Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
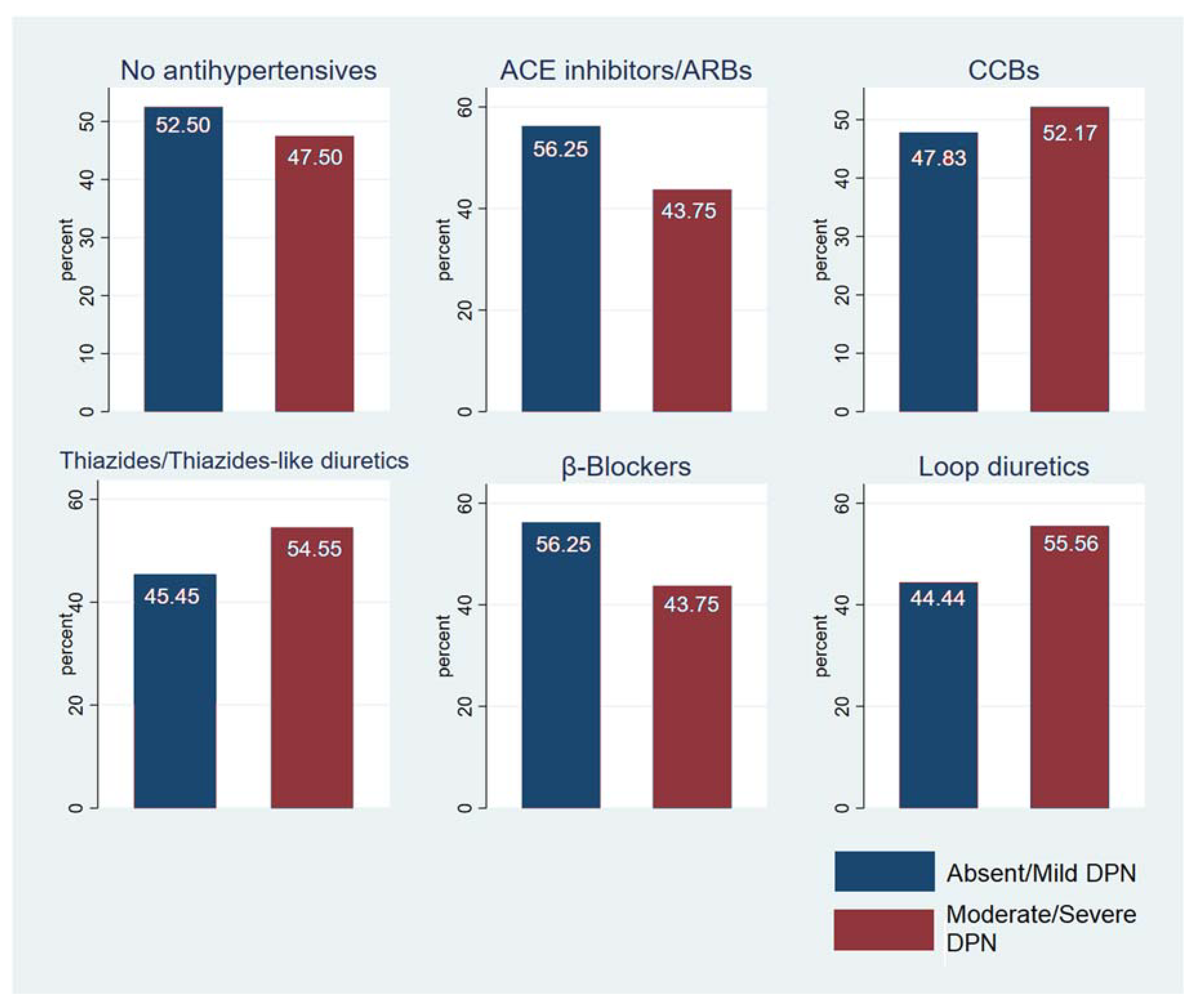
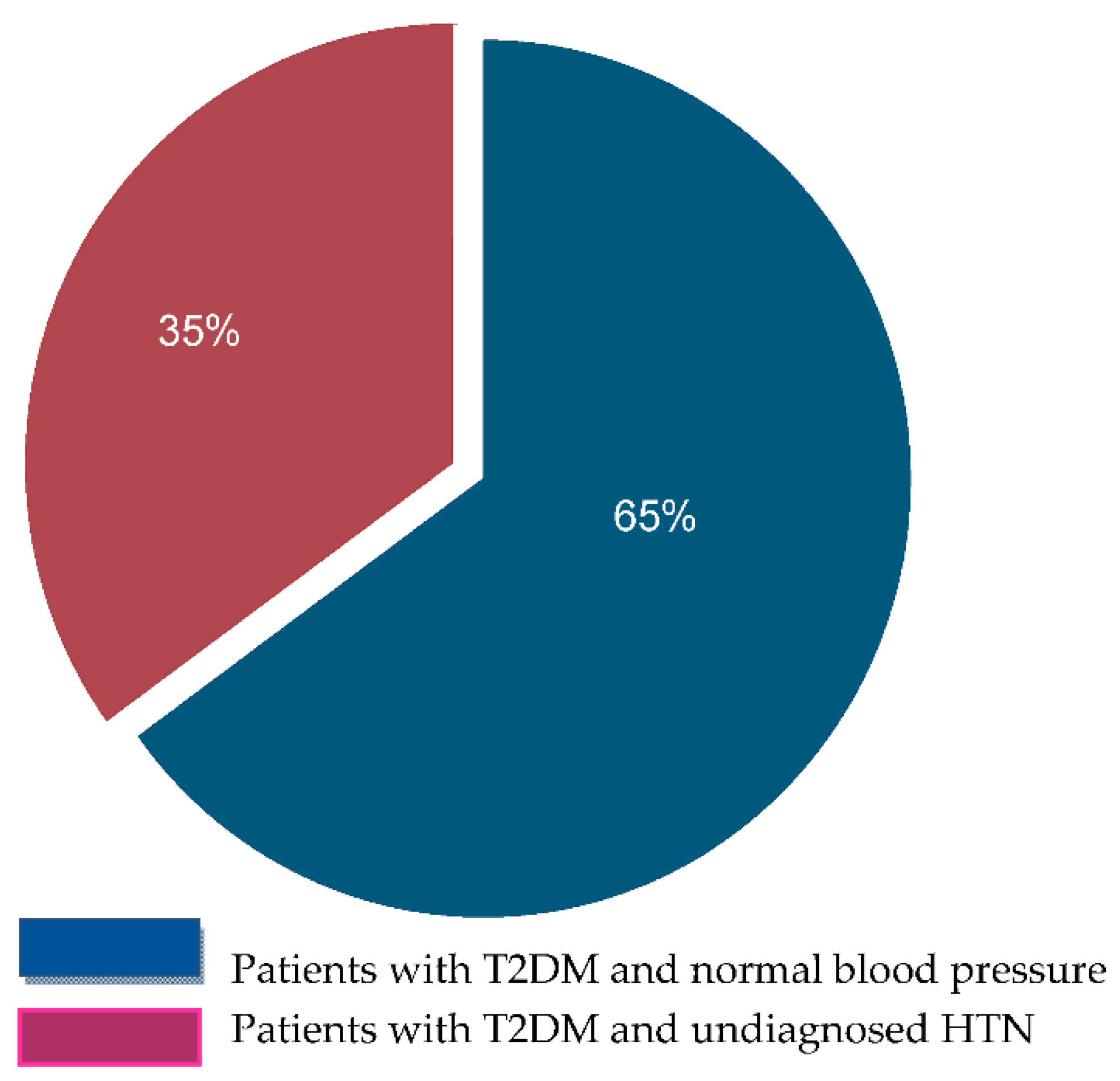
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr. Diabetes Rep. 2019, 19, 86. [Google Scholar] [CrossRef]
- Venguidesvarane, A.G.; Jasmine, A.; Varadarajan, S.; Shriraam, V.; Muthuthandavan, A.R.; Durai, V.; Thiruvengadam, G.; Mahadevan, S. Prevalence of Vascular Complications Among Type 2 Diabetic Patients in a Rural Health Center in South India. J. Prim. Care Community Health 2020, 11, 2150132720959962. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, Z.; Mi, J.; Wang, G.; Tian, L.; Zhao, Y.; Li, X.; Li, X.; Wang, X. Interventional Clinical Trials on Diabetic Peripheral Neuropathy: A Retrospective Analysis. J. Pain Res. 2021, 14, 2651–2664. [Google Scholar] [CrossRef]
- Dyck, P.J.; Kratz, K.M.; Karnes, J.L.; Litchy, W.J.; Klein, R.; Pach, J.M.; Wilson, D.M.; O’Brien, P.C.; Melton, L.J. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: The Rochester Diabetic Neuropathy Study. Neurology 1993, 43, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Darling, J.D.; McCallum, J.C.; Soden, P.A.; Meng, Y.; Wyers, M.C.; Hamdan, A.D.; Verhagen, H.J.; Schermerhorn, M.L. Predictive ability of the Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system following infrapopliteal endovascular interventions for critical limb ischemia. J. Vasc. Surg. 2016, 64, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Tommerdahl, K.L.; Shapiro, A.L.B.; Nehus, E.J.; Bjornstad, P. Early microvascular complications in type 1 and type 2 diabetes: Recent developments and updates. Pediatr. Nephrol. 2021, 37, 79–93. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, Z.; Azmi, S.; Yadav, R.; Ferdousi, M.; Kumar, M.; Cuthbertson, D.J.; Lim, J.; Malik, R.A.; Alam, U. Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Pharmacotherapy. Clin. Ther. 2018, 40, 828–849. [Google Scholar] [CrossRef]
- Martin, C.L.; Albers, J.W.; Pop-Busui, R. Neuropathy and related findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care 2014, 37, 31–38. [Google Scholar] [CrossRef]
- Pop-Busui, R.; Boulton, A.J.; Feldman, E.L.; Bril, V.; Freeman, R.; Malik, R.A.; Sosenko, J.M.; Ziegler, D. Diabetic Neuropathy: A Position Statement by the American Diabetes Association. Diabetes Care 2017, 40, 136–154. [Google Scholar] [CrossRef]
- Boulton, A.J.M. The diabetic foot: Grand overview, epidemiology and pathogenesis. Diabetes/Metab. Res. Rev. 2008, 24, S3–S6. [Google Scholar] [CrossRef]
- Al-Rubeaan, K.; Al Derwish, M.; Ouizi, S.; Youssef, A.M.; Subhani, S.N.; Ibrahim, H.M.; Alamri, B.N. Diabetic Foot Complications and Their Risk Factors from a Large Retrospective Cohort Study. PLoS ONE 2015, 10, e0124446. [Google Scholar] [CrossRef] [PubMed]
- Vithian, K.; Hurel, S. Microvascular complications: Pathophysiology and management. Clin. Med. 2010, 10, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef]
