Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps
Abstract
:1. Introduction
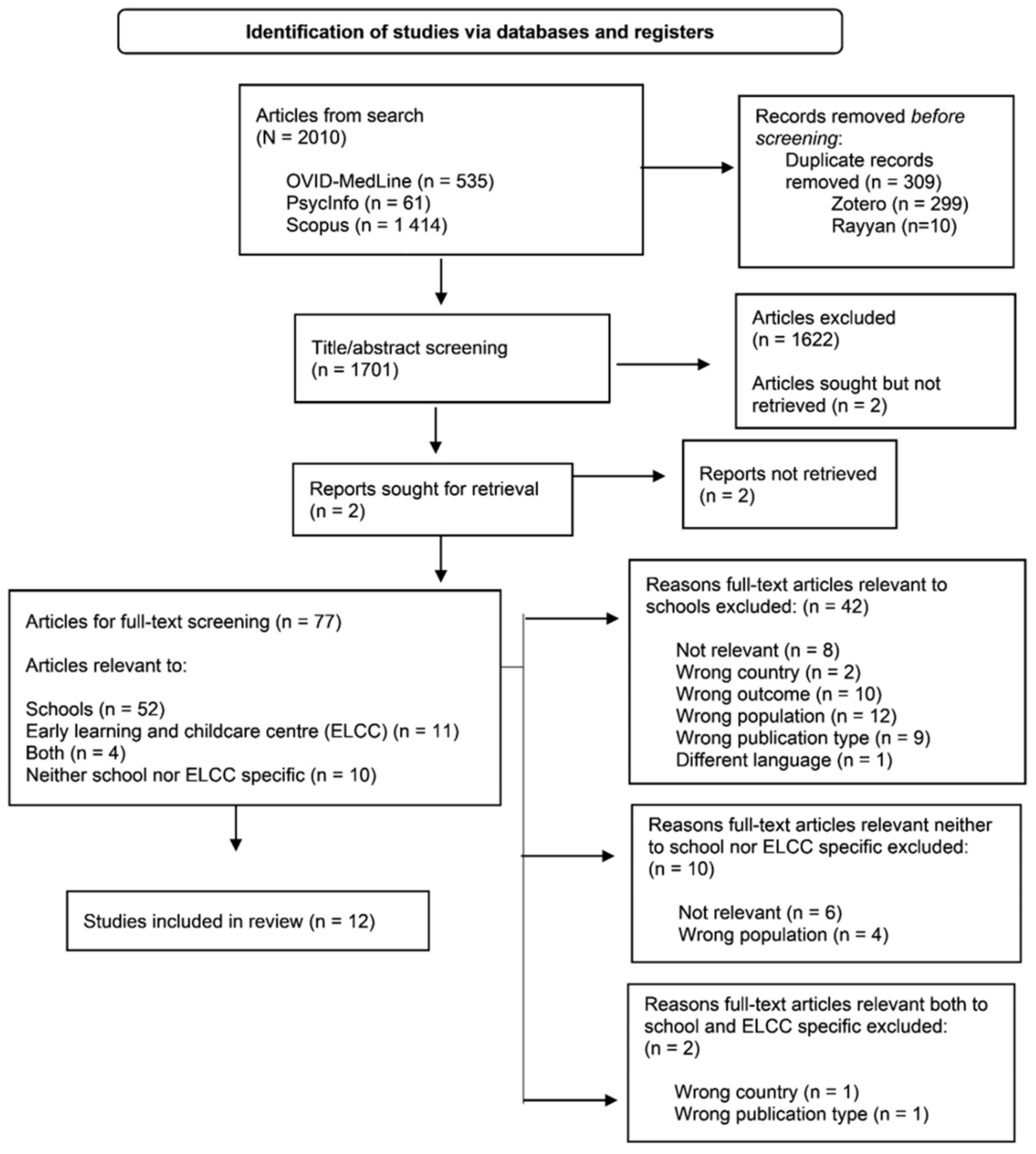
2. Materials and Methods
3. Results
3.1. Previous Experience in Food Allergy Management
3.2. Baseline Knowledge
3.3. In-School Emergency Preparedness
3.4. School-Based Policies and Guidelines
3.5. Post-Educational Intervention Knowledge
3.6. Future Educational Needs
4. Discussion
- Teachers and school staff play a pivotal role in emergency response.
