Inflammation 2021, 44, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Witaicenis, A.; Luchini, A.C.; Hiruma-Lima, C.A.; Felisbino, S.L.; Justulin, L.A.; Garrido-Mesa, N.; Utrilla, P.; Gálvez, J.; Di Stasi, L.C. Mechanism and Effect of Esculetin in an Experimental Animal Model of Inflammatory Bowel Disease. Eur. J. Inflamm. 2013, 11, 433–446. [Google Scholar] [CrossRef]
- Liu, M.; Zhang, G.; Zheng, C.; Song, M.; Liu, F.; Huang, X.; Bai, S.; Huang, X.; Lin, C.; Zhu, C.; et al. Activating the pregnane X receptor by imperatorin attenuates dextran sulphate sodium-induced colitis in mice. Br. J. Pharmacol. 2018, 175, 3563–3580. [Google Scholar] [CrossRef]
- Luchini, A.C.; Rodrigues-Orsi, P.; Cestari, S.H.; Seito, L.N.; Witaicenis, A.; Pellizzon, C.H.; Di Stasi, L.C. Intestinal anti-inflammatory activity of coumarin and 4-hydroxycoumarin in the trinitrobenzenesulphonic acid model of rat colitis. Biol. Pharm. Bull. 2008, 31, 1343–1350. [Google Scholar] [CrossRef]
- Hou, C.; Chen, L.; Yang, L.; Ji, X. An insight into anti-inflammatory effects of natural polysaccharides. Int. J. Biol. Macromol. 2020, 153, 248–255. [Google Scholar] [CrossRef]
- Wang, Y.; Zhu, H.; Wang, X.; Yu, Y.; Xie, J. Natural Food Polysaccharides Ameliorate Inflammatory Bowel Disease and Its Mechanisms. Foods 2021, 10, 1288. [Google Scholar] [CrossRef]
- Shao, S.; Wang, D.; Zheng, W.; Li, X.; Zhang, H.; Zhao, D.; Wang, M. A unique polysaccharide from Hericium erinaceus mycelium ameliorates acetic acid-induced ulcerative colitis rats by modulating the composition of the gut microbiota, short chain fatty acids levels and GPR41/43 respectors. Int. Immunopharmacol. 2019, 71, 411–422. [Google Scholar] [CrossRef]
- Zhao, D.; Dai, W.; Tao, H.; Zhuang, W.; Qu, M.; Chang, Y.-N. Polysaccharide isolated from Auricularia auricular-judae (Bull.) prevents dextran sulfate sodium-induced colitis in mice through modulating the composition of the gut microbiota. J. Food Sci. 2020, 85, 2943–2951. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, J.; Li, J.; Zhu, J.; Wang, R.; Xi, Q.; Wu, H.; Shi, T.; Chen, W. Astragalus polysaccharide prevents ferroptosis in a murine model of experimental colitis and human Caco-2 cells via inhibiting NRF2/HO-1 pathway. Eur. J. Pharmacol. 2021, 911, 174518. [Google Scholar] [CrossRef]
- Zhong, Y.; Xiao, Q.; Kang, Z.; Huang, J.; Ge, W.; Wan, Q.; Wang, H.; Zhou, W.; Zhao, H.; Liu, D. Astragalus polysaccharide alleviates ulcerative colitis by regulating the balance of Tfh/Treg cells. Int. Immunopharmacol. 2022, 111, 109108. [Google Scholar] [CrossRef]
- Kanwal, S.; Joseph, T.P.; Aliya, S.; Song, S.; Saleem, M.Z.; Nisar, M.A.; Wang, Y.; Meyiah, A.; Ma, Y.; Xin, Y. Attenuation of DSS induced colitis by Dictyophora indusiata polysaccharide (DIP) via modulation of gut microbiota and inflammatory related signaling pathways. J. Funct. Foods 2020, 64, 103641. [Google Scholar] [CrossRef]
- Li, Q.; Li, L.; Li, Q.; Wang, J.; Nie, S.; Xie, M. Influence of Natural Polysaccharides on Intestinal Microbiota in Inflammatory Bowel Diseases: An Overview. Foods 2022, 11, 1084. [Google Scholar] [CrossRef]
- Xu, Y.; Xie, L.; Zhang, Z.; Zhang, W.; Tang, J.; He, X.; Zhou, J.; Peng, W. Tremella fuciformis Polysaccharides Inhibited Colonic Inflammation in Dextran Sulfate Sodium-Treated Mice via Foxp3+ T Cells, Gut Microbiota, and Bacterial Metabolites. Front. Immunol. 2021, 12, 648162. [Google Scholar] [CrossRef] [PubMed]
- Su, L.; Mao, C.; Wang, X.; Li, L.; Tong, H.; Mao, J.; Ji, D.; Lu, T.; Hao, M.; Huang, Z.; et al. The Anti-colitis Effect of Schisandra chinensis Polysaccharide Is Associated with the Regulation of the Composition and Metabolism of Gut Microbiota. Front. Cell. Infect. Microbiol. 2020, 10, 519479. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Zhao, P.; Li, X.; Guo, L.; Gao, W. The potential roles of natural plant polysaccharides in inflammatory bowel disease: A review. Carbohydr. Polym. 2022, 277, 118821. [Google Scholar] [CrossRef] [PubMed]
- Yousef, M.; Pichyangkura, R.; Soodvilai, S.; Chatsudthipong, V.; Muanprasat, C. Chitosan oligosaccharide as potential therapy of inflammatory bowel disease: Therapeutic efficacy and possible mechanisms of action. Pharm. Res 2012, 66, 66–79. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Xie, J.; Wang, Y.; Jiang, H.; Chen, K.; Li, D.; Wang, J.; Liu, Y.; He, J.; Zhou, J.; et al. Mannose ameliorates experimental colitis by protecting intestinal barrier integrity. Nat. Commun. 2022, 13, 4804. [Google Scholar] [CrossRef]
- Tao, J.-H.; Duan, J.-A.; Jiang, S.; Feng, N.-N.; Qiu, W.-Q.; Ling, Y. Polysaccharides from Chrysanthemum morifolium Ramat ameliorate colitis rats by modulating the intestinal microbiota community. Oncotarget 2017, 8, 80790. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.-H.; Duan, J.-A.; Zhang, W.; Jiang, S.; Guo, J.-M.; Wei, D.-D. Polysaccharides from Chrysanthemum morifolium Ramat Ameliorate Colitis Rats via Regulation of the Metabolic Profiling and NF-κ B/TLR4 and IL-6/JAK2/STAT3 Signaling Pathways. Front. Pharmacol. 2018, 9, 746. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.; Sun, C.; Tang, X.; Zhang, X.; Han, D.; Liang, S.; Qu, R.; Hui, X.; Shan, Y.; Hu, L.; et al. Anti-Inflammatory and Intestinal Microbiota Modulation Properties of Jinxiang Garlic (Allium sativum L.) Polysaccharides toward Dextran Sodium Sulfate-Induced Colitis. J. Agric. Food Chem. 2020, 68, 12295–12309. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.; Liu, J.; Tan, Y.; Ao, H.; Wang, J.; Peng, C. Polysaccharides from Atractylodes macrocephala Koidz. Ameliorate ulcerative colitis via extensive modification of gut microbiota and host metabolism. Food Res. Int. 2020, 138, 109777. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Xiao, N.; Zeng, L.; Xiao, J.; Huang, J.; Xu, Y.; Chen, Y.; Ren, Y.; Du, B. Structural characteristics of a mannoglucan isolated from Chinese yam and its treatment effects against gut microbiota dysbiosis and DSS-induced colitis in mice. Carbohydr. Polym. 2020, 250, 116958. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-J.; Li, Q.-M.; Zha, X.-Q.; Luo, J.-P. Dendrobium fimbriatum Hook polysaccharide ameliorates dextran-sodium-sulfate-induced colitis in mice via improving intestinal barrier function, modulating intestinal microbiota, and reducing oxidative stress and inflammatory responses. Food Funct. 2022, 13, 143–160. [Google Scholar] [CrossRef]
- Zou, Q.; Zhang, X.; Liu, X.; Li, Y.; Tan, Q.; Dan, Q.; Yuan, T.; Liu, X.; Liu, R.H.; Liu, Z. Ficus carica polysaccharide attenuates DSS-induced ulcerative colitis in C57BL/6 mice. Food Funct. 2020, 11, 6666–6679. [Google Scholar] [CrossRef]
- Zeng, Z.; Xie, Z.; Chen, G.; Sun, Y.; Zeng, X.; Liu, Z. Anti-inflammatory and gut microbiota modulatory effects of polysaccharides from Fuzhuan brick tea on colitis in mice induced by dextran sulfate sodium. Food Funct. 2022, 13, 649–663. [Google Scholar] [CrossRef]
- Zhou, X.; Lu, Q.; Kang, X.; Tian, G.; Ming, D.; Yang, J. Protective Role of a New Polysaccharide Extracted from Lonicera japonica Thunb in Mice with Ulcerative Colitis Induced by Dextran Sulphate Sodium. BioMed Res. Int. 2021, 2021, 8878633. [Google Scholar] [CrossRef]
- Jin, M.-Y.; Wu, X.-Y.; Li, M.-Y.; Li, X.-T.; Huang, R.-M.; Sun, Y.-M.; Xu, Z.-L. Noni (Morinda citrifolia L.) Fruit Polysaccharides Regulated IBD Mice Via Targeting Gut Microbiota: Association of JNK/ERK/NF-κB Signaling Pathways. J. Agric. Food Chem. 2021, 69, 10151–10162. [Google Scholar] [CrossRef]
- Cui, L.; Guan, X.; Ding, W.; Luo, Y.; Wang, W.; Bu, W.; Song, J.; Tan, X.; Sun, E.; Ning, Q.; et al. Scutellaria baicalensis Georgi polysaccharide ameliorates DSS-induced ulcerative colitis by improving intestinal barrier function and modulating gut microbiota. Int. J. Biol. Macromol. 2021, 166, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Liu, Y.; Chen, B.; Zhang, G.; Ou, S.; Luo, J.; Peng, X. Ganoderma lucidum polysaccharide improves rat DSS-induced colitis by altering cecal microbiota and gene expression of colonic epithelial cells. Food Nutr. Res. 2019, 63, 1559. [Google Scholar] [CrossRef] [PubMed]
