Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China—Results from the China Health and Nutrition Survey
Abstract
1. Introduction
2. Materials and Methods
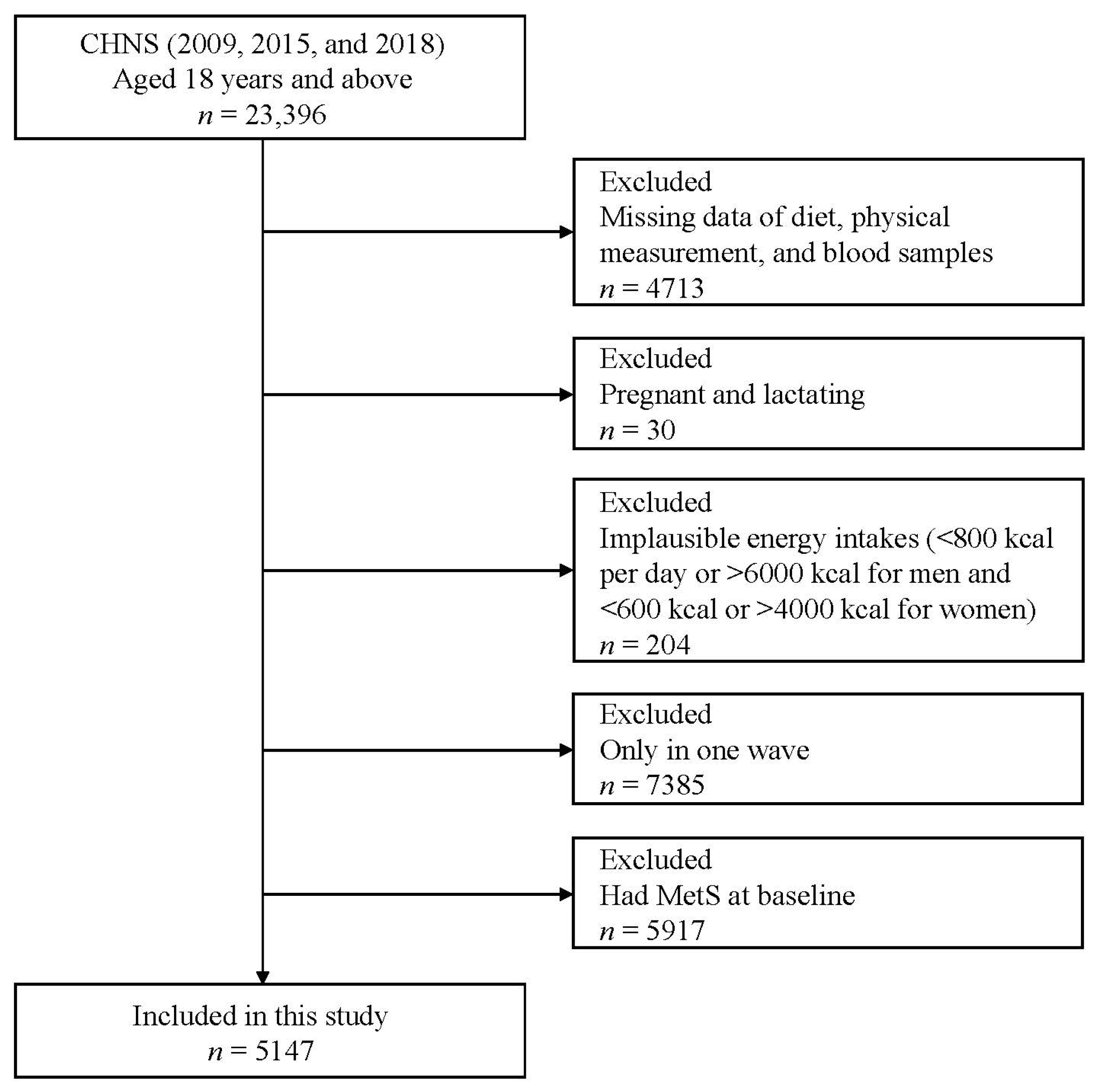
2.1. Study Design and Population
2.2. Dietary Assessment and UPF Consumption
2.3. Definition of Metabolic Syndrome
2.4. Covariates and Physical Measurement
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Associations of UPF Consumption with MetS and Its Components
3.3. Stratified Analyses of MetS Risk and UPF Consumption
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Gu, D.; Reynolds, K.; Wu, X.; Chen, J.; Duan, X.; Reynolds, R.F.; Whelton, P.K.; He, J.; Inter, A.C.G. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005, 365, 1398–1405. [Google Scholar] [CrossRef]
- He, Y.; Li, Y.; Bai, G.; Zhang, J.; Fang, Y.; Zhao, L.; Zhao, W.; Yang, X.; Ding, G. Prevalence of metabolic syndrome and individual metabolic abnormalities in China, 2002–2012. Asia Pac. J. Clin. Nutr. 2019, 28, 621–633. [Google Scholar] [CrossRef]
- Yao, F.; Bo, Y.; Zhao, L.; Li, Y.; Ju, L.; Fang, H.; Piao, W.; Yu, D.; Lao, X. Prevalence and Influencing Factors of Metabolic Syndrome among Adults in China from 2015 to 2017. Nutrients 2021, 13, 4475. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Zappala, G.; Bernardini, S.; Giambini, I.; Bes-Rastrollo, M.; Martinez-Gonzalez, M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: A meta-analysis of observational studies. Int. J. Food Sci. Nutr. 2017, 68, 138–148. [Google Scholar] [CrossRef]
- Mankowski, R.T.; Aubertin-Leheudre, M.; Beavers, D.P.; Botoseneanu, A.; Buford, T.W.; Church, T.; Glynn, N.W.; King, A.C.; Liu, C.; Manini, T.M.; et al. Sedentary time is associated with the metabolic syndrome in older adults with mobility limitations--The LIFE Study. Exp. Gerontol. 2015, 70, 32–36. [Google Scholar] [CrossRef]
- Kim, H.; Lee, K.; Rebholz, C.M.; Kim, J. Plant-based diets and incident metabolic syndrome: Results from a South Korean prospective cohort study. PLoS Med. 2020, 17, e1003371. [Google Scholar] [CrossRef] [PubMed]
- Fabiani, R.; Naldini, G.; Chiavarini, M. Dietary Patterns and Metabolic Syndrome in Adult Subjects: A Systematic Review and Meta-Analysis. Nutrients 2019, 11, 2056. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Srour, B.; Kordahi, M.C.; Bonazzi, E.; Deschasaux-Tanguy, M.; Touvier, M.; Chassaing, B. Ultra-processed foods and human health: From epidemiological evidence to mechanistic insights. Lancet Gastroenterol. Hepatol. 2022, 7, 1128–1140. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 67–77.e3. [Google Scholar] [CrossRef] [PubMed]