- At baseline, teachers and school staff have poor and variable knowledge and experience of food allergy.
- Teachers and school staff may benefit from standardized, annual food allergy training.
- Key elements of food allergy training may include epinephrine auto-injector (EAI) administration, causal foods, signs and symptoms of a reaction, and importance and usage of a emergency anaphylaxis plans (EAP).
- Implementation of EAP for all students with a food allergy and having stock EAI, in conjunction with annual training will improve student safety and schools’ emergency preparedness.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Clarke, A.E.; Elliott, S.J.; St Pierre, Y.; Soller, L.; La Vieille, S.; Ben-Shoshan, M. Temporal trends in prevalence of food allergy in Canada. J. Allergy Clin. Immunol. Pract. 2020, 8, 1428–1430.e5. [Google Scholar] [CrossRef] [PubMed]
- Venkataraman, D.; Erlewyn-Lajeunesse, M.; Kurukulaaratchy, R.J.; Potter, S.; Roberts, G.; Matthews, S.; Arshad, S.H. Prevalence and longitudinal trends of food allergy during childhood and adolescence: Results of the Isle of Wight Birth Cohort study. Clin. Exp. Allergy 2018, 48, 394–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R.S.; Springston, E.E.; Warrier, M.R.; Smith, B.; Kumar, R.; Pongracic, J.; Holl, J.L. The Prevalence, Severity, and Distribution of Childhood Food Allergy in the United States. Pediatrics 2011, 128, e9–e17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rona, R.; Keil, T.; Summers, C.; Gislason, D.; Zuidmeer-Jongejan, L.; Sodergren, E.; Sigurdardottir, S.T.; Lindner, T.; Goldhahn, K.; Dahlstrom, J.; et al. The prevalence of food allergy: A meta-analysis. J. Allergy Clin. Immunol. 2007, 120, 638–646. [Google Scholar] [CrossRef]
- Fraser Institute. Available online: https://www.fraserinstitute.org/studies/secondary-school-class-sizes-and-student-performance-in-canada (accessed on 6 October 2021).
- Boyce, J.A.; Assa’Ad, A.; Burks, A.W.; Jones, S.M.; Sampson, H.A.; Wood, R.A.; Plaut, M.; Cooper, S.F.; Fenton, M.J.; Arshad, S.H.; et al. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J. Allergy Clin. Immunol. 2010, 126, S1–S58. [Google Scholar] [CrossRef]
- Sampson, H.A.; Muñoz-Furlong, A.; Campbell, R.; Adkinson, N.F.; Bock, S.A.; Branum, A.; Brown, S.; Camargo, C.A.; Cydulka, R.; Galli, S.J.; et al. Second symposium on the definition and management of anaphylaxis: Summary report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J. Allergy Clin. Immunol. 2006, 117, 391–397. [Google Scholar] [CrossRef]
- Worm, M.; Moneret-Vautrin, A.; Scherer, K.; Lang, R.; Fernandez-Rivas, M.; Cardona, V.; Kowalski, M.L.; Jutel, M.; Poziomkowska-Gesicka, I.; Papadopoulos, N.; et al. First European data from the network of severe allergic reactions (NORA). Allergy 2014, 69, 1397–1404. [Google Scholar] [CrossRef]
- Umasunthar, T.; Leonardi-Bee, J.; Turner, P.J.; Hodes, M.; Gore, C.; Warner, J.O.; Boyle, R.J. Incidence of food anaphylaxis in people with food allergy: A systematic review and meta-analysis. Clin. Exp. Allergy 2015, 45, 1621–1636. [Google Scholar] [CrossRef] [Green Version]
- Panesar, S.S.; Javad, S.; De Silva, D.; Nwaru, B.I.; Hickstein, L.; Muraro, A.; Roberts, G.; Worm, M.; Bilò, M.B.; Cardona, V.; et al. The epidemiology of anaphylaxis in Europe: A systematic review. Allergy 2013, 68, 1353–1361. [Google Scholar] [CrossRef]
- Waserman, S.; Cruickshank, H.; Hildebrand, K.J.; Mack, D.; Bantock, L.; Bingemann, T.; Chu, D.K.; Cuello-Garcia, C.; Ebisawa, M.; Fahmy, D.; et al. Prevention and management of allergic reactions to food in child care centers and schools: Practice guidelines. J. Allergy Clin. Immunol. 2021, 147, 1561–1578. [Google Scholar] [CrossRef]
