Vitamin D and Calcium Supplementation in Nursing Homes—A Quality Improvement Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Recruitment of Nursing Homes
2.3. Baseline Data
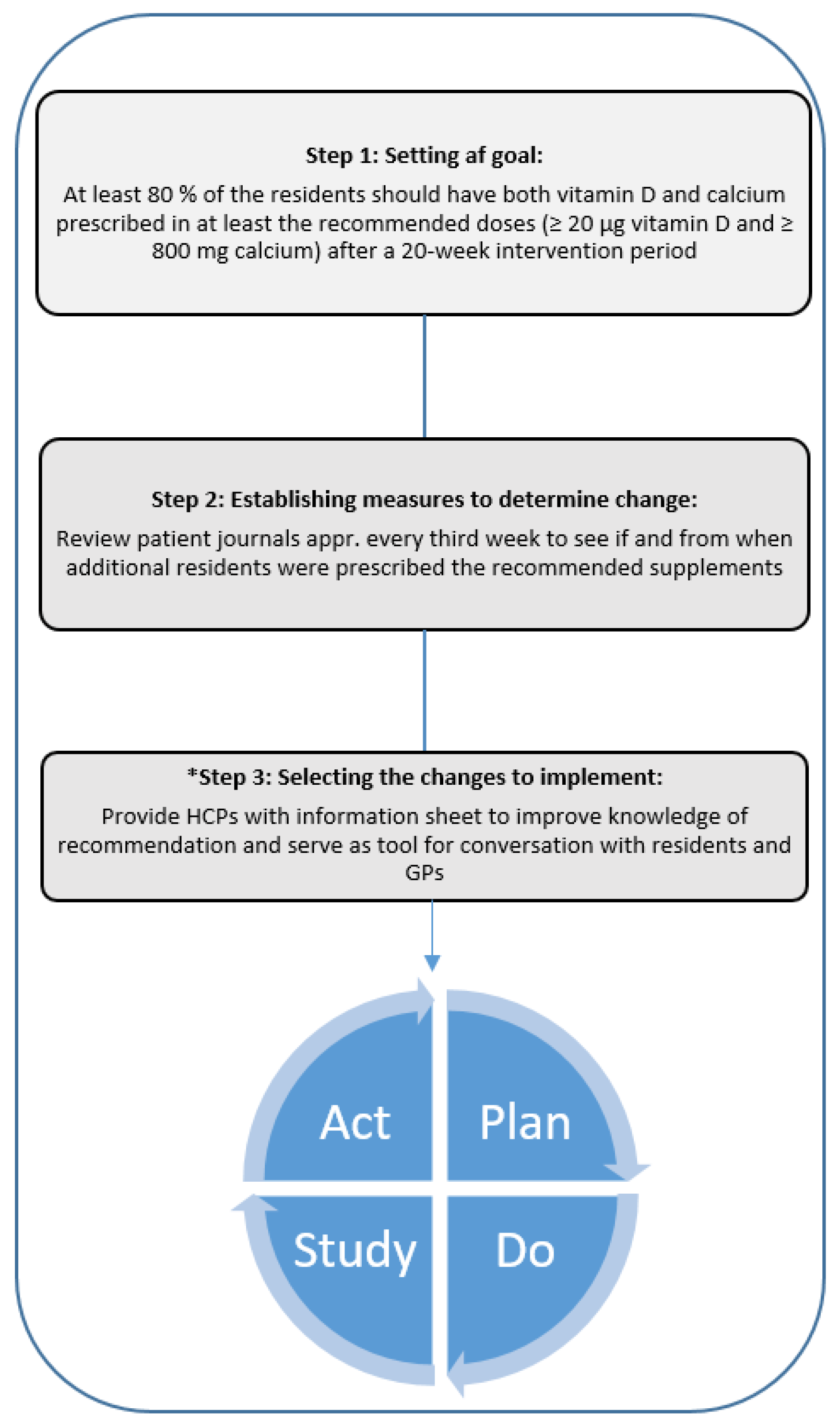
2.4. Steps in the Model for Improvement
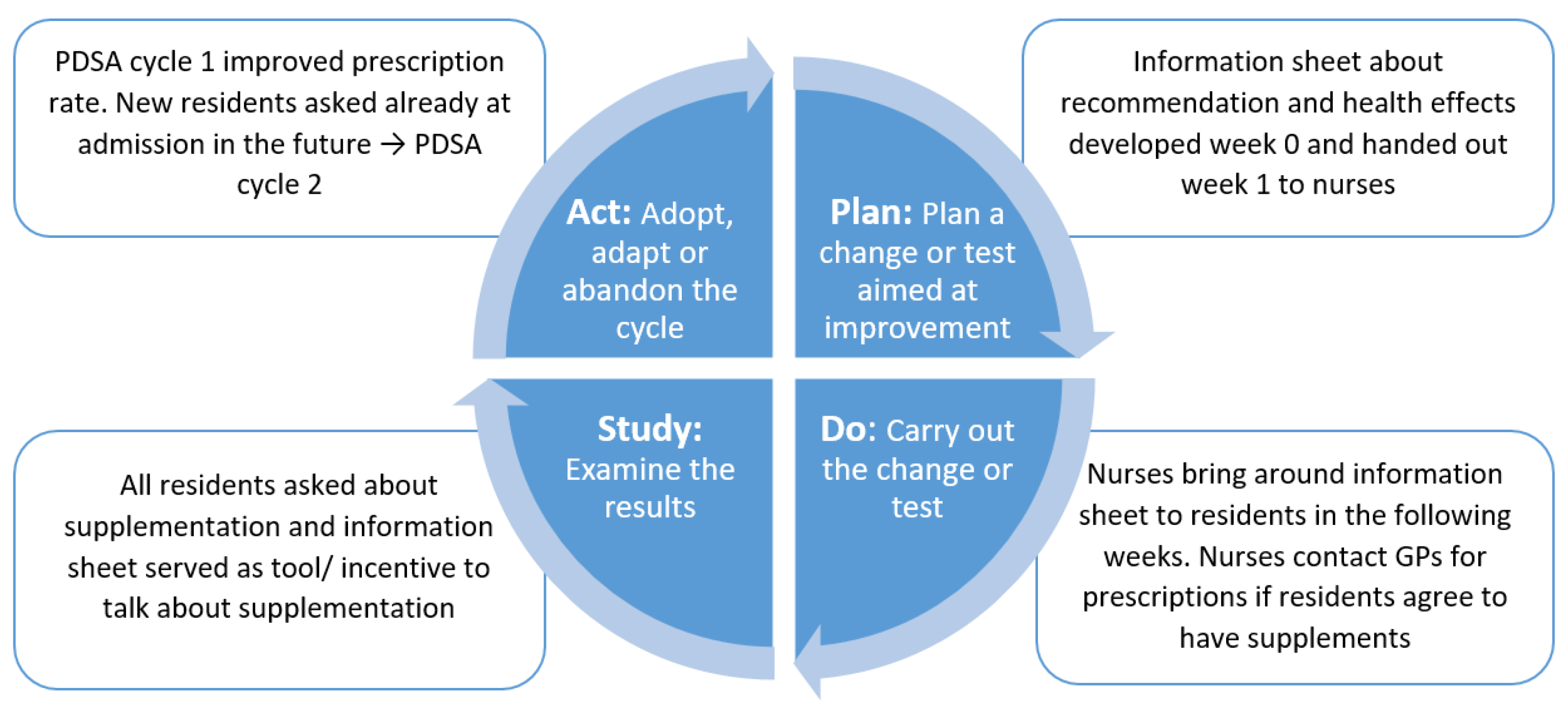
2.5. The Plan-Do-Study-Act Cycles
2.6. Effect Evaluation
2.7. Process Evaluation
2.8. Statistics
2.9. Ethics
3. Results
3.1. Baseline Data
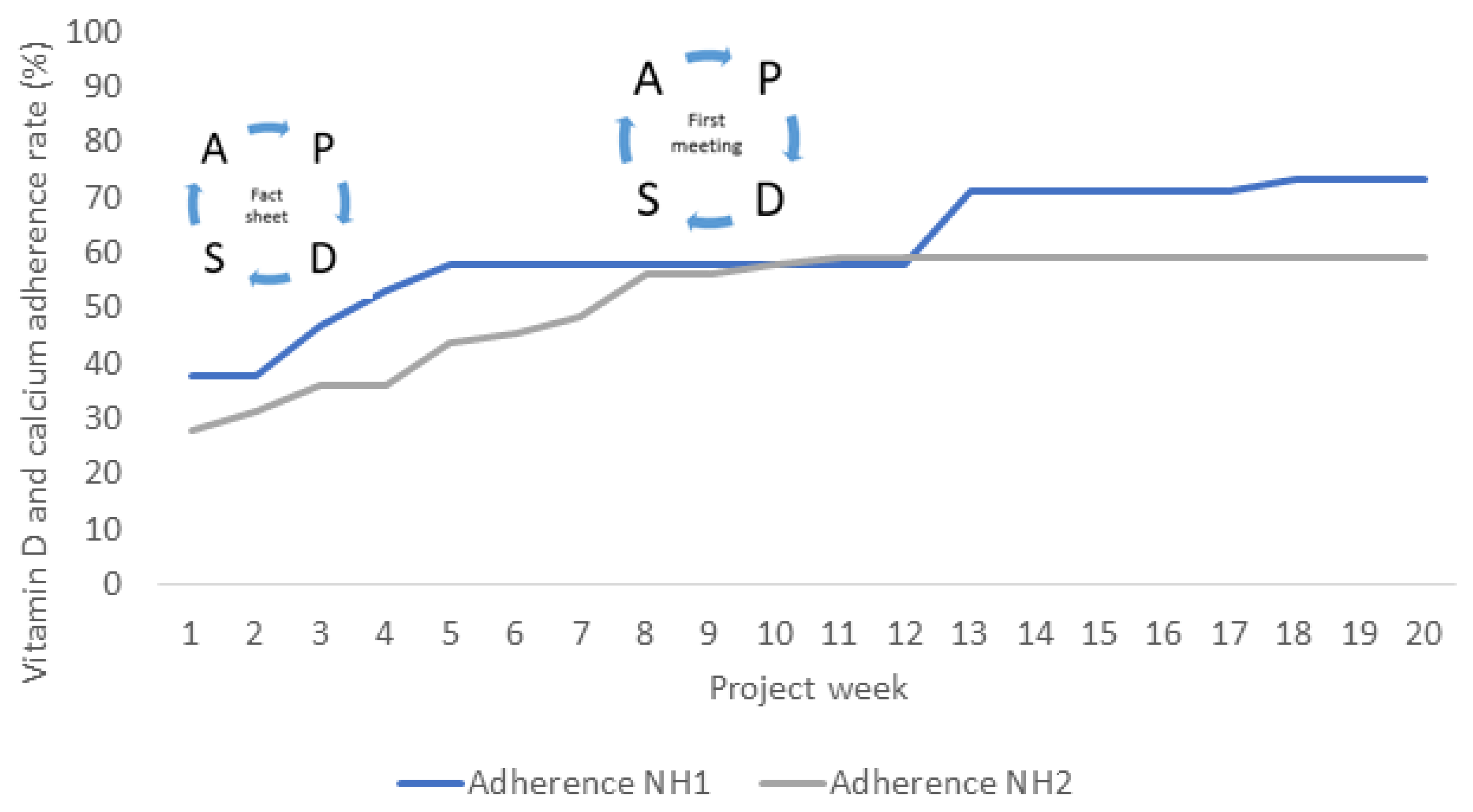
3.2. Effect of the Intervention
3.3. Process Evaluation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nordic Council of Ministers. Nordic Nutrition Recommendations 2012: Integrating Nutrition and Physical Activity, 1st ed.; Norden: Copenhagen, Denmark, 2014; Volume 5, ISBN 978-92-893-2670-4. [Google Scholar]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific Opinion on Dietary Reference Values for Vitamin D. Eur. Food Saf. Authority J. 2016, 14, 4547. [Google Scholar] [CrossRef]
- Byers, A.W.; Connolly, G.; Campbell, W.W. Vitamin D Status and Supplementation Impacts on Skeletal Muscle Function: Comparisons between Young Athletes and Older Adults. Curr. Opin. Clin. Nutr. Metab. Care 2020, 23, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Rolland, Y.; de Souto Barreto, P.; van Kan, G.A.; Annweiler, C.; Beauchet, O.; Bischoff-Ferrari, H.; Berrut, G.; Blain, H.; Bonnefoy, M.; Cesari, M.; et al. Vitamin D