Associations between Sociodemographic Factors, Lifestyle Behaviors, Pregnancy-Related Determinants, and Mediterranean Diet Adherence among Pregnant Women: The GESTAFIT Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Sociodemographic Factors
2.3. Maternal Anthropometry and Body Composition
2.4. Physical Activity Levels
2.5. Physical Fitness Tests
2.6. Clustered Physical Fitness
2.7. Dietary Assessment
2.8. Statistical Analysis
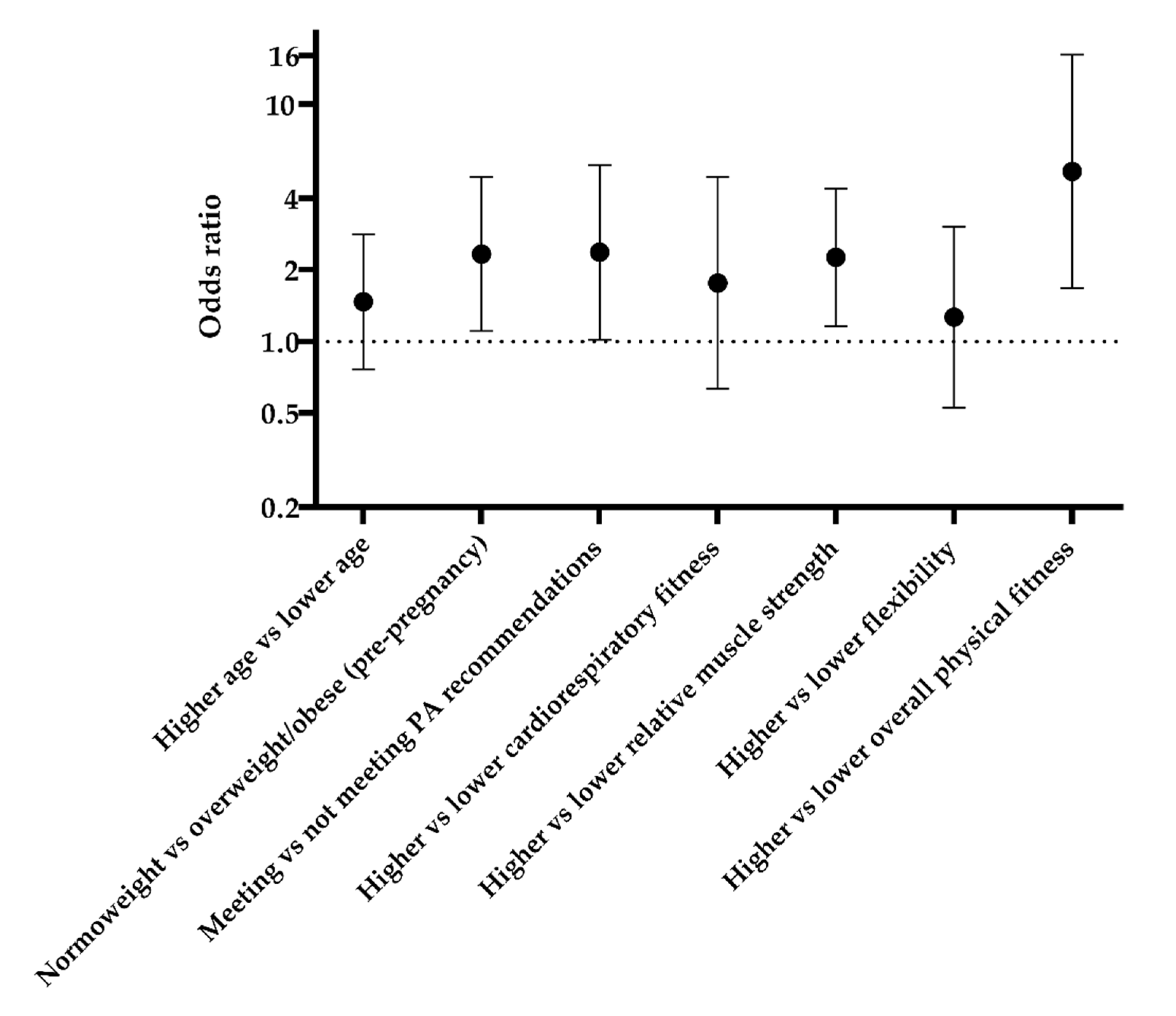
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wesolowska, E.; Jankowska, A.; Trafalska, E.; Kaluzny, P.; Grzesiak, M.; Dominowska, J.; Hanke, W.; Calamandrei, G.; Polanska, K. Sociodemographic, Lifestyle, Environmental and Pregnancy-Related Determinants of Dietary Patterns during Pregnancy. Int. J. Environ. Res. Public Health 2019, 16, 754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramakrishnan, U.; Grant, F.; Goldenberg, T.; Zongrone, A.; Martorell, R. Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: A systematic review. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. S1), 285–301. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, D.; Mao, X.; Xia, Y.; Baker, P.N.; Zhang, H. Maternal dietary patterns and pregnancy outcome. Nutrients 2016, 8, 351. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean Diet and Health Status: Meta-Analysis. BMJ Br. Med. J. 2008, 337, 673–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Biagi, C.; Nunzio, M.D.; Bordoni, A.; Gori, D.; Lanari, M. Effect of Adherence to Mediterranean Diet during Pregnancy on Children’s Health: A Systematic Review. Nutrients 2019, 11, 997. [Google Scholar] [CrossRef] [Green Version]
- Al Wattar, B.H.; Dodds, J.; Placzek, A.; Beresford, L.; Spyreli, E.; Moore, A.; Gonzalez Carreras, F.J.; Austin, F.; Murugesu, N.; Roseboom, T.J.; et al. Mediterranean-style diet in pregnant women with metabolic risk factors (ESTEEM): A pragmatic multicentre randomised trial. PLoS Med. 2019, 16, e1002857. [Google Scholar] [CrossRef]
- Timmermans, S.; Steegers-theunissen, R.P.M.; Vujkovic, M.; Bakker, R.; Den Breeijen, H.; Raat, H.; Russcher, H.; Lindemans, J.; Hofman, A.; Jaddoe, V.W.V.; et al. Major dietary patterns and blood pressure patterns during pregnancy: The Generation R Study. YMOB 2011, 205, 337.e1–337.e12. [Google Scholar] [CrossRef] [Green Version]
- Timmermans, S.; Steegers-Theunissen, R.P.; Vujkovic, M.; den Breeijen, H.; Russcher, H.; Lindemans, J.; Mackenbach, J.; Hofman, A.; Lesaffre, E.E.; Jaddoe, V.V.; et al. The Mediterranean diet and fetal size parameters: The Generation R Study. Br. J. Nutr. 2012, 108, 1399–1409. [Google Scholar] [CrossRef] [Green Version]