- Alqurashi, W.; Stiell, I.; Chan, K.; Neto, G.; Alsadoon, A.; Wells, G. Epidemiology and clinical predictors of biphasic reactions in children with anaphylaxis. Ann. Allergy Asthma Immunol. 2015, 115, 217–223.e2. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, L. Administration of Epinephrine for Life-Threatening Allergic Reactions in School Settings. Pediatrics 2005, 116, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Pulcini, J.M.; Sease, K.K.; Marshall, G.D. Disparity between the presence and absence of food allergy action plans in one school district. Allergy Asthma Proc. 2010, 31, 141–146. [Google Scholar] [CrossRef]
- Sicherer, S.H.; Furlong, T.J.; DeSimone, J.; Sampson, H.A. The US Peanut and Tree Nut Allergy Registry: Characteristics of reactions in schools and day care. J. Pediatrics 2001, 138, 560–565. [Google Scholar] [CrossRef]
- Pouessel, G.; Lejeune, S.; Dupond, M.-P.; Renard, A.; Fallot, C.; Deschildre, A. Individual healthcare plan for allergic children at school: Lessons from a 2015-2016 school year survey. Pediatric Allergy Immunol. 2017, 28, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Alberta Laws. Available online: https://docs.assembly.ab.ca/LADDAR_files/docs/bills/bill/legislature_30/session_1/20190521_bill-201.pdf (accessed on 22 February 2021).
- Ontario Laws. Available online: https://www.ontario.ca/laws/statute/05s07?_ga=2.97067992.650686573.1614619401-1441028624.1614013729 (accessed on 22 February 2021).
- Food Allergy Canada. Available online: https://foodallergycanada.ca/professional-resources/educators/school-k-to-12/national-school-policies/ (accessed on 18 September 2021).
- Winnipeg School Division. Available online: https://sbwsdstor.blob.core.windows.net/media/Default/medialib/march-19-2018.e6937d15056.pdf (accessed on 18 September 2021).
- Ben-Shoshan, M.; Kagan, R.; Primeau, M.-N.; Alizadehfar, R.; Verreault, N.; Yu, J.W.; Nicolas, N.; Joseph, L.; Turnbull, E.; Dufresne, C.; et al. Availability of the epinephrine autoinjector at school in children with peanut allergy. Ann. Allergy Asthma Immunol. 2008, 100, 570–575. [Google Scholar] [CrossRef]
- Shah, S.S.; Parker, C.L.; O’Brian Smith, E.; Davis, C.M. Disparity in the availability of injectable epinephrine in a large, diverse US school district. J. Allergy Clin. Immunol. Pract. 2014, 2, 288–293.e1. [Google Scholar] [CrossRef] [PubMed]
- Hogue, S.L.; Muniz, R.; Herrem, C.; Silvia, S.; White, M.V. Barriers to the Administration of Epinephrine in Schools. J. Sch. Health 2018, 88, 396–404. [Google Scholar] [CrossRef]
- Miles, L.M.; Ratnarajah, K.; Gabrielli, S.; Abrams, E.M.; Protudjer, J.L.; Bégin, P.; Chan, E.S.; Upton, J.; Waserman, S.; Watson, W.; et al. Community Use of Epinephrine for the Treatment of Anaphylaxis: A Review and Meta-Analysis. J. Allergy Clin. Immunol. Pract. 2021, 9, 2321–2333. [Google Scholar] [CrossRef]
- Tsuang, A.; Demain, H.; Patrick, K.; Pistiner, M.; Wang, J. Epinephrine use and training in schools for food-induced anaphylaxis among non-nursing staff. J. Allergy Clin. Immunol. Pract. 2017, 5, 1418–1420.e3. [Google Scholar] [CrossRef]
- Carlisle, S.K.; Vargas, P.A.; Noone, S.; Steele, P.; Sicherer, S.H.; Burks, A.W.; Jones, S.M. Food Allergy Education for School Nurses. J. Sch. Nurs. 2010, 26, 360–367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hui, J.W.; Copeland, M.; Lanser, B.J. Food Allergy Management at School in the Era of Immunotherapy. Curr. Allergy Asthma Rep. 2020, 20, 32. [Google Scholar] [CrossRef]
- Vale, S.; Smith, J.; Said, M.; Mullins, R.J.; Loh, R. ASCIA guidelines for prevention of anaphylaxis in schools, pre-schools and childcare: 2015 update. J. Paediatr. Child Health 2015, 51, 949–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- Lawlis, T.; Bakonyi, S.; Williams, L.T. Food allergy in schools: The importance of government involvement. Nutr. Diet. 2017, 74, 82–87. [Google Scholar] [CrossRef]
