Can the Substitution of Milk with Plant-Based Drinks Affect Health-Related Markers? A Systematic Review of Human Intervention Studies in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Study Selection
2.3. Data Extraction and Presentation
3. Results
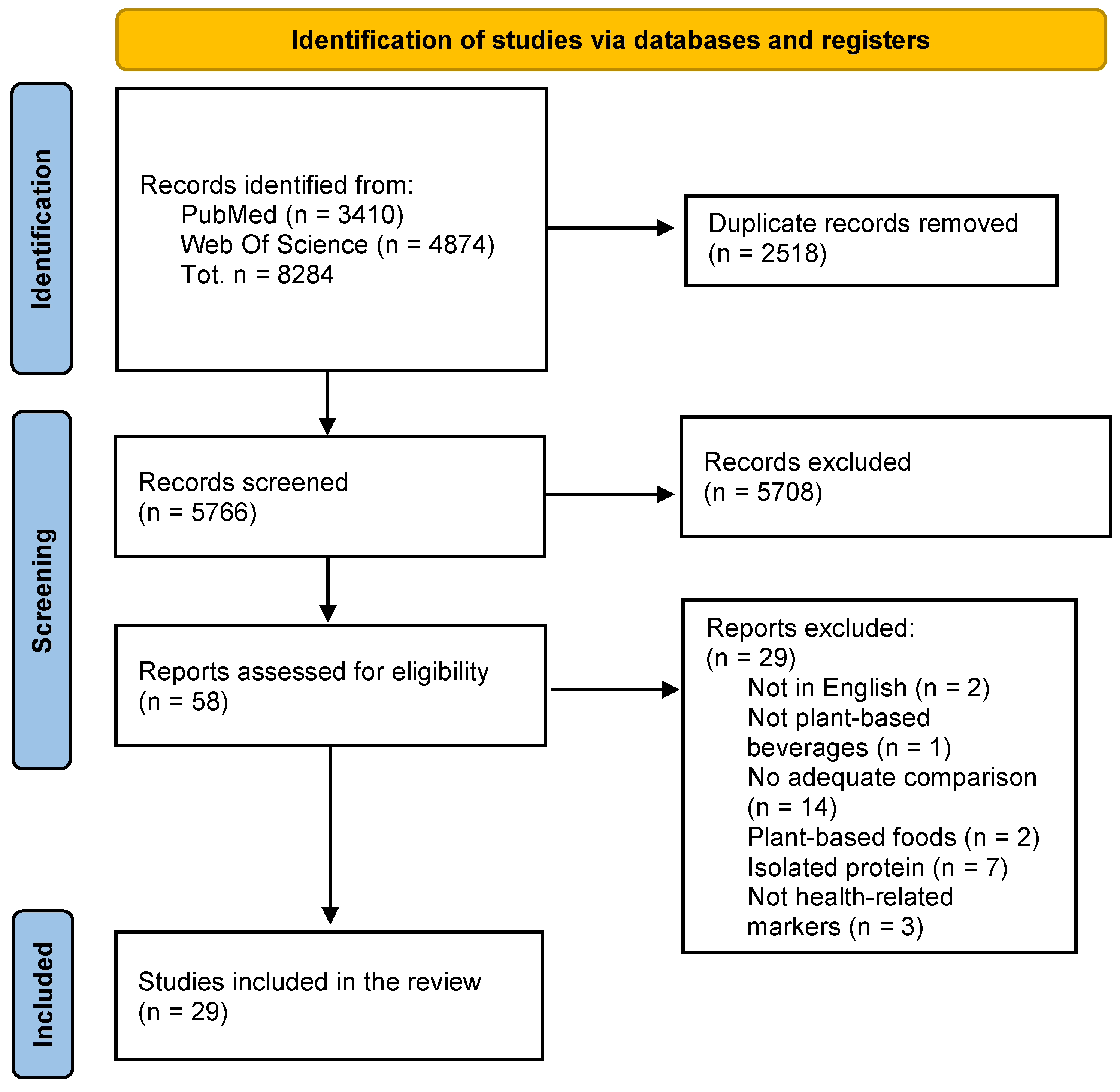
3.1. Study Selection
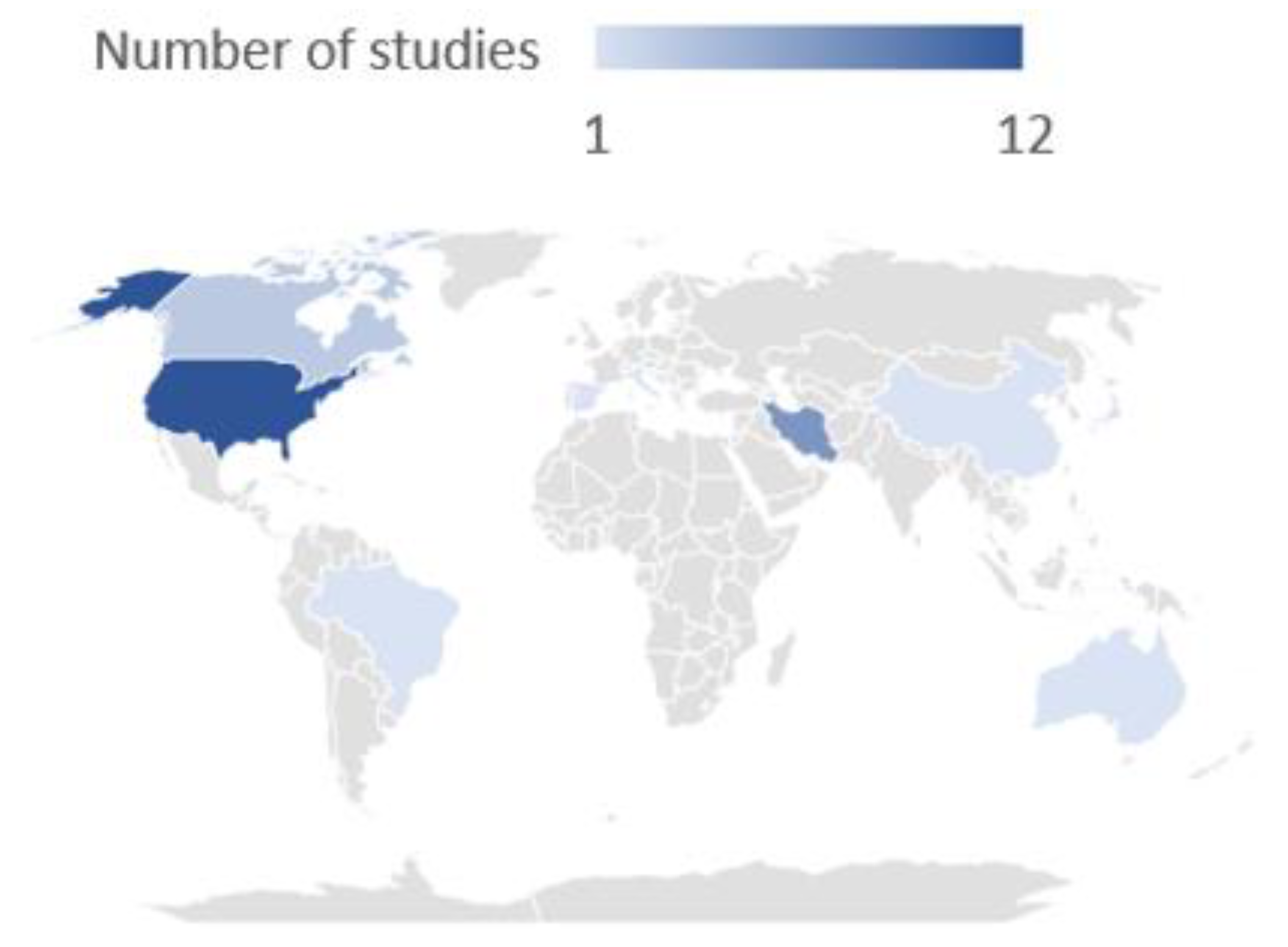
3.1.1. Study Design and Interventions
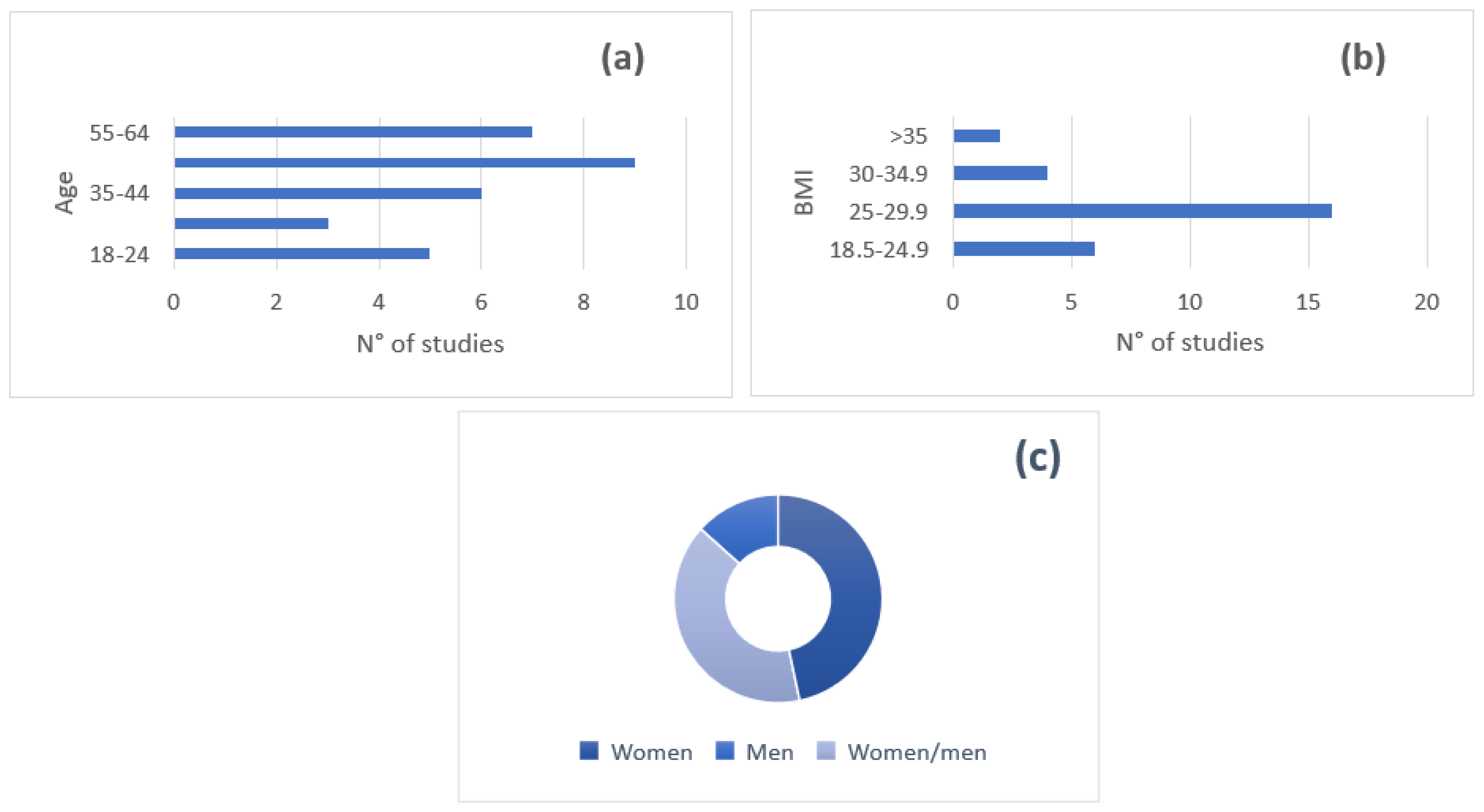
3.1.2. Subject Characteristics
3.2. Main Findings Derived from Comparisons between SD and CM
3.2.1. Comparison between SD and CM Effects on Markers of Bone Health
3.2.2. Comparison between SD and CM Effects on Anthropometric Parameters
3.2.3. Comparison between SD and CM Effects on Markers of Inflammation and Oxidative Stress
3.2.4. Comparison between SD and CM Effects on Lipid Profile
3.2.5. Comparison between SD and CM Effects on Blood Pressure
3.2.6. Comparison between SD and CM Effects on Glucose and Insulin Levels
3.2.7. Comparison between SD and CM Effects on Other Health-Related Parameters
3.3. Main Findings Derived from Comparisons between RD and CM
3.4. Main Findings Derived from the Comparison between AD and CM
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Comerford, K.B.; Miller, G.D.; Boileau, A.C.; Masiello Schuette, S.N.; Giddens, J.C.; Brown, K.A. Global Review of Dairy Recommendations in Food-Based Dietary Guidelines. Front. Nutr. 2021, 8, 671999. [Google Scholar] [CrossRef] [PubMed]
- Food Consumption Statistics for FoodEx2: Level 3. Available online: https://www.efsa.europa.eu/en/microstrategy/foodex2-level-3 (accessed on 1 March 2023).
- Silva, A.R.A.; Silva, M.M.N.; Ribeiro, B.D. Health Issues and Technological Aspects of Plant-Based Alternative Milk. Food Res. Int. 2020, 131, 108972. [Google Scholar] [CrossRef]
- Haas, R.; Schnepps, A.; Pichler, A.; Meixner, O. Cow Milk versus Plant-Based Milk Substitutes: A Comparison of Product Image and Motivational Structure of Consumption. Sustainability 2019, 11, 5046. [Google Scholar] [CrossRef]
- Boukid, F.; Lamri, M.; Dar, B.N.; Garron, M.; Castellari, M. Vegan Alternatives to Processed Cheese and Yogurt Launched in the European Market during 2020: A Nutritional Challenge? Foods 2021, 10, 2782. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Tyagi, S.K.; Anurag, R.K. Plant-Based Milk Alternatives an Emerging Segment of Functional Beverages: A Review. J. Food Sci. Technol. 2016, 53, 3408–3423. [Google Scholar] [CrossRef]
- Fructuoso, I.; Romão, B.; Han, H.; Raposo, A.; Ariza-Montes, A.; Araya-Castillo, L.; Zandonadi, R.P. An Overview on Nutritional Aspects of Plant-Based Beverages Used as Substitutes for Cow’s Milk. Nutrients 2021, 13, 2650. [Google Scholar] [CrossRef]
