Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Sources and Search Strategy
2.3. Study Selection, Data Extraction and Reporting
2.4. Quality Assessment
3. Results
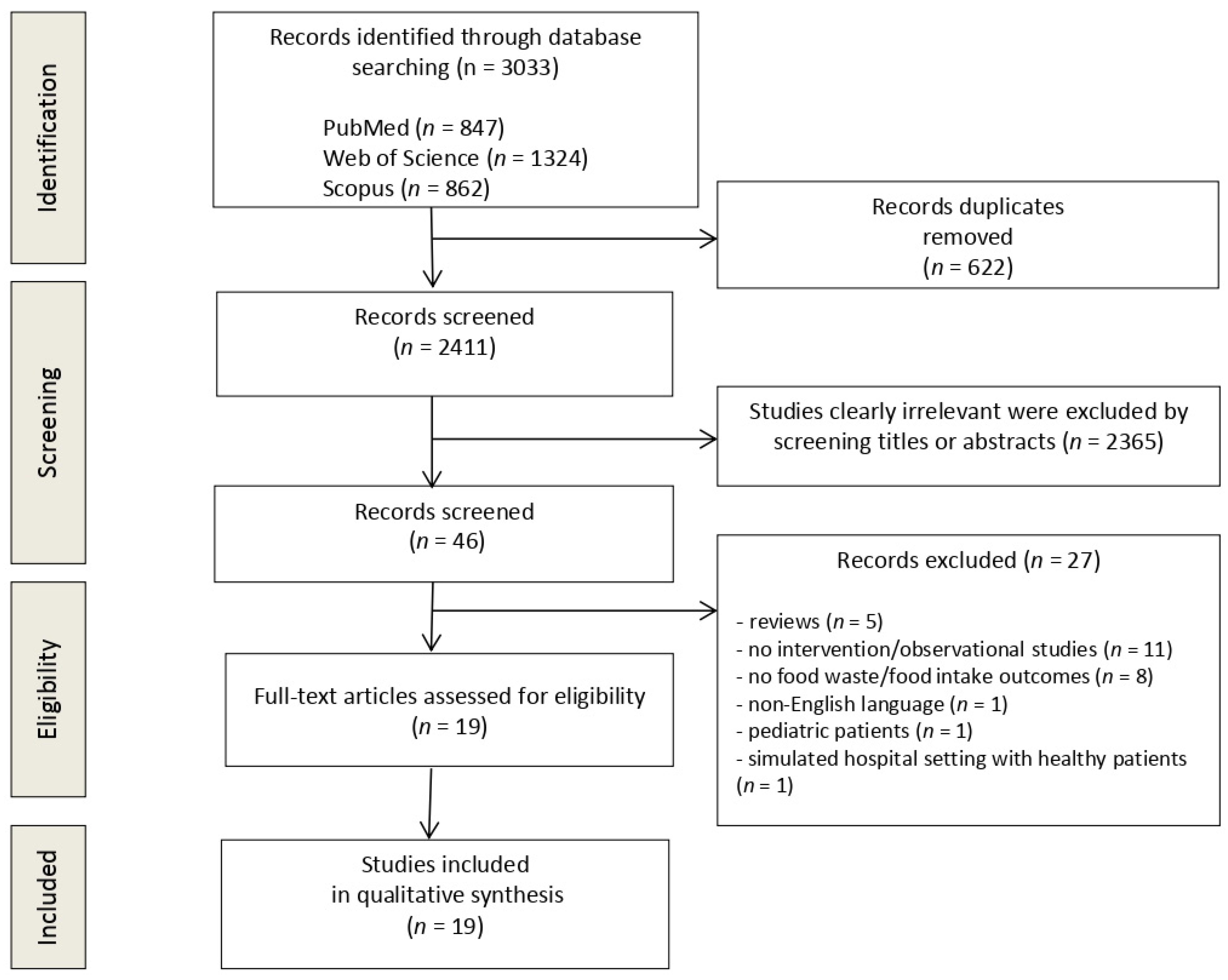
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment
3.4. Results
3.4.1. Food Service Systems including Catering and Room Service (n = 9)
3.4.2. Protected Mealtimes and Volunteer Feeding Assistance (n = 4)
3.4.3. Food Presentation (n = 3)
3.4.4. Nutritional Counselling and Education (n = 2)
3.4.5. Plant-Based Proteins Meal (n = 1)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rinninella, E.; Cintoni, M.; De Lorenzo, A.; Addolorato, G.; Vassallo, G.; Moroni, R.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. Risk, prevalence, and impact of hospital malnutrition in a Tertiary Care Referral University Hospital: A cross-sectional study. Intern. Emerg. Med. 2018, 13, 689–697. [Google Scholar] [CrossRef]
- Barker, L.A.; Gout, B.S.; Crowe, T.C. Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int. J. Environ. Res. Public Health 2011, 8, 514–527. [Google Scholar] [CrossRef] [PubMed]
- Elia, M. The Cost of Malnutrition in England and Potential Cost Savings from Nutritional Interventions; National Institute for Health Research Southampton Biomedical Research Centre: Southampton, UK, 2015. [Google Scholar]
- Schuetz, P.; Seres, D.; Lobo, D.N.; Gomes, F.; Kaegi-Braun, N.; Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet 2021, 398, 1927–1938. [Google Scholar] [CrossRef] [PubMed]
- Sanson, G.; Bertocchi, L.; Dal Bo, E.; Di Pasquale, C.L.; Zanetti, M. Identifying reliable predictors of protein-energy malnutrition in hospitalized frail older adults: A prospective longitudinal study. Int. J. Nurs. Stud. 2018, 82, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Cintoni, M.; De Lorenzo, A.; Anselmi, G.; Gagliardi, L.; Addolorato, G.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. May nutritional status worsen during hospital stay? A sub-group analysis from a cross-sectional study. Intern. Emerg. Med. 2019, 14, 51–57. [Google Scholar] [CrossRef]
- Eriksson, M.; Malefors, C.; Bergström, P.; Eriksson, E.; Osowski, C.P. Quantities and Quantification Methodologies of Food Waste in Swedish Hospital. Sustainability 2020, 12, 3116. [Google Scholar] [CrossRef]
- Alshqaqeep, F.; Twomey, J.; Overcash, M.; Sadkhi, A. A study of food waste in St. Francis Hospital. Int. J. Healthc. Manag. 2017, 13, 24–32. [Google Scholar] [CrossRef]
- Alshqaqeeq, F.; Twomey, J.M.; Overcash, M.R. Food waste in hospitals: Review. Int. J. Healthc. Technol. Manag. 2018, 17, 186–196. [Google Scholar] [CrossRef]
- Edwards, J.S.A.; Nash, A.H.M. The nutritional implications of food wastage in hospital food service management. Nutr. Food Sci. 1999, 99, 89–98. [Google Scholar] [CrossRef]
- Kallbekken, S.; Sælen, H. ‘Nudging’ hotel guests to reduce food waste as a win–win environmental measure. Econ. Lett. 2013, 119, 325–327. [Google Scholar] [CrossRef]
- Hao, N.; Zhang, Y.; Wang, H.; Wang, H.H. Which Consumer Perceptions Should Be Used in Food Waste Reduction Campaigns: Food Security, Food Safety or Environmental Concerns? Sustainability 2022, 14, 2010. [Google Scholar] [CrossRef]
- Chawla, G.; Lugosi, P.; Hawkins, R. Evaluating materiality in food waste reduction interventions. Ann. Tour. Res. Empir. Insights 2020, 1, 100002. [Google Scholar] [CrossRef]
