Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Participants
2.3. Measurement of Variables
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
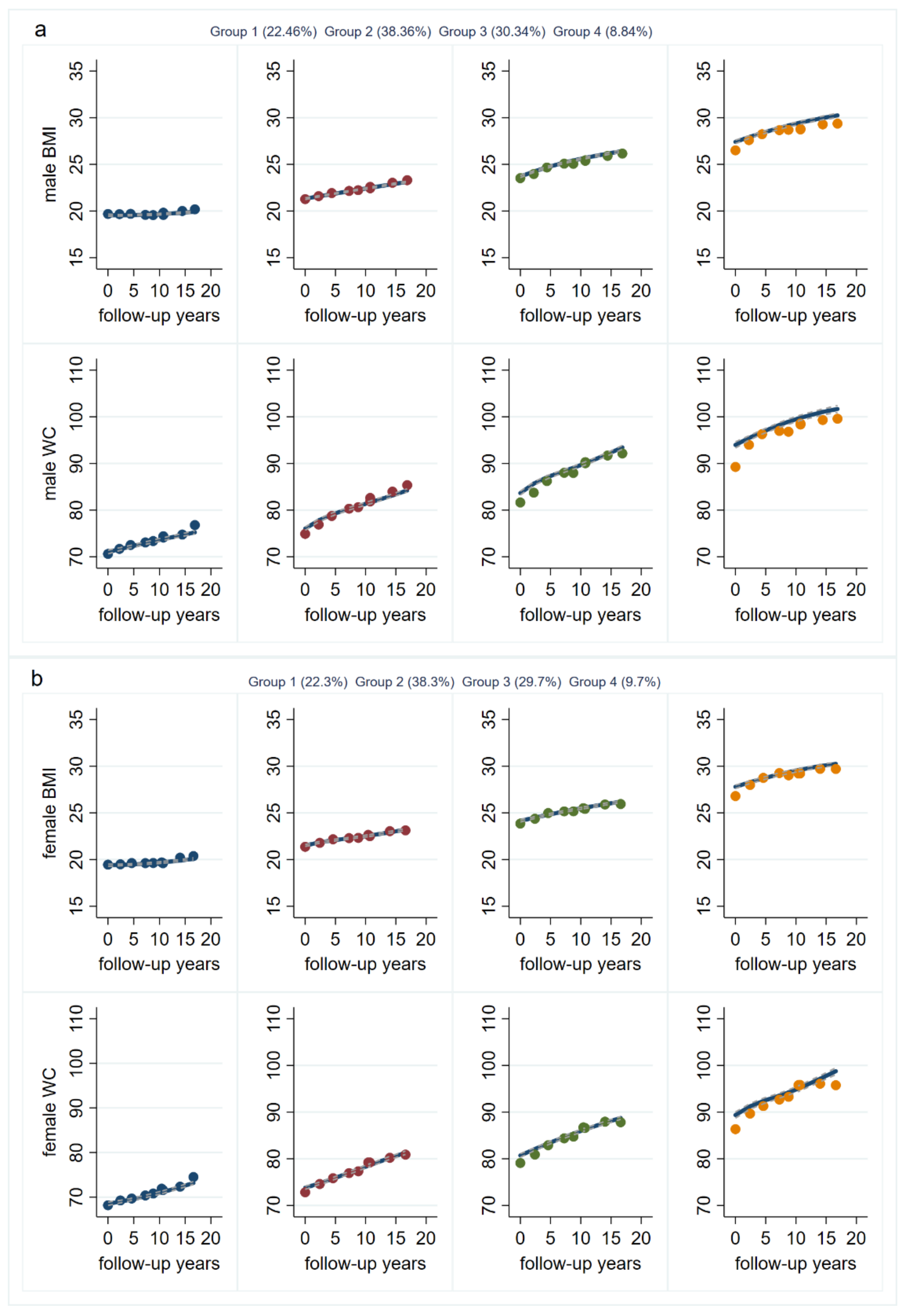
3.1. BMI and WC Trajectories
3.2. Baseline Characteristics by Trajectory Group
3.3. Associations between Multi-Trajectories and Hypertension
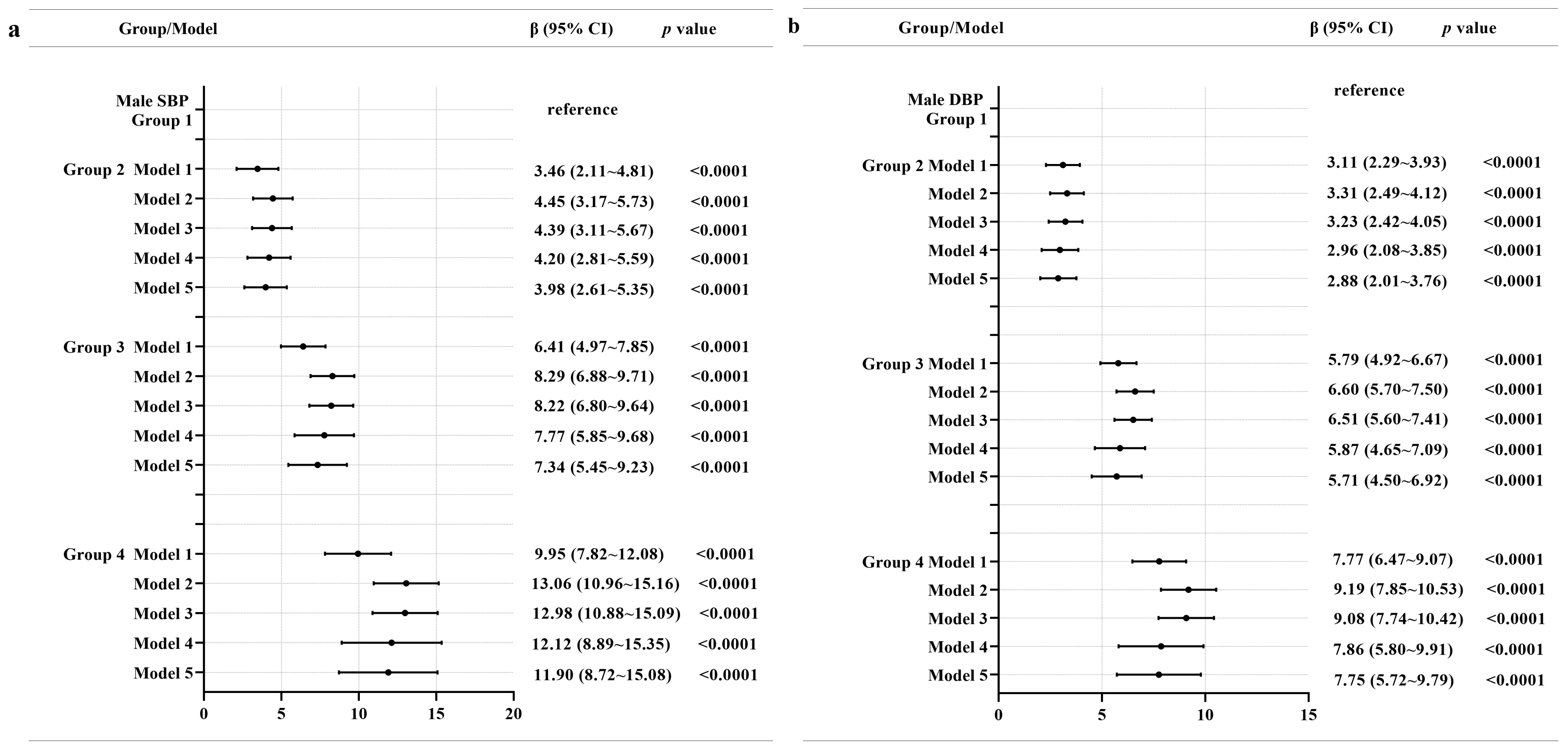
3.4. Associations between Multiple Trajectories and SBP and DBP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Y.; Yang, L.; Wang, L.; Zhang, M.; Huang, Z.; Deng, Q.; Zhou, M.; Chen, Z.; Wang, L. Burden of hypertension in China A nationally representative survey of 174621 adults. Int. J. Cardiol. 2017, 227, 516–523. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization (WHO) Hypertension. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 9 August 2022).