Supplementation in Older Adults: Searching for Specific Guidelines in Nursing Homes. J. Nutr. Health Aging 2013, 17, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Itkonen, S.T.; Andersen, R.; Björk, A.K.; Brugård Konde, Å.; Eneroth, H.; Erkkola, M.; Holvik, K.; Madar, A.A.; Meyer, H.E.; Tetens, I.; et al. Vitamin D Status and Current Policies to Achieve Adequate Vitamin D Intake in the Nordic Countries. Scand. J. Public Health 2020, 49, 616–627. [Google Scholar] [CrossRef]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D Supplementation Guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D Deficiency 2.0: An Update on the Current Status Worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef]
- Samefors, M.; Östgren, C.J.; Mölstad, S.; Lannering, C.; Midlöv, P.; Tengblad, A. Vitamin D Deficiency in Elderly People in Swedish Nursing Homes Is Associated with Increased Mortality. Eur. J. Endocrinol. 2014, 170, 667–675. [Google Scholar] [CrossRef]
- Reid, I.R.; Bolland, M.J. Controversies in Medicine: The Role of Calcium and Vitamin D Supplements in Adults. Med. J. Aust. 2019, 211, 468–473. [Google Scholar] [CrossRef]
- Houston, D.K.; Cesari, M.; Ferrucci, L.; Cherubini, A.; Maggio, D.; Bartali, B.; Johnson, M.A.; Schwartz, G.G.; Kritchevsky, S.B. Association between Vitamin D Status and Physical Performance: The InCHIANTI Study. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 440–446. [Google Scholar] [CrossRef]