- Munekata, P.E.S.; Domínguez, R.; Budaraju, S.; Roselló-Soto, E.; Barba, F.J.; Mallikarjunan, K.; Roohinejad, S.; Lorenzo, J.M. Effect of Innovative Food Processing Technologies on the Physicochemical and Nutritional Properties and Quality of Non-Dairy Plant-Based Beverages. Foods 2020, 9, 288. [Google Scholar] [CrossRef]
- Aydar, E.F.; Tutuncu, S.; Ozcelik, B. Plant-Based Milk Substitutes: Bioactive Compounds, Conventional and Novel Processes, Bioavailability Studies, and Health Effects. J. Funct. Foods 2020, 70, 103975. [Google Scholar] [CrossRef]
- Drewnowski, A. Perspective: Identifying Ultra-Processed Plant-Based Milk Alternatives in the USDA Branded Food Products Database. Adv. Nutr. 2021, 12, 2068–2075. [Google Scholar] [CrossRef]
- Drewnowski, A. Most Plant-Based Milk Alternatives in the USDA Branded Food Products Database Do Not Meet Proposed Nutrient Standards or Score Well on Nutrient Density Metrics. Nutrients 2022, 14, 4767. [Google Scholar] [CrossRef]
- Walther, B.; Guggisberg, D.; Badertscher, R.; Egger, L.; Portmann, R.; Dubois, S.; Haldimann, M.; Kopf-Bolanz, K.; Rhyn, P.; Zoller, O.; et al. Comparison of Nutritional Composition between Plant-Based Drinks and Cow’s Milk. Front. Nutr. 2022, 9, 988707. [Google Scholar] [CrossRef]
- Glover, A.; Hayes, H.E.; Ni, H.; Raikos, V. A Comparison of the Nutritional Content and Price between Dairy and Non-Dairy Milks and Cheeses in UK Supermarkets: A Cross Sectional Analysis. Nutr. Health 2022. Epub ahead of print. [Google Scholar] [CrossRef]
- Singhal, S.; Baker, R.D.; Baker, S.S. A Comparison of the Nutritional Value of Cow’s Milk and Nondairy Beverages. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 799–805. [Google Scholar] [CrossRef]
- Smith, N.W.; Dave, A.C.; Hill, J.P.; McNabb, W.C. Nutritional Assessment of Plant-Based Beverages in Comparison to Bovine Milk. Front. Nutr. 2022, 9, 957486. [Google Scholar] [CrossRef]
- Chalupa-Krebzdak, S.; Long, C.J.; Bohrer, B.M. Nutrient Density and Nutritional Value of Milk and Plant-Based Milk Alternatives. Int. Dairy J. 2018, 87, 84–92. [Google Scholar] [CrossRef]
- Angelino, D.; Rosi, A.; Vici, G.; dello Russo, M.; Pellegrini, N.; Martini, D. Nutritional Quality of Plant-Based Drinks Sold in Italy: The Food Labelling of Italian Products (FLIP) Study. Foods 2020, 9, 682. [Google Scholar] [CrossRef]
- Clegg, M.E.; Tarrado Ribes, A.; Reynolds, R.; Kliem, K.; Stergiadis, S. A Comparative Assessment of the Nutritional Composition of Dairy and Plant-Based Dairy Alternatives Available for Sale in the UK and the Implications for Consumers’ Dietary Intakes. Food Res. Int. 2021, 148, 110586. [Google Scholar] [CrossRef]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th Ed.; December 2020. Available online: https://DietaryGuidelines.gov (accessed on 30 March 2023).