- Acta Nutrimenta Sinica. Report on Nutrition and Chronic Diseases in China; Acta Nutrimenta Sinica: Beijing, China, 2020. [Google Scholar]
- Lu, J.; Lu, Y.; Wang, X.; Li, X.; Linderman, G.C.; Wu, C.; Cheng, X.; Mu, L.; Zhang, H.; Liu, J.; et al. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017, 390, 2549–2558. [Google Scholar] [CrossRef] [PubMed]
- Stanaway, J.D.; Afshin, A.; Gakidou, S.L.S.E.; Abate, D.; Abate, K.H.; Gakidou, E. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Ye, R.; Liu, K.; Zhang, Z.; Gong, S.; Chen, X. Health-related quality of life of hypertension in China: A systematic review and meta-analysis. J. Cardiovasc. Med. 2018, 19, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.J.; Wang, H.C.; Li, Y.C.; Zhao, W.H. Hypertension screening and follow-up management by Primary Health Care System among Chinese population aged 35 years and above. Biomed. Environ. Sci. 2015, 28, 330–340. [Google Scholar]
- Nurdiantami, Y.; Watanabe, K.; Tanaka, E.; Pradono, J.; Anme, T. Association of general and central obesity with hypertension. Clin. Nutr. 2018, 37, 1259–1263. [Google Scholar] [CrossRef]
- Hasan, M.; Shihab, L.A.M.A. Body mass index and risk of incident hypertension over the life Course: The Johns Hopkins Precursors Study. Circulation 2012, 126, 2983–2989. [Google Scholar]
- Wu, X.; Li, B.; Lin, W.Q.; Huang, L.L.; Wang, X.X.; Fu, L.Y.; Li, B.B.; Wang, P.X. The association between obesity indices and hypertension: Which index is the most notable indicator of hypertension in different age groups stratified by sex? Clin. Exp. Hypertens. 2019, 41, 373–380. [Google Scholar] [CrossRef]
- Zhou, Z.; Hu, D.; Chen, J. Association between obesity indices and blood pressure or hypertension: Which index is the best? Public Health Nutr. 2009, 12, 1061–1071. [Google Scholar] [CrossRef]
- Zhang, X.; Yao, S.; Sun, G.; Yu, S.; Sun, Z.; Zheng, L.; Xu, C.; Li, J.; Sun, Y. Total and abdominal obesity among rural Chinese women and the association with hypertension. Nutrition 2012, 28, 46–52. [Google Scholar] [CrossRef]
- Hu, L.; Huang, X.; You, C.; Li, J.; Hong, K.; Li, P.; Wu, Y.; Wu, Q.; Bao, H.; Cheng, X. Prevalence and risk factors of prehypertension and hypertension in Southern China. PLoS ONE 2017, 12, e170238. [Google Scholar] [CrossRef]
- Linderman, G.C.; Lu, J.; Lu, Y.; Sun, X.; Xu, W.; Nasir, K.; Schulz, W.; Jiang, L.; Krumholz, H.M. Association of body mass index with blood pressure among 1.7 million Chinese Adults. JAMA Netw. Open 2018, 1, e181271. [Google Scholar] [CrossRef] [PubMed]
- Foulds, H.J.A.; Bredin, S.S.D.; Warburton, D.E.R. The relationship between hypertension and obesity across different ethnicities. J. Hypertens. 2012, 30, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, R.; Upadhyay, S.K.; Khatri, B.; Bhattarai, J.R.; Kayastha, M.; Upadhyay, M.P. BMI, waist to height ratio and waist circumference as a screening tool for hypertension in hospital outpatients: A cross-sectional, non-inferiority study. BMJ Open 2021, 11, e50096. [Google Scholar] [CrossRef] [PubMed]