- Rauber, F.; Chang, K.; Vamos, E.P.; da Costa Louzada, M.L.; Monteiro, C.A.; Millett, C.; Levy, R.B. Ultra-processed food consumption and risk of obesity: A prospective cohort study of UK Biobank. Eur. J. Nutr. 2021, 60, 2169–2180. [Google Scholar] [CrossRef]
- Beslay, M.; Srour, B.; Mejean, C.; Alles, B.; Fiolet, T.; Debras, C.; Chazelas, E.; Deschasaux, M.; Wendeu-Foyet, M.G.; Hercberg, S.; et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Sante cohort. PLoS Med. 2020, 17, e1003256. [Google Scholar] [CrossRef]
- Canhada, S.L.; Luft, V.C.; Giatti, L.; Duncan, B.B.; Chor, D.; Fonseca, M.; Matos, S.M.A.; Molina, M.; Barreto, S.M.; Levy, R.B.; et al. Ultra-processed foods, incident overweight and obesity, and longitudinal changes in weight and waist circumference: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Public Health Nutr. 2020, 23, 1076–1086. [Google Scholar] [CrossRef]
- Scaranni, P.; Cardoso, L.O.; Chor, D.; Melo, E.C.P.; Matos, S.M.A.; Giatti, L.; Barreto, S.M.; da Fonseca, M.J.M. Ultra-processed foods, changes in blood pressure and incidence of hypertension: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Public Health Nutr. 2021, 24, 3352–3360. [Google Scholar] [CrossRef]
- Rezende-Alves, K.; Hermsdorff, H.H.M.; Miranda, A.; Lopes, A.C.S.; Bressan, J.; Pimenta, A.M. Food processing and risk of hypertension: Cohort of Universities of Minas Gerais, Brazil (CUME Project). Public Health Nutr. 2021, 24, 4071–4079. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, R.D.; Lopes, A.C.; Pimenta, A.M.; Gea, A.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am. J. Hypertens. 2017, 30, 358–366. [Google Scholar] [CrossRef]
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Alles, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultraprocessed Food Consumption and Risk of Type 2 Diabetes Among Participants of the NutriNet-Sante Prospective Cohort. JAMA Intern. Med. 2020, 180, 283–291. [Google Scholar] [CrossRef]
- Levy, R.B.; Rauber, F.; Chang, K.; Louzada, M.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2021, 40, 3608–3614. [Google Scholar] [CrossRef]
- Duan, M.J.; Vinke, P.C.; Navis, G.; Corpeleijn, E.; Dekker, L.H. Ultra-processed food and incident type 2 diabetes: Studying the underlying consumption patterns to unravel the health effects of this heterogeneous food category in the prospective Lifelines cohort. BMC Med. 2022, 20, 7. [Google Scholar] [CrossRef]
- Llavero-Valero, M.; Escalada-San Martín, J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M. Ultra-processed foods and type-2 diabetes risk in the SUN project: A prospective cohort study. Clin. Nutr. 2021, 40, 2817–2824. [Google Scholar] [CrossRef]