- Heikkilä, L.; Reinikainen, A.; Katajajuuri, J.M.; Silvennoinen, K.; Hartikainen, H. Elements affecting food waste in the food service sector. Waste Manag. 2016, 56, 446–453. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. In Oxford; University of Ottawa: Ottawa, ON, Canada, 2000. [Google Scholar]
- Herzog, R.; Álvarez-Pasquin, M.J.; Díaz, C.; Del Barrio, J.L.; Estrada, J.M.; Gil, Á. Are Healthcare Workers’ Intentions to Vaccinate Related to Their Knowledge, Beliefs and Attitudes? A Systematic Review. BMC Public Health 2013, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. BMJ 2011, 343, 5928. [Google Scholar] [CrossRef]
- Hartwell, H.; Edwrads, J.S.A. A comparative analysis of ‘plated’ and ‘bulk trolley’ hospital food service systems. Food Serv. Technol. 2003, 3, 133–142. [Google Scholar] [CrossRef]
- Edwards, J.S.; Hartwell, H.J. Hospital food service: A comparative analysis of systems and introducing the ‘Steamplicity’ concept. J. Hum. Nutr. Diet. 2006, 19, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Hickson, M.; Fearnley, L.; Thomas, J.; Evans, S. Does a new steam meal catering system meet patient requirements in hospital? J. Hum. Nutr. Diet. 2007, 20, 476–485. [Google Scholar] [CrossRef]
- Rüfenacht, U.; Rühlin, M.; Wegmann, M.; Imoberdorf, R.; Ballmer, P.E. Nutritional counseling improves quality of life and nutrient intake in hospitalized undernourished patients. Nutrition 2010, 26, 53–60. [Google Scholar] [CrossRef]
- Hickson, M.; Connolly, A.; Whelan, K. Impact of protected mealtimes on ward mealtime environment, patient experience and nutrient intake in hospitalised patients. J. Hum. Nutr. Diet. 2011, 24, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Manning, F.; Harris, K.; Duncan, R.; Walton, K.; Bracks, J.; Larby, L.; Vari, L.; Jukkola, K.; Bell, J.; Chan, M.; et al. Additional feeding assistance improves the energy and protein intakes of hospitalised elderly patients. A health services evaluation. Appetite 2012, 59, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Young, A.M.; Mudge, A.M.; Banks, M.D.; Ross, L.J.; Daniels, L. Encouraging, assisting and time to EAT: Improved nutritional intake for older medical patients receiving Protected Mealtimes and/or additional nursing feeding assistance. Clin. Nutr. 2013, 32, 543–549. [Google Scholar] [CrossRef]
- Maunder, K.; Lazarus, C.; Walton, K.; Williams, P.; Ferguson, M.; Beck, E. Energy and protein intake increases with an electronic bedside spoken meal ordering system compared to a paper menu in hospital patients. Clin. Nutr. ESPEN 2015, 10, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Navarro, D.A.; Boaz, M.; Krause, I.; Elis, A.; Chernov, K.; Giabra, M.; Levy, M.; Giboreau, A.; Kosak, S.; Mouhieddine, M.; et al. Improved meal presentation increases food intake and decreases readmission rate in hospitalized patients. Clin. Nutr. 2016, 35, 1153–1158. [Google Scholar] [CrossRef]
- Collins, J.; Porter, J.; Truby, H.; Huggins, C.E. A foodservice approach to enhance energy intake of elderly subacute patients: A pilot study to assess impact on patient outcomes and cost. Age Ageing 2017, 46, 486–493. [Google Scholar] [CrossRef]
- Farrer, O.; Olsen, C.; Mousley, K.; Teo, E. Does presentation of smooth pureed meals improve patients consumption in an acute care setting: A pilot study. Nutr. Diet. 2015, 73, 405–409. [Google Scholar] [CrossRef]
- Porter, J.; Haines, T.P.; Truby, H. The efficacy of Protected Mealtimes in hospitalised patients: A stepped wedge cluster randomised controlled trial. BMC Med. 2017, 15, 25. [Google Scholar] [CrossRef]