- Wei, B.; Zhang, R.; Zhai, J.; Zhu, J.; Yang, F.; Yue, D.; Liu, X.; Lu, C.; Sun, X. Suppression of Th17 Cell Response in the Alleviation of Dextran Sulfate Sodium-Induced Colitis by Ganoderma lucidum Polysaccharides. J. Immunol. Res. 2018, 2018, 2906494. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ji, X.; Yan, M.; Chen, X.; Kang, M.; Teng, L.; Wu, X.; Chen, J.; Deng, C. Protective effect and mechanism of polysaccharide from Dictyophora indusiata on dextran sodium sulfate-induced colitis in C57BL/6 mice. Int. J. Biol. Macromol. 2019, 140, 973–984. [Google Scholar] [CrossRef]
- Dalmasso, G.; Charrier–Hisamuddin, L.; Thu Nguyen, H.T.; Yan, Y.; Sitaraman, S.; Merlin, D. PepT1-Mediated Tripeptide KPV Uptake Reduces Intestinal Inflammation. Gastroenterology 2008, 134, 166–178. [Google Scholar] [CrossRef]
- Kovacs-Nolan, J.; Zhang, H.; Ibuki, M.; Nakamori, T.; Yoshiura, K.; Turner, P.V.; Matsui, T.; Mine, Y. The PepT1-transportable soy tripeptide VPY reduces intestinal inflammation. Biochim. Et Biophys. Acta (BBA)-Gen. Subj. 2012, 1820, 1753–1763. [Google Scholar] [CrossRef]
- Wada, S.; Sato, K.; Ohta, R.; Wada, E.; Bou, Y.; Fujiwara, M.; Kiyono, T.; Park, E.Y.; Aoi, W.; Takagi, T.; et al. Ingestion of Low Dose Pyroglutamyl Leucine Improves Dextran Sulfate Sodium-Induced Colitis and Intestinal Microbiota in Mice. J. Agric. Food Chem. 2013, 61, 8807–8813. [Google Scholar] [CrossRef]
- Guo, W.; Zeng, M.; Zhu, S.; Li, S.; Qian, Y.; Wu, H. Phycocyanin ameliorates mouse colitis via phycocyanobilin-dependent antioxidant and anti-inflammatory protection of the intestinal epithelial barrier. Food Funct. 2022, 13, 3294–3307. [Google Scholar] [CrossRef]
- Yaghoubi, A.; Amel Jamehdar, S.; Reza Akbari Eidgahi, M.; Ghazvini, K. Evaluation of the therapeutic effect of melittin peptide on the ulcerative colitis mouse model. Int. Immunopharmacol. 2022, 108, 108810. [Google Scholar] [CrossRef]
- Li, S.; Yuan, N.; Guo, W.; Chai, Y.; Song, Y.; Zhao, Y.; Zeng, M.; Wu, H. Antioxidant and anti-inflammatory protective effects of yellowtail (Seriola quinqueradiata) milt hydrolysates on human intestinal epithelial cells in vitro and dextran sodium sulphate-induced mouse colitis in vivo. Food Funct. 2022, 13, 9169–9182. [Google Scholar] [CrossRef]
- Cobos, C.; Bansal, P.S.; Jones, L.; Wangchuk, P.; Wilson, D.; Loukas, A.; Daly, N.L. Engineering of an Anti-Inflammatory Peptide Based on the Disulfide-Rich Linaclotide Scaffold. Biomedicines 2018, 6, 97. [Google Scholar] [CrossRef]
- Cobos Caceres, C.; Bansal, P.S.; Navarro, S.; Wilson, D.; Don, L.; Giacomin, P.; Loukas, A.; Daly, N.L. An engineered cyclic peptide alleviates symptoms of inflammation in a murine model of inflammatory bowel disease. J. Biol. Chem. 2017, 292, 10288–10294. [Google Scholar] [CrossRef]
- Sahu, K.K.; Minz, S.; Kaurav, M.; Pandey, R.S. Proteins and peptides: The need to improve them as promising therapeutics for ulcerative colitis. Artif. Cells Nanomed. Biotechnol. 2016, 44, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Ahmedy, O.A.; Ibrahim, S.M.; Salem, H.H.; Kandil, E.A. Antiulcerogenic effect of melittin via mitigating TLR4/TRAF6 mediated NF-κB and p38MAPK pathways in acetic acid-induced ulcerative colitis in mice. Chem.-Biol. Interact. 2020, 331, 109276. [Google Scholar] [CrossRef]
- Herlihy, N.; Feakins, R. Gut inflammation induced by drugs: Can pathology help to differentiate from inflammatory bowel disease? United Eur. Gastroenterol. J. 2022, 10, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Kiesler, P.; Fuss, I.J.; Strober, W. Experimental Models of Inflammatory Bowel Diseases. Cell. Mol. Gastroenterol. Hepatol. 2015, 1, 154–170. [Google Scholar] [CrossRef]
- Liang, J.; Liang, J.; Hao, H.; Lin, H.; Wang, P.; Wu, Y.; Jiang, X.; Fu, C.; Li, Q.; Ding, P.; et al. The Extracts of Morinda officinalis and Its Hairy Roots Attenuate Dextran Sodium Sulfate-Induced Chronic Ulcerative Colitis in Mice by Regulating Inflammation and Lymphocyte Apoptosis. Front. Immunol. 2017, 8, 905. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.-H.; Zhu, C.-X.; Quan, Y.-S.; Yang, Z.-Y.; Wu, S.; Luo, W.-W.; Tan, B.; Wang, X.-Y. Relationship between intestinal microbiota and ulcerative colitis: Mechanisms and clinical application of probiotics and fecal microbiota transplantation. World J. Gastroenterol. 2018, 24, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-J.; Li, S.; Gan, R.-Y.; Zhou, T.; Xu, D.-P.; Li, H.-B. Impacts of Gut Bacteria on Human Health and Diseases. Int. J. Mol. Sci. 2015, 16, 7493–7519. [Google Scholar] [CrossRef]
- Nascimento, R.d.P.d.; Machado, A.P.d.F.; Galvez, J.; Cazarin, C.B.B.; Maróstica Junior, M.R. Ulcerative colitis: Gut microbiota, immunopathogenesis and application of natural products in animal models. Life Sci. 2020, 258, 118129. [Google Scholar] [CrossRef]
- Wong, C.; Harris, P.J.; Ferguson, L.R. Potential Benefits of Dietary Fibre Intervention in Inflammatory Bowel Disease. Int. J. Mol. Sci. 2016, 17, 919. [Google Scholar] [CrossRef] [PubMed]
- Nie, Y.; Lin, Q.; Luo, F. Effects of Non-Starch Polysaccharides on Inflammatory Bowel Disease. Int. J. Mol. Sci. 2017, 18, 1372. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Li, Y.; Li, J.; Xue, J.-C.; Wang, Q.; Hou, X.-T.; Meng, H.; Nan, J.-X.; Zhang, Q.-G. Traditional Chinese Medicine and Natural Products: Potential Approaches for Inflammatory Bowel Disease. Front. Pharmacol. 2022, 13, 892790. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lei, H.; Hu, X.; Dong, W. Hesperetin ameliorates DSS-induced colitis by maintaining the epithelial barrier via blocking RIPK3/MLKL necroptosis signaling. Eur. J. Pharmacol. 2020, 873, 172992. [Google Scholar] [CrossRef]
- Araki, Y.; Mukaisyo, K.-I.; Sugihara, H.; Fujiyama, Y.; Hattori, T. Increased apoptosis and decreased proliferation of colonic epithelium in dextran sulfate sodium-induced colitis in mice. Oncol. Rep. 2010, 24, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zeng, Y.; Wen, Y.; Huang, X.; Liu, Y. Natural Products Modulate Cell Apoptosis: A Promising Way for the Treatment of Ulcerative Colitis. Front. Pharmacol. 2022, 13, 806148. [Google Scholar] [CrossRef]
- Lee, S.H. Intestinal Permeability Regulation by Tight Junction: Implication on Inflammatory Bowel Diseases. Intest. Res. 2015, 13, 11–18. [Google Scholar] [CrossRef]
- Paunovic, V.; Harnett, M.M. Mitogen-Activated Protein Kinases as Therapeutic Targets for Rheumatoid Arthritis. Drugs 2013, 73, 101–115. [Google Scholar] [CrossRef]
- Zhu, L.; Shen, H.; Gu, P.Q.; Liu, Y.J.; Zhang, L.; Cheng, J.F. Baicalin alleviates TNBS-induced colitis by inhibiting PI3K/AKT pathway activation. Exp. Ther. Med. 2020, 20, 581–590. [Google Scholar] [CrossRef]
- Huang, Y.; Xing, K.; Qiu, L.; Wu, Q.; Wei, H. Therapeutic implications of functional tea ingredients for ameliorating inflammatory bowel disease: A focused review. Crit. Rev. Food Sci. Nutr. 2022, 62, 5307–5321. [Google Scholar] [CrossRef]
- Grzybowska-Chlebowczyk, U.; Wysocka-Wojakiewicz, P.; Jasielska, M.; Cukrowska, B.; Więcek, S.; Kniażewska, M.; Chudek, J. Oxidative and Antioxidative Stress Status in Children with Inflammatory Bowel Disease as a Result of a Chronic Inflammatory Process. Mediat. Inflamm. 2018, 2018, 4120973. [Google Scholar] [CrossRef] [PubMed]
- Piechota-Polanczyk, A.; Fichna, J. Review article: The role of oxidative stress in pathogenesis and treatment of inflammatory bowel diseases. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2014, 387, 605–620. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.A.R.; Rodrigues, B.L.; Ayrizono, M.d.L.S.; Leal, R.F. The Immunological Basis of Inflammatory Bowel Disease. Gastroenterol. Res. Pract. 2016, 2016, 2097274. [Google Scholar] [CrossRef] [PubMed]