- Zochodne, D.W. Diabetes and the plasticity of sensory neurons. Neurosci. Lett. 2015, 596, 60–65. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; AgabitiRosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Rossboth, S.; Rossboth, B.; Schoenherr, H.; Lechleitner, M.; Oberaigner, W. Risk factors for diabetic foot complications among patients with type 2 diabetes in Austria–A registry-based retrospective cohort study. Endocrinol. Diabetes Metab. 2021, 4, e00286. [Google Scholar] [CrossRef]
- Khan, M.I.H.; Azhar, U.; Zubair, F.; Khan, Z.A. Can we link foot ulcer with risk factors in diabetics? A study in a tertiary care hospital. Pak. J. Med Sci. 2018, 34, 1375–1380. [Google Scholar] [CrossRef]
- Seid, M.A.; Akalu, Y.; Gela, Y.Y.; Belsti, Y.; Diress, M.; Fekadu, S.A.; Dagnew, B.; Getnet, M. Microvascular complications and its predictors among type 2 diabetes mellitus patients at Dessie town hospitals, Ethiopia. Diabetol. Metab. Syndr. 2021, 13, 86. [Google Scholar] [CrossRef]
- Stegenga, M.E.; van der Crabben, S.N.; Levi, M.; de Vos, A.F.; Tanck, M.W.; Sauerwein, H.P.; van der Poll, T. Hyperglycemia Stimulates Coagulation, Whereas Hyperinsulinemia Impairs Fibrinolysis in Healthy Humans. Diabetes 2006, 55, 1807–1812. [Google Scholar] [CrossRef]
- Stout, R.W. Insulin-stimulated lipogenesis in arterial tissue in relation to diabetes and atheroma. Lancet 1968, 292, 702–703. [Google Scholar] [CrossRef]
- Dandona, P.; Chaudhuri, A.; Dhindsa, S. Proinflammatory and Prothrombotic Effects of Hypoglycemia. Diabetes Care 2010, 33, 1686–1687. [Google Scholar] [CrossRef] [PubMed]
- Azhar, A.; Basheer, M.; Abdelgawad, M.S.; Roshdi, H.; Kamel, M.F. Prevalence of Peripheral Arterial Disease in Diabetic Foot Ulcer Patients and its Impact in Limb Salvage. Int. J. Low. Extrem. Wounds 2021, 15347346211027063. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, C.R.L.; Leite, N.C.; Bacan, G.; Ataíde, D.S.; Gorgonio, L.K.; Salles, G.F. Prognostic Importance of Resistant Hypertension in Patients With Type 2 Diabetes: The Rio de Janeiro Type 2 Diabetes Cohort Study. Diabetes Care 2020, 43, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Gebabo, T.F.; Zewdie, T.H.; Shagaro, S.S.; Haile, F. Determinants of peripheral neuropathy among diabetic patients under follow-up in chronic care clinics of public hospitals at Gamo and Gofa zones, southern Ethiopia. PLoS ONE 2021, 16, e0246722. [Google Scholar] [CrossRef]
- Huang, L.; Zhang, Y.; Wang, Y.; Shen, X.; Yan, S. Diabetic Peripheral Neuropathy Is Associated With Higher Systolic Blood Pressure in Adults With Type 2 Diabetes With and Without Hypertension in the Chinese Han Population. Can. J. Diabetes 2020, 44, 615–623. [Google Scholar] [CrossRef]
- Abougalambou, S.S.I.; Abougalambou, A.S. A study evaluating prevalence of hypertension and risk factors affecting on blood pressure control among type 2 diabetes patients attending teaching hospital in Malaysia. Diabetes Metab. Syndr. Clin. Res. Rev. 2013, 7, 83–86. [Google Scholar] [CrossRef]