- Strotmann, C.; Friedrich, S.; Kreyenschmidt, J.; Teitscheid, P.; Ritter, G. Comparing Food Provided and Wasted before and after Implementing Measures against Food Waste in Three Healthcare Food Service Facilities. Sustainability 2017, 9, 1409. [Google Scholar] [CrossRef]
- Barrington, V.; Maunder, K.; Kelaart, A. Engaging the patient: Improving dietary intake and meal experience through bedside terminal meal ordering for oncology patients. J. Hum. Nutr. Diet. 2018, 31, 803–809. [Google Scholar] [CrossRef]
- McCray, S.; Maunder, K.; Krikowa, R.; MacKenzie-Shalders, K. Room Service Improves Nutritional Intake and Increases Patient Satisfaction while Decreasing Food Waste and Cost. J. Acad. Nutr. Diet. 2018, 118, 284–293. [Google Scholar] [CrossRef]
- McCray, S.; Maunder, K.; Barsha, L.; Mackenzie-Shalders, K. Room service in a public hospital improves nutritional intake and increases patient satisfaction while decreasing food waste and cost. J. Hum. Nutr. Diet. 2018, 31, 734–741. [Google Scholar] [CrossRef] [PubMed]
- Neaves, B.; Bell, J.J.; McCray, S. Impact of room service on nutritional intake, plate and production waste, meal quality and patient satisfaction and meal costs: A single site pre-post evaluation. Nutr. Diet. 2022, 79, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Razalli, N.H.; Cheah, C.F.; Mohammad, N.M.A.; Manaf, Z.A. Plate waste study among hospitalised patients receiving texture-modified diet. Nutr. Res. Pract. 2021, 15, 655–671. [Google Scholar] [CrossRef] [PubMed]
- Berardy, A.; Egan, B.; Birchfield, N.; Sabaté, J.; Lynch, H. Comparison of Plate Waste between Vegetarian and Meat-Containing Meals in a Hospital Setting: Environmental and Nutritional Considerations. Nutrients 2022, 14, 1174. [Google Scholar] [CrossRef]
- Kuperberg, K.; Caruso, A.; Dello, S.; Mager, D. How will a room service delivery system affect dietary intake, food costs, food waste and patient satisfaction in a paediatric hospital? A pilot study. J. Foodserv. 2008, 19, 255–261. [Google Scholar] [CrossRef]
- Bell, A.F.; Tapsell, L.C.; Walton, K.; Batterham, M. Unwrapping nutrition: Exploring the impact of hospital food and beverage packaging on plate waste/intake in older people. Appetite 2020, 144, 104–463. [Google Scholar] [CrossRef]
| Criteria | Definition |
|---|---|
| Participants | Hospitalised patients ≥ 18 years old |
| Intervention | Any hospital food delivering practices |
| Comparator | Any comparator |
| Outcomes | Plate waste (in % or in kg), total food waste, food intake (%), energy intake (% or in kcal), protein intake (% or in g) |
| Study design | Peer-reviewed original experimental studies |
| First Author, Year of Publication, Country | Study Design | Sample Size | Patient Type | Setting | Intervention Type | Time of Observation | Endpoints | Methods of Assessment | Results |
|---|---|---|---|---|---|---|---|---|---|
| Hartwell, 2003 UK [19] | Observational | n = 62 | Women’s Health (n= 42) and orthopaedic (n = 20) inpatients | Hospital wards (n = 2) | Bulk trolley system = patients choosing food and amount from the trolley vs. Plated meal system = meals are ordered in advance (24 h before consumption) | 3 consecutive days before and after 6 months. | Nutrient intake Food waste | Food weighed pre- and post-consumption Microdiet computer software for nutritional content | No differences between the nutrient content of the food intakes (both lower than recommended dietary values) ↓ plate waste with the bulk trolley service (5.9% vs. 11.6%) but high waste left on the trolley (20.5%) with bulk trolley system. |