- Zaiatz Bittencourt, V.; Jones, F.; Doherty, G.; Ryan, E.J. Targeting Immune Cell Metabolism in the Treatment of Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2021, 27, 1684–1693. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Li, Y.R. Oxidative stress and redox signaling mechanisms of inflammatory bowel disease: Updated experimental and clinical evidence. Exp. Biol. Med. 2012, 237, 474–480. [Google Scholar] [CrossRef]
- Scott, O.; Roifman, C.M. NF-κB pathway and the Goldilocks principle: Lessons from human disorders of immunity and inflammation. J. Allergy Clin. Immunol. 2019, 143, 1688–1701. [Google Scholar] [CrossRef]
- Cui, L.; Wang, W.; Luo, Y.; Ning, Q.; Xia, Z.; Chen, J.; Feng, L.; Wang, H.; Song, J.; Tan, X.; et al. Polysaccharide from Scutellaria baicalensis Georgi ameliorates colitis via suppressing NF-κB signaling and NLRP3 inflammasome activation. Int. J. Biol. Macromol. 2019, 132, 393–405. [Google Scholar] [CrossRef]
- Cargnello, M.; Roux Philippe, P. Activation and Function of the MAPKs and Their Substrates, the MAPK-Activated Protein Kinases. Microbiol. Mol. Biol. Rev. 2011, 75, 50–83. [Google Scholar] [CrossRef]
- Gao, Z.; Yu, C.; Liang, H.; Wang, X.; Liu, Y.; Li, X.; Ji, K.; Xu, H.; Yang, M.; Liu, K.; et al. Andrographolide derivative CX-10 ameliorates dextran sulphate sodium-induced ulcerative colitis in mice: Involvement of NF-κB and MAPK signalling pathways. Int. Immunopharmacol. 2018, 57, 82–90. [Google Scholar] [CrossRef]
- Villarino, A.V.; Kanno, Y.; O’Shea, J.J. Mechanisms and consequences of Jak–STAT signaling in the immune system. Nat. Immunol. 2017, 18, 374–384. [Google Scholar] [CrossRef]
- Mao, L.; Kitani, A.; Strober, W.; Fuss, I.J. The Role of NLRP3 and IL-1β in the Pathogenesis of Inflammatory Bowel Disease. Front. Immunol. 2018, 9, 2566. [Google Scholar] [CrossRef]
- Shao, B.-Z.; Wang, S.-L.; Pan, P.; Yao, J.; Wu, K.; Li, Z.-S.; Bai, Y.; Linghu, E.-Q. Targeting NLRP3 Inflammasome in Inflammatory Bowel Disease: Putting out the Fire of Inflammation. Inflammation 2019, 42, 1147–1159. [Google Scholar] [CrossRef]
- Song, Y.; Zhao, Y.; Ma, Y.; Wang, Z.; Rong, L.; Wang, B.; Zhang, N. Biological functions of NLRP3 inflammasome: A therapeutic target in inflammatory bowel disease. Cytokine Growth Factor Rev. 2021, 60, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Venkataraman, B.; Ojha, S.; Belur, P.D.; Bhongade, B.; Raj, V.; Collin, P.D.; Adrian, T.E.; Subramanya, S.B. Phytochemical drug candidates for the modulation of peroxisome proliferator-activated receptor γ in inflammatory bowel diseases. Phytother. Res. 2020, 34, 1530–1549. [Google Scholar] [CrossRef] [PubMed]
- Dubuquoy, L.; Rousseaux, C.; Thuru, X.; Peyrin-Biroulet, L.; Romano, O.; Chavatte, P.; Chamaillard, M.; Desreumaux, P. PPARγ as a new therapeutic target in inflammatory bowel diseases. Gut 2006, 55, 1341. [Google Scholar] [CrossRef] [PubMed]
- Venkataraman, B.; Almarzooqi, S.; Raj, V.; Alhassani, A.T.; Alhassani, A.S.; Ahmed, K.J.; Subramanian, V.S.; Ojha, S.K.; Attoub, S.; Adrian, T.E.; et al. Thymoquinone, a Dietary Bioactive Compound, Exerts Anti-Inflammatory Effects in Colitis by Stimulating Expression of the Colonic Epithelial PPAR-γ Transcription Factor. Nutrients 2021, 13, 1343. [Google Scholar] [CrossRef] [PubMed]
- Venkataraman, B.; Almarzooqi, S.; Raj, V.; Dudeja, P.K.; Bhongade, B.A.; Patil, R.B.; Ojha, S.K.; Attoub, S.; Adrian, T.E.; Subramanya, S.B. α-Bisabolol Mitigates Colon Inflammation by Stimulating Colon PPAR-γ Transcription Factor: In Vivo and In Vitro Study. PPAR Res. 2022, 2022, 5498115. [Google Scholar] [CrossRef]
- Ekiert, H.M.; Szopa, A. Biological Activities of Natural Products. Molecules 2020, 25, 5769. [Google Scholar] [CrossRef]
- Katsandegwaza, B.; Horsnell, W.; Smith, K. Inflammatory Bowel Disease: A Review of Pre-Clinical Murine Models of Human Disease. Int. J. Mol. Sci. 2022, 23, 9344. [Google Scholar] [CrossRef] [PubMed]
- Zeng, M.; Yang, L.; He, D.; Li, Y.; Shi, M.; Zhang, J. Metabolic pathways and pharmacokinetics of natural medicines with low permeability. Drug Metab. Rev. 2017, 49, 464–476. [Google Scholar] [CrossRef] [PubMed]
- Taghipour, Y.D.; Bahramsoltani, R.; Marques, A.M.; Naseri, R.; Rahimi, R.; Haratipour, P.; Panah, A.I.; Farzaei, M.H.; Abdollahi, M. A systematic review of nano formulation of natural products for the treatment of inflammatory bowel disease: Drug delivery and pharmacological targets. DARU J. Pharm. Sci. 2018, 26, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Khare, T.; Palakurthi, S.S.; Shah, B.M.; Palakurthi, S.; Khare, S. Natural Product-Based Nanomedicine in Treatment of Inflammatory Bowel Disease. Int. J. Mol. Sci. 2020, 21, 3956. [Google Scholar] [CrossRef] [PubMed]
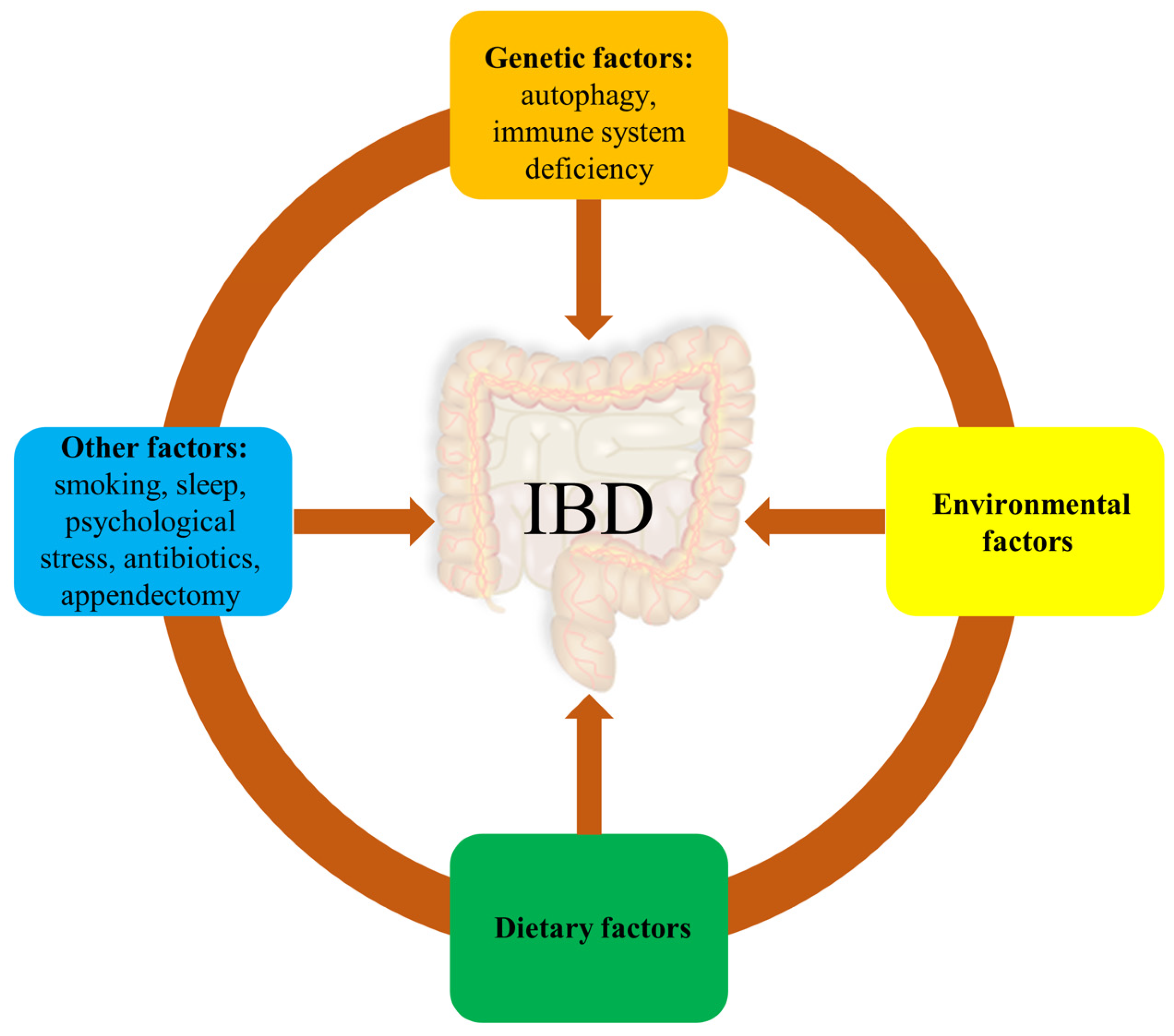
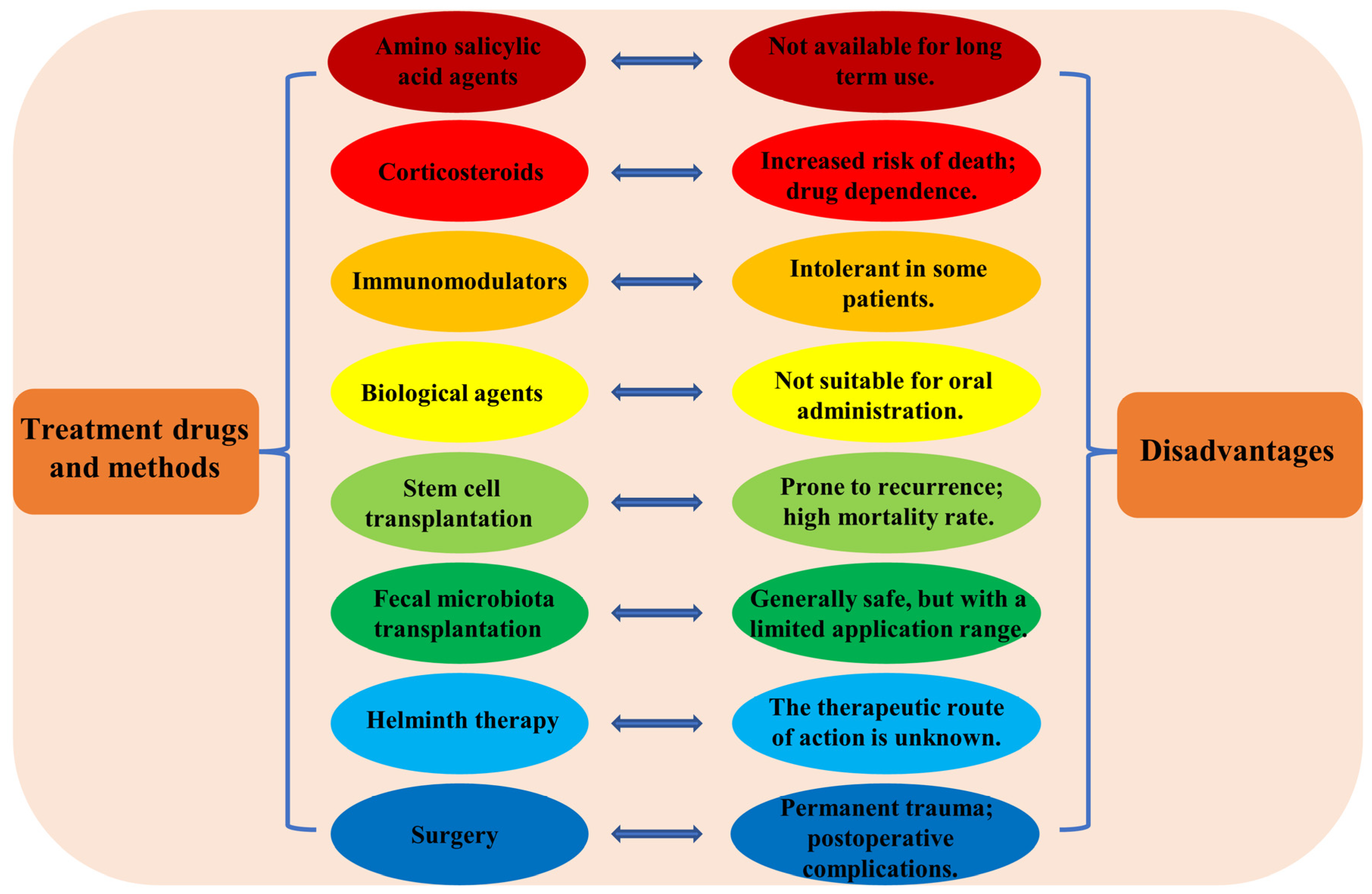

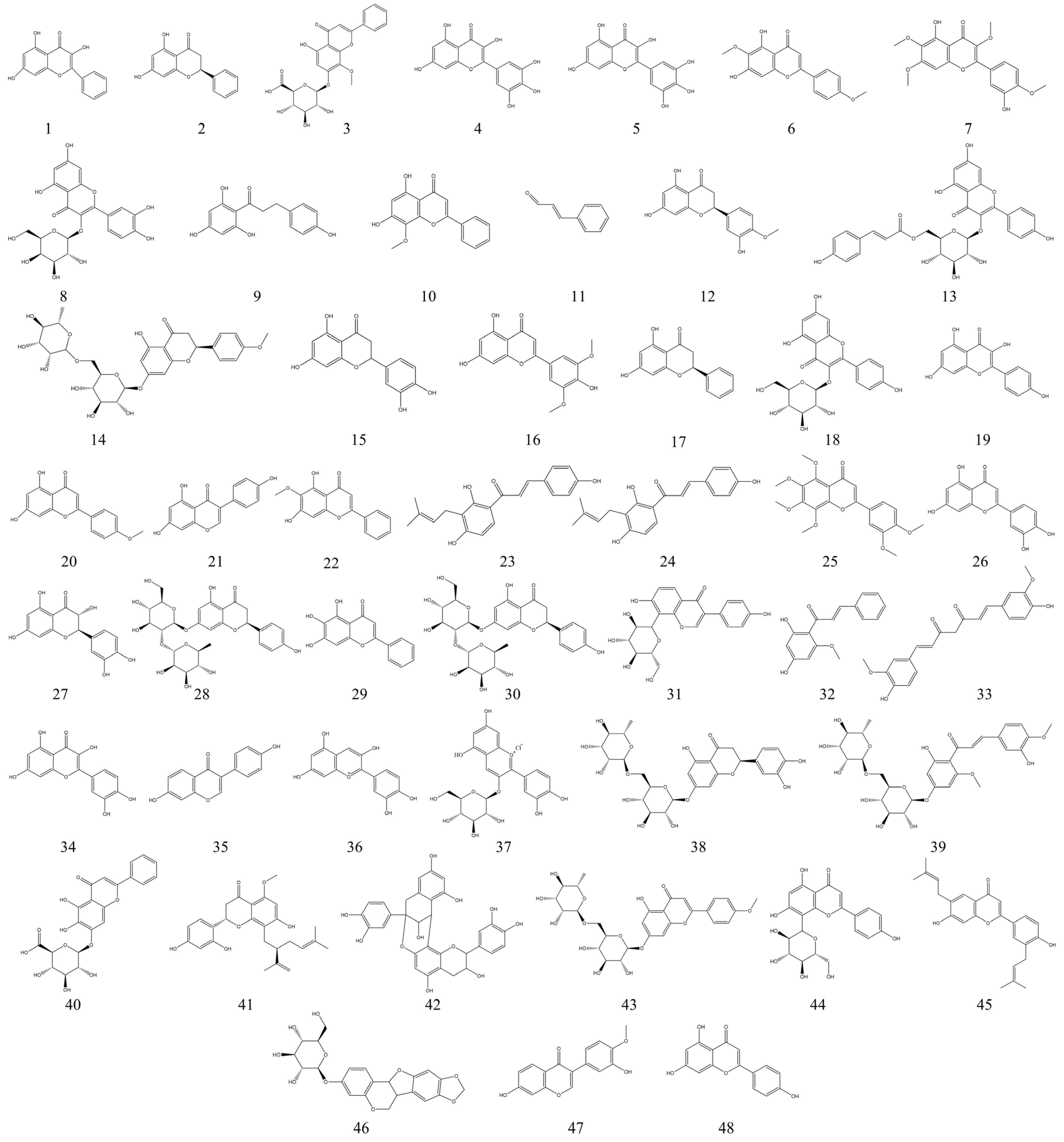
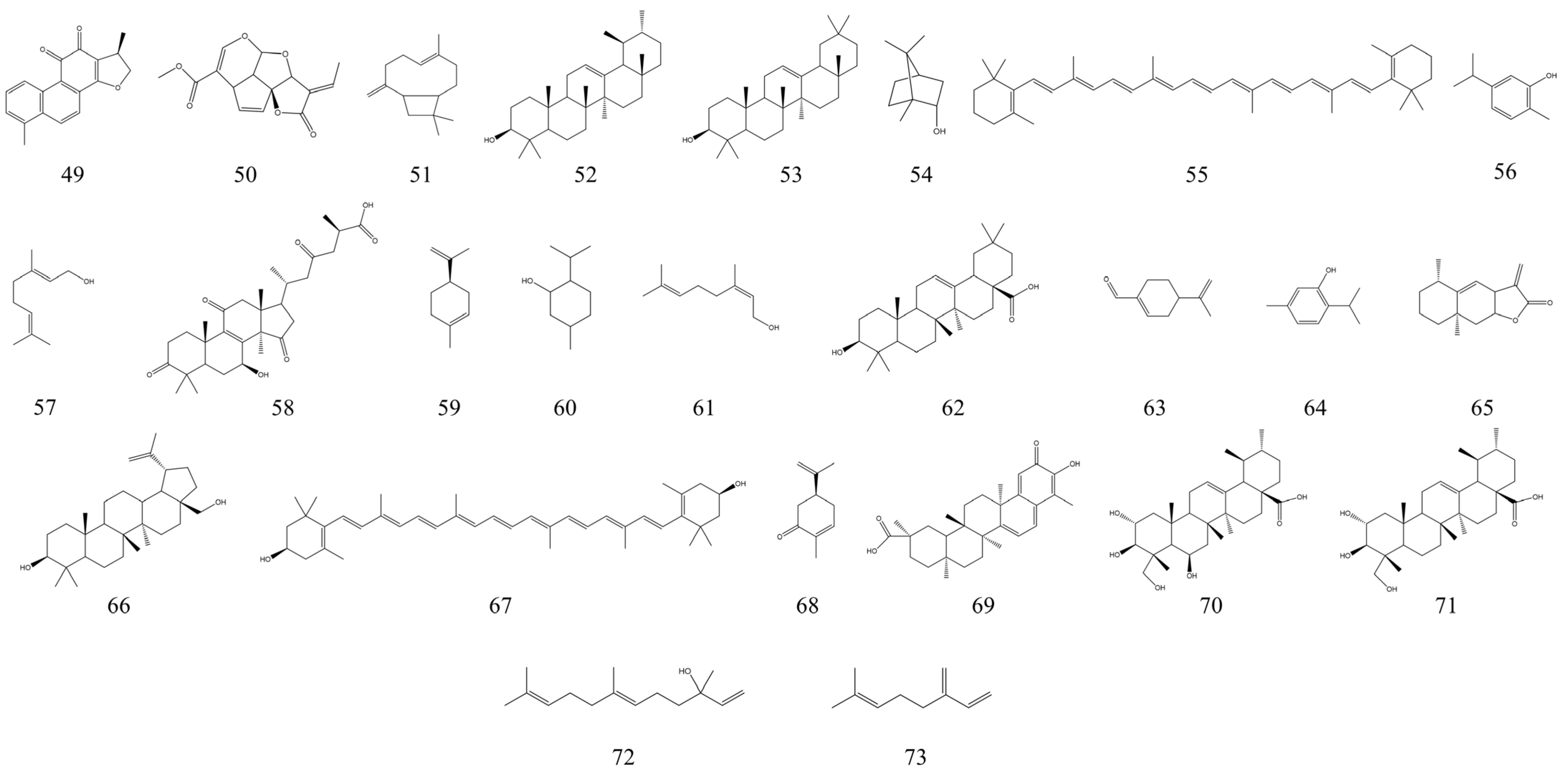
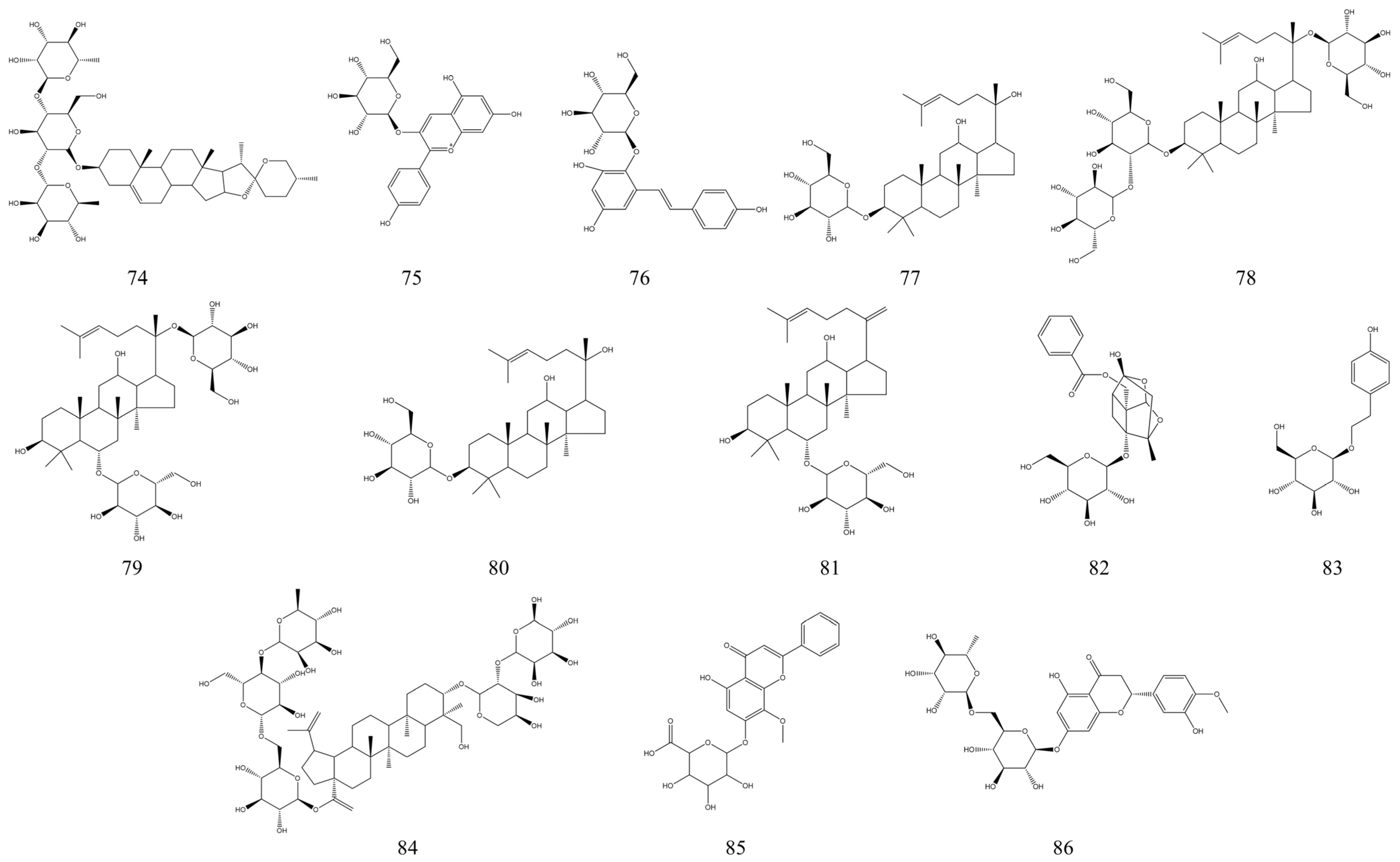
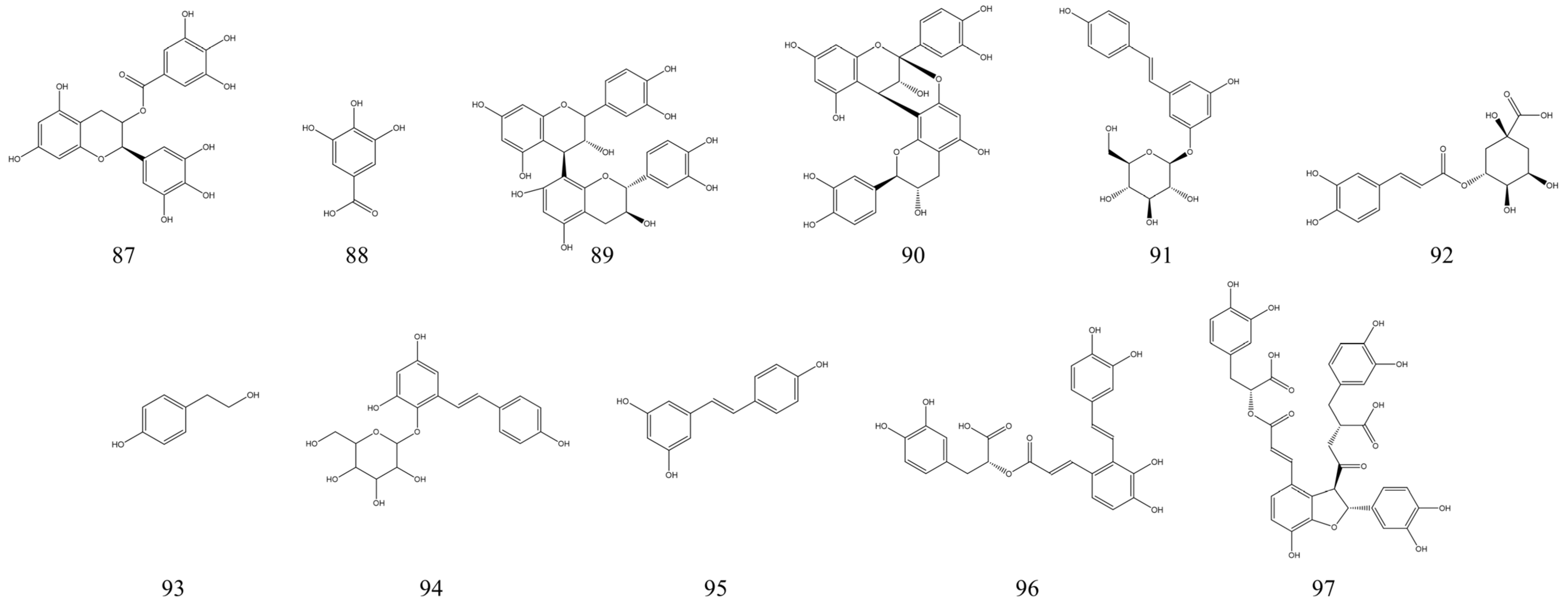

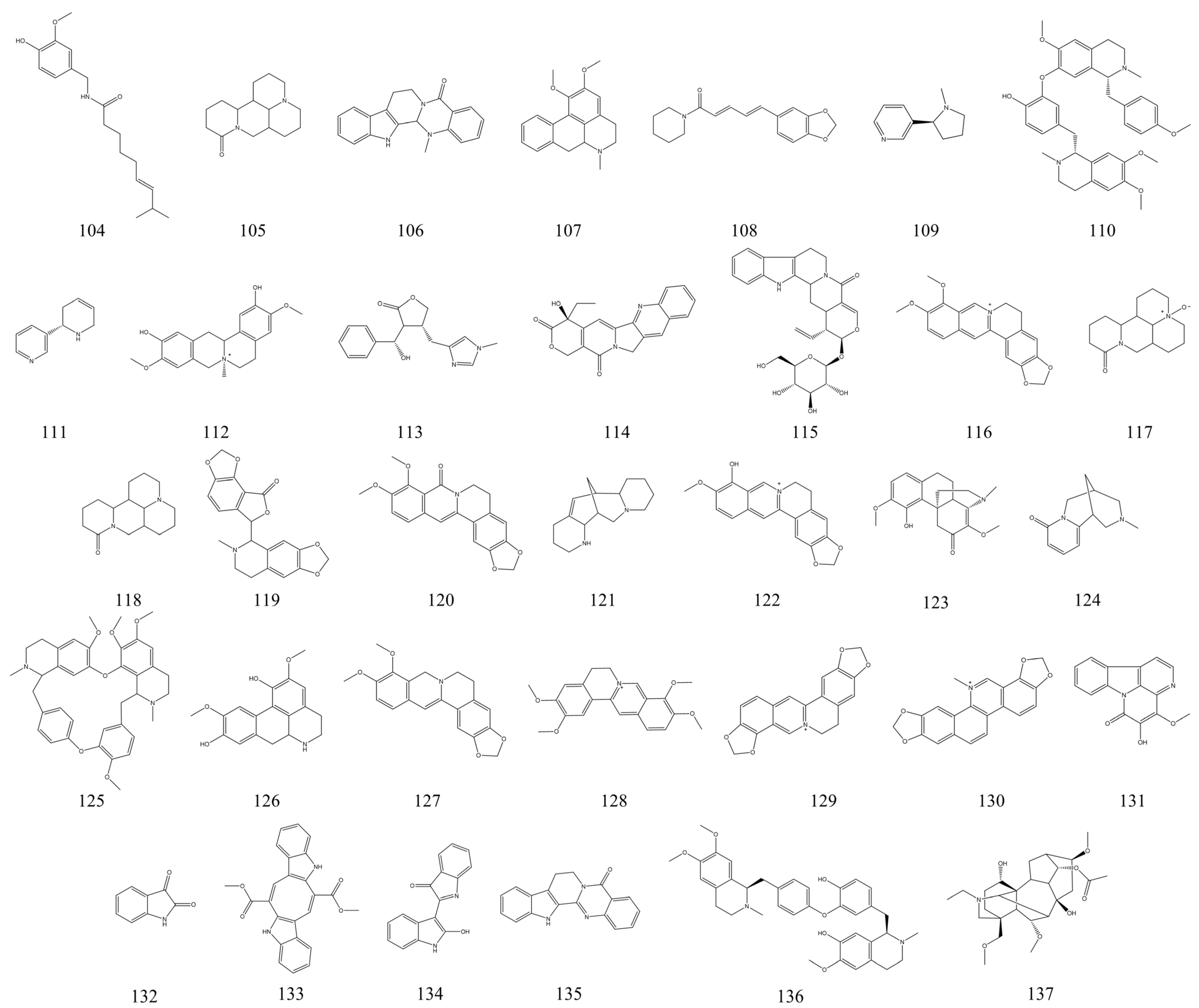
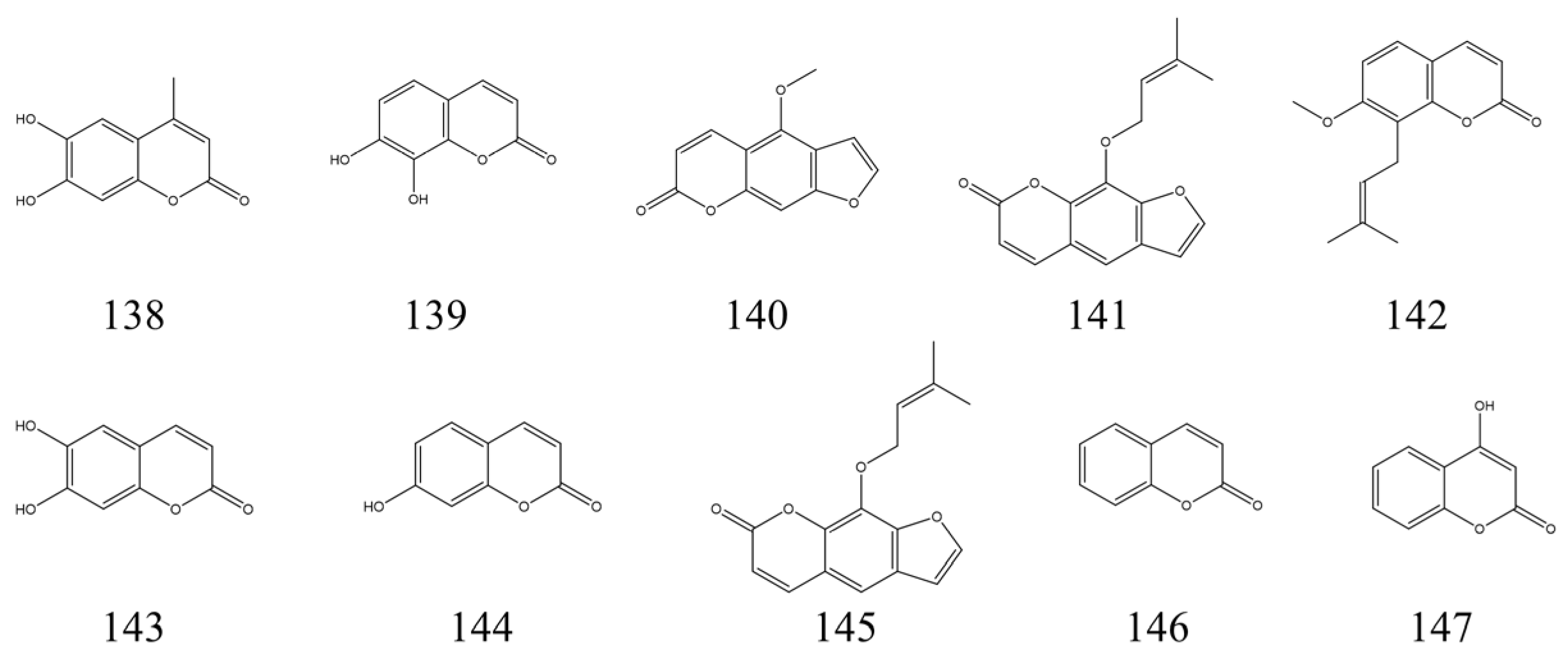
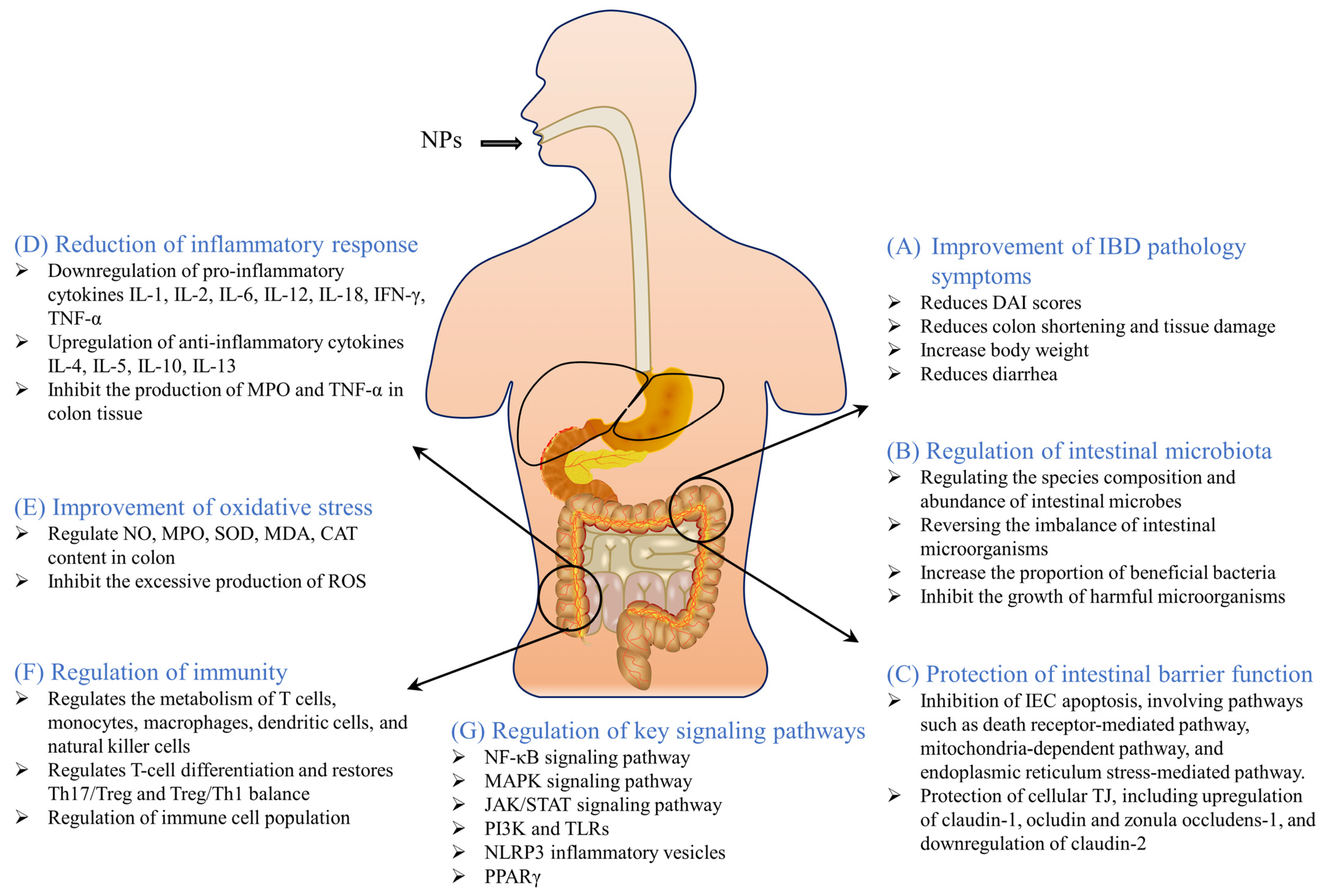
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 1 | Galangin | Hydroxyflavonol | Alpinia conchigera | 40 mg | DSS-induced ulcerative colitis in BALB/c mice | Inhibit inflammation and oxidative stress. | [79] |
| 40 mg | DSS-induced colitis in Swiss albino mice | Downregulation of toll-like receptor 4 expression, inhibition of NF-κB p65 activation, and reduction of inflammatory factor levels. | [80] | ||||
| 2 | Pinocembrin | Dihydroxyflavanone | Prunus leveilleana | 10 mg | DSS-induced rats ulcerative colitis model | Improves inflammation levels, intestinal barrier function, and regulates the intestinal microbiota. | [81] |
| 3 | Oroxindin | Flavonoid | Scutellaria discolor | 12.5 mg | DSS-induced rats ulcerative colitis model | Attenuates the inflammatory response by inhibiting the formation and activation of NLRP3 inflammatory vesicles. | [82] |
| 4 | Myricetin | Hexahydroxyflavone | Ficus auriculata | 80 mg | DSS-induced C57BL/6 mice ulcerative colitis model | Significantly increased the levels of IL-10, transforming growth factor b and the proportion of regulatory T cells. | [83] |
| 5 | Alpinetin | Flavonoid | Alpinia blepharocalyx | 100 mg | DSS-induced mice ulcerative colitis model | Reduces intestinal inflammation and oxidative stress dose-dependently associated with and regulates the expression of tight junctions between cells in UC mice. | [84] |
| 50 mg | DSS-induced C57BL/6 mice ulcerative colitis model | Helps to eliminate chemically induced IBD by activating PXR (a ligand of human pregnane X receptor). | [85] | ||||
| 6 | Pectolinarigenin | Dimethoxyflavone | Eupatorium cannabinum | 10 mg | DSS-induced C57BL/6 mice ulcerative colitis model | Dose-dependent reduction of DSS-induced colonic inflammation through modulation of NF-κB/Nrf2 signaling pathway and enhancement of myeloperoxidase (peroxisome) activity and redox regulators. | [86] |
| 7 | Casticin | Tetramethoxyflavone | Viticis Fructus | / | DSS-induced C57BL/6 mice ulcerative colitis model | Alleviation of DSS-induced UC by increasing the expression of the antioxidant enzymes peroxidase 3 and MnSOD and reduction of pro-inflammatory chemokine production by inhibiting AKT signaling. | [87] |
| 8 | Hyperoside | Tetramethoxyflavone | Lotus ucrainicus | 120 mg | DSS-induced acute colitis in mice | Reduction of colonic inflammation and apoptosis through activation of the Nrf2 signaling pathway. | [88] |
| 9 | Phloretin | Dihydrochalcone | Malus doumeri | 100 mg | DSS-induced C57BL/6 mice ulcerative colitis model | Inhibits inflammatory responses by regulating nuclear factor-κB (NF-κB), toll-like receptor 4 (TLR4), and peroxisome proliferator-activated receptor γ (PPARγ) pathways. | [89] |