- Polloni, L.; Baldi, I.; Lazzarotto, F.; Bonaguro, R.; Toniolo, A.; Celegato, N.; Gregori, D.; Muraro, A. School personnel’s self-efficacy in managing food allergy and anaphylaxis. Pediatr. Allergy Immunol 2016, 27, 356–360. [Google Scholar] [CrossRef]
- Canon, N.; Gharfeh, M.; Guffey, D.; Anvari, S.; Davis, C.M. Role of Food Allergy Education: Measuring Teacher Knowledge, Attitudes, and Beliefs. Allergy Rhinol. 2019, 10, 2152656719856324. [Google Scholar] [CrossRef]
- Shah, S.S.; Parker, C.L.; Davis, C.M. Improvement of teacher food allergy knowledge in socioeconomically diverse schools after educational intervention. Clin. Pediatr. 2013, 52, 812–820. [Google Scholar] [CrossRef]
- Wahl, A.; Stephens, H.; Ruffo, M.; Jones, A.L. The Evaluation of a Food Allergy and Epinephrine Autoinjector Training Program for Personnel Who Care for Children in Schools and Community Settings. J. Sch. Nurs. 2015, 31, 91–98. [Google Scholar] [CrossRef]
- Eldredge, C.; Patterson, L.; White, B.; Schellhase, K. Assessing the readiness of a school system to adopt food allergy management guidelines. Wis. Med. J. 2014, 113, 155–161. [Google Scholar]
- Raptis, G.; Perez-Botella, M.; Totterdell, R.; Gerasimidis, K.; Michaelis, L.J. A survey of school’s preparedness for managing anaphylaxis in pupils with food allergy. Eur. J. Pediatr. 2020, 179, 1537–1545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozturk Haney, M.; Ozbicakci, S.; Karadag, G. Turkish teachers’ self-efficacy to manage food allergy and anaphylaxis: A psychometric testing study. Allergol. Immunopathol. 2019, 47, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Ercan, H.; Ozen, A.; Karatepe, H.; Berber, M.; Cengizlier, R. Primary school teachers’ knowledge about and attitudes toward anaphylaxis. Pediatric Allergy Immunol. 2012, 23, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Ferran, L.; Gomez Tornero, N.; Cortes Alvarez, N.; Thorndike Piedra, F. Anaphylaxis at school. Are we prepared? Could we improve? Allergol. Immunopathol. 2020, 48, 384–389. [Google Scholar] [CrossRef]
- Gonzalez-Mancebo, E.; Gandolfo-Cano, M.; Trujillo-Trujillo, M.; Mohedano-Vicente, E.; Calso, A.; Juarez, R.; Melendez, A.; Morales, P.; Pajuelo, F. Analysis of the effectiveness of training school personnel in the management of food allergy and anaphylaxis. Allergol. Immunopathol. 2019, 47, 60–63. [Google Scholar] [CrossRef]
- Ravarotto, L.; Mascarello, G.; Pinto, A.; Schiavo, M.R.; Bagni, M.; Decastelli, L. Food allergies in school: Design and evaluation of a teacher-oriented training action. Ital. J. Pediatr. 2014, 40, 100. [Google Scholar] [CrossRef] [Green Version]
- Polloni, L.; Lazzarotto, F.; Toniolo, A.; Ducolin, G.; Muraro, A. What do school personnel know, think and feel about food allergies? Clin. Transl. Allergy 2013, 3, 39. [Google Scholar] [CrossRef] [Green Version]
- Polloni, L.; Baldi, I.; Lazzarotto, F.; Bonaguro, R.; Toniolo, A.; Gregori, D.; Muraro, A. Multidisciplinary education improves school personnel’s self-efficacy in managing food allergy and anaphylaxis. Pediatr. Allergy Immunol. 2020, 31, 380–387. [Google Scholar] [CrossRef]
- Gupta, R.S.; Kim, J.S.; Springston, E.E.; Smith, B.; Pongracic, J.A.; Wang, X.; Holl, J. Food allergy knowledge, attitudes, and beliefs in the United States. Ann. Allergy Asthma Immunol. 2009, 103, 43–50. [Google Scholar] [CrossRef]
- Abrams, E.M.; Greenhawt, M. The role of peanut-free school policies in the protection of children with peanut allergy. J. Public Health Pol. 2020, 41, 2013. [Google Scholar] [CrossRef] [PubMed]