| Edwards, 2006 UK [20] | Observational | n = 52 | Patients presenting a mixture of clinical conditions | NHS teaching Hospital | Steamplicity vs. Cook-chill food service | 3 consecutive days in 2-weeks periods for each arm | Food intake Food waste | Food weighed before and after the meal using digital weighing scales (individual food components separated when possible) | ↑ food intake in Steamplicity than cook-chill system (daily mean of 282 g vs. 202 g at lunch; 310 g vs. 226 g at dinner) ↓ food waste in Steamplicity system then in cook-chill service (33% vs. 49%) |
| Hickson, 2007 UK [21] | Observational | n = 57 | Patients presenting a mixture of clinical conditions; not at nutritional risk, without eating problems; and able to choose a menu | Hospital wards (n=7) | Steamplicity vs. Traditional bulk cook-chill system | 1 lunch meal/patient between March and April 2006 | Energy and protein requirements met with Steamplicity Energy and protein consumption between the two systems | Estimates of served food portion sizes Food waste weighed to calculate food intake and energy and protein intake (Nutritional analysis program) Comparison consumption and patient requirements | Steamplicity does not meet the patients’ energy requirements (36% deficit) ↓ energy intake in Steamplicity than in bulk cook-chill system (p = 0.04) No difference in protein intake between the two systems No difference in food wasted; more protein wasted in the Steamplicity system |
| Rufenacht, 2010 Germany [22] | RCT | n = 36 | Hospitalised patients with NRS-2002>3 | Internal Medicine hospital ward | NT: Nutritional counselling with a dietitian + ONS vs. ONS (without nutritional counselling) | 10–15 days | Energy intake Protein intake | Weighing of all meals before and after consumption Energy and protein intake calculated with nutritional software | NT group met the energy requirements by 107% and protein requirements by 94% ONS group met the energy requirements before discharge by 90% and protein requirements by 88% |
| Hickson, 2011 UK [23] | Observational | n = 253 | Hospitalised adult patients at high risk of malnutrition | Two large teaching hospitals | “Protected mealtimes” (PM) vs. Standard food service | June/July 2008: standard food service October/November 2009: PM | Nutritional (energy and protein) intake Food waste | Direct observation of meal consumption Weighing food consumed and food waste Evaluation of the intake by nutritional software | No impact of PM on energy intake (p = 0.25) ↓ protein intake (p = 0.04) in intervention group |
| Manning, 2012 Australia [24] | Monocentric observational | n = 23 | Elderly inpatients (almost all at risk of malnutrition) | Hospital 2 wards | Volunteer feeding assistance program vs. No volunteers (feeding provided by nurses) | 2 days for each arm | Energy and protein intake and % of energy and protein requirements met Food waste | Weighing of remaining food after meal consumption % of each item consumed Estimated energy and protein intake according to requirements | ↑ energy and protein intake at lunch (p = 0.005; p = 0.009) No difference in daily total energy intake (p = 0.113) ↑ total daily protein intake (p = 0.004) ↑ % of energy requirements met with volunteers (64% vs. 58%, with an additional 448 kJ) ↑ % of estimated protein requirements met with volunteers (71% vs. 59%, p = 0.003). |