| 10 | Wogonin | Dihydrochalcone | Scutellaria likiangensis | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Significantly reduced the intestinal inflammatory response in IBD mice by increasing the expression of IL-10. | [90] |
| 50 mg | DSS-induced acute colitis in BALB/c mice | Regulates the Nrf2 signaling pathway and reduces TLR-4/NF-κB triggering. | [91] | ||||
| 11 | Cinnamaldehyde | Flavonoid | Cinnamon trees | 90 mg | TNBS-induced ulcerative colitis in rats | Inhibition of TNBS-induced UC through antioxidant and anti-inflammatory properties and modulation of the JAk2/STAT3/SOCS3 pathway. | [92] |
| 10 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of Th17 cell differentiation via sphingosine-1-phosphate receptor 2. | [93] | ||||
| 12 | Hesperetin | Flavonoid | Brassica oleracea var. sabauda | 100 mg | TNBS-induced ulcerative colitis in rats | Inhibition of TNBS-induced UC through antioxidant and anti-inflammatory properties and modulation of the JAk2/STAT3/SOCS3 pathway. | [92] |
| 13 | Tiliroside | Glycosyloxyflavone | Galphimia gracilis | 50 mg | DSS-induced colitis model; TNBS-induced colitis model | Restoration of M1/M2 macrophage homeostasis through the HIF-1a/glycolytic pathway, resulting in improved UC. | [94] |
| 14 | Didymin | Flavonoid | Citrus latipes | 4 mg | DSS-induced acute colitis in C57BL/6 mice; DSS-induced chronic colitis in C57BL/6 mice | Didymin converts m1-like macrophages to m2-like macrophages and ameliorates UC through fatty acid oxidation. | [95] |
| 15 | Eriodictyol | Flavanone | Prunus campanulata | 50 mg | TNBS-induced animal model of enteritis in Wistar rats | Attenuation of TNBS-induced UC by inhibition of TLR4/NF-kB signaling pathway in rats. | [96] |
| 50 mg | DSS-induced acute colitis in C57BL/6 mice | Eriodictyol attenuates DSS-induced UC in mice by regulating the sonic hedgehog signaling pathway. | [97] | ||||
| 16 | Tricin | Trihydroxyflavone | Carex fraseriana | 150 mg | DSS-induced acute colitis in BALB/c mice | Improves colonic inflammation and regulates intestinal microbiota. | [98] |
| 17 | Pinocembrin | Dihydroxyflavanone | Prunus leveilleana | 50 mg | DSS-induced acute colitis in C57BL/6 mice | By modulating the intestinal flora, inhibiting the excessive activation of TLR4/MD2/NF-κB signaling pathway, and improving the intestinal barrier, thereby reducing DSS-induced colitis in mice. | [99] |
| 18 | Astragalin | Trihydroxyflavone | Salix atrocinerea | 100 mg | DSS-induced acute colitis in C57BL/6J mice | Attenuation of DSS-induced acute UC by attenuating intestinal microbiota dysbiosis and inhibiting NF-κB activation in mice. | [100] |
| 19 | Kaempferol | Tetrahydroxyflavone | Lotus ucrainicus | 50 mg | DSS-induced acute colitis in C57BL/6J mice | Reduction of experimental colitis in mice by restoring the intestinal microbiota and inhibiting the LPS-TLR4-NF-kB axis. | [101] |
| 20 | Acacetin | Dihydroxyflavanone | Verbascum lychnitis | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Improvement of experimental colitis in mice by inhibiting the inflammatory response of macrophages and modulating the composition of the intestinal microbiota. | [102] |
| 21 | Genistein | Isoflavone | Felmingia vestita | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Polarization of M1 to M2 macrophages and a reduction in systemic cytokines partially reduce the symptoms of colitis. | [103] |
| 22 | Oroxylin A | Dihydroxyflavanone | Scutellaria likiangensis | 50 mg | DSS-induced acute colitis in C57BL/6J mice | Maintains the colonic mucus barrier and regulates the intestinal microbiota. | [104] |
| 23 | Isobavachalcone | Trans-chalcone | Broussonetia papyrifera | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Amelioration of colitis in mice by inhibition of the NF-κB p65 pathway. | [105] |
| 24 | Naringenin | Flavanone | Elaeodendron croceum | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Protective effects on experimental colitis through inhibition of toll-like receptor 4/NF-κB signaling. | [106] |
| 25 | Nobiletin | Methoxyflavone | Citrus tankan | 50 mg | Ethanol-induced colitis in BALB/c mice | Reduced inflammatory signs and markers of colitis and deposition and expression of fibrotic collagen in mice. | [107] |
| 26 | Luteolin | Tetrahydroxyflavone | Verbascum lychnitis | / | DSS-induced acute colitis in C57BL/6 mice | Inhibits the elevation of 5-hydroxytryptamine. | [108] |
| 50 mg | DSS-induced acute colitis in C57BL/6 mice | Amelioration of colitis in mice by activating the Nrf2 signaling pathway. | [109] | ||||
| 27 | Taxifolin | Dihydroflavonol | Salix atrocinerea | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Alleviation of UC by acting on the gut microbiota to produce butyric acid. | [110] |
| 28 | Icariin | Glycosyloxyflavone | Epimedium pubescens | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Suppression of intestinal inflammation in UC mice through modulation of intestinal flora abundance and regulation of p-p65/p65 molecules. | [111] |
| 29 | Baicalein | Trihydroxyflavone | Scutellaria baicalensis | 40 mg | DSS-induced acute colitis in C57BL/6 mice | Improvement of the intestinal epithelial barrier through the AhR/IL-22 pathway in innate lymphoid cells. | [112] |
| 30 | Naringin | Dihydroxyflavanone | Citrus latipes | 100 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NF-κB and MAPK activation and regulation of the PPARγ pathway. | [113] |
| 31 | Puerarin | Dydroxyisoflavone | Neustanthus phaseoloides | 50 mg | DSS-induced acute colitis in BALB/c mice | Regulation of Nrf2 and antioxidant enzyme expression. | [114] |
| 32 | Cardamonin | Chalcone | Amomum subulatum | 60 mg | DSS-induced acute colitis in C57BL/6 mice; TNBS-induced colitis in BALB/c mice | Inhibition of NLRP3 inflammatory vesicle activation via the AhR/Nrf2/NQO1 pathway. | [115] |
| 33 | Curcumin | Diketone | Curcuma longa | 20 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NLRP3 inflammasome activation and IL-1β production. | [116] |
| 100 mg | DSS-induced ulcerative colitis complicating diabetes in C57BLKS/J mice | Restores Th17/Treg homeostasis and improves the composition of the intestinal flora. | [117] | ||||
| 34 | Quercetin | Pentahydroxyflavone | Quercus | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of colitis by induction of anti-inflammatory effects of macrophages and alteration of intestinal flora. | [118] |
| 35 | Daidzein | Hydroxyisoflavone | Pericopsis elata | 10 mg | DSS-induced acute colitis in BALB/c mice | Regulation of NF-κB signaling pathway. | [119] |
| 36 | Cyanidin | Flavonoid | Salix atrocinerea | 64.5 mg | TNBS-induced colitis model in BALB/c mice | Protects the intestinal barrier as well as inhibits the secretion of inflammatory cytokines. | [120] |
| 37 | Cyanidin-3-O-Glucoside | Flavonoid | Ipomoea batatas | 96.8 mg | TNBS-induced colitis model in BALB/c mice | Protects the intestinal barrier as well as inhibits the secretion of inflammatory cytokines. | [120] |
| 38 | Eriocitrin | Trihydroxyflavanone | Citrus latipes | 30 mg | DSS-induced acute colitis in C57BL/6J mice | Reduced MPO content, MMP-9, and NFκB activation. Inhibited the production of pro-inflammatory cytokines and the expression of iNOS and COX-2. | [121] |
| 39 | Hesperidin methylchalcone | Flavonoid | Myrtus communis | 30 mg | Acetic acid-induced colitis in Swiss and LysM-eGFP mice | Increases antioxidant response and reduces inflammation. | [122] |
| 40 | Baicalin | Dihydroxyflavanone | Scutellaria amoena | 100 mg | DSS-induced acute colitis in C57BL/6J mice | Decreased the expression of CD14 and inhibited NF-κB activity. | [123] |
| 41 | kurarinone | Flavonoid | Sophora flavescens | 200 mg | DSS-induced acute colitis in C57BL/6J mice | Improvement of UC through regulation of Th17/Treg cell homeostasis. | [124] |
| 42 | A-type proanthocyanidin | Flavonoid | Geranium niveum | / | DSS-induced acute colitis in BALB/c mice | Regulation of intestinal microbiota and colonic metabolism. | [125] |