- Rachel, P.; Wildman, D.G.K.R.; Gakidou, E. Are waist circumference and body mass index independently associated with cardiovascular disease risk in Chinese adults 1–3. Am. J. Clin. Nutr. 2005, 82, 1195–1202. [Google Scholar]
- Luo, W.; Guo, Z.; Hu, X.; Zhou, Z.; Ming, W.; Zhang, L.; Liu, J. A prospective study on association between 2 years change of waist circumference and incident hypertension in Han Chinese. Int. J. Cardiol. 2013, 167, 2781–2785. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, M.; Luo, X.; Wang, C.; Li, L.; Zhang, L.; Wang, B.; Ren, Y.; Zhou, J.; Han, C.; et al. Association of 6-year waist circumference gain and incident hypertension. Heart 2017, 103, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Zheng, M.; Wu, S.; Chen, M.; Cai, J.; Yang, X. Waist circumference and incidence of hypertension in Chinese adults. Herz 2017, 42, 677–683. [Google Scholar] [CrossRef]
- Adegbija, O.; Hoy, W.; Wang, Z. Prediction of cardiovascular disease risk using waist circumference among Aboriginals in a remote Australian community. BMC Public Health 2015, 15, 57. [Google Scholar] [CrossRef] [PubMed]
- Nagin, D.S.; Odgers, C.L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef] [PubMed]
- Fan, B.; Yang, Y.; Dayimu, A.; Zhou, G.; Liu, Y.; Li, S.; Chen, W.; Zhang, T.; Xue, F. Body mass index trajectories during young adulthood and incident hypertension: A longitudinal cohort in Chinese population. J. Am. Heart Assoc. 2019, 8, e011937. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Sun, L.; Zeng, Q. Trajectories of mid-life to elderly adulthood BMI and incident hypertension: The China Health and Nutrition Survey. BMJ Open 2021, 11, e47920. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Yi, Y.; Roebothan, B.; Colbourne, J.; Maddalena, V.; Wang, P.P.; Sun, G. Body mass index trajectories among middle-aged and elderly canadians and associated health outcomes. J. Environ. Public Health 2016, 2016, 7014857. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Li, Y.; Ma, W.; Jia, C. Trajectories of waist circumference during young adulthood and incident hypertension: The China Health and Nutrition Survey. J. Hum. Hypertens. 2022, 36, 767–774. [Google Scholar] [CrossRef]
- Ahanchi, N.S.; Tamehri Zadeh, S.S.; Khalili, D.; Azizi, F.; Hadaegh, F. Sex specific trajectories of central adiposity, lipid indices, and glucose level with incident hypertension: 12 years Follow-up in Tehran lipid and glucose study. J. Transl. Med. 2021, 19, 84. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhao, Y.; Wang, G.; Zhang, H.; Ren, Y.; Wang, B.; Zhang, L.; Yang, X.; Han, C.; Pang, C.; et al. Body mass index and waist circumference combined predicts obesity-related hypertension better than either alone in a rural Chinese population. Sci. Rep. 2016, 6, 31935. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China health and nutrition survey, 1989–2011. Obes. Rev. 2014, 15, 2–7. [Google Scholar] [CrossRef]
- WS/T 428-2013; Criteria of Weight for Adults. Standards Press of China: Beijing, China, 2013.
