The True Price of External Health Effects from Food Consumption
Abstract
:1. Introduction
1.1. The Potential Impact of Externalities on Food Prices
1.2. Calculating Health Costs
1.2.1. Challenges in Determining Health Costs
1.2.2. Calculating Health Impacts
2. Materials and Methods
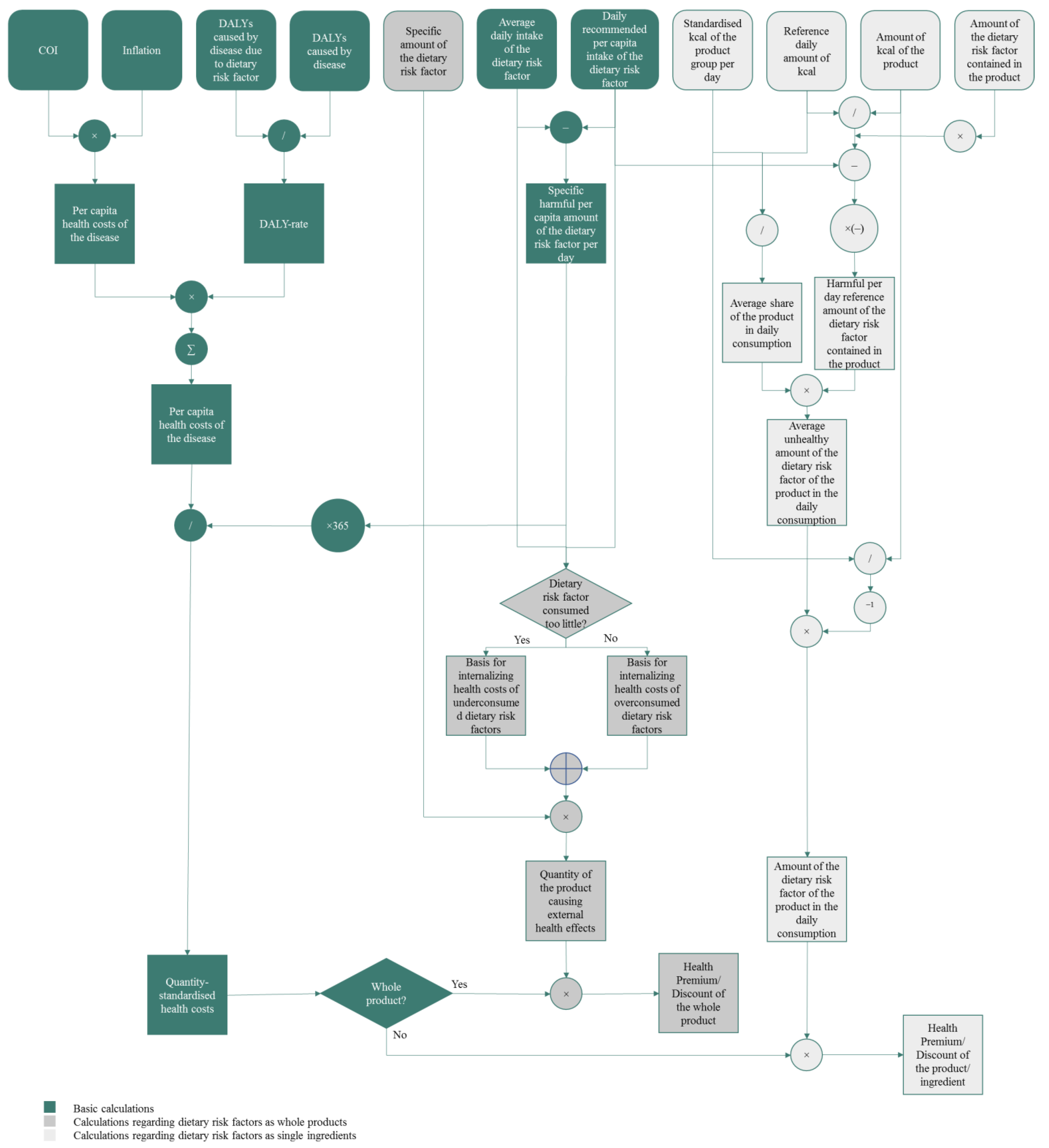
2.1. Method Outline
2.2. Method in Short
2.3. Input Data for Quantification and Monetisation
2.3.1. Input Data to Quantify the Burden of Diseases
2.3.2. Input Data to Monetise the Burden of Diseases
2.3.3. Input Data to Determine Harmful Daily Intakes
2.3.4. Input Data to Calculate Concrete Health Premiums for Products
3. Results
4. Discussion
4.1. Dealing with Uncertainties
4.2. Discussion of Results
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. What Is Climate Change? 2022. Available online: https://www.un.org/en/climatechange/what-is-climate-change (accessed on 18 July 2022).