- Martinez Steele, E.; Juul, F.; Neri, D.; Rauber, F.; Monteiro, C.A. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev. Med. 2019, 125, 40–48. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. 2), 21–28. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Lawrence, M.; Millett, C.; Nestle, M.; Popkin, B.M.; Scrinis, G.; Swinburn, B. The need to reshape global food processing: A call to the United Nations Food Systems Summit. BMJ Glob. Health 2021, 6, e006885. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, Z.; Du, W.; Huang, F.; Jiang, H.; Bai, J.; Zhang, X.; Zhang, B.; Wang, H. Twenty-Five-Year Trends in Dietary Patterns among Chinese Adults from 1991 to 2015. Nutrients 2021, 13, 1327. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shi, Z. Ultra-Processed Food Consumption Associated with Overweight/Obesity among Chinese Adults-Results from China Health and Nutrition Survey 1997–2011. Nutrients 2021, 13, 2796. [Google Scholar] [CrossRef]
- Li, M.; Shi, Z. Association between Ultra-Processed Food Consumption and Diabetes in Chinese Adults-Results from the China Health and Nutrition Survey. Nutrients 2022, 14, 4241. [Google Scholar] [CrossRef]
- Li, M.; Shi, Z. Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults-Results from China Health and Nutrition Survey 1997–2015. Nutrients 2022, 14, 4783. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989–2011. Obes. Rev. 2014, 15 (Suppl. S1), 2–7. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Yang, Y. China Food Composition 2004; Peking University Medical Press: Beijing, China, 2005. [Google Scholar]
- Yang, Y.; Wang, Y.; Pan, X. China Food Composition 2009; Peking University Medical Press: Beijing, China, 2010. [Google Scholar]
- Heng, D.; Ma, S.; Lee, J.J.; Tai, B.C.; Mak, K.H.; Hughes, K.; Chew, S.K.; Chia, K.S.; Tan, C.E.; Tai, E.S. Modification of the NCEP ATP III definitions of the metabolic syndrome for use in Asians identifies individuals at risk of ischemic heart disease. Atherosclerosis 2006, 186, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [PubMed]
- Lavigne-Robichaud, M.; Moubarac, J.C.; Lantagne-Lopez, S.; Johnson-Down, L.; Batal, M.; Laouan Sidi, E.A.; Lucas, M. Diet quality indices in relation to metabolic syndrome in an Indigenous Cree (Eeyouch) population in northern Quebec, Canada. Public Health Nutr. 2018, 21, 172–180. [Google Scholar] [CrossRef]
- Ivancovsky-Wajcman, D.; Fliss-Isakov, N.; Webb, M.; Bentov, I.; Shibolet, O.; Kariv, R.; Zelber-Sagi, S. Ultra-processed food is associated with features of metabolic syndrome and non-alcoholic fatty liver disease. Liver Int. 2021, 41, 2635–2645. [Google Scholar] [CrossRef] [PubMed]
- Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-analysis. Br. J. Nutr. 2021, 125, 308–318. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.S.; Guerrero, D.B.; Soto, M.B.; Diaz, S.P.; Martinez-Olmos, M.; Vidal, O. Metabolic syndrome, insulin resistance and the inflammation markers C-reactive protein and ferritin. Eur. J. Clin. Nutr. 2006, 60, 802–809. [Google Scholar] [CrossRef]
- Christ, A.; Lauterbach, M.; Latz, E. Western Diet and the Immune System: An Inflammatory Connection. Immunity 2019, 51, 794–811. [Google Scholar] [CrossRef]
- Batal, M.; Johnson-Down, L.; Moubarac, J.C.; Ing, A.; Fediuk, K.; Sadik, T.; Tikhonov, C.; Chan, L.; Willows, N. Quantifying associations of the dietary share of ultra-processed foods with overall diet quality in First Nations peoples in the Canadian provinces of British Columbia, Alberta, Manitoba and Ontario. Public Health Nutr. 2018, 21, 103–113. [Google Scholar] [CrossRef]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Abou-Setta, A.M.; Chauhan, B.F.; Rabbani, R.; Lys, J.; Copstein, L.; Mann, A.; Jeyaraman, M.M.; Reid, A.E.; Fiander, M.; et al. Nonnutritive sweeteners and cardiometabolic health: A systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. Can. Med. Assoc. J. 2017, 189, E929–E939. [Google Scholar] [CrossRef]
- Fardet, A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: A preliminary study with 98 ready-to-eat foods. Food Funct. 2016, 7, 2338–2346. [Google Scholar] [CrossRef]
- Fardet, A.; Mejean, C.; Laboure, H.; Andreeva, V.A.; Feron, G. The degree of processing of foods which are most widely consumed by the French elderly population is associated with satiety and glycemic potentials and nutrient profiles. Food Funct. 2017, 8, 651–658. [Google Scholar] [CrossRef]
- Ayton, A.; Ibrahim, A. The Western diet: A blind spot of eating disorder research?—A narrative review and recommendations for treatment and research. Nutr. Rev. 2020, 78, 579–596. [Google Scholar] [CrossRef] [PubMed]
- Ford, H.E.; Peters, V.; Martin, N.M.; Sleeth, M.L.; Ghatei, M.A.; Frost, G.S.; Bloom, S.R. Effects of oral ingestion of sucralose on gut hormone response and appetite in healthy normal-weight subjects. Eur. J. Clin. Nutr. 2011, 65, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, R.D.; Pimenta, A.M.; Gea, A.; de la Fuente-Arrillaga, C.; Martinez-Gonzalez, M.A.; Lopes, A.C.; Bes-Rastrollo, M. Ultraprocessed food consumption and risk of overweight and obesity: The University of Navarra Follow-Up (SUN) cohort study. Am. J. Clin. Nutr. 2016, 104, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Julia, C.; Martinez, L.; Alles, B.; Touvier, M.; Hercberg, S.; Mejean, C.; Kesse-Guyot, E. Contribution of ultra-processed foods in the diet of adults from the French NutriNet-Sante study. Public Health Nutr. 2018, 21, 27–37. [Google Scholar] [CrossRef]