- Brantsæter, A.L.; Haugen, M.; Myhre, R.; Sengpiel, V.; Englund-Ögge, L.; Nilsen, R.M.; Borgen, I.; Duarte-Salles, T.; Papadopoulou, E.; Vejrup, K. Diet matters, particularly in pregnancy-results from MoBa studies of maternal diet and pregnancy outcomes. Nor. Epidemiol. 2014, 24, 63–77. [Google Scholar] [CrossRef] [Green Version]
- Vujkovic, M.; Steegers, E.A.; Looman, C.W.; Ocké, M.C.; Van Der Spek, P.J.; Steegers-Theunissen, R.P. The maternal Mediterranean dietary pattern is associated with a reduced risk of spina bifida in the offspring. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Amati, F.; Hassounah, S.; Swaka, A. The Impact of Mediterranean Dietary Patterns During Pregnancy on Maternal and Offspring Health. Nutrients 2019, 11, 1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chatzi, L.; Rifas-Shiman, S.L.; Georgiou, V.; Joung, K.E.; Koinaki, S.; Chalkiadaki, G.; Margioris, A.; Sarri, K.; Vassilaki, M.; Vafeiadi, M.; et al. Adherence to the Mediterranean diet during pregnancy and offspring adiposity and cardiometabolic traits in childhood. Pediatr. Obes. 2017, 12 (Suppl. S1), 47–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jardí, C.; Aparicio, E.; Bedmar, C.; Aranda, N.; Abajo, S.; March, G.; Basora, J.; Arija, V.; the ECLIPSES Study Group. Food Consumption during Pregnancy and Post-Partum. ECLIPSES Study. Nutrients 2019, 11, 2447. [Google Scholar] [CrossRef] [Green Version]
- Aparicio, V.A.; Ocon, O.; Padilla-Vinuesa, C.; Soriano-Maldonado, A.; Romero-Gallardo, L.; Borges-Cosic, M.; Coll-Risco, I.; Ruiz-Cabello, P.; Acosta-Manzano, P.; Estevez-Lopez, F.; et al. Effects of supervised aerobic and strength training in overweight and grade I obese pregnant women on maternal and foetal health markers: The GESTAFIT randomized controlled trial. BMC Pregnancy Childbirth 2016, 16, 290. [Google Scholar] [CrossRef] [Green Version]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef]
- Ruiz, J.R.; España-Romero, V.; Ortega, F.B.; Sjöström, M.; Castillo, M.J.; Gutierrez, A. Hand span influences optimal grip span in male and female teenagers. J. Hand Surg. Am. 2006, 31, 1367–1372. [Google Scholar] [CrossRef]
- Lawman, H.G.; Troiano, R.P.; Perna, F.M.; Wang, C.-Y.; Fryar, C.D.; Ogden, C.L. Associations of Relative Handgrip Strength and Cardiovascular Disease Biomarkers in U.S. Adults, 2011–2012. Am. J. Prev. Med. 2016, 50, 677–683. [Google Scholar] [CrossRef]
- Mataix, J.L.; de Victoria, E.M.; Montellano, M.A.; Lopez, M.; Aranda, P.L. Valoración del Estado Nutricional de la Comunidad Autónoma de Andalucía; Consejería de Salud de la Junta de Andalucía: Sevilla, Spain, 2000. [Google Scholar]
- Huang, W.-Q.; Lu, Y.; Xu, M.; Huang, J.; Su, Y.-X.; Zhang, C.-X. Excessive fruit consumption during the second trimester is associated with increased likelihood of gestational diabetes mellitus: A prospective study. Sci. Rep. 2017, 7, 43620. [Google Scholar] [CrossRef] [Green Version]