- Bundesministerium für Wirtschaftliche Zusammenarbeit und Entwicklung. Agenda 2030. 2022. Available online: https://www.bmz.de/de/agenda-2030 (accessed on 18 July 2022).
- United Nations. THE 17 GOALS | Sustainable Development. 2022. Available online: https://sdgs.un.org/goals (accessed on 18 July 2022).
- UN Sustainable Development Group. UNSDG | The 5Ps of the SDGs: People, Planet, Prosperity, Peace and Partnership. 2022. Available online: https://unsdg.un.org/latest/videos/5ps-sdgs-people-planet-prosperity-peace-and-partnership (accessed on 18 July 2022).
- European Commission. Causes of Climate Change. 2022. Available online: https://ec.europa.eu/clima/climate-change/causes-climate-change_en (accessed on 18 July 2022).
- Nunez, C. Carbon Dioxide Levels Are at a Record High. Here’s What You Need to Know. National Geographic, 13 May 2019. Available online: https://www.nationalgeographic.com/environment/article/greenhouse-gases (accessed on 18 July 2022).
- Pieper, M.; Michalke, A.; Gaugler, T. Calculation of external climate costs for food highlights inadequate pricing of animal products. Nat. Commun. 2020, 11, 6117. [Google Scholar] [CrossRef] [PubMed]
- Pretty, J.; Brett, C.; Gee, D.; Hine, R.; Mason, C.; Morison, J.; Rayment, M.; Van Der Bijl, G.; Dobbs, T. Policy Challenges and Priorities for Internalizing the Externalities of Modern Agriculture. J. Environ. Plan. Manag. 2001, 44, 263–283. [Google Scholar] [CrossRef]
- Michalke, A.; Köhler, S.; Messmann, L.; Thorenz, A.; Tuma, A.; Gaugler, T. True cost accounting of organic and conventional food production. J. Clean. Prod. 2023, 408, 137134. [Google Scholar] [CrossRef]
- Hendriks, S.; de Groot Ruiz, A.; Acosta, M.H.; Baumers, H.; Galgani, P.; Mason-D’Croz, D.; Godde, C.; Waha, K.; Kanidou, D.; von Braun, J.; et al. The True Cost and True Price of Food; The Scientific Group of the U.N. Food Systems Summit: New York, NY, USA, 2021. [Google Scholar]
- Costa, N.; Derumeaux, H.; Rapp, T.; Garnault, V.; Ferlicoq, L.; Gillette, S.; Andrieu, S.; Vellas, B.; Lamure, M.; Grand, A.; et al. Methodological considerations in cost of illness studies on Alzheimer disease. Health Econ. Rev. 2012, 2, 18. [Google Scholar] [CrossRef]
- Byford, S.; Torgerson, D.J.; Raftery, J. Economic Note: Cost of illness studies. BMJ 2000, 320, 1335. [Google Scholar] [CrossRef] [PubMed]
- Koopmanschap, M.A. Cost-of-Illness Studies. Useful for Health Policy? Pharmacoeconomics 1998, 14, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Cost of Illness | POLARIS | Policy and Strategy | CDC. 2022. Available online: https://www.cdc.gov/policy/polaris/economics/cost-illness/index.html (accessed on 18 July 2022).