- Silva, F.M.; Giatti, L.; de Figueiredo, R.C.; Molina, M.; de Oliveira Cardoso, L.; Duncan, B.B.; Barreto, S.M. Consumption of ultra-processed food and obesity: Cross sectional results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort (2008–2010). Public Health Nutr. 2018, 21, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Dicken, S.J.; Batterham, R.L. The Role of Diet Quality in Mediating the Association between Ultra-Processed Food Intake, Obesity and Health-Related Outcomes: A Review of Prospective Cohort Studies. Nutrients 2021, 14, 23. [Google Scholar] [CrossRef] [PubMed]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Lin, Y.; Liu, Y.; Chen, K. Antibiotic exposure and risk of type 2 diabetes mellitus: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2021, 28, 65052–65061. [Google Scholar] [CrossRef]
- Li, X.; Song, J.; Lin, T.; Dixon, J.; Zhang, G.; Ye, H. Urbanization and health in China, thinking at the national, local and individual levels. Environ. Health 2016, 15 (Suppl. S1), 32. [Google Scholar] [CrossRef]
- Zhai, F.; Wang, H.; Du, S.; He, Y.; Wang, Z.; Ge, K.; Popkin, B.M. Prospective study on nutrition transition in China. Nutr. Rev. 2009, 67 (Suppl. S1), S56–S61. [Google Scholar] [CrossRef]
- Attard, S.M.; Howard, A.G.; Herring, A.H.; Zhang, B.; Du, S.; Aiello, A.E.; Popkin, B.M.; Gordon-Larsen, P. Differential associations of urbanicity and income with physical activity in adults in urbanizing China: Findings from the population-based China Health and Nutrition Survey 1991–2009. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 152. [Google Scholar] [CrossRef] [PubMed]
- Elizabeth, L.; Machado, P.; Zinocker, M.; Baker, P.; Lawrence, M. Ultra-Processed Foods and Health Outcomes: A Narrative Review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef]
| Quartile of UPF (g/Day) | |||||
|---|---|---|---|---|---|
| Q1 (<6.5) | Q2 (6.5–16.3) | Q3 (16.3–36.1) | Q4 (>36.1) | p-Value | |
| Gender | 0.070 | ||||
| Men | 610 (47.4) | 636 (49.4) | 651 (50.6) | 676 (52.5) | |
| Women | 676 (52.6) | 652 (50.6) | 635 (49.4) | 611 (47.5) | |
| Age | 0.566 | ||||
| 18–44 | 435 (33.8) | 455 (35.3) | 437 (34.0) | 477 (37.1) | |
| 45–59 | 511 (39.7) | 501 (38.9) | 525 (40.8) | 483 (37.5) | |
| ≥60 | 340 (26.4) | 332 (25.8) | 324 (25.2) | 327 (25.4) | |
| Education level | <0.001 | ||||
| Junior high school or below | 1050 (81.7) | 984 (76.4) | 954 (74.2) | 777 (60.4) | |