- Rivas, M.; Garay, R.P.; Escanero, J.F.; Cia, P.; Alda, J.O. Human Nutrition and Metabolism Research Communication Soy Milk Lowers Blood Pressure in Men and Women with Mild to Moderate Essential Hypertension. J. Nutr. 2002, 132, 1900–1902. [Google Scholar] [CrossRef]
- Sirtori, C.R.; Bosisio, R.; Pazzucconi, F.; Bondioli, A.; Gatti, E.; Lovati, M.R.; Murphy, P. Soy Milk with a High Glycitein Content Does Not Reduce Low-Density Lipoprotein Cholesterolemia in Type II Hypercholesterolemic Patients. Ann. Nutr. Metab. 2002, 46, 88–92. [Google Scholar] [CrossRef]
- Bricarello, L.P.; Kasinski, N.; Bertolami, M.C.; Faludi, A.; Pinto, L.A.; Relvas, W.G.M.; Izar, M.C.O.; Ihara, S.S.M.; Tufik, S.; Fonseca, F.A.H. Comparison between the Effects of Soy Milk and Non-Fat Cow Milk on Lipid Profile and Lipid Peroxidation in Patients with Primary Hypercholesterolemia. Nutrition 2004, 20, 200–204. [Google Scholar] [CrossRef]
- Ryan-Borchers, T.A.; Soon Park, J.; Chew, B.P.; McGuire, M.K.; Fournier, L.R.; Beerman, K.A. Soy Isoflavones Modulate Immune Function in Healthy Postmenopausal Women. Am. J. Clin. Nutr. 2006, 83, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Fournier, L.R.; Ryan-Borchers, T.A.; Robison, L.M.; Robison, L.; Wiediger, M.; Park, J.; Chew, B.; McGuire, M.; Sclar, D.; Skaer, T.; et al. The Effects of Soy Milk and Isoflavone Supplements on Cognitive Performance in Healthy, Postmenopausal Women. J. Nutr. Health Aging 2007, 11, 155–164. [Google Scholar]
- Gardner, C.D.; Kiazand, A.; Morris, J.L.; Messina, M.; Franke, A.A. Effect of Two Types of Soy Milk and Dairy Milk on Plasma Lipids in Hypercholesterolemic Adults: A Randomized Trial. J. Am. Coll. Nutr. 2007, 26, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Lukaszuk, J.M.; Luebbers, P.; Gordon, B.A. Preliminary Study: Soy Milk as Effective as Skim Milk in Promoting Weight Loss. J. Am. Diet Assoc. 2007, 107, 1811–1814. [Google Scholar] [CrossRef]
- Ryan-Borchers, T.; Boon, C.; Park, J.S.; McGuire, M.; Fournier, L.; Beerman, K. Effects of dietary and supplemental forms of isoflavones on thyroid function in healthy postmenopausal women. Top. Clin. Nutr. 2008, 23, 13–22. [Google Scholar] [CrossRef]
- Beavers, K.M.; Serra, M.C.; Beavers, D.P.; Cooke, M.B.; Willoughby, D.S. Soymilk Supplementation Does Not Alter Plasma Markers of Inflammation and Oxidative Stress in Postmenopausal Women. Nutr. Res. 2009, 29, 616–622. [Google Scholar] [CrossRef]
- Rideout, T.C.; Chan, Y.M.; Harding, S.v.; Jones, P.J.H. Low and Moderate-Fat Plant Sterol Fortified Soymilk in Modulation of Plasma Lipids and Cholesterol Kinetics in Subjects with Normal to High Cholesterol Concentrations: Report on Two Randomized Crossover Studies. Lipids Health Dis. 2009, 8, 45. [Google Scholar] [CrossRef]
- Beavers, K.M.; Serra, M.C.; Beavers, D.P.; Cooke, M.B.; Willoughby, D.S. Soy and the Exercise-Induced Inflammatory Response in Postmenopausal Women. Appl. Physiol. Nutr. Metab. 2010, 35, 261–269. [Google Scholar] [CrossRef]
- Beavers, K.M.; Serra, M.C.; Beavers, D.P.; Hudson, G.M.; Willoughby, D.S. The Lipid-Lowering Effects of 4 Weeks of Daily Soymilk or Dairy Milk Ingestion in a Postmenopausal Female Population. J. Med. Food 2010, 13, 650–656. [Google Scholar] [CrossRef]
- Azadbakht, L.; Nurbakhsh, S. Effect of Soy Drink Replacement in a Weight Reducing Diet on Anthropometric Values and Blood Pressure among Overweight and Obese Female Youths. Asia Pac. J. Clin. Nutr. 2011, 20, 383–389. [Google Scholar]
- Faghih, S.; Abadi, A.R.; Hedayati, M.; Kimiagar, S.M. Comparison of the Effects of Cows’ Milk, Fortified Soy Milk, and Calcium Supplement on Weight and Fat Loss in Premenopausal Overweight and Obese Women. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 499–503. [Google Scholar] [CrossRef]
- Fernandez-Raudales, D.; Hoeflinger, J.L.; Bringe, N.A.; Cox, S.B.; Dowd, S.E.; Miller, M.J.; Gonzalez de Mejia, E. Consumption of Different Soymilk Formulations Differentially Affects the Gut Microbiomes of Overweight and Obese Men. Gut Microbes 2012, 3, 490–500. [Google Scholar] [CrossRef]
- Gui, J.C.; Brašié, J.R.; Liu, X.D.; Gong, G.Y.; Zhang, G.M.; Liu, C.J.; Gao, G.Q. Bone Mineral Density in Postmenopausal Chinese Women Treated with Calcium Fortification in Soymilk and Cow’s Milk. Osteoporos. Int. 2012, 23, 1563–1570. [Google Scholar] [CrossRef]
- Keshavarz, S.A.; Nourieh, Z.; Javad, M.; Attar, H.; Azadbakht, L. Effect of Soymilk Consumption on Waist Circumference and Cardiovascular Risks among Overweight and Obese Female Adults. Int. J. Prev. Med. 2012, 3, 798–805. [Google Scholar]
- Miraghajani, M.S.; Esmaillzadeh, A.; Najafabadi, M.M.; Mirlohi, M.; Azadbakht, L. Soy Milk Consumption, Inflammation, Coagulation, and Oxidative Stress among Type 2 Diabetic Patients with Nephropathy. Diabetes Care 2012, 35, 1981–1985. [Google Scholar] [CrossRef]
- Nourieh, Z.; Keshavarz, S.; Hosseinzadehattar, M.; Azadbakht, L. Effect of Soymilk Consumption on Inflammatory Markers and Lipid Profiles among Non-Menopausal Overweight and Obese Female Adults. J. Res. Med. Sci. 2012, 17, 1–8. [Google Scholar]
- Serra, M.C.; Beavers, K.M.; Beavers, D.P.; Willoughby, D.S. Effects of 28 Days of Dairy or Soy Ingestion on Skeletal Markers of Inflammation and Proteolysis in Post-Menopausal Women. Nutr. Health 2012, 21, 117–130. [Google Scholar] [CrossRef]
- Miraghajani, M.S.; Najafabadi, M.M.; Surkan, P.J.; Esmaillzadeh, A.; Mirlohi, M.; Azadbakht, L. Soy Milk Consumption and Blood Pressure Among Type 2 Diabetic Patients With Nephropathy. J. Ren. Nutr. 2013, 23, 277–282.e1. [Google Scholar] [CrossRef]
- Nourozi, M.; Haghollahi, F.; Ramezanzadeh, F.; Hanachi, P. Effect of Soy Milk Consumption on Quality of Life in Iranian Postmenopausal Women. J. Fam. Reprod. Health 2015, 9, 93–100. [Google Scholar]
- Sun, L.; Tan, K.W.J.; Siow, P.C.; Henry, C.J. Soya Milk Exerts Different Effects on Plasma Amino Acid Responses and Incretin Hormone Secretion Compared with Cows’ Milk in Healthy, Young Men. Br. J. Nutr. 2016, 116, 1216–1221. [Google Scholar] [CrossRef]