- Devi, P.; Rao, M.; A Sigamani, A.; A Faruqui, A.; Jose, M.; Gupta, R.; Kerkar, P.; Jain, R.K.; Joshi, R.; Chidambaram, N.; et al. Prevalence, risk factors and awareness of hypertension in India: A systematic review. J. Hum. Hypertens. 2013, 27, 281–287. [Google Scholar] [CrossRef]
- Benenson, I.; Waldron, F.A.; Jadotte, Y.T.; Dreker, M.P.; Holly, C. Risk factors for hypertensive crisis in adult patients: A systematic review. JBI Èvid. Synth. 2021, 19, 1292–1327. [Google Scholar] [CrossRef]
- Naing, C.; Aung, K. Prevalence and risk factors of hypertension in myanmar: A systematic review and meta-analysis. Medicine 2014, 93, e100. [Google Scholar] [CrossRef]
- Van Der Velde, J.H.P.M.; Koster, A.; Strotmeyer, E.S.; Mess, W.H.; Hilkman, D.; Reulen, J.P.H.; Stehouwer, C.D.A.; Henry, R.M.A.; Schram, M.T.; Van Der Kallen, C.J.H.; et al. Cardiometabolic risk factors as determinants of peripheral nerve function: The Maastricht Study. Diabetologia 2020, 63, 1648–1658. [Google Scholar] [CrossRef]
- Rossboth, S.; Lechleitner, M.; Oberaigner, W. Risk factors for diabetic foot complications in type 2 diabetes—A systematic review. Endocrinol. Diabetes Metab. 2021, 4, e00175. [Google Scholar] [CrossRef] [PubMed]
- Baxi, H.; Habib, A.; Hussain, S.; Hussain, S.; Dubey, K. Prevalence of peripheral neuropathy and associated pain in patients with diabetes mellitus: Evidence from a cross-sectional study. J. Diabetes Metab. Disord. 2020, 19, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.A.; Park, T.S.; Jin, H.Y. Non-glucose risk factors in the pathogenesis of diabetic peripheral neuropathy. Endocrine 2020, 70, 465–478. [Google Scholar] [CrossRef]
- Vinik, A.I.; Erbas, T.; Stansberry, K.B.; Pittenger, G.L. Small fiber neuropathy and neurovascular disturbances in diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 2001, 109 (Suppl. 2), S451–S473. [Google Scholar] [CrossRef]
- Han, L.; Ji, L.; Chang, J.; Wen, J.; Zhao, W.; Shi, H.; Zhou, L.; Li, Y.; Hu, R.; Hu, J.; et al. Peripheral neuropathy is associated with insulin resistance independent of metabolic syndrome. Diabetol. Metab. Syndr. 2015, 7, 14. [Google Scholar] [CrossRef]
- Lee, K.O.; Nam, J.S.; Ahn, C.W.; Hong, J.; Kim, S.M.; Sunwoo, I.-N.; Moon, J.-S.; Na, S.-J.; Choi, Y.-C. Insulin resistance is independently associated with peripheral and autonomic neuropathy in Korean type 2 diabetic patients. Acta Diabetol. 2012, 49, 97–103. [Google Scholar] [CrossRef]
- Feldman, E.L.; Nave, K.-A.; Jensen, T.S.; Bennett, D.L.H. New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and Pain. Neuron 2017, 93, 1296–1313. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.M.; Callaghan, B.C.; Smith, A.L.; Feldman, E. Diabetic neuropathy: Cellular mechanisms as therapeutic targets. Nat. Rev. Neurol. 2011, 7, 573–583. [Google Scholar] [CrossRef]
- Edwards, J.L.; Vincent, A.M.; Cheng, H.T.; Feldman, E.L. Diabetic neuropathy: Mechanisms to management. Pharmacol. Ther. 2008, 120, 1–34. [Google Scholar] [CrossRef]