| Young, 2012 Australia [25] | Prospective pre-post | n = 254 | Inpatients aged >65 years | Internal Medicine wards (n = 3) of a large metropilitan Hospital | 3 mealtime assistance interventions: PM AIN: A nutritional focused staff-member assisting patients with meals PM + AIN: combined intervention | 1 day in the first week of hospitalisation | Daily energy and protein intake | Visual estimation of plate waste (none, 1/8, 1/4, 1/2, 3/4, all) Intake evaluation by nutrient analysis software. | ↑ energy intake, no differences between intervention groups (p = 0.16) ↑ protein intake (p = 0.07), no differences between the three interventions (p = 0.20). ↑ adequate EER (p < 0.01), no difference between interventions (p = 0.29). ↑ adequate protein intake (intake > EPR) (p = 0.03); no difference between interventions (p = 0.57). |
| Maunder, 2015 Australia [26] | Prospective | n = 119 | Hospitalised adult patients | Private hospital | Bedside electronic meal ordering system (BMOS) vs. Paper menu (PM) group with default meals | 48 h period × 2 | Energy intake Protein intake | Use of photography and five-point visual wastage scale (0%, 25%, 50%, 75% and 100% wasted). Estimation of dietary intake by total meal eaten weight and calculated by nutritional analysis software analysis | In BMOS vs. PM group: ↑ energy intake: 8273 vs. 6273 kJ/day (p < 0.05) ↑ protein intake: 83 vs. 66 g/day (p < 0.05) |
| Navarro, 2016 Israel [27] | Prospective | n = 206 | Adult hospitalised patients | Hospital Internal medicine ward | Improved meal presentation vs. standard lunch | Mean 4.7 days (intervention group) Mean 5.25 days (control group) | Food intake Food waste | Digital Imaging Method and visual estimation of plate waste (6-point scale: 0%, 25%, 50%, 75%, 90%, 100%) Estimation of food intake by nutritionDay questionnaire | +19% of food intake in the intervention group compared with control group (p < 0.05) ↓ starch and main course waste in the intervention group compared with control group (p < 0.05) |
| Collins, 2016 Australia [28] | Parallel controlled pilot study | n = 124 | Elderly subacute patients (38% malnourished at admission) | Hospital, subacute geriatric ward | Modified hospital menu with higher energy foods including ONS (and a visual menu) vs. Control group: standard cook-chill meals (no visual menu) | 14 days/group | Nutritional (energy and protein) intake Food waste | Visual estimation of plate waste before and after meal consumption Calibrated seated scales or self-reported or medical notes (if unable to be measured) Daily energy (kJ) and protein (g) intake estimated from plate waste data by nutritional software | In intervention vs. control group: ↑ mean energy intake (132 vs. 105 kj/kg/day; p = 0.003) ↑ mean protein intake (1.4 vs. 1.1 g protein/kg/day; p = 0.035) |
| Farrer, 2016 Australia [29] | Prospective | n = 65 | Acute care inpatients prescribed smooth pureed meals | Acute care hospital | Smooth pureed meals in a moulded format (intervention group) vs. Smooth pureed meals in the standard format (control) | 2 weeks | Food intake Plate waste | Weighing meal wastage with calibrated electronic scales | ↑ food intake from <1/4 to >3/4 of the meal in the moulded form (p = 0.03) compared with control ↓ 120 g of plate waste in the intervention group compared with control group even if not significant (p = 0.09) |