- Law, M.; Huot, P.S.P.; Lee, Y.T.; Vien, S.; Luhovyy, B.L.; Anderson, G.H. The Effect of Dairy and Nondairy Beverages Consumed with High Glycemic Cereal on Subjective Appetite, Food Intake, and Postprandial Glycemia in Young Adults. Appl. Physiol. Nutr. Metab. 2017, 42, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Tan, K.W.J.; Han, C.M.S.; Leow, M.K.S.; Henry, C.J. Impact of Preloading Either Dairy or Soy Milk on Postprandial Glycemia, Insulinemia and Gastric Emptying in Healthy Adults. Eur. J. Nutr. 2017, 56, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, M.; Suzuki, A.; Kikuchi, M.; Arai, H. Soymilk Intake Has Desirable Effects on Phosphorus and Calcium Metabolism. J. Clin. Biochem. Nutr. 2018, 62, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.; Walker, G.D.; Yuan, Y.; Reynolds, C.; Stanton, D.P.; Fernando, J.R.; Reynolds, E.C. Effects of Soy and Bovine Milk Beverages on Enamel Mineral Content in a Randomized, Double-Blind in Situ Clinical Study. J. Dent. 2019, 88, 103160. [Google Scholar] [CrossRef]
- Ballard, K.D.; Mah, E.; Guo, Y.; Pei, R.; Volek, J.S.; Bruno, R.S. Low-Fat Milk Ingestion Prevents Postprandial Hyperglycemia-Mediated Impairments in Vascular Endothelial Function in Obese Individuals with Metabolic Syndrome. J. Nutr. 2013, 143, 1602–1610. [Google Scholar] [CrossRef]
- Alba, B.K.; Stanhewicz, A.E.; Kenney, W.L.; Alexander, L.M. Acute Dairy Milk Ingestion Does Not Improve Nitric Oxide-Dependent Vasodilation in the Cutaneous Microcirculation. Br. J. Nutr. 2016, 116, 204–210. [Google Scholar] [CrossRef]
- Mintel Group Ltd Milk and Non-Dairy Milk-US—October 2019. Available online: https://academic.mintel.com/display/919346/ (accessed on 19 December 2022).
- Schiano, A.N.; Nishku, S.; Racette, C.M.; Drake, M.A. Parents’ Implicit Perceptions of Dairy Milk and Plant-Based Milk Alternatives. J. Dairy Sci. 2022, 105, 4946–4960. [Google Scholar] [CrossRef]
- Iuliano, S.; Hill, T.R. Dairy Foods and Bone Health throughout the Lifespan: A Critical Appraisal of the Evidence. Br. J. Nutr. 2019, 121, 763–772. [Google Scholar] [CrossRef]
- Rizzoli, R. Dairy Products and Bone Health. Aging Clin. Exp. Res. 2021, 34, 9–24. [Google Scholar] [CrossRef]
- Ratajczak, A.E.; Zawada, A.; Rychter, A.M.; Dobrowolska, A.; Krela-Kaźmierczak, I. Milk and Dairy Products: Good or Bad for Human Bone? Practical Dietary Recommendations for the Prevention and Management of Osteoporosis. Nutrients 2021, 13, 1329. [Google Scholar] [CrossRef]
- Goulding, A.; Rockell, J.E.P.; Black, R.E.; Grant, A.M.; Jones, I.E.; Williams, S.M. Children Who Avoid Drinking Cow’s Milk Are at Increased Risk for Prepubertal Bone Fractures. J. Am. Diet Assoc. 2004, 104, 250–253. [Google Scholar] [CrossRef]
- Lana, A.; Rodriguez-Artalejo, F.; Lopez-Garcia, E. Dairy Consumption and Risk of Frailty in Older Adults: A Prospective Cohort Study. J. Am. Geriatr. Soc. 2015, 63, 1852–1860. [Google Scholar] [CrossRef]
- Menzel, J.; Abraham, K.; Stangl, G.I.; Ueland, P.M.; Obeid, R.; Schulze, M.B.; Herter-Aeberli, I.; Schwerdtle, T.; Weikert, C. Vegan Diet and Bone Health—Results from the Cross-Sectional RBVD Study. Nutrients 2021, 13, 685. [Google Scholar] [CrossRef]
- Iguacel, I.; Miguel-Berges, M.L.; Gómez-Bruton, A.; Moreno, L.A.; Julián, C. Veganism, Vegetarianism, Bone Mineral Density, and Fracture Risk: A Systematic Review and Meta-Analysis. Nutr. Rev. 2019, 77, 1–18. [Google Scholar] [CrossRef]
- Godos, J.; Tieri, M.; Ghelfi, F.; Titta, L.; Marventano, S.; Lafranconi, A.; Gambera, A.; Alonzo, E.; Sciacca, S.; Buscemi, S.; et al. Dairy Foods and Health: An Umbrella Review of Observational Studies. Int. J. Food Sci. Nutr. 2020, 71, 138–151. [Google Scholar] [CrossRef]
- Duranti, M.; Dani, V.; Barbiroli, A.; Scarafoni, A.; Lovati, M.R.; Castiglioni, S.; Ponzone, C.; Morazzoni, P. The A′ Subunit from Soybean 7S Globulin Lowers Plasma Lipids and Upregulates Liver β-VLDL Receptors in Rats Fed a Hypercholesterolemic Diet. J. Nutr. 2004, 134, 1334–1339. [Google Scholar] [CrossRef]
- Wong, W.W.; Smith, E.O.; Stuff, J.E.; Hachey, D.L.; Heird, W.C.; Pownell, H.J. Cholesterol-Lowering Effect of Soy Protein in Normocholesterolemic and Hypercholesterolemic Men. Am. J. Clin. Nutr. 1998, 68, 1385S–1389S. [Google Scholar] [CrossRef]
- Yousef, M.I.; Kamel, K.I.; Esmail, A.M.; Baghdadi, H.H. Antioxidant Activities and Lipid Lowering Effects of Isoflavone in Male Rabbits. Food Chem. Toxicol. 2004, 42, 1497–1503. [Google Scholar] [CrossRef]
- Zhuo, X.-G.; Melby, M.K.; Watanabe, S. Soy Isoflavone Intake Lowers Serum LDL Cholesterol: A Meta-Analysis of 8 Randomized Controlled Trials in Humans. J. Nutr. 2004, 134, 2395–2400. [Google Scholar] [CrossRef]
- Ras, R.T.; Geleijnse, J.M.; Trautwein, E.A. LDL-Cholesterol-Lowering Effect of Plant Sterols and Stanols across Different Dose Ranges: A Meta-Analysis of Randomised Controlled Studies. Br. J. Nutr. 2014, 112, 214–219. [Google Scholar] [CrossRef]
- Dudásová, S.; Grancicová, E. Influence of Casein and Soy Flour Proteins on Aminoacid Content in the Liver of Experimental Animals. Physiol. Res. 1992, 41, 411–416. [Google Scholar]
- De Leo, F.; Panarese, S.; Gallerani, R.; Ceci, L. Angiotensin Converting Enzyme (ACE) Inhibitory Peptides: Production and Implementation of Functional Food. Curr. Pharm. Des. 2009, 15, 3622–3643. [Google Scholar] [CrossRef] [PubMed]
- Ralston, R.A.; Lee, J.H.; Truby, H.; Palermo, C.E.; Walker, K.Z. A Systematic Review and Meta-Analysis of Elevated Blood Pressure and Consumption of Dairy Foods. J. Hum. Hypertens. 2012, 26, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Aljuraiban, G.S.; Stamler, J.; Chan, Q.; van Horn, L.; Daviglus, M.L.; Elliott, P.; Oude Griep, L.M. Relations between Dairy Product Intake and Blood Pressure. J. Hypertens. 2018, 36, 2049–2058. [Google Scholar] [CrossRef] [PubMed]