- Bartnikas, L.M.; Sheehan, W.J.; Hoffman, E.B.; Permaul, P.; Dioun, A.F.; Friedlander, J.; Baxi, S.N.; Schneider, L.C.; Phipatanakul, W. Predicting food challenge outcomes for baked milk: Role of specific IgE and skin prick testing. Ann. Allergy Asthma Immunol. 2012, 109, 309–313.e1. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
| First Author, Year | Country | Research Design | Methods | Teachers and School Staff (n) | Type of School (n) |
|---|---|---|---|---|---|
| Polloni 2013 [43] | Italy | Quasi experimental pre/post-intervention | School staff attended an educational course by the Veneto Food Allergy Center and completed pre/post surveys. | 1184 Teachers and Principals | Primary school (n = 598) Middle and high school (n = 291) |
| Polloni 2020 [44] | Italy | Quasi experimental pre/post-intervention | Teachers and school caretakers (class assistants and meal supervisors) participated in an educational intervention by the Veneto Food Allergy Center. The SPSMFAA questionnaire [32] was completed pre/post-session. | 592 Teachers (n = 474) Caretakers (n = 118) | Primary school (n = 216) Middle and high school (n = 152) |
| Ravarotto 2014 [42] | Italy | Mixed methods (Focus group, pre/post-intervention) | Phase 1: 3–90-minute focus groups of teachers informed the intervention’s communication strategy. Phase 2: Information workshop and “The Theatre of Health” show was held in various provinces. Phase 3: Teachers who attended the session completed pre/post questionnaires. | Three focus groups (n = 25 participants) Information workshop (n = 197) Assessment questionnaires (n = 158) | All primary schools. Focus groups (n = 3) Information workshops and questionnaire (n = 5) |
| Gonzalez-Mancebo 2019 [41] | Spain | Quasi experimental pre/post-intervention | “Management of Food Allergy in Children and Adolescents in School Centers” conference participants were provided an education session and a pre/post SPSMFAA questionnaire [32]. Training efficacy results between cafeteria monitors and teachers were compared. | 191 Cafeteria monitors (n = 97) Teachers (n = 46) Cooks (n = 25); Other professions (n =23) | Number of primary schools not reported |
| Rodríguez Ferran 2020 [40] | Spain | Multi-center quasi experimental pre/post-intervention | Teachers and canteen staff from three schools, as requested by patients’ family members, participated in an educational session and pre/post questionnaire. Grade-specific data were not disclosed. | 53 Teachers (n = 45) Canteen staff (n = 8) | Varied types of schools included. (n = 3) Schools had students aged 3–12y. |
| Ercan 2012 [39] | Turkey | Cross-sectional survey | Private and public-school teachers completed questionnaires, and food allergy knowledge was compared. | 237 Public school teachers (n = 91) Private school teachers (n = 146) | Number of primary schools not reported |
| Ozturk Haney 2019 [38] | Turkey | Cross-sectional survey | Private and public-school teachers participated and completed the SPSMFAA questionnaire [32]. | 282 Public school teachers (n = 169) Private school teachers (n = 113) | All primary school (n = 12), of which 4 were private and 8 were public. |
| Canon 2019 [33] | USA | Multi-center pre/post-randomized intervention | Six Houston private schools were assigned to intervention (n = 4) or control groups (n = 2). Both groups completed the Chicago Food Allergy Research Survey [45]. Intervention groups received education sessions while control groups did not, and food allergy knowledge was compared. | 375 Intervention (n = 302) Control (n = 73) | All private schools (n = 6) |
| Eldredge 2014 [36] | USA | Cross-sectional survey | Private, parochial schools participated in the survey. Electronic questionnaires were answered by principals or administrators. Grade-specific data were not disclosed. | 78 Principals (n = 70) Administrators (n = 8) | Varied types of schools included. (n = 71) 76.0% were pre-K/K-6th or 8th grade. |