| Porter, 2017 Australia [30] | RCT | n = 149 | Admitted to the subacute setting | 3 hospitals 3 wards n.2 geriatric evaluation and management wards and n.1 rehabilitation wards | PM (Intervention period) vs. Usual care (Control period) | 4 weeks | Daily energy intake Daily protein intake Daily energy deficit | One quarter portion method per day; per patient per meal period and per interruption Use of nutritional software to estimate energy and protein intake | No significant differences between the intervention and control conditions for unadjusted analysis. ↓ energy deficit in intervention periods vs control periods if adjusted for age, nutritional status and type of subacute ward. |
| Strotmann, 2017 Germany [31] | Case study | n = 367 | Hospitalised patients | Hospital surgery | A package of measures including: - Sensitisation of employees to food waste - Order assistance training - Analysis of the flow of communication along the supply chain - Configuration of a food catalogue with detailed description of meals - Change of order and delivery process - Change of portion sizes according to target group-specific standards and their needs vs. Usual care | 2 weeks | Daily food waste rate (per person) Total food waste rate | Weighing food before and after consumption using electronic scales | ↓ 20% in the average quantity of food served daily per person in hospital (p < 0.0001) No difference in hospital total waste; rate remained the same after implementing measure |
| Barrington, 2018 Australia [32] | Observational prospective | n = 96 (control) n = 105 (intervention) | Oncologic hospitalised patients | Hospital | BMOS vs. PM group with default meals | 2 weeks | Total food intake Energy intake Protein intake Food waste | Use of photography and five-point visual wastage scale (0%, 25%, 50%, 75% and 100% wasted). Estimation of dietary intake by total meal eaten weight and calculated by nutritional analysis software analysis | ↑ average energy intake (p < 0.001) in BMOS ↑ average protein intake (p < 0.001) in BMOS ↑ in receiving the food ordered (p < 0.001) in BMOS ↑ in choosing food that patients liked (p = 0.006) in BMOS No significant differences in average plate waste between the groups (34.3% in the BMOS vs. 35.3% in PM, p = 0.75) |
| McCray, 2018° Australia [33] | Retrospective analysis of data pre- and post-intervention | n = 148 | Case mix of patients (general medical, surgical, and oncology wards) | 2 adult care hospitals | Room service (RS) = meals ordered by patients from a “a la carte menu” and delivered within 45 min vs. Traditional foodservice model = meals ordered completing a paper menu (cook fresh, 14-day cycle) up to 24 h before meals | A 24-h consecutive period for 4 days | Nutritional intake Energy and protein intake as % of requirements Food waste | Meal intake observation tool using a five-point visual scale (0, 1/4, 1/2, 3/4, all) Nutrition analysis by nutritional software | In room service intervention vs. traditional foodservice model ↑ mean energy intake (1588 kcal/d vs. 1306 kcal/d; p < 0.005) ↑ mean protein intake (65.9 g/d vs. 52.3 g/d; p < 0.003) ↑ % of requirements of energy (75.1 vs. 63; p < 0.024) and protein (84.7 vs. 65; p < 0.011) intake ↓ total mean plate waste (12% vs. 29%; p < 0.001) |