| 43 | Linarin | Glucoside | Chrysanthemum indicum | 50 mg | DSS-induced acute colitis in C57BL/6J mice | Improves intestinal barrier, inhibits inflammatory response, and regulates intestinal microbiota. | [126] |
| 44 | Vitexin | Trihydroxyflavone | Itea omeiensis | / | DSS-induced acute colitis in mice | Reduced inflammation, intestinal barrier dysfunction, and intestinal flora dysbiosis in mice with colitis. | [127] |
| 45 | Licoflavone B | Isoprene flavonoid | Glycyrrhiza glabra | 120 mg | DSS-induced colitis in C57BL/6 mice | Rebuilding the intestinal barrier and regulating intestinal flora. | [128] |
| 46 | Trifolirhizin | Isoflavone | Sophora flavescens | 50 mg | DSS-induced colitis in C57BL/6 mice | Regulation of Th17/Treg cell homeostasis and inflammation in UC mice through inhibition of TXNIP-mediated NLRP3 inflammatory vesicle activation. | [129] |
| 47 | Calycosin | O-methylated isoflavone | Astragalus membranaceus | 50 mg | DSS-induced acute colitis in BALB/c mice | Significantly inhibited NF-κB pathway and JNK phosphorylation. | [130] |
| 48 | Apigenin | Trihydroxyflavone | Cordia dichotoma | / | DSS-induced chronic colitis in C57BL/6 mice | Anti-inflammatory effects through inhibition of classical and non-classical inflammatory vesicle signaling pathways. | [131] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) or Concentrations | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 49 | Dihydrotanshinone I | Diterpenoid | Salvia miltiorrhiza | 25 mg | DSS-induced acute colitis in C57BL/6J mice | Attenuation of DSS-induced UC in mice by inhibition of pro-inflammatory mediators and modulation of the RIPs-MLKL-caspase-8 axis. | [136] |
| 50 | Plumericin | Terpene lactone | Himatanthus drasticus | 3 mg | DNBS-induced colitis in CD1 mice | Reduces inflammation and oxidative stress. | [135] |
| 51 | β-caryophyllene | Bicyclic sesquiterpene | Syzygium aromaticum | 50 mg | DSS- and oxazolone-induced acute colitis in CD1 mice | Anti-inflammatory effects via CB2 and PPARγ pathways. | [137] |
| 52 | α-Amyrin | Pentacyclic triterpenoid | Ficus pertusa | 10 mg | DSS-induced acute colitis in CD1 mice | Reduces leukocyte influx into the colon; inhibits the production of pro-inflammatory cytokines; decreases mRNA expression of colonic adhesion molecules. | [138] |
| 53 | β-Amyrin | ||||||
| 54 | (+)-Borneol | Bicyclic monoterpene | Blumea balsamifera | 3 mg | DSS-induced acute colitis in C57BL/6 mice | Promoting M2 macrophage polarization through the JAK2-STAT3 signaling pathway. | [139] |
| 55 | β-Carotene | Tetraterpene carotenoid | Dunaliella salina | 20 mg | DSS-induced acute colitis in Swiss Albino mice | Reduces inflammation, oxidative stress, fibrosis and DNA damage in the colon. | [140] |
| 56 | Carvacrol | Phenolic monoterpene | Origanum vulgare | 100 mg | Acetic acid-induced colitis in C57BL/6 mice | Reduces inflammation, injurious nociceptive, and oxidative damage. | [134] |
| 57 | Geraniol | Monoterpenoid | Cinnamomum tenuipilum | 120 mg | DSS-induced acute colitis in C57BL/6 mice | Reduction of ecological disorders and systemic inflammation. | [141] |
| 250 mg | TNBS-induced colitis in Wistar rats | Reduction of colitis through Wnt/β-catenin, p38MAPK, NFκB, and PPARγ signaling pathways. | [142] | ||||
| 58 | Ganoderic acid C1 | Triterpenoid | Ganoderma lucidum | 40 μg/mL | Lamina Propria Mononuclear Cells | Downregulation of NF-κB signaling. | [143] |
| 59 | D-Limonene | Cyclic monoterpene | Vitis rotundifolia | 10 mg | TNBS-induced colitis in Wistar HsdBrlHan rats | Inhibits the inflammatory response. | [144] |
| 100 mg | TNBS-induced colitis in Sprague–Dawley rats | Exhibits anti-inflammatory and antioxidant properties through modulation of iNOS, COX-2, PGE2, and ERK signaling pathways. | [145] | ||||
| 60 | Menthol | Cyclic monoterpene | Chaerophyllum macrospermum | 80 mg | Acetic acid-induced colitis in Wistar rats | Significantly reduces inflammation. | [146] |
| 61 | Nerol | Monoterpenoid alcohol | Citrus aurantium | 300 mg | Oxazolone-induced colitis in BALB/c mice | Improves the pathological features of colitis, protects the stomach from damage, and has immunomodulatory effects. | [147] |
| 62 | Oleanolic Acid | Pentacyclic triterpenoid | Ophiopogon japonicus | 10 mg | DSS-induced acute colitis in C57BL/6 mice | Restoration of Th17/Treg cell homeostasis and inhibition of NF-κB signaling pathway. | [148] |
| 62 | Perillaldehyde | Monoterpene | Perilla frutescens | 100 mg | DSS-induced acute colitis in C57BL/6 mice | Improvement of intestinal inflammation through JNK-mediated cytokine regulation. | [149] |
| 64 | Thymol | Monoterpene | Xylopia aromatica | 100 mg | Acetic acid-induced colitis in Wistar rats | Inhibition of NF-kB signaling pathway to reduce inflammatory response. | [150] |
| 65 | Alantolactone | Sesquiterpene lactone | Eupatorium cannabinum | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NF-κB inflammatory signaling mediated by PXR. | [151] |
| 66 | Betulin | Pentacyclic triterpenoid | Diospyros morrisiana | 8 mg | Acetic acid-induced colitis in Sprague–Dawley rats | Inhibition of colonic apoptosis by reducing colonic caspase-3 and caspase-8 expression; potential mechanisms include downregulation of TLR4/NF-κB and subsequent downstream signaling pathways. | [152] |
| 67 | Zeaxanthin | Carotenoid | Bangia fuscopurpurea | 50 mg | Acetic acid-induced colitis in Sprague Dawley rats | Regulation of pro-inflammatory cytokines and oxidative stress. | [153] |
| 68 | D-Carvone | Terpenoid | Carum carvi | 40 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of COX-2 and TNF-α. | [154] |
| 69 | Celastrol | Triterpenoid | Tripterygium wilfordii | 1 mg | DSS-induced acute colitis in BALB/c mice | Improves Treg/Th1 and Treg/Th17 balance to maintain colonic immune homeostasis; regulates intestinal microbiota. | [155] |
| 70 | Asiatic acid | Triterpenoid | Centella asiatica | 30 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibits mitochondria-mediated activation of NLRP3 inflammatory vesicles. | [133] |
| 71 | Madecassic acid | Triterpenoid | Centella asiatica | 25 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of γδT17 cell activation via PPARγ-PTEN/Akt/GSK3β/NFAT pathway. | [156] |
| 72 | Nerolidol | Sesquiterpene alcohol | Brassavola nodosa | 150 mg | DSS-induced acute colitis in C57BL/6J mice | Reduce colonic inflammation by exerting its antioxidant and anti-inflammatory activities. | [157] |
| 73 | β-Myrcene | Monoterpene | Teucrium montanum | 100 mg | DSS-induced acute colitis in C57BL/6J mice | Inhibition of MAPK and NF-κB pathways. | [158] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 74 | Dioscin | Steroidal saponin | Ophiopogon intermedius | 160 mg | DSS-induced acute colitis in BALB/c mice | Regulates the polarization of macrophages. | [172] |
| 75 | Pelargonidin 3-glucoside | Anthocyanidin glycoside | Lonicera caerulea | 8 mg | DSS-induced chronic IBD in rats | Reduces inflammation and reduces IBD symptoms. | [173] |
| 76 | 2,3,5,4′-Tetrahydroxystilbene-2-O-β-D-glucoside | Glucoside | Polygonum multiflorum | 100 mg | DSS-induced acute colitis in BALB/c mice | Reduces inflammation and regulates the intestinal microbiota. | [174] |
| 77 | Ginsenoside Rb1 | Ginsenoside | Panax vietnamensis | 40 mg | DSS-induced acute colitis in C57BL/6 mice | Attenuation of mouse colitis by activation of the endoplasmic reticulum resident E3 ubiquitin ligase Hrd1 signaling pathway. | [16] |
| 78 | Ginsenoside Rd | Ginsenoside | Panax vietnamensis | 20 mg | Sprague–Dawley rats injected with indomethacin | Stimulates the proliferation and differentiation of endogenous intestinal stem cells and restores intestinal function. | [168] |
| 79 | Ginsenoside Rg1 | Ginsenoside | Panax vietnamensis | 200 mg | DSS-induced acute colitis in C57BL/6 mice | Alleviation of acute UC by modulating gut microbiota and microbial tryptophan metabolism. | [169] |