- Gemmill-Herren, B.; Baker, L.E.; Daniels, P.A. True Cost Accounting for Food; Series: Routledge Studies in Food, Society and the Environment; Routledge: New York, NY, USA, 2021. [Google Scholar]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492 . [Google Scholar] [CrossRef]
- Maschkowski, G. Planetary Health Diet—Herausforderung und Chance für eine nachhaltige Transformation unseres Ernährungssystems. 2020, 1, 14–21. Available online: https://www.researchgate.net/publication/340061442_Planetary_Health_Diet_-_Herausforderung_und_Chance_fur_eine_nachhaltige_Transformation_unseres_Ernahrungssystems (accessed on 27 July 2022).
- Perotti, A. Moving Towards a Sustainable Swiss Food System: An Estimation of the True Cost of Food in Switzerland and Implications for Stakeholders. Master’s Thesis, ETH Zurich, Zürich, Switzerland, 2020. [Google Scholar]
- Michalke, A.; Stein, L.; Fichtner, R.; Gaugler, T.; Stoll-Kleemann, S. True cost accounting in agri-food networks: A German case study on informational campaigning and responsible implementation. Sustain. Sci. 2022, 17, 2269–2285. [Google Scholar] [CrossRef]
- de Sadeleer, N. (Ed.) The Polluter-Pays Principle. In Environmental Principles. From Political Slogans to Legal Rules, 2nd ed.; Oxford University Press: Oxford, UK, 2020; pp. 31–84. Available online: https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=OCDE/GD(92)81&docLanguage=En (accessed on 18 July 2022).
- Hentschl, M.; Michalke, A.; Pieper, M.; Gaugler, T.; Stoll-Kleemann, S. Dietary change and land use change: Assessing preventable climate and biodiversity damage due to meat consumption in Germany. Sustain. Sci. 2023. [Google Scholar] [CrossRef]
- Wilkins, E.; Wilson, L.; Wickramasinghe, K.; Bhatnagar, P.; Leal, J.; Luengo-Fernandez, R.; Burns, R.; Rayner, M.; Townsend, N. European Cardiovascular Disease Statistics 2017; European Heart Network: Brussels, Belgium, 2007. [Google Scholar]
- Köster, I.; Huppertz, E.; Hauner, H.; Schubert, I. Costs of Diabetes Mellitus (CoDiM) in Germany, direct per-capita costs of managing hyperglycaemia and diabetes complications in 2010 compared to 2001. Exp. Clin. Endocrinol. Diabetes 2014, 122, 510–551. [Google Scholar] [CrossRef]
- Müller, N.; Heller, T.; Freitag, M.H.; Gerste, B.; Haupt, C.M.; Wolf, G.; Müller, U.A. Healthcare utilization of people with Type 2 diabetes in Germany: An analysis based on health insurance data. Diabet. Med. 2015, 32, 951–957. [Google Scholar] [CrossRef]
- Ulrich, S.; Holle, R.; Wacker, M.; Stark, R.; Icks, A.; Thorand, B.; Peters, A.; Laxy, M. Cost burden of type 2 diabetes in Germany: Results from the population-based KORA studies. BMJ Open 2016, 6, e012527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, E.; Hoyer, A.; Brinks, R.; Icks, A.; Kuß, O.; Rathmann, W. Healthcare costs of Type 2 diabetes in Germany. Diabet. Med. 2017, 34, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Stegbauer, C.; Falivena, C.; Moreno, A.; Hentschel, A.; Rosenmöller, M.; Heise, T.; Szecsenyi, J.; Schliess, F. Costs and its drivers for diabetes mellitus type 2 patients in France and Germany: A systematic review of economic studies. BMC Health Serv. Res. 2020, 20, 1043. [Google Scholar] [CrossRef] [PubMed]
- Hofmarcher, T.; Lindgren, P.; Wilking, N.; Jönsson, B. The cost of cancer in Europe 2018. Eur. J. Cancer 2020, 129, 41–49. [Google Scholar] [CrossRef] [Green Version]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Institute for Health Metrics and Evaluation. GBD Compare | IHME Viz Hub. University of Washington. 2022. Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 18 July 2022).