- Joint Committee for Guideline Revision. 2018 Chinese guidelines for the management of hypertension. Chin J Cardiovasc Med. 2019, 24, 24–56. [Google Scholar]
- Jones, B.L.; Nagin, D.S. A note on a stata plugin for estimating group-based trajectory models. Sociol. Methods. Res. 2013, 42, 608–613. [Google Scholar] [CrossRef]
- Jones, B.L.; Nagin, D.S. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol. Methods. Res. 2007, 35, 542–571. [Google Scholar] [CrossRef]
- Nagin, D.S.; Jones, B.L.; Passos, V.L.; Tremblay, R.E. Group-based multi-trajectory modeling. Stat. Methods Med. Res. 2018, 27, 2015–2023. [Google Scholar] [CrossRef] [PubMed]
- Ford, N.D.; Martorell, R.; Mehta, N.K.; Perrine, C.G.; Ramirez-Zea, M.; Stein, A.D. Lifecourse body mass index trajectories and cardio-metabolic disease risk in Guatemalan adults. PLoS ONE 2020, 15, e240904. [Google Scholar] [CrossRef] [PubMed]
- Araujo, J.; Barros, H.; Ramos, E.; Li, L. Trajectories of total and central adiposity throughout adolescence and cardiometabolic factors in early adulthood. Int. J. Obes. 2016, 40, 1899–1905. [Google Scholar] [CrossRef]
- Wang, L.; Lee, Y.; Wu, Y.; Zhang, X.; Jin, C.; Huang, Z.; Wang, Y.; Wang, Z.; Kris-Etherton, P.; Wu, S.; et al. A prospective study of waist circumference trajectories and incident cardiovascular disease in China: The Kailuan Cohort Study. Am. J. Clin. Nutr. 2021, 113, 338–347. [Google Scholar] [CrossRef]
- Kuchibhatla, M.N.; Fillenbaum, G.G.; Kraus, W.E.; Cohen, H.J.; Blazer, D.G. Trajectory classes of body mass index in a representative elderly community sample. J. Gerontol. Ser. A 2013, 68, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Xian, H.; Vasilopoulos, T.; Liu, W.; Hauger, R.L.; Jacobson, K.C.; Lyons, M.J.; Panizzon, M.; Reynolds, C.A.; Vuoksimaa, E.; Kremen, W.S.; et al. Steeper change in body mass across four decades predicts poorer cardiometabolic outcomes at midlife. Obesity 2017, 25, 773–780. [Google Scholar] [CrossRef]
- Fan, H.; Zhang, X. Body mass index trajectory across childhood and subsequent risk of elevated blood pressure. J. Clin. Hypertens. 2020, 22, 1902–1907. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Cao, S.; Liu, B.; Li, H.; Song, F.; Gan, Y.; Li, W.; Opoku, S.; Yan, S.; Yue, W.; et al. Association of general and central adiposity with blood pressure among Chinese adults. J. Hypertens. 2018, 36, 2406–2413. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.; Smith, G.D. A Life Course Approach to Chronic Disease Epidemiology. Annu. Rev. Public Health 2005, 26, 1–35. [Google Scholar] [CrossRef]
- Mikkelsen, B.; Williams, J.; Rakovac, I.; Wickramasinghe, K.; Hennis, A.; Shin, H.; Farmer, M.; Weber, M.; Berdzuli, N.; Borges, C.; et al. Life course approach to prevention and control of non-communicable diseases. BMJ 2019, 364, l257. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, Y.; Kuh, D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int. J. Epidemiol. 2002, 31, 285–293. [Google Scholar] [CrossRef] [PubMed]