- Cameron, I.D.; Dyer, S.M.; Panagoda, C.E.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for Preventing Falls in Older People in Care Facilities and Hospitals. Cochrane Database Syst. Rev. 2018, 2018, CD005465. [Google Scholar] [CrossRef]
- Kojima, G.; Tanabe, M. Frailty Is Highly Prevalent and Associated with Vitamin D Deficiency in Male Nursing Home Residents. J. Am. Geriatr. Soc. 2016, 64, e33–e35. [Google Scholar] [CrossRef] [PubMed]
- Pilz, S.; Dobnig, H.; Tomaschitz, A.; Kienreich, K.; Meinitzer, A.; Friedl, C.; Wagner, D.; Piswanger-Sölkner, C.; März, W.; Fahrleitner-Pammer, A. Low 25-Hydroxyvitamin D Is Associated with Increased Mortality in Female Nursing Home Residents. J. Clin. Endocrinol. Metab. 2012, 97, E653–E657. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, C.; Tetens, I.; Kristensen, M.; Snitkjaer, P.; Beck, A.M. Adherence and Barriers to the Vitamin D and Calcium Supplement Recommendation at Danish Nursing Homes: A Cross-Sectional Study. BMC Geriatr. 2022, 22, 27. [Google Scholar] [CrossRef] [PubMed]
- Munir, J.; Wright, R.J.; Carr, D.B. A Quality Improvement Study on Calcium and Vitamin D Supplementation in Long-Term Care. J. Am. Med. Dir. Assoc. 2006, 7, 305–309. [Google Scholar] [CrossRef]
- Yanamadala, M.; Heflin, M.T.; White, H.K.; Buhr, G.T. Ensuring Vitamin D Supplementation in Nursing Home Patients—A Quality Improvement Project. J. Nutr. Gerontol. Geriatr. 2012, 31, 158–171. [Google Scholar] [CrossRef]