- Sugimoto, K.; Baba, M.; Suzuki, S.; Yagihashi, S. The Impact of Low-Dose Insulin on Peripheral Nerve Insulin Receptor Signaling in Streptozotocin-Induced Diabetic Rats. PLoS ONE 2013, 8, e74247. [Google Scholar] [CrossRef]
- Plum, L.; Schubert, M.; Brüning, J.C. The role of insulin receptor signaling in the brain. Trends Endocrinol. Metab. 2005, 16, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Baiou, D.; Santha, P.; Avelino, A.; Charrua, A.; Bacskai, T.; Matesz, K.; Cruz, F.; Nagy, I. Neurochemical characterization of insulin receptor-expressing primary sensory neurons in wild-type and vanilloid type 1 transient receptor potential receptor knockout mice. J. Comp. Neurol. 2007, 503, 334–347. [Google Scholar] [CrossRef] [PubMed]
- Murakawa, Y.; Zhang, W.; Pierson, C.R.; Brismar, T.; Östenson, C.-G.; Efendic, S.; Sima, A.A.F. Impaired glucose tolerance and insulinopenia in the GK-rat causes peripheral neuropathy. Diabetes/Metabolism Res. Rev. 2002, 18, 473–483. [Google Scholar] [CrossRef]
- Grote, C.W.; Wright, D.E. A Role for Insulin in Diabetic Neuropathy. Front. Neurosci. 2016, 10, 581. [Google Scholar] [CrossRef] [PubMed]
- Roden, M.; Shulman, G.I. The integrative biology of type 2 diabetes. Nature 2019, 576, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Laakso, M.; Kuusisto, J. Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat. Rev. Endocrinol. 2014, 10, 293–302. [Google Scholar] [CrossRef]
- Groop, P.-H.; Forsblom, C.; Thomas, M.C. Mechanisms of Disease: Pathway-selective insulin resistance and microvascular complications of diabetes. Nat. Clin. Pract. Endocrinol. Metab. 2005, 1, 100–110. [Google Scholar] [CrossRef]
- Thrainsdottir, S.; Malik, R.A.; Dahlin, L.B.; Wiksell, P.; Eriksson, K.F.; Rosén, I.; Petersson, J.; Greene, D.A.; Sundkvist, G. Endoneurial Capillary Abnormalities Presage Deterioration of Glucose Tolerance and Accompany Peripheral Neuropathy in Man. Diabetes 2003, 52, 2615–2622. [Google Scholar] [CrossRef]
- Corbin, K.D.; Driscoll, K.A.; Pratley, R.E.; Smith, S.R.; Maahs, D.M.; Mayer-Davis, E.J. Obesity in Type 1 Diabetes: Pathophysiology, Clinical Impact, and Mechanisms. Endocr. Rev. 2018, 39, 629–663. [Google Scholar] [CrossRef]
- Kilpatrick, E.S.; Rigby, A.S.; Atkin, S.L. Insulin resistance, the metabolic syndrome, and complication risk in type 1 diabetes: “double diabetes” in the Diabetes Control and Complications Trial. Diabetes Care 2007, 30, 707–712. [Google Scholar] [CrossRef]
- Ferrannini, E.; Galvan, A.Q.; Gastaldelli, A.; Camastra, S.; Sironi, A.M.; Toschi, E.; Baldi, S.; Frascerra, S.; Monzani, F.; Antonelli, A.; et al. Insulin: New roles for an ancient hormone. Eur. J. Clin. Investig. 1999, 29, 842–852. [Google Scholar] [CrossRef] [PubMed]
- King, G.L.; Goodman, A.D.; Buzney, S.; Moses, A.; Kahn, C.R. Receptors and growth-promoting effects of insulin and insulinlike growth factors on cells from bovine retinal capillaries and aorta. J. Clin. Investig. 1985, 75, 1028–1036. [Google Scholar] [CrossRef] [PubMed]