- Springmann, M. Valuation of the Health and Climate-Change Benefits of Healthy Diets; FAO: Rome, Italy, 2020. [Google Scholar]
- Springmann, M.; Mason-D’croz, D.; Robinson, S.; Wiebe, K.; Godfray, H.C.J.; Rayner, M.; Scarborough, P. Health-motivated taxes on red and processed meat: A modelling study on optimal tax levels and associated health impacts. PLoS ONE 2018, 13, e0204139. [Google Scholar] [CrossRef] [Green Version]
- Devleesschauwer, B.; Havelaar, A.H.; de Noordhout, C.M.; Haagsma, J.A.; Praet, N.; Dorny, P.; Duchateau, L.; Torgerson, P.R.; Van Oyen, H.; Speybroeck, N. Calculating disability-adjusted life years to quantify burden of disease. Int. J. Public Health 2014, 59, 565–569. [Google Scholar] [CrossRef] [PubMed]
- Gerald, J.; Dorothy, R. Friedman School of Nutrition Science and Policy. Dietary Data by Country | Global Dietary Database. Tufts University. 2019. Available online: https://www.globaldietarydatabase.org/our-data/data-visualizations/dietary-data-country (accessed on 18 July 2022).
- Statistisches Bundesamt. Bevölkerung: Deutschland, Stichtag, Geschlecht. GENESIS-Online: Ergebnis 12411-0003. 2022. Available online: https://gdk.gdi-de.org/geonetwork/srv/api/records/30303031-3234-4031-312d-303030330002 (accessed on 22 July 2022).
- Finanzen.net: Inflationsrechner. 2022. Available online: https://www.finanzen.net/konjunktur/inflationsrechner (accessed on 18 July 2022).
- Statistisches Bundesamt. Statistisches Bundesamt Deutschland—GENESIS-Online: Ergebnis 61111-0001. 2022. Available online: https://www-genesis.destatis.de/genesis/online?operation=previous&levelindex=1&step=1&titel=Ergebnis&levelid=1658413531419&acceptscookies=false#abreadcrumb (accessed on 21 July 2022).
- Countrymeters.info. Deutschland Bevölkerung 2022 | Bevölkerungsuhr. 2022. Available online: https://countrymeters.info/de/Germany (accessed on 18 July 2022).
- Statistisches Bundesamt. Konsumausgaben der Privaten Haushalte in Deutschland für Nahrungsmittel in den Jahren 1991 bis 2021 (in Milliarden Euro), Quoted According to de.statista.com. 2022. Available online: https://de.statista.com/statistik/daten/studie/296815/umfrage/konsumausgaben-in-deutschland-fuer-nahrungsmittel (accessed on 22 July 2022).
- Robert Koch-Institut. Natriumzufuhr in Deutschland; Robert Koch-Institut: Berlin, Germany, 2016. [Google Scholar]
- European Commission. Whole Grain Intake across European Countries | Knowledge for Policy. 2021. Available online: https://knowledge4policy.ec.europa.eu/health-promotion-knowledge-gateway/whole-grain-5_en (accessed on 18 July 2022).
- Strohm, D.; Boeing, H.; Leschik-Bonnet, E.; Heseker, H.; Arens-Azevêdo, U.; Bechthold, A.; Knorpp, L.; Kroke, A. Salt intake in Germany, health consequences, and resulting recommendations for action. A scientific statement from the German Nutrition Society (DGE). Ernahr. Umsch. 2016, 63, 62–70. [Google Scholar]
- Institute for Health Metrics and Evaluation. Terms Defined. 2022. Available online: https://www.healthdata.org/terms-defined (accessed on 20 July 2022).
- Marktguru. Äpfel im Angebot bei EDEKA—Juli 2022—Marktguru.de. 2022. Available online: https://www.marktguru.de/rc/edeka/aepfel (accessed on 26 July 2022).