| Mc Cray, 2018b Australia [34] | Prospective | n = 187 | Adult hospitalised patients | Acute care hospital | Food and Nutrition Solutions (FNS) and Room Service ChoiceTM vs. Traditional model (TM) with paper menu | 4 days | Energy intake Protein intake Plate waste | Meal intake observation tool using a five-point visual scale (0, 1/4, 1/2, 3/4, all) Calculation of the nutritional intake using the FNS software | Compared with TM group, in FNS group: ↑ energy intake: 6379 vs. 5513 kJ/day (p = 0.020) ↑ protein intake: 74 vs. 53 g/day (p < 0.001) ↑ % of energy requirements met: 78% vs. 64% (p = 0.002) ↑ % of protein requirements met: 99% vs. 70% (p < 0.001) ↓ total average plate waste 17% vs. 30% (p < 0.001) |
| Neaves, 2021 Australia [35] | Retrospective analysis | n = 210 | Adult hospitalised patients | Large tertiary hospital 3 wards: surgical, thoracic, cystic fibrosis | RS vs. Thaw-retherm service control group | 5 weekdays | Nutritional (energy and protein) intake % of energy and protein met Food waste | Visual tool for nutritional intake and plate waste five-point visual scale (0%, 25%, 50%, 75%, 100%) and weight estimation of % wasted food | In RS compared to control group ↑ average energy and protein intake (p < 0.001). ↓ plate waste (15% vs. 40%) and production waste (5.6% vs. 15%, p < 0.001) ↓ food waste (p < 0.01) ↓ total average production waste (p < 0.001) |
| Razalli, 2021 Malaysia [36] | Cross-sectional | n = 95 | Adult patients prescribed with texture-modified diet | Hospital | Texture modified diets 3 types: -Blended diet -Mixed porridge -Minced diet | from 1 to over 7 days | % plate waste % protein plate waste | Visual estimation of plate waste through Visual Comstock Scale (6-point scale: 0%, 25%, 50%, 75%, 90%, 100%) Digital food weighing scale | ↑ plate waste (65%) in blended diet (65%) than minced diet (56%) and mixed porridge (35%) (based on weighing method) ↑ protein waste (61.1%) in minced diet compared with other diets (based on weighing method) |
| Berardy, 2022 USA [37] | Prospective | n = 447 | Adult hospitalised patients | Hospital | Type of protein source vegetarian meals (peanut butter, tofu, black beans, brown lentils and hummus) vs. meat-containing meals | 7 days | Total food waste Food waste of categories of food | Weighing of containers removing container weight Use of recipes for composite foods to determine proportional weights for individual categories of food | ↑ 34.05 g of food waste (p = 0.05) in patients with meat-containing meals compared with vegetarian meals Largest category of food waste in meat-containing meals: vegetables. Largest category of food waste in vegetarian meals: grains and vegetables |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rinninella, E.; Raoul, P.; Maccauro, V.; Cintoni, M.; Cambieri, A.; Fiore, A.; Zega, M.; Gasbarrini, A.; Mele, M.C. Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review. Nutrients 2023, 15, 310. https://doi.org/10.3390/nu15020310
Rinninella E, Raoul P, Maccauro V, Cintoni M, Cambieri A, Fiore A, Zega M, Gasbarrini A, Mele MC. Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review. Nutrients. 2023; 15(2):310. https://doi.org/10.3390/nu15020310
Chicago/Turabian StyleRinninella, Emanuele, Pauline Raoul, Valeria Maccauro, Marco Cintoni, Andrea Cambieri, Alberto Fiore, Maurizio Zega, Antonio Gasbarrini, and Maria Cristina Mele. 2023. "Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review" Nutrients 15, no. 2: 310. https://doi.org/10.3390/nu15020310
APA StyleRinninella, E., Raoul, P., Maccauro, V., Cintoni, M., Cambieri, A., Fiore, A., Zega, M., Gasbarrini, A., & Mele, M. C. (2023). Hospital Services to Improve Nutritional Intake and Reduce Food Waste: A Systematic Review. Nutrients, 15(2), 310. https://doi.org/10.3390/nu15020310