- Niskanen, L.K.; I Uusitupa, M.; Sarlund, H.; Siitonen, O.; Pyörälä, K. Five-Year Follow-Up Study on Plasma Insulin Levels in Newly Diagnosed NIDDM Patients and Nondiabetic Subjects. Diabetes Care 1990, 13, 41–48. [Google Scholar] [CrossRef]
- Singh, B.; Xu, Y.; McLaughlin, T.; Singh, V.; Martinez, J.A.; Krishnan, A.; Zochodne, D.W. Resistance to trophic neurite outgrowth of sensory neurons exposed to insulin. J. Neurochem. 2012, 121, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Partanen, J.; Niskanen, L.; Lehtinen, J.; Mervaala, E.; Siitonen, O.; Uusitupa, M. Natural History of Peripheral Neuropathy in Patients with Non-Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1995, 333, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Brussee, V.; Cunningham, F.A.; Zochodne, D.W. Direct Insulin Signaling of Neurons Reverses Diabetic Neuropathy. Diabetes 2004, 53, 1824–1830. [Google Scholar] [CrossRef]
- Najafi, M.T.; Khaloo, P.; Alemi, H.; Jaafarinia, A.; Blaha, M.J.; Mirbolouk, M.; Mansournia, M.A.; Afarideh, M.; Esteghamati, S.; Nakhjavani, M.; et al. Ambulatory blood pressure monitoring and diabetes complications. Medicine 2018, 97, e12185. [Google Scholar] [CrossRef]
- Kario, K. Prognosis in Relation to Blood Pressure Variability. Hypertension 2015, 65, 1163–1169. [Google Scholar] [CrossRef]
- Epstein, M.; Sowers, J.R. Diabetes mellitus and hypertension. Hypertension 1992, 19, 403–418. [Google Scholar] [CrossRef]
- Kim, Y.-S.; Davis, S.C.A.T.; Stok, W.J.; van Ittersum, F.J.; van Lieshout, J.J. Impaired nocturnal blood pressure dipping in patients with type 2 diabetes mellitus. Hypertens. Res. 2019, 42, 59–66. [Google Scholar] [CrossRef]
- Spallone, V. Blood Pressure Variability and Autonomic Dysfunction. Curr. Diabetes Rep. 2018, 18, 137. [Google Scholar] [CrossRef] [PubMed]
- Spallone, V.; Bernardi, L.; Ricordi, L.; Soldà, P.; Maiello, M.R.; Calciati, A.; Gambardella, S.; Fratino, P.; Menzinger, G. Relationship Between the Circadian Rhythms of Blood Pressure and Sympathovagal Balance in Diabetic Autonomic Neuropathy. Diabetes 1993, 42, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Mahabala, C.; Kamath, P.; Bhaskaran, U.; Pai, N.D.; Pai, A.U. Antihypertensive therapy: Nocturnal dippers and nondippers. Do we treat them differently? Vasc. Health Risk Manag. 2013, 9, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ye, Y.; Liu, C.; Zhou, Y.; Lv, L.; Cheng, C.; Li, S.; Lou, T.; Liu, X. Evening versus morning dosing regimen drug therapy for chronic kidney disease patients with hypertension in blood pressure patterns: A systematic review and meta-analysis. Intern. Med. J. 2017, 47, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, X.; Huang, W.; Leo, S.; Li, Y.; Liu, M.; Yuan, H. Evening -Versus Morning- Dosing Drug Therapy for Chronic Kidney Disease Patients with Hypertension: A Systematic Review. Kidney Blood Press. Res. 2014, 39, 427–440. [Google Scholar] [CrossRef]