- Flor-Alemany, M.; Nestares, T.; Alemany-Arrebola, I.; Marín-Jiménez, N.; Aparicio, V.A. Influence of Dietary Habits and Mediterranean Diet Adherence on Sleep Quality during Pregnancy. The GESTAFIT Project. Nutrients 2020, 12, 3569. [Google Scholar] [CrossRef] [PubMed]
- Papazian, T.; Serhal, A.; Hout, H.; Younes, H.; Tayeh, G.A.; Azouri, J.; Moussa Lteif, F.H.; Kesrouani, A.; Khabbaz, L.R. Discrepancies among different tools evaluating Mediterranean diet adherence during pregnancy, correlated to maternal anthropometric, dietary and biochemical characteristics. Clin. Nutr. 2019, 38, 1398–1405. [Google Scholar] [CrossRef] [PubMed]
- Villar-Vidal, M.; Amiano, P.; Rodriguez-Bernal, C.; Santa Marina, L.; Mozo, I.; Vioque, J.; Navarrete-Munoz, E.M.; Romaguera, D.; Valvi, D.; Fernandez Samoano, A.; et al. Compliance of nutritional recommendations of Spanish pregnant women according to sociodemographic and lifestyle characteristics: A cohort study. Nutr. Hosp. 2015, 31, 1803–1812. [Google Scholar] [CrossRef] [PubMed]
- Olmedo-Requena, R.; Gómez-Fernández, J.; Amezcua-Prieto, C.; Mozas-Moreno, J.; Khan, K.S.; Jiménez-Moleón, J.J. Pre-Pregnancy Adherence to the Mediterranean Diet and Gestational Diabetes Mellitus: A Case-Control Study. Nutrients 2019, 11, 1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, I.-M.; Borrmann, B.; Grosser, A.; Razum, O.; Spallek, J. Determinants of dietary patterns and diet quality during pregnancy: A systematic review with narrative synthesis. Public Health Nutr. 2017, 20, 1009–1028. [Google Scholar] [CrossRef]
- Laraia, B.A.; Bodnar, L.M.; Siega-Riz, A.M. Pregravid body mass index is negatively associated with diet quality during pregnancy. Public Health Nutr. 2007, 10, 920–926. [Google Scholar] [CrossRef] [Green Version]
- Pinto, E.; Barros, H.; dos Santos Silva, I. Dietary intake and nutritional adequacy prior to conception and during pregnancy: A follow-up study in the north of Portugal. Public Health Nutr. 2009, 12, 922–931. [Google Scholar] [CrossRef] [Green Version]
- Cucó, G.; Fernández-Ballart, J.; Sala, J.; Viladrich, C.; Iranzo, R.; Vila, J.; Arija, V. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur. J. Clin. Nutr. 2006, 60, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Olmedo-Requena, R.; Gómez-Fernández, J.; Mozas-Moreno, J.; Lewis-Mikhael, A.-M.; Bueno-Cavanillas, A.; Jiménez-Moleón, J.-J. Factors associated with adherence to nutritional recommendations before and during pregnancy. Women Health 2018, 58, 1094–1111. [Google Scholar] [CrossRef]
- Crozier, S.R.; Robinson, S.M.; Borland, S.E.; Godfrey, K.M.; Cooper, C.; Inskip, H.M.; Group, S.W.S.S. Do women change their health behaviours in pregnancy? Findings from the Southampton Women’s Survey. Paediatr. Perinat. Epidemiol. 2009, 23, 446–453. [Google Scholar] [CrossRef] [Green Version]