| Shah 2013 [34] | USA | Multi-center pre/post- randomized intervention | One school each from higher/ lower socioeconomic areas in the Houston area were recruited. Intervention groups received education sessions while control groups did not, and food allergy knowledge was compared. | Pre-intervention (n = 195) Post-intervention (n = 131) | All public primary schools (n = 4) |
| Wahl 2015 [35] | USA | Quasi experimental pre/post- intervention | A school and community personnel training program provided education sessions and a survey. A follow-up survey was given 3–12-months post-intervention. Participants who participated in a food allergy emergency post-intervention were followed-up via phone interviews. | Primary survey (n = 4088) Secondary survey (n = 332) Phone interview (n = 21) Participant roles: Teachers (48%) Childcare providers (6%) School Aide (5%) Administrator (5%) School Nurses (2%) Other (34%) (Included camp counsellors, bus drivers, multiple of specified job titles, parents, volunteers, coaches, food service workers or no indication of job title) | Varied types of schools included. Number of primary schools not reported. |
| Raptis 2020 [37] | UK | Cross-sectional survey | All schools in the region were invited to participate in the survey. Only primary school data was presented in this study. | Specific participant roles not reported. | Primary schools (n = 157) High schools (n = 22) * |
| First Author, Year | Policies | EAP Availability | EAI Availability | Other Management Practices |
|---|---|---|---|---|
| Eldredge 2014 [36] | 71.0% of schools had some sort of guideline/policy for food allergy while 25.0% of schools had none. | 56.0% of schools required an EAP. | Not reported | 76.0% of schools needed special arrangements (i.e., peanut-free classroom, allergen-free areas or cafeteria tables, increased monitoring, physical distancing, and having special meals for students with food allergy). 57.0% of schools had handwashing guidelines. 30.0% had no food sharing policies. 58.0% had classroom project food substitution guidelines and 45.0% had cleaning surfaces with allergen contact. |
| Ercan 2012 [39] | Not reported | 6.0% of teachers, all from private schools, had available EAP. 86.0% of teachers had no EAP, and 8.0% were uncertain if EAPs were available. | Not reported | Not reported |
| Raptis 2020 [37] | 76.0% of schools had standard protocols related to allergic reactions. | 89.5% of schools reported having an EAP for students with anaphylaxis history. | 0.7% (n = 165) of students with food allergy had prescribed EAI. 45.2% of schools reported their students at risk of anaphylaxis carried an EAI. | Schools had guidelines for: staff food handling guidelines (79.0%), special mealtime supervision (49.0%), no food sharing policy (63.0%), no utensil sharing policy (45.0%), aware of food packaging regulations (66.0%), reviewed curriculum to remove allergen foods (68.0%), and no eating on transportation policy (48.0%), communication systems during emergencies (94.1%), identifying staff roles (82.1%), documenting staff emergency response (81.9%), and preparing for allergic reactions in students without prior allergic history (60.7%). |
| Rodriguez Ferran 2020 [40] | Not reported | 83.0% of teachers and school staff reported they had EAP. | 66.0% of teachers and school staff knew where EAI was in their school. | 56.0% of teachers and school staff had meetings with parents/guardians of students with food allergy in their care. |
| Shah 2013 [34] | Not reported | Not reported | Schools in economically-disadvantaged areas had 1 EAI each. Schools in economically-advantaged areas had 6 and 9 EAI each. | Not reported |
| First Author, Year, Country | Intervention and Session Topics | Key Intervention Outcomes |