- Kennedy, C.C.; Ioannidis, G.; Thabane, L.; Adachi, J.D.; Marr, S.; Giangregorio, L.M.; Morin, S.N.; Crilly, R.G.; Josse, R.G.; Lohfeld, L.; et al. Successful Knowledge Translation Intervention in Long-Term Care: Final Results from the Vitamin D and Osteoporosis Study (ViDOS) Pilot Cluster Randomized Controlled Trial. Trials 2015, 16, 214. [Google Scholar] [CrossRef]
- Walker, P.; Kifley, A.; Kurrle, S.; Cameron, I.D. Increasing the Uptake of Vitamin D Supplement Use in Australian Residential Aged Care Facilities: Results from the Vitamin D Implementation (ViDAus) Study. BMC Geriatr. 2020, 20, 383. [Google Scholar] [CrossRef]
- Williams, J.; Williams, C. Responsibility for Vitamin D Supplementation of Elderly Care Home Residents in England: Falling through the Gap between Medicine and Food. BMJ Nutr. Prev. Health 2020, 3, 256–262. [Google Scholar] [CrossRef]
- Danish Patient Safety Authority. Proper handling of medication. A tool for care centers, home care etc. Responsibility, safety and tasks [Korrekt håndtering af medicin. Et værktøj for plejecentre, hjemmepleje, hjemmesyge, bosteder m.v. Ansvar, sikkerhed og opgaver]. 2019, Volume 2, pp. 1–20. Available online: https://stps.dk/da/udgivelser/2019/korrekt-medicinhaandtering/~/media/0E30EDB960FA47DBA41FDA577A0AB979 (accessed on 15 September 2022). (In Danish).