| 80 | Ginsenoside Rh2 | Ginsenoside | Panax vietnamensis | 50 mg | DSS-induced acute colitis in C57BL/6J mice | Mitigation of UC by regulating STAT3/miR-214 signaling pathway. | [170] |
| 81 | Ginsenoside Rk3 | Ginsenoside | Panax vietnamensis | 40 mg | DSS-induced acute colitis in C57BL/6 mice | Protection of the colonic barrier and inhibition of NLRP3 inflammatory vesicles. | [171] |
| 82 | Paeoniflorin | Terpene glycoside | Paeonia | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NF-κB and MAPK pathway activation by reducing TLR4 expression. | [175] |
| 20 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of inflammatory response and eosinophil infiltration. | [161] | ||||
| 83 | Salidroside | Glycoside | Salix atrocinerea | 40 mg | DSS-induced acute colitis in C57BL/6 mice | Protection of mice with colitis by activation of the SIRT1/FoxOs pathway, which is associated with oxidative stress and apoptosis in colonic tissues. | [162] |
| 84 | Anemoside B4 | Saponin | Pulsatilla chinensis | 100 mg | DSS-induced acute colitis in C57BL/6 mice | Regulation of inflammatory response, colonic transcriptome, and intestinal microbiota. | [176] |
| 85 | Wogonoside | Flavonoid glycoside | Scutellaria baicalensis | 50 mg | DSS-induced acute colitis in C57BL/6 mice | Improving intestinal epithelial barrier function through the MLCK/pMLC2 pathway alleviates colitis. | [163] |
| 86 | Hesperidin | Flavanone glycoside | Citrus aurantium | 40 mg | DSS-induced acute colitis in C57BL/6 mice | Prevents intestinal inflammation by restoring intestinal barrier function and upregulating Treg cells. | [164] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 87 | Epigallocatechin-3-gallate | Catechin | Limoniastrum guyonianum | 50 mg | DSS-induced acute colitis in C57BL/6J mice | Improves intestinal epithelial homeostasis and regulates intestinal microbiota. | [188] |
| 88 | Gallic acid | Trihydroxybenzoic acid | Visnea mocanera | 10 mg | DSS-induced acute colitis in BALB/c mice | Downregulation of IL-21 and IL-23 expression levels. Activation of enzymatic antioxidants via the Nrf2 pathway to provide cryoprotection. | [189] |
| 89 | Procyanidin B2 | Polyphenol | Begonia fagifolia | 30 mg | DSS-induced acute colitis in C57/BL6 mice | Inhibition of oxidative stress through the Nrf2/ARE signaling pathway, which in turn promotes intestinal damage repair. | [190] |
| 90 | Procyanidin A1 | Polyphenol | Tainia latifolia | 10 mg | DSS-induced acute colitis in BALB/c mice | Regulation of AMPK/mTOR/p70S6K-mediated autophagy. | [191] |
| 91 | Polydatin | Polyphenol | Vitis rupestris | 45 mg | DSS-induced acute colitis in C57/BL6 mice | Partial reduction of oxidative stress and apoptosis through sonic hedgehog signaling pathway. | [192] |
| 92 | Chlorogenic acid | Cinnamate ester | Calluna vulgaris | 120 mg | DSS-induced acute colitis in C57BL/6 mice | Reduces tissue inflammation and apoptosis by a mechanism related to the MAPK/ERK/JNK signaling pathway. | [193] |
| 40 mg | DSS-induced acute colitis in BALB/c mice | Downregulation of miR-155 expression and inactivation of NF-κB/NLRP3 inflammasome pathway in macrophages. | [194] | ||||
| 93 | Tyrosol | Phenylethanoid | olive oil | 20 mg | DSS-induced acute colitis in Wistar albino rats | Exerts anti-inflammatory and antioxidant activity. | [195] |
| 94 | 2,3,5,4′-tetrahydroxystilbene-2-O-beta-D-glucoside | Polyphenol | Fallopia multiflora | 60 mg | Acetic acid-induced colitis in Kunming mice | Involved in the upregulation of PPAR-γ and inhibition of NF-κB inflammatory pathway. | [196] |
| 95 | Resveratrol | Polyphenol | Red grapes | 100 mg | TNBS-induced colitis in BALB/c mice | Simultaneous inhibition of inflammatory Th1/Th17 cells through induction of Tregs; regulation of microbiota. | [185] |
| DSS-induced chronic colitis in C57BL/6 mice | Reduction of intestinal mucosal barrier dysfunction in UC mice by enhancing autophagy of intestinal epithelial cells. | [184] | |||||
| DSS-induced acute colitis in BALB/c mice | Inhibition of PI3K/Akt pathway activation and reduction of VEGFA gene expression. | [183] | |||||
| 96 | Salvianolic acid A | Phenolic acids | Salvia miltiorrhiza | 8 mg | DSS-induced acute colitis in Sprague–Dawley | Reduces intestinal inflammation; regulates the imbalance of intestinal microbiota. | [197] |
| 97 | Salvianolic acid B | Phenolic acids | Salvia miltiorrhiza | 100 mg | DSS-induced acute colitis in C57BL/6 mice | Reduces inflammation; increases the production of short-chain fatty acids; affects the composition of the intestinal microbiota in mice. | [198] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 98 | Juglone | Naphthoquinone | Juglans nigra | 1 mg | DSS-induced ulcerative colitis in ICR mice | Regulation of intestinal microbiota and restoration of Th17/Treg homeostasis. | [18] |
| 99 | Emodin | Trihydroxyanthraquinone | Rheum palmatum | 20 mg | DSS-induced acute colitis in C57BL/6J mice | Increased PPAR-γ expression and inhibited NF-κB activity. | [123] |
| 100 | Shikonin | Naphthoquinone | Echium plantagineum | 25 mg | DSS-induced acute colitis in C57BL/6 mice | Alleviation of inflammation and mucosal barrier damage in UC. | [200] |
| 101 | Thymoquinone | Benzoquinone | Nigella sativa | 40 mg | DSS-induced acute colitis in C57BL/6J mice | Reducing inflammation through the Nrf2/Keap1 system. | [201] |
| 102 | Naphthoquinone-2 | Naphthoquinone derivative | Juglans nigra | 100 mg | DSS-induced acute colitis in Wistar rats | Suppression of colonic length, colonic mass index, and intestinal histopathology score. | [202] |
| 103 | Plumbagin | Naphthoquinone | Drosera slackii | 10 mg | DSS-induced acute colitis in C57BL/6J mice | Significantly reduced levels of circulating inflammatory monocytes (CD14+/CD16+) and cytokines (TNF-α and +-IFN-γ). | [203] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) or Concentrations | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 104 | Capsaicin | Vanilloid | Capsicum | 12 mg | DSS-induced acute colitis in Sprague–Dawley rats | Inhibits oxidative stress, inflammatory response, and pain signaling. | [211] |
| 105 | Matrine | Quinolizidine alkaloid | Sophora flavescens | 12 mg/mL | TNBS-ethanol-induced ulcerative colitis in Wistar rats | Reduces inflammatory response and oxidative stress damage. | [212] |
| 20 mg | DSS-induced acute colitis in BALB/c mice | Improves the integrity of the intestinal barrier, inhibits the PPAR-α signaling pathway, and regulates intestinal flora. | [213] | ||||
| 106 | Evodiamine | Alkaloid | Evodia rutaecarpa | 30 mg | DSS-induced chronic colitis in C57BL/6 mice | Reduces the inflammatory response by preventing damage to the intestinal mucosal barrier and regulating the secretion of inflammatory cytokines. | [214] |
| 107 | Nuciferine | Alkaloid | Nymphaea caerulea | 20 mg | DSS-induced acute colitis in BALB/c mice | Regulation of gut microbiota homeostasis and immune function in UC mice. | [215] |
| 108 | Piperine | Piperidine alkaloid | Piper boehmeriifolium | 40 mg | TNBS-induced colitis in Sprague–Dawley rats | Inhibits IκB-α/NF-κB and induces the tight junction proteins claudin-1, occludin, and ZO-1. | [209] |
| 10 mg | Acetic acid-induced ulcerative colitis in Swiss albino mice | Downregulated the production and expression of inflammatory mediators and reduced the FFA-induced TLR4-mediated inflammatory response. | [208] | ||||
| 109 | Nicotine | Alkaloid | Tobacco | 10 μg | DSS-induced acute colitis in C57BL/6 mice | Regulates autophagy via AMPK/mTOR pathway; improves inflammation levels. | [40] |
| 110 | Neferine | Isoquinoline alkaloid | Nelumbo nucifera | 10 mg | DSS-induced acute colitis in C57BL/6J mice | Inhibition of inflammatory response. | [216] |
| 25 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibited iNOS, COX-2, receptor-interacting protein 1 (RIP1), RIP3, and increased caspase-8 protein expression in colonic tissues. | [217] | ||||