| Canon 2019 [33] USA | 1-hour education session with HCP Sessions taught case scenarios, common food allergens, routes of exposure, reaction recognition and prevention, epinephrine administration, importance of EAP, bullying of students with food allergy and classroom protocols. | Intervention group had higher post-intervention survey scores compared to controls (95% CI = 16.62–22.53; p < 0.001) and their pre-test surveys (95% CI = 18.17–21.38; p < 0.001). Intervention vs control group post-intervention were more likely to recognizing food allergy as life-threatening and agree that children with food allergy were treated differently and bullied (p < 0.001), 5 times more likely to acknowledge food avoidance is hard (p = 0.003) and 874 times more likely to agree that EAI is an important lifesaving measure and use it in an emergency (p = 0.173). |
| Gonzalez-Mancebo 2019 [41] Spain | Education session and EAI workshop for school staff included practical EAI training. Sessions taught food allergy definition, diagnosis, problems of children with food allergy in school settings, allergic reaction recognition and prevention measures, coordination of care, anaphylaxis treatment and, and EAP discussion | Significant improvements in SPSMFAA questionnaire [32] mean scores were observed (p < 0.05). The largest pre-post mean score difference was in managing allergen avoidance (mean = 4.29, SD = 0.98 vs. mean = 4.51, SD = 0.72). The smallest difference was in administering drugs (e.g., EAI) to a student having a severe and sudden reaction (mean = 3.08, SD = 1.41 vs. mean = 4.51, SD = 0.84). Case study scores also improved from pre- post intervention (25.5% vs 96.9%, respectively). |
| Polloni 2013 [43] Italy | 2-hour session with a pediatric allergist, dietician, psychologist, and a lawyer. Session topics were not specified. | Primary school teachers scored higher than nursery or high schools (F-value: 13.450, df = 2, p < 0.001). Mean scores significantly increased from pre-post-intervention. From pre-post-intervention, more participants thought anaphylaxis could be managed in schools (82.6% vs. 96.5%, respectively; p < 0.001) and is school staff responsibility (82.8% vs. 93.9%, respectively; p < 0.001). Feelings related to food allergy management were concern (66.9%), anxiety (15.8%), fear (3.7%) and helplessness (7.0%). |
| Polloni 2020 [44] Italy | 2-hour session with an allergist, psychologist, and a lawyer. Practical EAI training was included. Sessions taught description of allergic mechanisms, signs and symptoms, prevention and treatment, explanation of EAPs and presentation of national and regional regulations on food allergy-related drug administration in schools and discussions on food allergy-related psychosocial and emotional issues. | Improvements in SPSMFAA questionnaire [32] mean scores were observed. Post–pre score differences in anaphylaxis management (0.67–1.67, respectively), was higher than food allergy management difference (0.2–1.0, respectively). The largest pre-post mean SPSMFAA [32] score difference was in administering drugs (e.g., EAI) to a student having a severe and sudden reaction (mean = 1.3) and the lowest in guaranteeing students with food allergy full participation to all school activities (mean = 0.47). Median scores increased, as evaluated through conditional regression, from pre-post-intervention (<17 to 25, respectively), independent of all other covariates (type of job, age, school, gender, previous anaphylaxis and food allergy knowledge, training, and experience). |