- Salles, G.F.; Reboldi, G.; Fagard, R.H.; Cardoso, C.R.; Pierdomenico, S.D.; Verdecchia, P.; Eguchi, K.; Kario, K.; Hoshide, S.; Polonia, J.; et al. Prognostic Effect of the Nocturnal Blood Pressure Fall in Hypertensive Patients: The Ambulatory Blood Pressure Collaboration in Patients With Hypertension (ABC-H) Meta-Analysis. Hypertension 2016, 67, 693–700. [Google Scholar] [CrossRef]
- Vij, R.; Peixoto, A.J. Management of nocturnal hypertension. Expert Rev. Cardiovasc. Ther. 2009, 7, 607–618. [Google Scholar] [CrossRef]
- Hermida, R.C.; Ayala, D.E.; Fernández, J.R.; Mojón, A.; Smolensky, M.H. Hypertension: New perspective on its definition and clinical management by bedtime therapy substantially reduces cardiovascular disease risk. Eur. J. Clin. Investig. 2018, 48, e12909. [Google Scholar] [CrossRef]
- Schillaci, G.; Battista, F.; Settimi, L.; Schillaci, L.; Pucci, G. Antihypertensive Drug Treatment and Circadian Blood Pressure Rhythm: A Review of the Role of Chronotherapy in Hypertension. Curr. Pharm. Des. 2015, 21, 756–772. [Google Scholar] [CrossRef]
- Fagard, R.H.; Thijs, L.; A Staessen, J.; Clement, D.L.; De Buyzere, M.L.; A De Bacquer, D. Night–day blood pressure ratio and dipping pattern as predictors of death and cardiovascular events in hypertension. J. Hum. Hypertens. 2009, 23, 645–653. [Google Scholar] [CrossRef]
- Hermida, R.C.; Hermida-Ayala, R.G.; Smolensky, M.H.; Mojón, A.; Crespo, J.J.; Otero, A.; Ríos, M.T.; Domínguez-Sardiña, M.; Fernández, J.R. Does Timing of Antihypertensive Medication Dosing Matter? Curr. Cardiol. Rep. 2020, 22, 118. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, H.C. Reduction of cardiovascular events and microvascular complications in diabetes with ACE inhibitor treatment: HOPE and MICRO-HOPE. Diabetes/Metab. Res. Rev. 2002, 18, S82–S85. [Google Scholar] [CrossRef] [PubMed]
- Hermida, R.C.; Ayala, D.E.; Mojón-Ojea, A.; Fernández, J.R. Influence of circadian time of hypertension treatment on cardiovascular risk: Results of the MAPEC study. Chronobiol. Int. 2010, 27, 1629–1651. [Google Scholar] [CrossRef] [PubMed]
- Hermida, R.C.; Crespo, J.J.; Domínguez-Sardiña, M.; Otero, A.; Moyá, A.; Ríos, M.T.; Sineiro, E.; Castiñeira, M.C.; A Callejas, P.; Pousa, L.; et al. Bedtime hypertension treatment improves cardiovascular risk reduction: The Hygia Chronotherapy Trial. Eur. Hear. J. 2020, 41, 4565–4576. [Google Scholar] [CrossRef]
- Xie, Z.; Zhang, J.; Wang, C.; Yan, X. Chronotherapy for morning blood pressure surge in hypertensive patients: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2021, 21, 274. [Google Scholar] [CrossRef]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R.; et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Rural and Urban Communities in High-, Middle-, and Low-Income Countries. JAMA 2013, 310, 959–968. [Google Scholar] [CrossRef]
- Lindholt, J.S.; Søgaard, R. Population screening and intervention for vascular disease in Danish men (VIVA): A randomised controlled trial. Lancet 2017, 390, 2256–2265. [Google Scholar] [CrossRef]