- Heidari, Z.; Rashidi Pour Fard, N.; Clark, C.C.T.; Haghighatdoost, F. Dairy Products Consumption and the Risk of Hypertension in Adults: An Updated Systematic Review and Dose–Response Meta-Analysis of Prospective Cohort Studies. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1962–1975. [Google Scholar] [CrossRef]
- Wang, H.; Chen, L.; Cao, Y.; Xie, K.; Wang, C.; Pei, P.; Guo, Y.; Bragg, F.; Yu, M.; Chen, Z.; et al. Association between Frequency of Dairy Product Consumption and Hypertension: A Cross-Sectional Study in Zhejiang Province, China. Nutr. Metab. 2022, 19, 67. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Dong, J.; Yang, S.; Zhuang, Q.; Sun, J.; Wei, P.; Zhao, X.; Chen, Y.; Chen, X.; Li, M.; Wei, L.; et al. The Associations of Lipid Profiles With Cardiovascular Diseases and Death in a 10-Year Prospective Cohort Study. Front. Cardiovasc. Med. 2021, 8, 745539. [Google Scholar] [CrossRef]
- Kjeldsen, S.E. Hypertension and Cardiovascular Risk: General Aspects. Pharmacol. Res. 2018, 129, 95–99. [Google Scholar] [CrossRef]
- Scholz-Ahrens, K.E.; Ahrens, F.; Barth, C.A. Nutritional and Health Attributes of Milk and Milk Imitations. Eur. J. Nutr. 2020, 59, 19–34. [Google Scholar] [CrossRef]
| Parameter | Inclusion Criteria |
|---|---|
| Population | Age > 18 years |
| Intervention | Dietary interventions evaluating the effect of PBD |
| Comparison | CM |
| Outcomes | Health and disease markers |
| Study design | Clinical trials |
| (a) Acute Intake (i.e., Single Meal) | ||||||
|---|---|---|---|---|---|---|
| Reference, Country | Study Design | Study Population a | Soy Drink (SD) Intervention b | Cow’s Milk (CM) Intervention b | Health Outcome c | Health-Related Findings c |
| [42] | Postprandial, randomized, crossover, controlled trial (washout period 1 week) | 20 healthy men Age: 21–26 years BMI: 18.3–24.4 kg/m2 | 322 mL of SD (containing approximately 12 g of soy protein) Composition: n.a. | 322 mL of CM (containing approximately 12 g of milk protein) Composition: n.a. | Plasma total active GLP-1, GIP and plasma amino acid profile | ↑ Postprandial active GLP-1 at 90, 120 min with CM vs. SD ↑ GIP with SD at 30, 60, 90 min vs. CM Positive correlations between changes in alanine and arginine and the corresponding change in GIP for the first 30 min ↑ Plasma BCAAs in CM vs. SD |
| [43] | Postprandial, randomized, non-blinded, crossover, controlled trial (washout period ≥ 1 week) | 26 healthy adults (13 F, 13 M) Age: 23.0 ± 2.6 years BMI: 22.3 ± 1.5 kg/m2 | 250 mL of SD Composition per 100 mL:
| 250 mL of CM Composition per 100 mL:
| Subjective appetite, insulin and GLU | Post-treatment blood GLU changes from baseline affected by treatment, time and a time-by-treatment interaction ↓ GLU peak at 30 min with SD vs. CM ↓ Post-treatment GLU with SD vs. CM Post-treatment changes in insulin concentrations from baseline affected by treatment, time and a time-by-treatment interaction ↑ Insulin concentrations post-treatment with CM vs. SD ↓ Post-treatment value of iAUCs for insulin with SD vs. CM ⟷ For appetite between CM vs. SD |
| [44] | Postprandial, randomized, crossover, non-blind trial (washout period 1 week) | 12 healthy males Age: 21–26 years BMI: 21.5 ± 1.4 kg/m2 | 322 mL of sweetened SD Composition: n.a. The test meals were: (1) Preload SD + white bread consumed 30 min later (P-SD) (2) Co-ingestion of SD and bread (CI-SD) For the meal (SD + white bread):
| 322 mL of CM Composition: n.a. The test meals were: (1) Preload low-fat cow’s milk + white bread consumed 30 min later (P-CM) (2) Co-ingestion of low-fat CM with bread (CI-CM) For the meal (CM + white bread):
| GLU, insulin, GI, II and gastric emptying | Blood GLU response affected by time, treatment and the interaction between time and treatment ↓ GLU with P-SD at 30–60 min vs. CI-SD ↑ GLU with P-SD at 120, 150 min vs. CI-SD ↓ GLU after test meal with P-CM at 15, 30 and 45 vs. CI-CM ↑ GLU with P-SD at 30, 45 and 60 vs. P-CM ↓ Peak of GLU response with preloading both drinks vs. their co-ingestion ↑ GLU iAUCs (30, 45, 60 min) P-SD vs. P-CM ↓ GLU iAUCs (from 30 to 120 min) P-SD vs. C-SD ↓ GLU iAUCs P-CM vs. C-CM at all time points ↓ GI of the preload drinks vs. co-ingestion drinks Plasma insulin response dependent on time, treatment and the interaction between time and treatment ↓ Insulin response with P-SD at 30, 60 min vs. CI-SD ↑ Insulin response with P-SD at 120, 210 min vs. CI-SD ↑ Insulin response with CI-CM at 30, 45 min vs. P-CM ↓ Insulin response with CI-CM at 120, 180 min vs. P-CM ↑ Insulin response with P-SD at 30, 45 min vs. P-CM ↓ Peak of insulin response and II with preloading with both drinks vs. their co-ingestion ↓ Insulin iAUCs with P-CM (between 30 and 150 min after the meal) vs. P-SD ↑ Insulin iAUCs at 45–120 min with CI-SD vs. P-SD ↑ II after P-SD vs. P-CM Gastric emptying affected by time, treatment, and the interaction between time and treatment ↑ Slow gastric emptying CI-SD at 15 min and P-CM at 120 min vs. P-SD |
| [45] | Postprandial, randomized, crossover trial (washout period 1 week) | 10 healthy subjects (6 F, 4 M) Age: 22.4 ± 1.2 years BMI: 20.3 ± 6.3 kg/m2 | (1) 335 g of SD Composition per 100 mL:
| 225 g of CM Composition per 100 mL:
| Serum insulin, plasma GLU and intact PTH levels, serum and urine Pi and Ca | ↑ S-PTH levels with SD meal at 30, 60, 120, 240, 360 vs. CM meal ↑ S-PTH levels with SD-Ca meal at 60, 120, 240, 360 vs. SD + Ca meal ↑ S-Pi levels with CM meal vs. SD meal (at 30, 60 and 120 min) and SD + Ca meal (at 60 and 120 min) ↓ S-Ca levels with SD meal vs. CM meal (at 60, 120, 240 and 360 min) and SD + Ca meal (at 30, 60, 120, 240 and 360 min) ⟷ For other parameters between CM vs. SD |
| Reference | Study Design | Study Population a | Rice Drink Intervention b | Cow’s Milk Intervention b | Health Outcome c | Health-Related Findings c |
| [47] | Postprandial, randomized, double-blind, crossover trial (washout period 1 week for men, 1 month for women) | 19 adults (5 F, 14 M) with metabolic syndrome Age: 28.5 ± 2.2 § years BMI: 35.0 ± 0.9 § kg/m2 | 435 mL of RD Composition per 100 mL:
| 475 mL of low-fat CM Composition per 100 mL:
| FMD, plasma GLU, insulin and TGs, AUCSR, MDA, ADMA, ADMA:ARG ratio, fasting mean arterial pressure, heart rate, antioxidant status and oxidative/nitrative stress | ↓ Postprandial FMD of the brachial artery with RD at 30, 60 min vs. baseline ↑ Time-matched FMD responses at 30 min with CM vs. RD ↑ FMD AUC0–3h with CM vs. RD ↓ Main effect of time on maximal post-occlusion diameter with RD at 30 min vs. baseline ↓ AUCSR with CM and RD at 30 min vs. baseline ↑ GLU (from 30 to 120 min) with RD vs. baseline ↑ GLU (30, 120, 150 min) with CM vs. baseline ↑ Insulin (from 30 to 150 min) with RD vs. baseline ↑ Insulin (from 30 to 120 min) with CM vs. baseline The increase in GLU (from 30 to 150 min) was larger during the RD compared to the CM trial ↑ ARG and ARG AUC0–3 h with CM vs. RD ↑ ADMA at 30 min with RD and ↑ at 30–60 min with CM compared to baseline ↑ Time-matched ADMA concentrations at 90, 120 and 180 min with CM vs. RD ↑ ADMA/ARG ratio with CM at 30 min vs. baseline ↑ ADMA/ARG ratio with RD at 60–180 min vs. baseline ↑ ADMA/ARG AUC0–3h with RD vs. CM |
| [48] | Postprandial, randomized, crossover, controlled trial (washout period ≥ 1 week) | 11 healthy subjects (6 F, 5 M) Age: 61 ± 2 § years BMI: 26.1 ± 0.6 § kg/m2 | (1) 473 mL (2 servings) of RD (2) 946 mL (4 servings) of RD Composition per 100 mL of SD:
| (1) 473 mL (2 servings) of CM (2) 946 mL (4 servings) of CM Composition per 100 mL:
| NO-dependent vasodilation (RBF, CVC) and insulin | ↓ %NO-dependent vasodilation with CM vs. RD ingestion ↓ Plasma insulin concentration with CM vs. RD for both the 2 and 4 servings; it was associated with a reduction in NO-dependent vasodilation |
| (b) Long-Term Intake | ||||||
| Reference, Country | Study Design | Study Population a | Soy Drink (SD) Intervention b | Cow’s Milk (CM) Intervention b | Health Outcome c | Health-Related Findings c |
| [20] | 3-month, randomized, parallel, double-blind, controlled trial | 40 adults (15 F, 25 M) with mild-to-moderate hypertension SD group (n = 20: 6 F, 14 M) Age: 47.5 ± 10.4 years BMI: n.a. CM group (n = 20: 9 F, 11 M) Age: 49.4 ± 10.8 years BMI: n.a. | 1 L/d of SD Composition per 100 mL:
| 1 L/d of CM Composition per 100 mL:
| SBP, DBP, MBP | ↓ SBP, DBP and MBP with SD vs. CM ↓ SBP, DBP and MBP with SD vs. baseline Urinary genistein excretion was negatively correlated with the ↓ in DBP |
| [21] | 4-week, double-blind crossover trial (washout period 4 weeks) | 20 patients with hypercholesterolemia (16 F, 4 M) Age: 59.5 ± 8.3 years BMI: 24.2 ± 3.5 kg/m2 | 500 mL/d of SD Composition per 100 mL:
| 500 mL/d of CM Composition: n.a. | Lipid profile (TC, LDL-C) and BW | ⟷ Between CM and SD |
| [22] | 6-week, randomized, double-blind, crossover trial (no washout period) | 60 outpatients with primary hypercholesterolemia (45 F, 15 M) Age: 56 ± 1 § years BMI: 24.9 ± 0.3 § kg/m2 | 1 L/d of SD Composition per 100 mL:
| 1 L/d of CM Composition per 100 mL:
| Lipid profile (TC, HDL-C, LDL-C, triacylglycerols) TBARs and BMI | ↓ LDL-C with SD vs. baseline and CM ↑ HDL-C with SD vs. baseline and CM ↓ TBARs with SD vs. CM ⟷ Triacylglycerols, TC with SD vs. baseline, CM No significant BMI changes in CM and SD |
| [23] | 16-week, randomized, placebo-controlled, parallel, double-blind trial | 52 postmenopausal women SD group (n = 18) Age: 56.1 ± 4.4 § years BMI: 27.4 ± 6.2 § kg/m2 SD + Supplement group (n = 15) Age: 55.9 ± 3.5 § years BMI: 28.8 ± 5.4 § kg/m2 CTRL group (n = 19) Age: 55.4 ± 3.9 § years BMI: 27.5 ± 4.9 § kg/m2 | 706 mL/d of SD plus a placebo supplement Composition per 100 mL:
| (1) 706 mL/d of CM plus a placebo supplement (CTRL) Composition per 100 mL:
Composition per 100 mL of CM:
| Lymphocyte subsets (total T cells, T cytotoxic cells, T helper cells, ratio of Th to Tc cells, B cells, natural killer cells), cytokine production (IFN-γ, TNF-a, IL-2), CRP, lipid peroxidation (8-Isoprostane), DNA damage (8-OHdG) and BMI | A significant effect of group on percentage of B cells ↑ B cell populations in SD and supplement groups vs. CTRL Significant effects of group, week and group x week interaction on plasma 8-OHdg ↓ Plasma concentrations of 8-OHdg in SD and supplement groups vs. CTRL ⟷ For other parameters between CM and SD |
| [24] | 16-week, randomized, parallel, double-blind, controlled trial | 79 postmenopausal women SD group (n = 25) Age: 56.1 ± 0.9 § years BMI: 26.8 ± 1.2 § kg/m2 SD + Supplement group (n = 27) Age: 55.7 ± 0.7 § years BMI: 28.2 ± 0.9 § kg/m2 CTRL group (n = 27) Age: 56.4 ± 0.8 § years BMI: 28.5 ± 1.3 § kg/m2 | 706 mL/d of SD plus a placebo supplement Composition per 100 mL:
| (1) 706 mL/d of CM plus a placebo supplement (CTRL) Composition per 100 mL:
Composition per 100 mL of SD:
| Selective attention (Stroop task), visual long-term memory (pattern recognition), short-term visuospatial memory (Benton Visual Retention Test), visuospatial working memory (Color Match Task), verbal working memory (Digit Ordering Task), verbal memory span (Forward Digit Span), spatial memory span (Corsi Block-Tapping) | ↓ Verbal working memory (Digit Ordering Task) in SD group relative to baseline vs. soy supplement and CTRL groups ↑ Improvements in Color Match performance and in pattern recognition relative to baseline for all the groups ⟷ For other parameters between SD and CM |
| [25] | 4-week, randomized, crossover trial (washout period ≥ 4 week) | 28 hypercholesterolemic adults (22 F, 6 M) Age: 52 ± 9 years BMI: 26 ± 4 kg/m2 | (1) 32 (946.3 mL) oz/d of WB Composition per 100 mL:
Composition per 100 mL:
| 18.5 (547.1 mL) oz/d of organic CM Composition per 100 mL:
| Lipid profile (triacylglycerols, HDL-C, LDL-C), insulin, and GLU | ↓ LDL-C concentration with WB and SPI vs. CM ↑ LDL-C/HDL-C differences among WB and SPI groups vs. CM group ⟷ For other parameters between CM and SD |