- Crozier, S.R.; Robinson, S.M.; Godfrey, K.M.; Cooper, C.; Inskip, H.M. Women’s Dietary Patterns Change Little from Before to During Pregnancy. J. Nutr. 2009, 139, 1956–1963. [Google Scholar] [CrossRef] [PubMed]
- Galobardes, B.; Morabia, A.; Bernstein, M.S. Diet and socioeconomic position: Does the use of different indicators matter? Int. J. Epidemiol. 2001, 30, 334–340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maugeri, A.; Barchitta, M.; Agrifoglio, O.; Favara, G.; La Mastra, C.; La Rosa, M.C.; Magnano San Lio, R.; Panella, M.; Cianci, A.; Agodi, A. The impact of social determinants and lifestyles on dietary patterns during pregnancy: Evidence from the “Mamma & Bambino” study. Ann. Ig. 2019, 31, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Olmedo-Requena, R.; Fernández, J.G.; Prieto, C.A.; Moreno, J.M.; Bueno-Cavanillas, A.; Jiménez-Moleón, J.J. Factors associated with a low adherence to a Mediterranean diet pattern in healthy Spanish women before pregnancy. Public Health Nutr. 2014, 17, 648–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Entrala-Bueno, A.; Iglesias, C.; de Jesús, F. Diet and physical activity: A healthful binomial. Eur. J. Clin. Nutr. 2003, 57 (Suppl. S1), S63–S65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savard, C.; Lemieux, S.; Carbonneau, É.; Provencher, V.; Gagnon, C.; Robitaille, J.; Morisset, A.-S. Trimester-Specific Assessment of Diet Quality in a Sample of Canadian Pregnant Women. Int. J. Environ. Res. Public Health 2019, 16, 311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maugeri, A.; Barchitta, M.; Fiore, V.; Rosta, G.; Favara, G.; La Mastra, C.; La Rosa, M.C.; Magnano San Lio, R.; Agodi, A. Determinants of Adherence to the Mediterranean Diet: Findings from a Cross-Sectional Study in Women from Southern Italy. Int. J. Environ. Res. Public Health 2019, 16, 2963. [Google Scholar] [CrossRef] [Green Version]
- Baena-García, L.; Coll-Risco, I.; Ocón-Hernández, O.; Romero-Gallardo, L.; Acosta-Manzano, P.; May, L.; Aparicio, V.A. Association of objectively measured physical fitness during pregnancy with maternal and neonatal outcomes. The GESTAFIT Project. PLoS ONE 2020, 15, e0229079. [Google Scholar] [CrossRef] [Green Version]
- Eslami, O.; Zarei, M.; Shidfar, F. The association of dietary patterns and cardiorespiratory fitness: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1442–1451. [Google Scholar] [CrossRef]
- Shikany, J.M.; Jacobs, D.R., Jr.; Lewis, C.E.; Steffen, L.M.; Sternfeld, B.; Carnethon, M.R.; Richman, J.S. Associations between food groups, dietary patterns, and cardiorespiratory fitness in the Coronary Artery Risk Development in Young Adults study. Am. J. Clin. Nutr. 2013, 98, 1402–1409. [Google Scholar] [CrossRef] [Green Version]