- SupermarktCheck. Gut & Günstig Gemischtes Hackfleisch zum Braten: Preis, Angebote & Bewertungen. 2022. Available online: https://www.supermarktcheck.de/product/20113-gut-guenstig-gemischtes-hackfleisch- (accessed on 26 July 2022).
- kaufDA. Prospekte und Angebote in Deiner Nähe Online auf kaufDA.de. 2022. Available online: https://www.kaufda.de/webapp/viewer/1708349308?lat=48.266&lng=10.892&publisher=&page=4&adFormat=ad_format__brochure_box_page&adPlacement=ad_placement__seo_brochure_box&pageType=google.analytics.PORTAL.RETAILER_PRODUCT_PAGE.withExactBrochure&retailerName=EDEKA&zip=86343&sourceType=PORTAL_RETAILER_PRODUCT_LANDING&sourceValue=Hackfleisch&visitOriginType=WEB_REFERRER_SEO (accessed on 26 July 2022).
- SupermarktCheck. Gut & Günstig Salami Hauchfein: Preis, Angebote, Kalorien & Nutri-Score. 2022. Available online: https://www.supermarktcheck.de/product/85333-gut-guenstig-salami-hauchfein (accessed on 26 July 2022).
- SupermarktCheck. Edeka Bio Delikatess Salami: Preis, Angebote, Kalorien & Nutri-Score. 2022. Available online: https://www.supermarktcheck.de/product/83255-edeka-bio-delikatess-salami (accessed on 26 July 2022).
- SupermarktCheck. Aerzener Das Pure: Preis, Angebote, Kalorien & Nutri-Score. 2022. Available online: https://www.supermarktcheck.de/product/225078-aerzener-das-pure (accessed on 25 July 2022).
- SupermarktCheck. Preis & Kalorien für Hülsenfrüchte getrocknet | SupermarktCheck. 2022. Available online: https://www.supermarktcheck.de/huelsenfruechte-getrocknet/produkte/ (accessed on 21 July 2022).
- SupermarktCheck. Hochland Sandwich Scheiben Bauernhof Gouda in Scheiben: Preis, Angebote, Kalorien & Nutri-Score. 2022. Available online: https://www.supermarktcheck.de/product/80891-hochland-sandwich-scheiben-bauernhof-gouda (accessed on 23 October 2022).
- SupermarktCheck. San Fabio Mozzarella: Preis, Angebote, Kalorien & Nutri-Score. 2022. Available online: https://www.supermarktcheck.de/product/196317-san-fabio-mozzarella (accessed on 20 July 2022).
- Bundesministerium für Ernährung und Landwirtschaft. BMEL-Statistik: Milch und Milcherzeugnisse. 2022. Available online: https://www.bmel-statistik.de/ernaehrung-fischerei/versorgungsbilanzen/milch-und-milcherzeugnisse (accessed on 18 July 2022).
- Deutscher Fleischer-Verband. Pro-Kopf-Konsum von Fleisch- und Wurstwaren in Deutschland nach Art in den Jahren 2019 und 2020 (in Kilogramm), Quoted According to de.statista.com. Available online: https://de.statista.com/statistik/daten/studie/163791/umfrage/pro-kopf-konsum-von-wurstwaren-und-sonstigen-fleischerzeugnissen-in-deutschland/ (accessed on 18 July 2022).
- Michalke, A.; Fitzer, F.; Pieper, M.; Kohlschütter, N.; Gaugler, T. How Much Is the Dish?–Was Kosten uns Lebensmittel Wirklich? 2019. Available online: https://opus.bibliothek.uni-augsburg.de/opus4/files/86213/michalke_86213.pdf (accessed on 26 July 2022).