| 111 | Anatabine | Bipyridines | Nicotiana cavicola | 20 mg | DSS-induced colitis in C57BL/6 mice | Improves intestinal inflammation and reduces the production of pro-inflammatory factors. | [218] |
| 112 | Phellodendrine | Alkaloid | Phellodendron chinense | 30 mg | DSS-induced acute colitis in C57BL/6 mice | Reduces inflammatory response and promotes autophagy by regulating AMPK-mTOR signaling pathway. | [219] |
| 113 | Epiisopiloturine | Imidazole alkaloid | jaborandi | 1 mg | TNBS-induced colitis in Wistar rats | Downregulation of inflammatory processes by inhibiting the synthesis and release of inflammatory products, lipid peroxidation, and expression of inflammatory enzymes. | [220] |
| 114 | Camptothecin | Quinoline alkaloid | Camptotheca acuminata | 1.5 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of inflammatory responses through AKT, NF-κB and MAPK signaling pathways. | [210] |
| 115 | Strictosamide | Beta-carboline | Amsonia orientalis | 40 mg | DSS-induced acute colitis in BALB/c mice | Improving the inflammatory response and NF-κB signaling pathway. | [221] |
| 116 | Berberine | Isoquinoline alkaloid | Berberis vulgaris | 40 mg | DSS-induced acute colitis in BALB/c mice | Regulates the intestinal microbiota and protects the mucosal barrier. | [206] |
| 100 mg | DSS-induced acute colitis in C57BL/6 mice and Sprague–Dawley rats | Regulation of intestinal glial cell-intestinal epithelial cell-immune cell interactions. | [207] | ||||
| 117 | Oxymatrine | Quinolizidine alkaloid | Sophora pachycarpa | 20 mg | DSS-induced acute colitis in Kunming mice | Reduces inflammatory response and re-establishes antioxidant/oxidant balance. | [222] |
| 50 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of PI3K/AKT signaling pathway. | [223] | ||||
| 118 | Sophocarpine | Quinolizidine alkaloid | Daphniphyllum oldhamii | 30 mg | DSS-induced acute colitis in BALB/c mice | Maintains the integrity of the colonic barrier and inhibits the development of colitis. | [224] |
| 119 | Capnoidine | Tetrahydroisoquinoline alkaloid | Fumaria capreolata | / | TNBS-induced acute colitis in C57BL/6 mice | Reduction of colonic histological inflammation. | [225] |
| 120 | Oxyberberine | Benzyl tetrahydroisoquinoline alkaloid | Thalictrum lucidum | 50 mg | DSS-induced acute colitis in BALB/c mice | Influence on the intestinal epithelial barrier, intestinal microbiota, and TLR4-MyD88-NF-κB pathway. | [226] |
| 121 | Aloperine | Quinolizidine alkaloid | Thinicola incana | 40 mg | DSS-induced acute colitis in BALB/c mice | Inhibits the PP2A-Mediated PI3K/Akt/mTOR signaling pathway. | [227] |
| 122 | Berberrubine | Benzyl tetrahydroisoquinoline alkaloid | Coptischinensis | 20 mg | DSS-induced acute colitis in BALB/c mice | Reduction of mucosal lesions and inflammation. | [228] |
| 123 | Sinomenine | Morphinane alkaloid | Sinomenium acutum | 100 mg | DSS-induced acute colitis in C57BL/6 mice | Alleviation of colitis through the Nrf2/NQO 1 signaling pathway. | [229] |
| 124 | N-Methylcytisine | Quinolizidine alkaloid | Thermopsis lanceolata | 16 mg | DSS-induced acute colitis in ICR mice | Inhibition of NF-κB activation. | [230] |
| 125 | Tetrandrine | Bisbenzylisoquinoline alkaloid | Pachygone dasycarpa | / | DSS-induced acute colitis in mice | Promoting occludin expression through the AhR-miR-429 pathway. | [231] |
| 40 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NF-κB activation. | [232] | ||||
| 126 | Norisoboldine | Benzyl tetrahydroisoquinoline alkaloid | Cassytha pubescens | 40 mg | TNBS-induced colitis in BALB/c mice | Regulation of the AhR/Nrf2/ROS signaling pathway inhibits NLRP3 inflammasome activation. | [233] |
| 127 | Dihydroberberine | Isoquinoline alkaloid | Thalictrum foliolosum | 50 mg | DSS-induced acute colitis in BALB/c mice | Improved intestinal barrier function; reduced colonic pro-inflammatory cytokines and immunoglobulins by blocking TLR4/MyD88/NF-κB signaling pathway; improved colonic immune inflammation status. | [234] |
| 128 | Palmatine | Isoquinoline alkaloid | Berberis poiretii | 50 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of tryptophan metabolism and regulation of intestinal flora. | [235] |
| 100 mg | DSS-induced acute colitis in BALB/c mice | Promoting PINK1/Parkin-driven mitochondrial autophagy and thereby inactivating NLRP3 inflammasome in macrophages. | [236] | ||||
| 129 | Coptisine | Tetrahydroisoquinoline alkaloid | Fumaria capreolata | 100 mg | DSS-induced acute colitis in BALB/c mice | Improvement of intestinal barrier dysfunction and inhibition of inflammatory response. | [237] |
| 130 | Sanguinarine | Benzophenanthridine alkaloid | Sanguinaria canadensis | 10 mg | Acetic acid-induced ulcerative colitis in Kunming mice | Effective inhibition of p65 NF-κB protein expression and MPO activity accumulation. | [238] |
| 131 | 5-Hydroxy-4-methoxycanthin-6-one | Indole alkaloid | Picrasma quassioides | 100 mg | DSS-induced acute colitis in Sprague–Dawley rats | Regulation of metabolic profile and inhibition of NF-κB/p65 signaling pathway. | [239]` |
| 132 | Isatin | Indole alkaloid | Couroupita guianensis | 25 mg | TNBS-induced colitis in Wistar Hannover rats | Protects the intestinal mucosa from TNBS-induced damage through a combination of antioxidant and anti-inflammatory properties. | [240] |
| 133 | Caulerpin | Indole alkaloid | Caulerpa obscura | 4 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibition of NF-κB pathway activation. | [241] |
| 134 | Indirubin | Indole alkaloid | Isatis tinctoria | 10 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of DSS-induced activation of NF-κB and MAPK pathways. | [242] |
| 10 mg | DSS-induced acute colitis in BALB/c mice | Inhibition of inflammation and induction of regulatory T cell expression foxp3. | [243] | ||||
| 135 | Rutaecarpine | Indole alkaloid | Tetradium ruticarpum | 80 mg | DSS-induced acute colitis in C57BL/6J mice | Inhibition of KEAP1-NRF2 interaction and activation of NRF2. | [244] |
| 136 | Daurisoline | Isoquinoline alkaloid | Menispermum dauricum | 40 mg | DSS-induced acute colitis in BALB/c mice | Involved in NF-κB and Wnt/β-Catenin pathways. | [245] |
| 137 | 14-O-acetylneoline | Diterpenoid alkaloid | Aconitum laciniatum | / | TNBS-induced colitis in C57BL/6 mice | Reduced IFN-γ mRNA levels in colonic tissues. | [246] |
| No. | Name | Type | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 138 | 4-methylesculetin | Hydroxycoumarin | / | 25 mg | DSS-induced acute colitis in Swiss albino mice | Exerts anti-inflammatory properties. | [251] |
| 5 mg | TNBS-induced colitis in Wistar rats | Reduction of colonic oxidative stress and inhibition of pro-inflammatory cytokine production. | [252] | ||||
| 139 | Daphnetin | Hydroxycoumarin | Euphorbia dracunculoides | 16 mg | DSS-induced acute colitis in BALB/c mice | Regulation of microbiota composition and T reg/T h 17 balance. | [253] |
| 140 | Bergapten | Furocoumarin | Ficus virens | 30 mg | Acetic acid-induced colitis in Sprague–Dawley rats | Reduction of acetic acid-induced inflammation, colonic damage and mast cell degranulation in rats. | [254] |
| 141 | Imperatorin | Furocoumarin | Angelica dahurica | 60 mg | TNBS-induced colitis in Sprague–Dawley rats | Regulation of Nrf-2/ARE/HO-1 pathway in rats. | [255] |
| 142 | Osthole | Derivative of coumarin | Cnidium monnieri | 100 mg | TNBS-induced colitis in C57BL/6 mice | Reducing the expression of inflammatory mediators and decreasing the phosphorylation level of p38. | [248] |
| 40 mg | DSS-induced acute colitis in BALB/c mice | Blocking the activation of NF-κB and MAPK/p38 pathways. | [249] | ||||
| 143 | Esculetin | Hydroxycoumarin | Artemisia eriopoda | 5 mg | TNBS-induced colitis in Wistar rats | Inhibition of pro-inflammatory cytokine secretion and increased defense against reactive oxygen species. | [256] |