- Román, G.C.; Jackson, R.E.; Gadhia, R.; Román, A.N.; Reis, J. Mediterranean diet: The role of long-chain ω-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and Alzheimer disease. Rev. Neurol. 2019, 175, 724–741. [Google Scholar] [CrossRef] [PubMed]
- Talegawkar, S.A.; Bandinelli, S.; Bandeen-Roche, K.; Chen, P.; Milaneschi, Y.; Tanaka, T.; Semba, R.D.; Guralnik, J.M.; Ferrucci, L. A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J. Nutr. 2012, 142, 2161–2166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Billingsley, H.E.; Rodriguez-Miguelez, P.; Del Buono, M.G.; Abbate, A.; Lavie, C.J.; Carbone, S. Lifestyle Interventions with a Focus on Nutritional Strategies to Increase Cardiorespiratory Fitness in Chronic Obstructive Pulmonary Disease, Heart Failure, Obesity, Sarcopenia, and Frailty. Nutrients 2019, 11, 2849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cicero, A.F.G.; Ertek, S.; Borghi, C. Omega-3 polyunsaturated fatty acids: Their potential role in blood pressure prevention and management. Curr. Vasc. Pharmacol. 2009, 7, 330–337. [Google Scholar] [CrossRef] [Green Version]
- Romagnolo, D.F.; Selmin, O.I. Mediterranean Diet and Prevention of Chronic Diseases. Nutr. Today 2017, 52, 208–222. [Google Scholar] [CrossRef] [Green Version]
- Wu, F.; Wills, K.; Laslett, L.L.; Oldenburg, B.; Jones, G.; Winzenberg, T. Associations of dietary patterns with bone mass, muscle strength and balance in a cohort of Australian middle-aged women. Br. J. Nutr. 2017, 598–606. [Google Scholar] [CrossRef] [Green Version]
- Marqueta, P.M.; Bonafonte, L.F.; Orellana, J.N.; Cuixart, D.B.; Nogués, J.C.; Soto, C.C.; de Teresa Galván, C.; del Valle Soto, M.; Ruiz, V.E.; Canales, M.G. Pruebas de esfuerzo en medicina del deporte. Documento de consenso de la Sociedad Española de Medicina del Deporte (SEMED-FEMEDE). Arch. Med. Deporte Rev. Fed. Esp. Med. Deporte Confed. Iberoam. Med. Deporte 2016, 33, 5–83. [Google Scholar]
- Acosta-Manzano, P.; Segura-Jiménez, V.; Coll-Risco, I.; Borges-Cosic, M.; Castro-Piñero, J.; Delgado-Fernández, M.; Aparicio, V.A. Association of sedentary time and physical fitness with ideal cardiovascular health in perimenopausal women: The FLAMENCO project. Maturitas 2019, 120, 53–60. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
| All Women (n = 152) | Low MD Adherence (n = 89) | High MD Adherence (n = 63) | p | |
|---|---|---|---|---|
| Age (years) | 32.9 (4.6) | 32.2 (4.4) | 33.9 (4.7) | 0.022 |
| Pre-pregnancy BMI (kg/m2) (n = 81 vs. 57) | 24.9 (4.2) | 24.9 (4.5) | 23.2 (3.7) | 0.020 |
| Physical activity (n = 72 vs. 60) | ||||
| Sedentary time (min/day) | 514.0 (91.5) | 509.1 (93.0) | 519.8 (90.0) | 0.509 |