- Smith-Spangler, C.; Brandeau, M.L.; Hunter, G.E.; Bavinger, J.C.; Pearson, M.; Eschbach, P.J.; Sundaram, V.; Liu, H.; Schirmer, P.; Stave, C.; et al. Are Organic Foods Safer or Healthier Than Conventional Alternatives? A systematic review. Ann. Intern. Med. 2012, 157, 348–366. [Google Scholar] [CrossRef] [Green Version]
- Slavin, J.L. Dietary fiber and body weight. Nutrition 2005, 21, 411–418. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA); Turck, D.; Castenmiller, J.; De Henauw, S.; Hirsch-Ernst, K.-I.; Kearney, J.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; et al. Dietary reference values for sodium. EFSA J. 2019, 17, e05778. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025.; 2020. Available online: DietaryGuidelines.gov (accessed on 18 July 2022).
- World Health Organization. Salt reduction. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 19 July 2022).
- Mente, A.; O’donnell, M.; Yusuf, S. Sodium Intake and Health: What Should We Recommend Based on the Current Evidence? Nutrients 2021, 13, 3232. [Google Scholar] [CrossRef] [PubMed]
- Federal Statistical Office. Global Animal Farming, Meat Production and Meat Consumption. 2022. Available online: https://www.destatis.de/EN/Themes/Countries-Regions/International-Statistics/Data-Topic/AgricultureForestryFisheries/livestock_meat.html (accessed on 23 August 2022).
- Institute for Health Metrics and Evaluation. Socio-Demographic Index (SDI). 2022. Available online: https://www.healthdata.org/taxonomy/glossary/socio-demographic-index-sdi (accessed on 23 August 2022).
- Stein, A.D.; Obrutu, O.E.; Behere, R.V.; Yajnik, C.S. Developmental undernutrition, offspring obesity and type 2 diabetes. Diabetologia 2019, 62, 1773–1778. [Google Scholar] [CrossRef] [Green Version]
- Sanders, L.M.; Wilcox, M.L.; Maki, K.C. Red meat consumption and risk factors for type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 2022, 77, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Kurth, T.; Rubel, H.; zum Felde, A.M.; Krüger, J.-A.; Zielcke, S.; Günther, M.; Kemmerling, B. Die Zukunft der deutschen Landwirtschaft nachhaltig sichern-Denkanstöße und Szenarien für Ökologische, Ökonomische und Soziale Nachhaltigkeit; Boston Consulting Group: Berlin, Germany, 2019. [Google Scholar]
- Gossard, M.H.; York, R. Social structural influences on meat consumption. Hum. Ecol. Rev. 2003, 10, 1–9. [Google Scholar]
- Koch, F.; Heuer, T.; Krems, C.; Claupein, E. Meat consumers and non-meat consumers in Germany: A characterisation based on results of the German National Nutrition Survey II. J. Nutr. Sci. 2019, 8, e21. [Google Scholar] [CrossRef] [Green Version]
- Smil, V. Eating Meat: Evolution, Patterns, and Consequences. Popul. Dev. Rev. 2002, 28, 599–639. [Google Scholar] [CrossRef]
- Leroy, F.; Praet, I. Meat traditions. The co-evolution of humans and meat. Appetite 2015, 90, 200–211. [Google Scholar] [CrossRef]







| Diseases | ||||
|---|---|---|---|---|