| [26] | 8-week, randomized, prospective, parallel, controlled trial | 14 women with overweight/obesity SD group (n = 7) Age: 33.7 ± 6.3 years BMI: 38.4 ± 10.0 kg/m2 Skimmed CM group (n = 7) Age: 29.4 ± 11.0 years BMI: 33.9 ± 10.6 kg/m2 | 720 mL/d of SD Composition: n.a. | 720 mL/d skimmed CM Composition: n.a. | BW, BF%, AC, BMI and FFM, | ↓ Attenuating loss of FFM with CM, SD vs. baseline ↓ BMI, BW, BF% and AC with CM, SD vs. baseline ⟷ For other parameters between CM vs. SD |
| [27] | 16-week, randomized, placebo-controlled, parallel, double-blinded trial | 77 healthy postmenopausal women CTRL group (n = 27) Age: 55.7 ± 0.8 years BMI: 29.4 ± 1.3 kg/m2 SD group (n = 26) Age: 55.8 ± 0.9 years BMI: 27.5 ± 1.2 kg/m2 Supplement group (n = 24) Age: 54.8 ± 0.7 years BMI: 28.6 ± 1.2 kg/m2 | 706 mL/d of SD with placebo tablets (maltodextrin) Composition per 100 mL:
| (1) 706 mL/d of CM + placebo tablet (maltodextrin) Composition per 100 mL:
Composition per 100 mL:
| Serum TSH | ⟷ For TSH between CM and SD |
| [28] | 4-week, single-blind, randomized, parallel, controlled trial | 31 postmenopausal women Vanilla SD group (n = 16) Age: 53.9 ± 3.7 years BMI: 25.4 ± 4.1 kg/m2 Reduced-fat CM group (n = 15) Age: 55.0 ± 3.1 years BMI: 26.3 ± 4.0 kg/m2 | 732 mL/d (3 servings of 244 mL) of SD Composition per 100 mL:
| 709.8 mL/d (3 servings of 236.6 mL) of CM Composition per 100 mL:
| BW, markers of inflammation (TNF-α, IL-6, IL-1β) and oxidative stress (SOD, GPx, COX-2) | ⟷ For the investigated parameters between CM vs. SD |
| [29] | 4-week, two randomized, crossover, controlled, trials (washout period 4 weeks) | STUDY 1 33 (18 F, 15 M) normal to hypercholesterolemic subjects Age: 43.0 ± 2.4 years BMI: 29.1 ± 1.0 kg/m2 | STUDY 1 720 mL/d low-fat PS-enriched SD Composition per 100 mL:
| STUDY 1 720 mL/d CM Composition per 100 mL:
| STUDY 1 TC, HDL-C LDL-C, TG | STUDY 1 ↓ TC and LDL-C with low-fat PS-enriched SD vs. CM ↓ LDL/HDL and TC/HDL ratios with low-fat PS-enriched SD vs. CM ⟷ HDL-C and TG between low-fat PS-enriched SD vs. CM In a subgroup of subjects with initial LDL-C > 3.4 mmol/L, ↓ TC concentrations and LDL-C with low-fat PS-enriched SD vs. CM |
| STUDY 2 23 (13 F, 10 M) hypercholesterolemic subjects Age: 43.9 ± 0.3 years BMI: 30.0 ± 1.5 kg/m2 | STUDY 2 720 mL/d moderate-fat PS-enriched SD Composition per 100 mL:
| STUDY 2 720 mL/d CM Composition per 100 mL:
| STUDY 2 TC, HDL-C, LDL-C, TG, cholesterol absorption and synthesis | STUDY 2 ↓ TC and LDL-C with moderate-fat PS-enriched SD vs. CM ↓ Fasting TG with moderate-fat PS-enriched SD vs. CM ↓ LDL/HDL and TC/HDL ratios with moderate-fat PS-enriched SD vs. CM ↓ Cholesterol absorption with moderate-fat PS-enriched SD vs. CM ⟷ Cholesterol synthesis and HDL-C between moderate-fat PS-enriched SD vs. CM | ||
| [30] | 4-week, single-blind, randomized, parallel, controlled trial | 31 postmenopausal women SD group (n = 16) Age: 53.9 ± 3.7 years BMI: 25.4 ± 4.1 kg/m2 CM group (n = 15) Age: 55.0 ± 3.1 years BMI: 26.3 ± 4.0 kg/m2 | 3 servings/d of vanilla SD Composition per serving:
| 3 servings/d of reduced-fat CM Composition per serving:
| Markers of inflammation (TNF-α, IL-1β, IL-6) and oxidative stress (SOD, GPx COX-2), | A group-by-time effect in the CM group: ↑ TNF-α post-supplementation, ↓ TNF-α in the postexercise period Time effects for plasma SOD and IL-6: ↓ SOD activity from pre-exercise to the 4 h time period ↑ IL-6 from pre-exercise to the 4 h time period No significant group, group-by-time interaction or time effects on other parameters |
| [31] | 4-week, single-blind, randomized, parallel, controlled trial | 32 postmenopausal women Vanilla SD group (n = 16) Age: 53.9 ± 3.7 years BMI: 25.4 ± 4.1 kg/m2 Reduced-fat CM (n = 16) Age: 54.9 ± 3.1 years BMI: 26.3 ± 3.8 kg/m2 | 732 mL/d (3 servings of 244 mL) of SD Composition per 100 mL:
| 709.8 mL/d (3 servings of 236.6 mL) of reduced-fat CM Composition per 100 mL:
| Lipid profile (TC, TG, LDL, HDL) and BW | ⟷ For the lipid profile variables between CM and SD No significant BW changes in CM and SD |
| [32] | 6-week, randomized, open-label, crossover trial (washout period of 3 weeks) | 23 overweight and obese women Age: 22.1 ± 2.7 years BMI: 28.1 ± 0.5 kg/m2 | 240 mL/d of SD Composition per 100 mL:
| 240 mL/d of CM Composition: n.a. | BW, WC, HC, … BMI, DBP and SBP | ↓ SBP, DBP with SD vs. CM ⟷ For other parameters between CM vs. SD |
| [33] | 8-week, randomized, parallel, controlled trial | 85 healthy overweight or obese premenopausal women CTRL group (n = 20) Age: 38.3 ± 9.5 years BMI: 30.8 ± 3.1 kg/m2 Ca group (n = 22) Age: 35.8 ± 8.7 years BMI: 31.5 ± 4.1 kg/m2 CM group (n = 22) Age: 38.3 ± 10.4 years BMI: 30.0 ± 3.6 kg/m2 SD group (n = 21) Age: 37.5 ± 9.3 years BMI: 31.1 ± 4.1 kg/m2 | 660 mL/d (3 servings of 220 mL) of Ca-fortified SD Composition: n.a. | 660 mL/d (3 servings of 220 mL) of low-fat milk CM Composition: n.a. | BW, WC, BMI, WHR, BFM and BF% | ↓ BW, BMI, WC, WHR, BFM and BF% with CM and SD vs. baseline ↑ BW change (% of initial) in the CM vs. SD group ⟷ For other parameters between CM vs. SD |
| [34] | 3-month, randomized, parallel, double-blind trial | 64 overweight and obese male volunteers Age: 32 ± 7 years BMI: 29 ± 4 kg/m2 | (1) 500 mL/d of LGS (49.5% β-conglycinin/6% glycinin) Composition per 100 mL:
Composition per 100 mL:
| 500 mL/d of CM Composition per 100 mL:
| Total bacterial abundance, Bacteroides-Prevotella, Bifidobacterium and Lactobacillus, bacterial diversity, richness and phylogenic abundance profile | ↑ Total bacterial copy numbers with all treatments ↑ Copy number od Bacteroides-Prevotella with LGS vs. baseline ↓ Relative abundance of Firmicutes, copy number of Bifidobacterium and Firmicutes-to-Bacteroidetes ratio with LGCS and SD vs. baseline ↑ Copy number of Lactobacillus with CM vs. baseline ↓ Bacterial diversity and richness and ↑ relative abundance of members in the phylum Proteobacteria with LGS, SD and CM vs. baseline ↑ Relative abundance of Bacteroidetes with LGS and SD vs. baseline ⟷ For other parameters between CM vs. SD |