- Altunkeser, B.B.; Avci, A.; Demir, K.; Kaya, Z.; Marakoglu, K.; Ceylan, E.; Ekmekci, A.H.; Yilmaz, M.B.; Demir, A. Arterial Stiffness and Carotid Intima-Media Thickness in Diabetic Peripheral Neuropathy. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2014, 20, 2074–2081. [Google Scholar] [CrossRef][Green Version]
- Wang, S.; Randall, D.C.; Knapp, C.F.; Patwardhan, A.R.; Nelson, K.R.; Karounos, D.G.; Evans, J.M. Blood pressure regulation in diabetic patients with and without peripheral neuropathy. Am. J. Physiol. Integr. Comp. Physiol. 2012, 302, R541–R550. [Google Scholar] [CrossRef]
- Lambadiari, V.; Triantafyllou, K.; Dimitriadis, G.D. Insulin action in muscle and adipose tissue in type 2 diabetes: The significance of blood flow. World J. Diabetes 2015, 6, 626–633. [Google Scholar] [CrossRef]

| Characteristics | Total n = 102 | Absent/Mild DPN n = 54 | Moderate/ Severe DPN n = 48 | p-Value |
|---|---|---|---|---|
| Sex, n (%) | 0.111 1 | |||
| Males | 64 (62.75) | 30 (55.56) | 34 (70.83) | |
| Females | 38 (37.25) | 24 (44.44) | 14 (29.17) | |
| Age (years) | 60.45 (±11.3) | 61.91 (±11.37) | 58.81 (±11.12) | 0.1687 2 |
| BMI (kg/m2) | 30.37 (±5.94) | 28.78 (±4.39) | 32.1 (±6.9) | 0.0047 2 |
| Duration of HTN (years) | 6.88 (±8.7) | 8.07 (±9.59) | 5.54 (±7.45) | 0.1432 2 |
| Duration of DΜ (years) | 14.03 (±9.84) | 13.94 (±10.08) | 14.13 (±9.67) | 0.9268 2 |
| DM Type, n (%) | ||||
| T1DM | 7 (6.86) | 2 (3.70) | 5 (10.42) | 0.181 1 |
| T2DM | 95 (93.10) | 52 (96.30) | 43 (89.58) | |
| HbA1c (%) | 7.65 (±1.76) | 7.29 (±1.36) | 8.05 (±2.07) | 0.0306 2 |
| 24 h ABPM (mmHg) | Total n = 102 | Absent/ Mild DPN n = 54 | Moderate/ Severe DPN n = 48 | p-Value |
|---|---|---|---|---|
| 24 h SBP | 123.47 (11.92) | 121.96 (12.46) | 125.17 (11.17) | 0.1767 |
| 24 h DBP | 71.23 (7.45) | 69.59 (7.06) | 73.06 (7.52) | 0.0181 |
| Daytime SBP | 125.4 (11.44) | 124.5 (12.02) | 126.42 (10.77) | 0.4009 |
| Daytime DBP | 73.32 (7.21) | 72.24 (7.05) | 74.54 (7.26) | 0.1079 |
| Nighttime SBP | 117.39 (16.76) | 114.14 (17.5) | 121.44 (15.04) | 0.0371 |
| Nighttime DBP | 64.63 (9.45) | 62.33 (8.5) | 67.49 (9.88) | 0.0085 |
| 24 h ABPM | Total n = 102 | Absent/ Mild DPN n = 54 | Moderate/ Severe DPN n = 48 | p-Values |
|---|---|---|---|---|
| 24 h HTN stages, n (%) | ||||
| <120/<80 | 37 (36.27) | 21 (38.89) | 16 (33.33) | 0.854 |
| 120–129 and /80–84 | 31 (30.39) | 17 (31.48) | 14 (29.17) | |
| 130–139 or /85–89 | 24 (23.53) | 11 (20.37) | 13 (27.08) | |
| >140 or /90 | 10 (9.8) | 5 (9.26) | 5 (10.42) | |
| ABPM patterns, n (%) | 0.323 | |||
| No extra pattern | 57 (55.88) | 32 (59.26) | 25 (52.08) | |
| WCH | 37 (36.27) | 16 (29.63) | 21 (43.75) | |
| Masked HTN | 7 (6.86) | 5 (9.26) | 2 (4.17) | |
| ABPM dipping status, n (%) | 0.061 | |||
| Dippers | 36 (37.5) | 24 (47.06) | 12 (26.67) | |
| Non-dippers | 36 (37.5) | 14 (27.45) | 22 (48.89) | |
| Reverse dippers | 24 (25) | 13 (25.49) | 11 (24.44) | |
| Univariate Model | Multivariate Model | |||||
|---|---|---|---|---|---|---|
| Variables | OR | 95% CI | p-Value | OR | 95% CI | p-Value |