| Dietary Risk Factor Diets… | CVD | T2DM | Neoplasms | |
| …high in red Meat | DALYs DALY rate | 261,516.67 0.051 | 120,508.68 0.117 | 70,241.83 0.013 |
| …high in processed Meat | DALYs DALY rate | 158,826.85 0.031 | 163,747.32 0.159 | 43,881.09 0.008 |
| …low in whole Grains | DALYs DALY rate | 394,528.87 0.077 | 49,234.42 0.048 | 99,494.97 0.019 |
| …low in Legumes | DALYs DALY rate | 397,559.75 0.077 | - - | - - |
| …low in Fruits | DALYs DALY rate | 149,354.58 0.029 | 47,852.02 0.046 | 55,993.24 0.011 |
| …high in Sodium | DALYs DALY rate | 226,479.22 0.044 | - - | 15,593.78 0.003 |
| Total (not only because of the Diet) | DALYs DALY rate | 5,129,871.3 1 | 1,032,452.88 1 | 5,316,908.62 1 |
| CVD | |
|---|---|
| Direct (2015) | |
| Primary Care | 3,215,531,000.00 € |
| Outpatient Care | 4,730,257,000.00 € |
| A&E | 115,223,000.00 € |
| Inpatient Care | 14,965,129,000.00 € |
| Medications | 5,279,912,000.00 € |
| Cdir,CVD,2015 | 28,306,052,000.00 € |
| Indirect (2015) | |
| Prod. Loss from prem. Mort. | 8,556,221,000.00 € |
| Prod. Loss from Morbidity | 8,495,837,000.00 € |
| Informal Care | 12,149,160,000.00 € |
| Cind,CVD,2015 | 29,201,218,000.00 € |
| Total | |
| CCVD,2015 | 57,507,270,000.00 € |
| y1 | 2015 |
| p2015 | 82,175,684.00 |
| CPI2022/ CPI2015 | 1.13 |
| CCVD,cap,2015 | 699.81 € |
| CCVD,cap,2022 | 790.78 € |
| T2DM | |
|---|---|
| Direct (2010) | |
| Hospitals/ Inpatient Treatment | 1,986.00 € |
| Pharmacies/ Medication | 1,285.00 € |
| Physicians/ Outpatient care | 786.00 € |
| Dentists | 155.00 € |
| Sick Benefits | 149.00 € |
| Other | 785.00 € |
| cdir,T2DM,cap,2010 | 5,146.00 € |
| Cdir,T2DM,2010 | 16,100,000,000.00 € |
| Indirect (2011) | |
| cind,T2DM,cap,2011 | 4,103.00 € |
| CPI2010/ CPI2011 | 0.98 |
| Indirect (2010) | |
| cind,T2DM,cap,2011 | 4,016.80 € |
| Cind,T2DM,2010 | 12,567,143,526.67 € |
| Total | |
| CT2DM,2010 | 28,667,143,526.67 € |
| y1 | 2010 |
| p2010 | 81,715,602.00 |
| CPI2022/ CPI2010 | 1.22 |
| CT2DM,cap,2010 | 350.66 € |
| CT2DM,cap,2022 | 427.81 € |
| Neoplasms | |
|---|---|
| Direct (2018) | |
| Health Expenditure on Care | 25,537,000,000.00 € |
| Cdir,neoplasms,2018 | 25,537,000,000.00 € |
| Indirect (2018) | |
| Informal Care | 5,141,000,000.00 € |
| Prod. Loss from prem. Mort. | 11,516,000,000.00 € |
| Prod. Loss from Morbidity | 4,370,000,000.00 € |
| Cind,neoplasms,2018 | 21,027,000,000.00 € |
| Total | |
| Cneoplasms,2018 | 46,564,000,000.00 € |
| y1 | 2018 |
| p2018 | 83,019,213.00 |
| CPI2022/ CPI2018 | 1.10 |
| Cneoplasms,cap,2018 | 560.88 € |
| Cneoplasms,cap,2022 | 616.97 € |
| Population: Germany, Reference Date, Sex | |||
|---|---|---|---|
| Reference Date | Sex | ||
| Male | Female | Total | |
| 31 December 2021 | 41,066,785.00 | 42,170,339.00 | 83,237,124.00 |
| 49.34% | 50.66% | 100.00% | |
| 1 January 2022 | 83,756,658.00 | ||
| Dietary Risk Factors | ||||||
|---|---|---|---|---|---|---|
| Diets High in… | Diets Low in… | |||||