- Danish Health Authority. Recommendations on Vitamin D [Anbefalinger om D-vitamin]. Available online: https://www.sst.dk/da/viden/ernaering/anbefalinger-om-d-vitamin (accessed on 15 March 2021). (In Danish).
- Buckinx, F.; Reginster, J.Y.; Cavalier, E.; Petermans, J.; Ricour, C.; Dardenne, C.; Bruyère, O. Determinants of Vitamin D Supplementation Prescription in Nursing Homes: A Survey among General Practitioners. Osteoporos. Int. 2016, 27, 881–886. [Google Scholar] [CrossRef]
- Bauer, M.S.; Damschroder, L.; Hagedorn, H.; Smith, J.; Kilbourne, A.M. An Introduction to Implementation Science for the Non-Specialist. BMC Psychol. 2015, 3, 32. [Google Scholar] [CrossRef]
- Morris, Z.S.; Wooding, S.; Grant, J. The Answer Is 17 Years, What Is the Question: Understanding Time Lags in Translational Research. J. R. Soc. Med. 2011, 104, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; McNicholas, C.; Nicolay, C.; Darzi, A.; Bell, D.; Reed, J.E. Systematic Review of the Application of the Plan–do–study–act Method to Improve Quality in Healthcare. BMJ Qual. Saf. 2014, 23, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Crowl, A.; Sharma, A.; Sorge, L.; Sorensen, T. Accelerating Quality Improvement within Your Organization: Applying the Model for Improvement. J. Am. Pharm. Assoc. 2015, 55, e364–e376. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, S.V.; Laursen, H.V.B.; Johnsen, S.P.; Bartels, P.D.; Ehlers, L.H.; Mainz, J. Can Quality Improvement Improve the Quality of Care? A Systematic Review of Reported Effects and Methodological Rigor in Plan-Do-Study-Act Projects. BMC Health Serv. Res. 2019, 19, 683. [Google Scholar] [CrossRef] [PubMed]
- Reed, J.E.; Card, A.J. The Problem with Plan-Do-Study-Act Cycles. BMJ Qual. Saf. 2016, 25, 147–152. [Google Scholar] [CrossRef]
- Kring Schjørring, M.; Tjørnhøj-Thomsen, T.; Hulvej Rod, M. Evaluation of “in Safe Hands” [Evaluering Af I Sikre Hænder]. Natl. Inst. Public Health Dan. Statens Inst. Folk. 2017, 2017, 1–45. (In Danish) [Google Scholar]
- The Danish Data Protection Agency. The General Notification System Ends [Den Generelle Anmeldelsesordning Ophører]. Available online: https://www.datatilsynet.dk/presse-og-nyheder/nyhedsarkiv/2018/maj/den-generelle-anmeldelsesordning-ophoerer (accessed on 22 February 2022). (In Danish).
- Ministry of Health and the Elderly. National Examination of Conditions in Nursing [National Undersøgelse Af Forholdende På Plejecentre]. Available online: https://dsr.dk/sites/default/files/192/undersoegelse-af-forholdene-paa-plejecentreashx_.pdf (accessed on 22 February 2022). (In Danish).