| 144 | Umbelliferone | Hydroxycoumarin | Ficus septica | 30 mg | Acetic acid-induced colitis in Wistar rats | Regulation of TLR4/NF-κB-p65/iNOS and SIRT1/PPARγ signaling pathways in rats. | [250] |
| 145 | Imperatorin | Furocoumarin | Angelica archangelica | 100 mg | DSS-induced acute colitis in C57BL/6 mice | By inhibiting NF-κB-mediated pro-inflammatory responses in a PXR/NF-κB-dependent manner. | [257] |
| 146 | Coumarin | Chromenone | Coumarou | 5 mg | TNBS-induced colitis in Wistar rats | Prevents glutathione depletion due to colonic inflammation. | [258] |
| 147 | 4-Hydroxycoumarin | Hydroxycoumarin | Coumarou | 25 mg | TNBS-induced colitis in Wistar rats | Prevents glutathione depletion due to colonic inflammation. | [258] |
| No. | Name | Origin | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|
| 148 | Chitosan oligosaccharide | Dietary fiber chitosan | 10 mg | DSS-induced acute colitis in ICR mice | Inhibition of NF- B signaling pathway and apoptosis in intestinal epithelial cells. | [270] |
| 149 | Mannose | / | 500 mg | DSS-induced acute colitis in C57BL/6 mice | Enhanced lysosomal integrity and limited release of histone B; reduced intestinal barrier damage. | [271] |
| 150 | Lycium barbarum polysaccharides | Lycium barbarum | 100 mg | DSS-induced acute colitis in Sprague–Dawley rats | Inhibition of oxidative stress, inflammatory response, and pain signaling. | [211] |
| 151 | Astragalus polysaccharides | Astragalus membranaceus | 300 mg | DSS-induced acute colitis in C57BL/6 mice | Inhibits the NRF2/HO-1 pathway. | [263] |
| 200 mg | DSS-induced acute colitis in C57BL/6 mice | Regulation of Tfh/Treg cell homeostasis. | [264] | |||
| 152 | Chrysanthemum polysaccharides | Chrysanthemum morifolium | 100 mg | TNBS-induced acute colitis in Sprague–Dawley rats | Promotes the growth of beneficial intestinal flora, regulates the intestinal micro-ecological balance, and restores the immune system. | [272] |
| 50 mg | TNBS-induced acute colitis in Sprague–Dawley rats | Regulation of metabolic profiles and NF-κ B/TLR4 and IL-6/JAK2/STAT3 signaling pathways. | [273] | |||
| 153 | Garlic polysaccharides | Allium sativum L. | 400 mg | DSS-induced acute colitis in C57BL/6 mice | Improves the mucosal barrier, blocks pro-inflammatory cytokines, and regulates the intestinal microbiota. | [274] |
| 154 | Polysaccharides from Atractylodes macrocephala Koidz. | Atractylodes macrocephala Koidz. | 40 mg | DSS-induced acute colitis in C57BL/6J mice | Modification of intestinal flora and host metabolism to improve UC. | [275] |
| 155 | Mannoglucan | Chinese yam | 300 mg | DSS-induced acute colitis in C57BL/6J mice | Inhibits excessive production of pro-inflammatory cytokines, suppresses activation of colonic inflammatory signaling pathways, enhances mRNA expression of ligand proteins, and regulates intestinal microbiota. | [276] |
| 156 | Dendrobium fimbriatum polysaccharides | Dendrobium fimbriatum | / | DSS-induced acute colitis in C57BL/6J mice | Improves intestinal barrier function, regulates intestinal flora, and reduces oxidative stress and inflammatory response. | [277] |
| 157 | Ficus carica polysaccharides | Ficus carica | 300 mg | DSS-induced chronic colitis in C57BL/6 mice | Improvement of colon length and inhibition of inflammatory cell infiltration in the intestine. | [278] |
| 158 | Crude Fuzhuan brick tea polysaccharides | Fuzhuan brick tea | / | DSS-induced colitis in C57BL/6 mice | Regulates intestinal flora, reduces inflammatory response, and improves intestinal barrier function. | [279] |
| 159 | Lonicera japonica Thunb polysaccharides | Lonicera japonica Thunb | 150 mg | DSS-induced acute colitis in BALB/c mice | Restoration of immune disorders and improvement of anti-inflammatory activity of immune organs in UC mice. | [280] |
| 160 | Noni fruit polysaccharides | Morinda citrifolia L. | 10 mg | DSS-induced acute colitis in BALB/c mice | Targeting intestinal microbiota regulation; inhibition of JNK, ERK, and NF-κB phosphorylation in IBD mice. | [281] |
| 161 | Scutellaria baicalensis Georgi polysaccharides | Scutellaria baicalensis Georgi | 200 mg | DSS-induced acute colitis in C57BL/6 mice | Improvement of intestinal barrier function and regulation of intestinal microbiota. | [282] |
| 162 | Auricularia auricular-judae polysaccharides | Auricularia auricular-judae | 40 mg | DSS-induced acute colitis in BALB/c mice | Regulation of the composition of the intestinal microbiota. | [262] |
| 163 | Ganoderma lucidum polysaccharides | Ganoderma lucidum | / | DSS-induced acute colitis in Wistar rats | Alteration of cecum microbiota and colonic epithelial cell gene expression. | [283] |
| 100 mg | DSS-induced acute colitis in C57BL/6 mice | Reduces inflammation, maintains intestinal homeostasis, and regulates intestinal immune barrier function. | [284] | |||
| 164 | Tremella fuciformis polysaccharides | Tremella fuciformis | 300 mg | DSS-induced acute colitis in C57BL/6 mice | Regulation of intestinal microbiota and bacterial metabolites. | [267] |
| 165 | Dictyophora indusiata polysaccharides | Dictyophora indusiata | 33 mg | DSS-induced acute colitis in BALB/c mice | By improving intestinal damage, oxidative stress and production of pro-inflammatory cytokines; regulating intestinal flora. | [265] |
| 100 mg | DSS-induced acute colitis in C57BL/6 mice | Reduced oxidative stress and inflammatory response, inhibited key signaling pathways associated with colitis, improved expression of tight junction proteins, and downregulated polarization of M1 macrophages. | [285] |
| No. | Name | Origin | Amino Acid Sequence | Optimal Doses (/kg Body Weight) | Model | Potential Mechanism | References |
|---|---|---|---|---|---|---|---|
| 166 | Soy tripeptide | soy | VPY | 100 mg | DSS-induced acute colitis in BALB/c mice | Downregulation of pro-inflammatory cytokine expression in the colon and amelioration of inflammation in colonic tissue. | [287] |
| 167 | Pyroglutamyl leucine | wheat gluten hydrolysate | pyroGlu-Leu | 0.1 mg | DSS-induced acute colitis in C57BL/6 mice | Regulation of intestinal microorganisms. | [288] |
| 168 | Phycocyanin | Aphanizomenon flos-aquae | / | / | DSS-induced acute colitis in C57BL/6 mice | Protects the intestinal epithelial barrier; anti-inflammatory and antioxidant. | [289] |
| 169 | Melittin peptide | Apis mellifera | GIGAVLKVLTTGLPALISWIKRKRQQ | 2.4 mg | DSS-induced acute colitis in C57BL/6 mice | Eliminates histological damage to colonic tissue and reduces inflammation. Regulates oxidative/antioxidant balance. | [290] |
| / | 40 μg | Acetic acid-induced colitis in Swiss albino mice | Attenuates TLR4/TRAF6-mediated activation of NF-κB and p38MAPK pathways. | [295] | |||
| 170 | Yellowtail milt hydrolysates | Seriola quinqueradiata | / | / | DSS-induced acute colitis in C57BL/6 mice | Improvement of colitis symptoms and intestinal epithelial barrier dysfunction in mice. | [291] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.; Wang, D.; Yan, W. Treatment Effects of Natural Products on Inflammatory Bowel Disease In Vivo and Their Mechanisms: Based on Animal Experiments. Nutrients 2023, 15, 1031. https://doi.org/10.3390/nu15041031
Zhou Y, Wang D, Yan W. Treatment Effects of Natural Products on Inflammatory Bowel Disease In Vivo and Their Mechanisms: Based on Animal Experiments. Nutrients. 2023; 15(4):1031. https://doi.org/10.3390/nu15041031
Chicago/Turabian StyleZhou, Yaxi, Diandian Wang, and Wenjie Yan. 2023. "Treatment Effects of Natural Products on Inflammatory Bowel Disease In Vivo and Their Mechanisms: Based on Animal Experiments" Nutrients 15, no. 4: 1031. https://doi.org/10.3390/nu15041031
APA StyleZhou, Y., Wang, D., & Yan, W. (2023). Treatment Effects of Natural Products on Inflammatory Bowel Disease In Vivo and Their Mechanisms: Based on Animal Experiments. Nutrients, 15(4), 1031. https://doi.org/10.3390/nu15041031