| Age (in years) | 0.98 | (0.94–1.01) | 0.169 | 0.98 | (0.94–1.02) | 0.335 |
| Sex | ||||||
| Females vs. Males | 0.51 | (0.23–1.17) | 0.113 | 0.35 | (0.14–0.92) | 0.033 |
| Smoking | ||||||
| Yes vs. No | 1.75 | (0.73–4.21) | 0.212 | |||
| ΒΜΙ | 1.11 | (1.02–1.20) | 0.008 | |||
| HTN (years) | 0.96 | (0.92–1.01) | 0.148 | |||
| DM (years) | 1.00 | (0.96–1.04) | 0.926 | |||
| HbA1c (%) | 1.30 | (1.02–1.66) | 0.037 | |||
| No. of antihypertensives vs. no. medication | ||||||
| 1 | 0.64 | (0.20–2.05) | 0.448 | |||
| 2 | 0.73 | (0.23–2.27) | 0.583 | |||
| >2 | 0.5 | (0.19–1.33) | 0.164 | |||
| Type of antidiabetic vs. diet | ||||||
| Tablets | 0.22 | (0.02–2.29) | 0.206 | |||
| Insulin | 0.21 | (0.18–2.47) | 0.215 | |||
| Oral agents and Insulin | 0.5 | (0.04–5.40) | 0.568 | |||
| ABPM dipping | ||||||
| Non-dippers vs. dippers | 3.14 | (1.19–8.24) | 0.02 | 3.93 | (1.33–11.64) | 0.013 |
| Reverse dippers | 1.69 | (0.59–4.88) | 0.331 | 1.74 | (0.54–5.65) | 0.354 |
| ABPM status | ||||||
| Hypertensives vs. Normotensives | 1.43 | (0.64–3.20) | 0.386 | |||
| 24 h SBP | 1.02 | (0.99–1.06) | 0.177 | |||
| 24 h DBP | 1.07 | (1.00–1.13) | 0.022 | |||
| Daytime SBP | 1.02 | (0.98–1.05) | 0.397 | |||
| Daytime DBP | 1.05 | (0.99–1.11) | 0.11 | |||
| Nighttime SBP | 1.03 | (1.00–1.06) | 0.042 | |||
| Nighttime DBP | 1.06 | (1.01–1.12) | 1,012 | |||
| 24 h-Hypertension stages | ||||||
| <120/<80 | Reference category | Reference category | ||||
| 120–129 and/80–84 | 1.08 | (0.41–2.82) | 0.874 | 0.89 | (0.30–2.69) | 0.848 |
| 130–139 or /85–89 | 1.55 | (0.32–5.32) | 0.405 | 0.95 | (0.29–3.14) | 0.932 |
| 140 or /90 | 1.31 | (0.32–5.32) | 0.703 | 1.18 | (0.23–5.99) | 0.843 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ntavidi, S.; Katsanou, P.; Marakomichelakis, G.; Kasdagli, M.-I.; Antiochou, E.; Mpali, I.; Kakou, A.-M.; Tsioufis, K.; Dimitriadis, G.; Lambadiari, V. Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece. Nutrients 2023, 15, 72. https://doi.org/10.3390/nu15010072
Ntavidi S, Katsanou P, Marakomichelakis G, Kasdagli M-I, Antiochou E, Mpali I, Kakou A-M, Tsioufis K, Dimitriadis G, Lambadiari V. Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece. Nutrients. 2023; 15(1):72. https://doi.org/10.3390/nu15010072
Chicago/Turabian StyleNtavidi, Styliani, Panagiota Katsanou, George Marakomichelakis, Maria-Iosifina Kasdagli, Eleni Antiochou, Ioulia Mpali, Anda-Monica Kakou, Konstantinos Tsioufis, George Dimitriadis, and Vaia Lambadiari. 2023. "Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece" Nutrients 15, no. 1: 72. https://doi.org/10.3390/nu15010072
APA StyleNtavidi, S., Katsanou, P., Marakomichelakis, G., Kasdagli, M.-I., Antiochou, E., Mpali, I., Kakou, A.-M., Tsioufis, K., Dimitriadis, G., & Lambadiari, V. (2023). Association of Non-Dipping Blood Pressure Patterns with Diabetic Peripheral Neuropathy: A Cross-Sectional Study among a Population with Diabetes in Greece. Nutrients, 15(1), 72. https://doi.org/10.3390/nu15010072