| Senior high school or above | 236 (18.4) | 304 (23.6) | 332 (25.8) | 510 (39.6) | |
| Place of residence | <0.001 | ||||
| Urban areas | 267 (20.8) | 352 (27.3) | 445 (34.6) | 626 (48.6) | |
| Rural areas | 1019 (79.2) | 936 (72.7) | 841 (65.4) | 661 (51.4) | |
| Region of residence | <0.001 | ||||
| Northern regions | 424 (33.0) | 493 (38.3) | 475 (36.9) | 554 (43.1) | |
| Southern regions | 862 (67.0) | 795 (61.7) | 811 (63.1) | 733 (56.9) | |
| Individual annual income | <0.001 | ||||
| Low | 536 (41.7) | 493 (38.3) | 411 (32.0) | 303 (23.5) | |
| Medium | 449 (34.9) | 450 (34.9) | 436 (33.9) | 370 (28.8) | |
| High | 301 (23.4) | 345 (26.8) | 439 (34.1) | 614 (47.7) | |
| Smoking history | 0.340 | ||||
| Yes | 382 (29.7) | 346 (26.9) | 369 (28.7) | 382 (29.7) | |
| No | 904 (70.3) | 942 (73.1) | 917 (71.3) | 905 (70.3) | |
| Drinking past year | 0.549 | ||||
| Yes | 393 (30.6) | 387 (30.1) | 399 (31.0) | 419 (32.6) | |
| No | 893 (69.4) | 901 (70.0) | 887 (69.0) | 868 (67.4) | |
| Physical activity | <0.001 | ||||
| Low | 424 (33.0) | 405 (31.4) | 422 (32.8) | 464 (36.1) | |
| Medium | 406 (31.6) | 427 (33.2) | 410 (31.9) | 475 (36.9) | |
| High | 456 (35.5) | 456 (35.4) | 454 (35.3) | 348 (27.0) | |
| Urbanization | <0.001 | ||||
| Low | 571 (44.4) | 487 (37.8) | 402 (31.3) | 321 (24.9) | |
| Medium | 414 (32.2) | 424 (32.9) | 422 (32.8) | 417 (32.4) | |
| High | 301 (23.4) | 377 (29.3) | 462 (35.9) | 549 (42.7) | |
| BMI (kg/m2) | 0.014 | ||||
| <18.5 | 82 (6.4) | 97 (7.5) | 84 (6.5) | 70 (5.4) | |
| 18.5–23.9 | 812 (63.1) | 758 (58.9) | 761 (59.2) | 742 (57.7) | |
| ≥24.0 | 392 (30.5) | 433 (33.6) | 441 (34.3) | 475 (36.9) | |
| Energy (kcal/day) | 2165.5 ± 703.2 | 2188.5 ± 677.1 | 2217.8 ± 709.9 | 2259.2 ± 743.4 | 0.025 |
| Protein (g/day) | 66.1 ± 24.1 | 69.9 ± 24.8 | 72.2 ± 26.9 | 76.4 ± 30.4 | <0.001 |
| Fat (g/day) | 74.5 ± 38.4 | 79.1 ± 38.5 | 83.3 ± 41.3 | 88.8 ± 43.7 | <0.001 |
| Carbohydrate (g/day) | 299.1 ± 117.2 | 286.6 ± 108.4 | 282.2 ± 106.7 | 278.1 ± 109.6 | <0.001 |
| Sodium (mg/day) | 4380.3 ± 4188.8 | 4778.0 ± 3575.4 | 5439.8 ± 6152.9 | 5859.4 ± 5939.3 | <0.001 |
| WC (cm) | 79.95 ± 9.33 | 80.35 ± 9.34 | 80.43 ± 10.50 | 80.68 ± 10.73 | 0.052 |
| TG (mmol/L) | 1.21 ± 0.77 | 1.23 ± 0.80 | 1.21 ± 0.83 | 1.18 ± 0.73 | 0.284 |
| HDL-C (mmol/L) | 1.49 ± 0.37 | 1.49 ± 0.44 | 1.47 ± 0.42 | 1.45 ± 0.35 | 0.045 |
| SBP (mmHg) | 121.54 ± 17.06 | 122.17 ± 17.09 | 122.47 ± 17.05 | 121.32 ± 15.94 | 0.272 |
| DBP (mmHg) | 78.58 ± 10.72 | 79.24 ± 10.90 | 79.18 ± 10.31 | 78.59 ± 9.75 | 0.199 |
| FPG (mmol/L) | 5.12 ± 1.02 | 5.11 ± 0.99 | 5.09 ± 0.90 | 5.03 ± 0.97 | 0.011 |