| …Red Meat | …Processed Meat | …Sodium | …Whole Grains | …Legumes | …Fruits | |
| Ir,cap [g] | 69.10 | 35.53 | 4.10 | 130.03 | 10.20 | 169.60 |
| Irecr,cap [g] | 14.00 | 2.00 | 2.30 | 232.00 | 75.00 | 200.00 |
| xr,cap [g] | 55.10 | 33.53 | 1.80 | –101.97 | –64.80 | –30.40 |
| i (hr/lr) | 0.80 | 0.94 | - | 0.44 | 0.86 | 0.15 |
| Dietary Risk Factors | ||||||
|---|---|---|---|---|---|---|
| Diets High in… | Diets Low in… | |||||
| …Red Meat | …Processed Meat | …Sodium | …Whole Grains | …Legumes | …Fruits | |
| xr,cap 1 [g] | 55.1000 | 33.5300 | 1.8000 | –101.9700 | –64.8000 | –30.4000 |
| HCr,cap,2022 2 [€] | 98.3983 | 97.4259 | 36.7219 | 92.7638 | 61.2849 | 49.3488 |
| HHCr,2022 3 [€/g] | 0.0049 | 0.0080 | 0.0559 | –0.0025 | –0.0026 | –0.0044 |
| Dietary Risk Factors | |||||
|---|---|---|---|---|---|
| Diets High in… | Diets Low in… | ||||
| …Red Meat | …Processed Meat | …Whole Grains | …Legumes | …Fruits | |
| HHCr,2022 1 [€/g] | 0.0049 | 0.0080 | –0.0025 | –0.0026 | –0.0044 |
| i (hr/lr) 2 | 0.7974 | 0.9437 | 0.4395 | 0.8640 | 0.1520 |
| mr 3 [g] | 1000.0000 | 1000.0000 | 1000.0000 | 1000.0000 | 1000.0000 |
| mr,i 4 [g] | 797.3951 | 943.7095 | 439.5259 | 864.0000 | 152.0000 |
| HPr 5 [€] | 3.9014 | 7.5125 | –1.0955 | –2.2387 | –0.6760 |
| Product | ||||
|---|---|---|---|---|
| Edeka | Penny-Market | |||
| Organic Salami (100 g) | Conventional Salami (100 g) | Hochland Gouda (150 g) | San Fabio Mozzarella (220 g) | |
| ap,cal 1 [kcal] | 373.00 | 344.00 | 510.00 | 547.80 |
| qcal 2 | 6.70 | 7.27 | 4.90 | 4.56 |
| mr,p 3 [g] | 1.80 | 1.60 | 0.90 | 0.53 |
| mr,day 4 [g] | 12.06 | 11.63 | 4.41 | 2.41 |
| Hmr,day 5 [g] | 9.76 | 9.33 | 2.11 | 0.11 |
| apg,cal,day 6 [kcal] | 268.76 | 247.87 | 235.67 | 172.59 |
| qp,day 7 | 0.11 | 0.10 | 0.09 | 0.07 |
| nr,day 8 [g] | 1.05 | 0.92 | 0.20 | 0.01 |
| nr,p 9 [g] | 1.46 | 1.28 | 0.43 | 0.02 |
| HPp 10 | 0.0814 € | 0.0717 € | 0.0241 € | 0.0013 € |
| HPp for 1000 g | 0.81 € | 0.72 € | 0.16 € | 0.01 € |
| Current Price | 1.69 € | 1.24 € | 2.29 € | 0.59 € |
| New Price | 1.77 € | 1.31 € | 2.31 € | 0.59 € |
| Price Increase | 4.82% | 5.79% | 1.05% | 0.23% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seidel, F.; Oebel, B.; Stein, L.; Michalke, A.; Gaugler, T. The True Price of External Health Effects from Food Consumption. Nutrients 2023, 15, 3386. https://doi.org/10.3390/nu15153386
Seidel F, Oebel B, Stein L, Michalke A, Gaugler T. The True Price of External Health Effects from Food Consumption. Nutrients. 2023; 15(15):3386. https://doi.org/10.3390/nu15153386
Chicago/Turabian StyleSeidel, Felix, Benjamin Oebel, Lennart Stein, Amelie Michalke, and Tobias Gaugler. 2023. "The True Price of External Health Effects from Food Consumption" Nutrients 15, no. 15: 3386. https://doi.org/10.3390/nu15153386
APA StyleSeidel, F., Oebel, B., Stein, L., Michalke, A., & Gaugler, T. (2023). The True Price of External Health Effects from Food Consumption. Nutrients, 15(15), 3386. https://doi.org/10.3390/nu15153386