- The Danish Health Data Authority [Sundhedsdatastyrelsen]. Many Have a Long Stay in Nursing Home [Mange Bor Længe På Plejehjem]. Available online: https://sundhedsdatastyrelsen.dk/da/nyheder/2020/plejehjemsbeboere_161220 (accessed on 22 February 2022). (In Danish).
- Mol, R.; Kansu, A.D.; Cebe, T.; Yildiz, S.; Butun, V.K.; Simsek, B.; Cakatay, U. High versus Moderate Dosage of Daily and Weekly Administration of Vitamin D Supplements in the Form of Oil Drop in Nursing Home Residents. J. Coll. Physicians Surg. Pak. 2018, 28, 618–622. [Google Scholar] [CrossRef]
- O’Neill, C.M.; Kazantzidis, A.; Ryan, M.J.; Barber, N.; Sempos, C.T.; Durazo-Arvizu, R.A.; Jorde, R.; Grimnes, G.; Eiriksdottir, G.; Gudnason, V.; et al. Seasonal Changes in Vitamin D-Effective UVB Availability in Europe and Associations with Population Serum 25-Hydroxyvitamin D. Nutrients 2016, 8, 533. [Google Scholar] [CrossRef]
- Hansen, L.; Tjønneland, A.; Køster, B.; Brot, C.; Andersen, R.; Cohen, A.S.; Frederiksen, K.; Olsen, A. Vitamin D Status and Seasonal Variation among Danish Children and Adults: A Descriptive Study. Nutrients 2018, 10, 1801. [Google Scholar] [CrossRef]
- Frantzen, C.; Videbæk, P.N.; Andersen, B.V.; Kidmose, U.; Lähteenmäki, L.; Grønhøj, A. Anbefalinger Om Tilskud Af D-Vitamin Og Calcium-Viden, Accept Og Efterlevelse Blandt de 55+ Årige. Aarhus Univ. 2019, 157, 59. [Google Scholar]
- Sanders, K.M.; Scott, D.; Ebeling, P.R. Vitamin D Deficiency and Its Role in Muscle-Bone Interactions in the Elderly. Curr. Osteoporos. Rep. 2014, 12, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.M.; Eslick, G.D.; Nowson, C.; Smith, C.; Bensoussan, A. Use of Calcium or Calcium in Combination with Vitamin D Supplementation to Prevent Fractures and Bone Loss in People Aged 50 Years and Older: A Meta-Analysis. Lancet 2007, 370, 657–666. [Google Scholar] [CrossRef] [PubMed]
| Nursing Home 1 | Nursing Home 2 | |
|---|---|---|
| Number of residents (n) | 45 | 64 |
| Adherence to the recommendation n (%) | 17 (37.8) | 18 (28.1) |
| General practitioner affiliated | Yes | No |
| Baseline Week 1 n (%) | Endpoint Week 20 n (%) | Week 1–20 1 p-Values | |
|---|---|---|---|
| NH1 (n = 45) | 17 (37.8%) | 33 (73.3%) | <0.001 |
| NH2 (n = 64) | 18 (28.1%) | 38 (59.4%) | <0.001 |
| NH1 + NH2 (n = 109) | 35 (32.1%) | 71 (65.1%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mortensen, C.; Tetens, I.; Kristensen, M.; Beck, A.M. Vitamin D and Calcium Supplementation in Nursing Homes—A Quality Improvement Study. Nutrients 2022, 14, 5360. https://doi.org/10.3390/nu14245360
Mortensen C, Tetens I, Kristensen M, Beck AM. Vitamin D and Calcium Supplementation in Nursing Homes—A Quality Improvement Study. Nutrients. 2022; 14(24):5360. https://doi.org/10.3390/nu14245360
Chicago/Turabian StyleMortensen, Charlotte, Inge Tetens, Michael Kristensen, and Anne Marie Beck. 2022. "Vitamin D and Calcium Supplementation in Nursing Homes—A Quality Improvement Study" Nutrients 14, no. 24: 5360. https://doi.org/10.3390/nu14245360
APA StyleMortensen, C., Tetens, I., Kristensen, M., & Beck, A. M. (2022). Vitamin D and Calcium Supplementation in Nursing Homes—A Quality Improvement Study. Nutrients, 14(24), 5360. https://doi.org/10.3390/nu14245360