| Quartile of UPF (g/Day) | |||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | p Trend | |
| MetS a | |||||
| Median | 3.3 | 10.9 | 23.5 | 60.8 | |
| Model 1 | 1.00 (ref) | 1.08 (0.95, 1.24) | 1.08 (0.94, 1.24) | 1.14 (0.99, 1.31) | 0.126 |
| Model 2 | 1.00 (ref) | 1.08 (0.95, 1.24) | 1.09 (0.95, 1.25) | 1.16 (1.00, 1.33) * | 0.075 |
| Model 3 | 1.00 (ref) | 1.08 (0.94, 1.23) | 1.08 (0.94, 1.24) | 1.17 (1.01, 1.35) * | 0.047 |
| Central obesity b | |||||
| Median | 3.3 | 11.6 | 26.5 | 67.0 | |
| Model 1 | 1.00 (ref) | 1.07 (0.95, 1.20) | 1.12 (0.99, 1.26) | 1.28 (1.13, 1.44) *** | <0.001 |
| Model 2 | 1.00 (ref) | 1.08 (0.96, 1.21) | 1.13 (1.01, 1.28) * | 1.30 (1.15, 1.47) *** | <0.001 |
| Model 3 | 1.00 (ref) | 1.07 (0.95, 1.20) | 1.13 (1.01, 1.28) * | 1.33 (1.18, 1.51) *** | <0.001 |
| Raised TG c | |||||
| Median | 3.4 | 11.4 | 25.0 | 63.5 | |
| Model 1 | 1.00 (ref) | 1.06 (0.91, 1.23) | 1.07 (0.92, 1.25) | 1.25 (1.07, 1.46) ** | 0.003 |
| Model 2 | 1.00 (ref) | 1.06 (0.91, 1.24) | 1.08 (0.92, 1.25) | 1.26 (1.08, 1.48) ** | 0.002 |
| Model 3 | 1.00 (ref) | 1.06 (0.91, 1.23) | 1.08 (0.92, 1.26) | 1.26 (1.08, 1.48) ** | 0.003 |
| Reduced HDL-C d | |||||
| Median | 3.4 | 11.0 | 23.7 | 60.3 | |
| Model 1 | 1.00 (ref) | 1.07 (0.92, 1.24) | 1.21 (1.04, 1.40) * | 1.18 (1.01, 1.38) * | 0.044 |
| Model 2 | 1.00 (ref) | 1.08 (0.93, 1.25) | 1.22 (1.05, 1.41) ** | 1.21 (1.04, 1.41) * | 0.023 |
| Model 3 | 1.00 (ref) | 1.08 (0.93, 1.26) | 1.24 (1.07, 1.44) ** | 1.25 (1.07, 1.46) ** | 0.007 |
| Raised BP e | |||||
| Median | 3.3 | 11.6 | 26.9 | 66.9 | |
| Model 1 | 1.00 (ref) | 1.05 (0.94, 1.17) | 1.05 (0.93, 1.17) | 1.14 (1.02, 1.29) * | 0.033 |
| Model 2 | 1.00 (ref) | 1.06 (0.95, 1.18) | 1.05 (0.94, 1.18) | 1.16 (1.03, 1.31) * | 0.022 |
| Model 3 | 1.00 (ref) | 1.05 (0.94, 1.18) | 1.04 (0.93, 1.16) | 1.16 (1.03, 1.32) * | 0.018 |
| Raised FPG f | |||||
| Median | 3.4 | 11.3 | 25.2 | 64.4 | |
| Model 1 | 1.00 (ref) | 1.04 (0.92, 1.18) | 1.04 (0.92, 1.17) | 1.07 (0.94, 1.22) | 0.404 |
| Model 2 | 1.00 (ref) | 1.06 (0.94, 1.20) | 1.05 (0.93, 1.19) | 1.09 (0.96, 1.24) | 0.287 |
| Model 3 | 1.00 (ref) | 1.05 (0.93, 1.19) | 1.07 (0.94, 1.21) | 1.11 (0.98, 1.27) | 0.141 |
| Quartile of UPF (g/Day) | |||||
|---|---|---|---|---|---|
| Q1 (<6.5) | Q2 (6.5–16.3) | Q3 (16.3–36.1) | Q4 (>36.1) | p for Interaction | |
| Gender | 0.208 | ||||
| Men | 1.00 (ref) | 1.12 (0.93, 1.36) | 1.06 (0.87, 1.28) | 1.09 (0.89, 1.33) | |
| Women | 1.00 (ref) | 1.00 (0.82, 1.22) | 1.10 (0.90, 1.34) | 1.26 (1.02, 1.55) * | |
| Age | 0.093 | ||||
| 18–44 | 1.00 (ref) | 0.98 (0.76, 1.26) | 0.91 (0.70, 1.18) | 0.97 (0.74, 1.27) | |
| 45–59 | 1.00 (ref) | 1.16 (0.94, 1.44) | 1.27 (0.91, 1.40) | 1.29 (1.03, 1.61) * | |