| [35] | 18-month, randomized, parallel, open-label, controlled trial | 98 postmenopausal women without osteoporosis CM group (n = 50) Age: 55.8 ± 4.1 years BMI: 24.9 ± 3.2 kg/m2 SD group (n = 50) Age: 56.1 ± 4.2 years BMI: 24.0 ± 3.0 kg/m2 CTRL group (n = 41) Age: 57.3 ± 4.3 years BMI: 24.5 ± 2.6 kg/m2 | 250 mL/d of Ca-fortified SD Composition per 100 mL:
| 250 mL/d of CM Composition per 100 mL:
| BMD | ↑ Hip and femoral neck BMD at 18 months with CM vs. baseline ⟷ Lumbar BMD among the three groups |
| [36] | 4-week, randomized, non-blinded, crossover trial (washout period 2 weeks) | 24 overweight and obese women Age: 37.7 ± 1.3 § years BMI: 31.1 ± 0.8 kg/m2 | 240 mL/d of SD Composition per 100 mL:
| 240 mL/d of CM Composition per 100 mL:
| BW, BMI, WC, WHR, DBP, SBP, liver enzymes (AST, ALT), fibrinogen, FBS and insulin | ↓ WC with SD vs. CM ⟷ For other parameters between CM vs. SD |
| [37] | 4-week, randomized, crossover trial (washout period 2 weeks) | 25 type 2 diabetic patients with nephropathy (15 F, 10 M) Age: 51 ± 10 years BMI: 28 ± 4 kg/m2 | 240 mL/d of SD Composition per 100 mL:
| 240 mL/d of CM Composition per 100 mL:
| BW, markers of inflammation (TNF-α, IL-6, hs-CRP) and oxidative stress (MDA), fibrinogen and D-dimer | ↑ Percent changes (reduction) in D-dimer levels with SD vs. CM ⟷ For other parameters between CM vs. SD |
| [38] | 4-week, randomized, non-blinded, crossover trial (washout period 2 weeks) | 24 non-menopausal overweight and obese women Age: 37.7 ± 1.3 years BMI: 30.9 ± 0.8 kg/m2 | 240 mL/d of SD Composition per 100 mL:
| 240 mL/d of CM Composition per 100 mL:
| BW, markers of inflammation (Hs-CRP, IL-6) and lipid profiles (TG, TC, HDL-C, LDL-C) | ↓ Serum LDL with SD vs. CM ⟷ For other parameters between CM and SD |
| [39] | 4-week, single-blinded, randomized, parallel, controlled trial | 31 postmenopausal women SD Group (n = 16) Age: 54 ± 4 years BMI: 25.4 ± 4.1 kg/m2 CM group (n = 15) Age: 55 ± 3 years BMI: 26.3 ± 4.0 kg/m2 | 732 mL/d (3 servings of 244 mL) of SD Composition per 100 mL:
| 720 mL/d (3 servings of 240 mL) of reduced-fat CM Composition per 100 mL:
| Skeletal muscle mRNA expression of inflammatory (TNF-a, IL-1β, IL-6) and proteolytic (calpain 1, calpain 2, ubiquitin, E2, atrogin-1, muRF-1) markers | No group-by-time interactions for the parameters but significant main effects for both groups |
| [40] | 4-week, randomized, non-blinded, crossover, controlled trial (washout period 2 weeks) | 25 type 2 diabetic patients with nephropathy (15 F, 10 M)Age: 51 ± 10 years BMI: 28 ± 4 kg/m2 | 240 mL/d of SD Composition per 100 mL:
| 240 mL/d of CM Composition per 100 mL:
| BW, DBP, SBP, markers of kidney function (blood urea nitrogen, proteinuria, urine/serum creatinine, GFR), lipid profiles (serum TC, TG, HDL-C, LDL-C), serum insulin, GLU and HbA1C | ↓ SBP with SD vs. CM ⟷ For other parameters between CM and SD |
| [41] | 8-month, randomized, parallel, controlled trial | 57 healthy postmenopausal women SD group (n = 34) Age: 52.1 ± 3.1 years BMI: 28.7 ± 3.8 kg/m2 CM group (n = 23) Age: 51.4 ± 2.9 years BMI: 28.6 ± 4.1 kg/m2 | 500 mL/d SD Composition per 100 mL:
| 500 mL/d low-fat CM Composition: n.a. | Quality of life (domains: vasomotor, psychosocial, physical, and sexual) | ↓ Mean score of vasomotor domain (improvement in quality of life) with SD, CM vs. baseline ↑ Mean score of sexual domain (deterioration in quality of life) with CM vs. baseline, SD ⟷ For other parameters between CM vs. SD |
| [46] | 2-week, randomized double-blind, crossover trial (washout period 1 week) | 8 participants (5 F, 3 M) Mean age: 43 (29–60) years BMI: n.a. | 200 mL/d of SD Composition per 100 mL:
| 200 mL/d of CM Composition per 100 mL:
| Enamel lesion depth (LDb, Lda LDb-Lda) | ↓ LDb-Lda with SD vs. CM ↑ ΔZb–Δza with CM (remineralization of the pre-existing subsurface enamel lesions) vs. SD |
| Reference | Study Design | Study Population a | Almond Drink Intervention b | Cow’s Milk Intervention b | Health Outcome c | Health-Related Findings c |
| [43] | Postprandial, randomized, non-blinded, crossover, controlled trial (washout period ≥ 1 week) | 26 healthy adults (13 F, 13 M) Age: 23.0 ± 2.6 years BMI: 22.3 ± 1.5 kg/m2 | 250 mL of AD Composition per 100 mL:
| 250 mL of CM Composition per 100 mL:
| Subjective appetite, insulin and PPG | ⟷ For appetite between CM and SD Glucose/insulin iAUC ratio with AD vs. CM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biscotti, P.; Del Bo’, C.; Carvalho, C.; Torres, D.; Reboul, E.; Pellegrini, B.; Vinelli, V.; Polito, A.; Censi, L.; Porrini, M.; et al. Can the Substitution of Milk with Plant-Based Drinks Affect Health-Related Markers? A Systematic Review of Human Intervention Studies in Adults. Nutrients 2023, 15, 2603. https://doi.org/10.3390/nu15112603
Biscotti P, Del Bo’ C, Carvalho C, Torres D, Reboul E, Pellegrini B, Vinelli V, Polito A, Censi L, Porrini M, et al. Can the Substitution of Milk with Plant-Based Drinks Affect Health-Related Markers? A Systematic Review of Human Intervention Studies in Adults. Nutrients. 2023; 15(11):2603. https://doi.org/10.3390/nu15112603
Chicago/Turabian StyleBiscotti, Paola, Cristian Del Bo’, Catarina Carvalho, Duarte Torres, Emmanuelle Reboul, Beatrice Pellegrini, Valentina Vinelli, Angela Polito, Laura Censi, Marisa Porrini, and et al. 2023. "Can the Substitution of Milk with Plant-Based Drinks Affect Health-Related Markers? A Systematic Review of Human Intervention Studies in Adults" Nutrients 15, no. 11: 2603. https://doi.org/10.3390/nu15112603
APA StyleBiscotti, P., Del Bo’, C., Carvalho, C., Torres, D., Reboul, E., Pellegrini, B., Vinelli, V., Polito, A., Censi, L., Porrini, M., Martini, D., & Riso, P. (2023). Can the Substitution of Milk with Plant-Based Drinks Affect Health-Related Markers? A Systematic Review of Human Intervention Studies in Adults. Nutrients, 15(11), 2603. https://doi.org/10.3390/nu15112603