| Ravarotto 2014 [42] Italy | 2-hour workshop with allergist or pediatrician, a veterinarian, and a scientific communication expert. Sessions taught common allergenic foods, difference between allergy and intolerance, allergic reaction signs and symptoms, first aid introduction, available training tools/ resources and regulations to protect consumers | The number of correct answers determined knowledge categories. Pre-intervention, 3.2% had poor knowledge, 56.3% had fair, 39.9% had satisfactory, and 0.6% had good knowledge. Post-intervention, the percentage of correct answers increased to 1.3% fair, 67.7% satisfactory, and 31.0% good knowledge. Increased knowledge was unrelated to previous food allergy training (χ2 = 0.143, p = 0.931). |
| Rodríguez 2020 [40] Spain | 40–50-minute presentation by pediatric allergist and a 10–20-minute EAI practical session by pediatric nurse. Sessions taught allergy definition allergic reactions pathophysiology, reactions prevention and recognition, communication with family and EAP development, anaphylaxis management, legal aspects and official recommendations. | From pre-post-intervention, participants had significantly better anaphylaxis recognition (40.0% vs. 81.0%, respectively; p < 0.001). Knowledge of how and when to use the EAI increased from 19.0% and 13.0%, respectively, to 100.0% of participants (p < 0.001). |
| Shah 2013 [34] USA | 1-hour education session with physician. Sessions taught food allergy prevalence, causal foods, signs of local and systemic reactions, reaction prevention and treatment. | Teachers in the economically-disadvantaged vs. economically-advantaged school areas had a larger increase in correct answers post-intervention (34.6%; 95% CI = 32.1–103.9 vs. 24.6%, 95% CI = 21.5–74.1, respectively). Teachers from both economically-disadvantaged and advantaged school areas had increased scores from pre-post-intervention in questions related to treatment of local and systemic reactions, causal foods, and signs of anaphylaxis. |
| Wahl 2015 [35] USA | 45-minute presentation by a food allergy Educator nurse. Practical EAI training was included. Sessions taught key food allergies facts, allergic reactions, prevention, and recognition, and importance of immediate treatment. | Post-intervention, most teachers and school staff had better confidence in prevention of allergic reactions (94.0%), recognizing reaction signs and symptoms (96%), know what to do in an emergency (97%), and administer an EAI (94%). Approximately half of participants had prior food allergy training. 95.0% of participants had positive feedback about food allergy management confidence in preventing allergic reactions, symptom recognition, and knowing what to do in emergencies 3–12-months post-intervention. 57.0% of participants recalled three key messages from the sessions. 21 participants who experienced a food allergy emergency post-intervention were interviewed. 61.9% found that signs and symptoms recognition and 52.3% reported EAI training were useful in real-life situations. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, M.J.L.; Merrill, K.A.; Gerdts, J.D.; Ben-Shoshan, M.; Protudjer, J.L.P. Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps. Nutrients 2022, 14, 732. https://doi.org/10.3390/nu14040732
Santos MJL, Merrill KA, Gerdts JD, Ben-Shoshan M, Protudjer JLP. Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps. Nutrients. 2022; 14(4):732. https://doi.org/10.3390/nu14040732
Chicago/Turabian StyleSantos, Mae Jhelene L., Kaitlyn A. Merrill, Jennifer D. Gerdts, Moshe Ben-Shoshan, and Jennifer L. P. Protudjer. 2022. "Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps" Nutrients 14, no. 4: 732. https://doi.org/10.3390/nu14040732
APA StyleSantos, M. J. L., Merrill, K. A., Gerdts, J. D., Ben-Shoshan, M., & Protudjer, J. L. P. (2022). Food Allergy Education and Management in Schools: A Scoping Review on Current Practices and Gaps. Nutrients, 14(4), 732. https://doi.org/10.3390/nu14040732