| Baseline Characteristics | Trajectory Groups | p-Value | |||
|---|---|---|---|---|---|
| Male | Group 1 | Group 2 | Group 3 | Group 4 | |
| N (%) | 1009 (22.46) | 1723 (38.36) | 1363 (30.34) | 397 (8.84) | |
| Age, year (mean [SD]) | 41.31 (14.80) | 39.57 (13.01) | 40.75 (12.69) | 41.21 (13.33) | 0.0080 |
| Education level, N (%) | <0.0001 | ||||
| Primary school and below | 491 (48.66) | 626 (36.33) | 380 (27.88) | 72 (18.14) | |
| Middle school | 341 (33.80) | 646 (37.49) | 501 (36.76) | 174 (43.83) | |
| High school and above | 177 (17.54) | 451 (26.18) | 482 (35.36) | 151 (38.04) | |
| Geographic region, N (%) | <0.0001 | ||||
| Rural | 835 (82.76) | 1258 (73.01) | 801 (58.77) | 215 (54.16) | |
| Urban | 174 (17.27) | 465 (26.99) | 562 (41.23) | 182 (45.84) | |
| Smoking, N (%) | 0.0018 | ||||
| Nonsmoker | 357 (35.38) | 618 (35.87) | 544 (39.91) | 176 (44.33) | |
| Current smoker | 652 (64.62) | 1105 (64.13) | 819 (60.09) | 221 (55.67) | |
| Alcohol drinking, N (%) | <0.0001 | ||||
| Nondrinker | 426 (42.22) | 633 (36.74) | 471 (34.56) | 123 (30.98) | |
| Current drinker | 583 (57.78) | 1090 (63.26) | 892 (65.44) | 274 (69.02) | |
| Follow-up time, year (median [IQR]) | 18.00 (11.00–22.00) | 16.00 (9.00–21.00) | 14.00 (7.00–18.00) | 9.00 (7.00–15.00) | <0.0001 |
| BMI, mg/kg (mean [SD]) | 19.55 (1.57) | 21.28 (1.55) | 23.69 (1.93) | 27.37 (2.36) | <0.0001 |
| WC, cm (mean [SD]) | 70.73 (5.61) | 76.02 (5.95) | 83.69 (7.19) | 93.88 (8.23) | <0.0001 |
| SBP, mmHg (mean [SD]) | 111.37 (10.85) | 113.82 (10.22) | 117.54 (10.20) | 120.28 (9.42) | <0.0001 |
| DBP, mmHg (mean [SD]) | 72.81 (7.71) | 74.27 (7.52) | 76.52 (7.10) | 78.77 (6.21) | <0.0001 |
| Female | Group 1 | Group 2 | Group 3 | Group 4 | |
| N (%) | 1131 (21.92) | 2000 (38.77) | 1536 (29.77) | 492 (9.54) | |
| Age, year (mean [SD]) | 39.87 (14.49) | 40.05 (12.06) | 42.67 (11.91) | 44.78 (12.10) | <0.0001 |
| Education level, N (%) | 0.0054 | ||||
| Primary school and below | 591 (52.25) | 955 (47.75) | 782 (50.91) | 264 (53.66) | |
| Middle school | 294 (25.99) | 581 (29.05) | 423 (27.54) | 154 (31.30) | |
| High school and above | 246 (21.75) | 464 (23.20) | 331 (21.55) | 74 (15.04) | |
| Geographic region, N (%) | <0.0001 | ||||
| Rural | 815 (72.06) | 1344 (67.20) | 975 (63.48) | 313 (63.62) | |
| Urban | 316 (27.94) | 656 (32.80) | 561 (36.52) | 179 (36.38) | |
| Smoking, N (%) | 0.0071 | ||||
| Nonsmoker | 1071 (94.69) | 1937 (96.85) | 1486 (96.74) | 468 (95.12) | |
| Current smoker | 60 (5.31) | 63 (3.15) | 50 (3.26) | 24 (4.88) | |
| Alcohol drinking, N (%) | 0.0596 | ||||
| Nondrinker | 1025 (90.63) | 1791 (89.55) | 1345 (87.57) | 433 (88.01) | |
| Current drinker | 106 (9.37) | 209 (10.45) | 191 (12.43) | 59 (11.99) | |