| ≥60 | 1.00 (ref) | 1.02 (0.80, 1.32) | 1.16 (0.90, 1.50) | 1.27 (0.96, 1.66) | |
| Education level | 0.250 | ||||
| Junior high school or below | 1.00 (ref) | 1.14 (0.98, 1.32) | 1.14 (0.97, 1.33) | 1.13 (0.95, 1.34) | |
| Senior high school or above | 1.00 (ref) | 0.83 (0.60, 1.14) | 0.88 (0.64, 1.20) | 1.13 (0.84, 1.51) | |
| Place of residence | 0.013 | ||||
| Urban areas | 1.00 (ref) | 1.19 (0.89, 1.60) | 1.11 (0.84, 1.47) | 1.41 (1.07, 1.86) * | |
| Rural areas | 1.00 (ref) | 1.05 (0.90, 1.22) | 1.09 (0.92, 1.28) | 1.01 (0.84, 1.21) | |
| Region of residence | 0.365 | ||||
| Northern regions | 1.00 (ref) | 0.95 (0.76, 1.18) | 1.00 (0.80, 1.25) | 1.02 (0.81, 1.28) | |
| Southern regions | 1.00 (ref) | 1.17 (0.98, 1.39) | 1.14 (0.95, 1.36) | 1.29 (1.06, 1.55) ** | |
| Individual annual income | 0.252 | ||||
| Low | 1.00 (ref) | 1.04 (0.84, 1.29) | 1.05 (0.83, 1.32) | 1.22 (0.95, 1.58) | |
| Medium | 1.00 (ref) | 1.17 (0.94, 1.47) | 1.06 (0.83, 1.34) | 1.05 (0.81, 1.36) | |
| High | 1.00 (ref) | 0.98 (0.74, 1.30) | 1.11 (0.85, 1.44) | 1.17 (0.90, 1.51) | |
| Urbanization | 0.008 | ||||
| Low | 1.00 (ref) | 1.13 (0.91, 1.39) | 1.09 (0.87, 1.36) | 0.99 (0.77, 1.29) | |
| Medium | 1.00 (ref) | 1.01 (0.79, 1.29) | 1.02 (0.79, 1.32) | 0.96 (0.74, 1.24) | |
| High | 1.00 (ref) | 1.08 (0.82, 1.41) | 1.15 (0.86, 1.49) | 1.45 (1.11, 1.89) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, F.; Wang, Z.; Wang, H.; Zhang, J.; Su, C.; Jia, X.; Du, W.; Jiang, H.; Li, W.; Wang, L.; et al. Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China—Results from the China Health and Nutrition Survey. Nutrients 2023, 15, 752. https://doi.org/10.3390/nu15030752
Pan F, Wang Z, Wang H, Zhang J, Su C, Jia X, Du W, Jiang H, Li W, Wang L, et al. Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China—Results from the China Health and Nutrition Survey. Nutrients. 2023; 15(3):752. https://doi.org/10.3390/nu15030752
Chicago/Turabian StylePan, Feng, Zhihong Wang, Huijun Wang, Jiguo Zhang, Chang Su, Xiaofang Jia, Wenwen Du, Hongru Jiang, Weiyi Li, Liusen Wang, and et al. 2023. "Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China—Results from the China Health and Nutrition Survey" Nutrients 15, no. 3: 752. https://doi.org/10.3390/nu15030752
APA StylePan, F., Wang, Z., Wang, H., Zhang, J., Su, C., Jia, X., Du, W., Jiang, H., Li, W., Wang, L., Hao, L., Zhang, B., & Ding, G. (2023). Association between Ultra-Processed Food Consumption and Metabolic Syndrome among Adults in China—Results from the China Health and Nutrition Survey. Nutrients, 15(3), 752. https://doi.org/10.3390/nu15030752