| Moderate-to-vigorous physical activity (min/day) | 36.4 (20.8) | 33.2 (20.7) | 40.3 (20.5) | 0.054 |
| Total physical activity (min/day) | 423.7 (88.9) | 411.8 (90.5) | 437.9 (85.4) | 0.092 |
| Physical fitness | ||||
| Cardiorespiratory fitness (m) (n = 37 vs. 25) | 605.7 (48.1) | 590.8 (44.2) | 627.7 (45.8) | 0.002 |
| Relative muscle strength (kg/body weight) (n = 89 vs. 60) | 0.414 (0.08) | 0.402 (0.08) | 0.431 (0.07) | 0.021 |
| Flexibility (cm) (n = 89 vs. 61) | 3.9 (6.0) | 3.1 (6.2) | 5.2 (5.3) | 0.032 |
| Overall physical fitness (Z-score) (n = 37 vs. 25) | 0.1 (0.7) | −0.2 (0.6) | 0.5 (0.5) | <0.001 |
| Miscarriages n (%) | ||||
| No | 63 (41.4) | 39 (43.8) | 24 (38.1) | 0.480 |
| Yes | 89 (58.6) | 50 (56.2) | 39 (61.9) | |
| Parity n (%) | ||||
| Nullipara | 91 (59.9) | 52 (58.4) | 39 (61.9) | 0.667 |
| Primipara | 61 (40.1) | 37 (41.6) | 24 (38.1) | |
| Marital status n (%) | ||||
| Non-married | 62 (40.8) | 34 (22.4) | 28 (18.4) | 0.440 |
| Married | 90 (59.2) | 55 (61.8) | 35 (55.6) | |
| Educational level n (%) | ||||
| No university studies | 62 (40.8) | 41 (46.1) | 21 (33.3) | 0.116 |
| University studies | 90 (59.2) | 48 (53.9) | 42 (66.7) | |
| Working status n (%) | ||||
| Unemployed | 48 (31.6) | 31 (34.8) | 17 (27.0) | 0.305 |
| Employed | 104 (68.4) | 58 (65.2) | 46 (73.0) | |
| Smoking habit n (%) | ||||
| No smoking | 139 (91.4) | 80 (89.9) | 59 (93.7) | 0.414 |
| Smoking | 13 (8.6) | 9 (10.1) | 4 (6.3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flor-Alemany, M.; Nestares, T.; Jiménez, N.M.; Baena-García, L.; Aparicio, V.A. Associations between Sociodemographic Factors, Lifestyle Behaviors, Pregnancy-Related Determinants, and Mediterranean Diet Adherence among Pregnant Women: The GESTAFIT Project. Nutrients 2022, 14, 1348. https://doi.org/10.3390/nu14071348
Flor-Alemany M, Nestares T, Jiménez NM, Baena-García L, Aparicio VA. Associations between Sociodemographic Factors, Lifestyle Behaviors, Pregnancy-Related Determinants, and Mediterranean Diet Adherence among Pregnant Women: The GESTAFIT Project. Nutrients. 2022; 14(7):1348. https://doi.org/10.3390/nu14071348
Chicago/Turabian StyleFlor-Alemany, Marta, Teresa Nestares, Nuria Marín Jiménez, Laura Baena-García, and Virginia A. Aparicio. 2022. "Associations between Sociodemographic Factors, Lifestyle Behaviors, Pregnancy-Related Determinants, and Mediterranean Diet Adherence among Pregnant Women: The GESTAFIT Project" Nutrients 14, no. 7: 1348. https://doi.org/10.3390/nu14071348
APA StyleFlor-Alemany, M., Nestares, T., Jiménez, N. M., Baena-García, L., & Aparicio, V. A. (2022). Associations between Sociodemographic Factors, Lifestyle Behaviors, Pregnancy-Related Determinants, and Mediterranean Diet Adherence among Pregnant Women: The GESTAFIT Project. Nutrients, 14(7), 1348. https://doi.org/10.3390/nu14071348