| Follow-up time, year (median [IQR]) | 16.00 (9.00–21.00) | 14.00 (9.00–21.00) | 14.00 (9.00–21.00) | 12.00 (7.00–18.00) | <0.0001 |
| BMI, mg/kg (mean [SD]) | 19.34 (1.57) | 21.49 (1.62) | 24.15 (1.98) | 27.82 (2.62) | <0.0001 |
| WC, cm (mean [SD]) | 68.28 (5.79) | 73.75 (6.15) | 80.65 (7.07) | 89.28 (7.85) | <0.0001 |
| SBP, mmHg (mean [SD]) | 106.89 (11.82) | 109.95 (11.61) | 113.50 (11.71) | 116.89 (11.08) | <0.0001 |
| DBP, mmHg (mean [SD]) | 70.15 (8.17) | 71.98 (8.08) | 74.21 (7.88) | 76.18 (7.13) | <0.0001 |
| Gender | Model | Trajectory Groups | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Group 1 (N = 1009) | Group 2 (N = 1723) | Group 3 (N = 1363) | Group 4 (N = 397) | ||||
| HR | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | ||
| Model 1 | 1 | 1.34 (1.19~1.51) | <0.0001 | 2.23 (1.98~2.51) | <0.0001 | 3.86 (3.30~4.52) | <0.0001 | |
| Model 2 | 1 | 1.45 (1.29~1.63) | <0.0001 | 2.36 (2.08~2.67) | <0.0001 | 3.71 (3.14~4.38) | <0.0001 | |
| Model 3 | 1 | 1.43 (1.27~1.61) | <0.0001 | 2.33 (2.05~2.64) | <0.0001 | 3.65 (3.09~4.31) | <0.0001 | |
| Model 4 | 1 | 1.33 (1.18~1.51) | <0.0001 | 1.97 (1.68~2.30) | <0.0001 | 2.65 (2.06~3.41) | <0.0001 | |
| Model 5 | 1 | 1.30 (1.15~1.48) | <0.0001 | 1.86 (1.58~2.18) | <0.0001 | 2.60 (2.02~3.34) | <0.0001 | |
| Female | Group 1 (N = 1131) | Group 2 (N = 2000) | Group 3 (N = 1536) | Group 4 (N = 492) | ||||
| HR | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | ||
| Model 1 | 1 | 1.41 (1.24~1.59) | <0.0001 | 2.39 (2.11~2.70) | <0.0001 | 3.75 (3.22~4.36) | <0.0001 | |
| Model 2 | 1 | 1.47 (1.30~1.67) | <0.0001 | 2.30 (2.03~2.61) | <0.0001 | 3.16 (2.71~3.68) | <0.0001 | |
| Model 3 | 1 | 1.48 (1.30~1.67) | <0.0001 | 2.31 (2.04~2.62) | <0.0001 | 3.19 (2.73~3.72) | <0.0001 | |
| Model 4 | 1 | 1.38 (1.21~1.58) | <0.0001 | 2.01 (1.70~2.37) | <0.0001 | 2.51 (1.96~3.21) | <0.0001 | |
| Model 5 | 1 | 1.35 (1.18~1.54) | <0.0001 | 1.92 (1.62~2.26) | <0.0001 | 2.37 (1.85~3.03) | <0.0001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Song, X.; Du, S.; Du, W.; Su, C.; Zhang, J.; Zhang, X.; Jia, X.; Ouyang, Y.; Li, L.; et al. Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients 2023, 15, 751. https://doi.org/10.3390/nu15030751
Wang Q, Song X, Du S, Du W, Su C, Zhang J, Zhang X, Jia X, Ouyang Y, Li L, et al. Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients. 2023; 15(3):751. https://doi.org/10.3390/nu15030751
Chicago/Turabian StyleWang, Qi, Xiaoyun Song, Shufa Du, Wenwen Du, Chang Su, Jiguo Zhang, Xiaofan Zhang, Xiaofang Jia, Yifei Ouyang, Li Li, and et al. 2023. "Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study" Nutrients 15, no. 3: 751. https://doi.org/10.3390/nu15030751
APA StyleWang, Q., Song, X., Du, S., Du, W., Su, C., Zhang, J., Zhang, X., Jia, X., Ouyang, Y., Li, L., Zhang, B., & Wang, H. (2023). Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients, 15(3), 751. https://doi.org/10.3390/nu15030751







