Young Adults with Higher Salt Intake Have Inferior Hydration Status: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
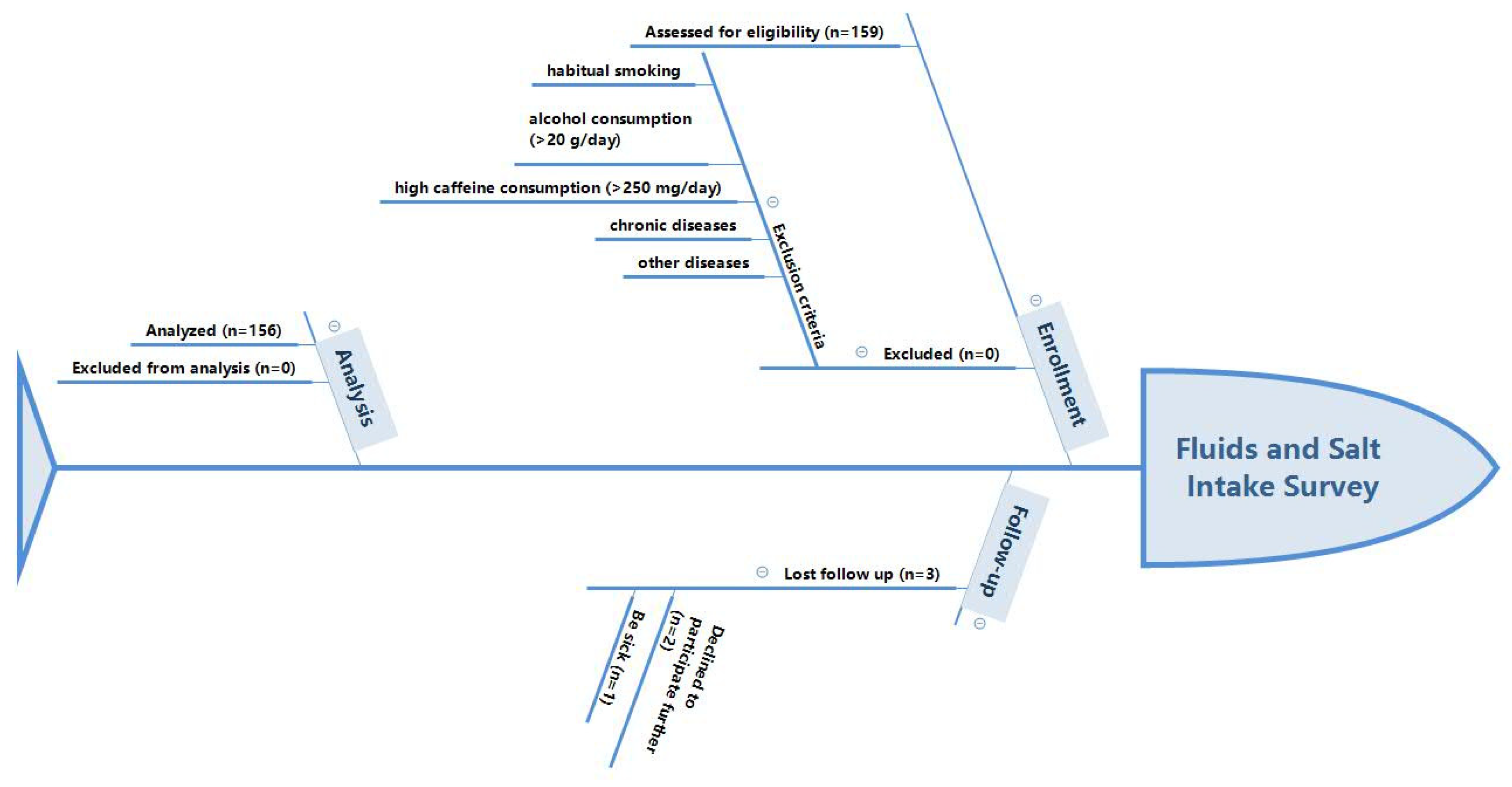
2.1. Study Design
2.2. Sample Size Calculation
2.3. Participants
2.4. Study Procedure
2.5. Measurement of Total Water Intake
2.6. Temperature and Humidity of the Environment
2.7. Anthropometric Measurements
2.8. Urine Collection and Measurements
2.9. Plasma Collection and Measurements
2.10. Calculation Formulas Used
2.11. Statistics
3. Results
3.1. Measurement of Water Intake Patterns
3.2. Drinking Patterns
3.3. Water from Food
3.4. Measurement of Urinary and Plasma Indexes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LS | Low salt |
| HS | High salt |
| TWI | Total water intake |
| EFSA | European Food Safety Authority |
References
- Thornton, S.N. Thirst and hydration: Physiology and consequences of dysfunction. Physiol. Behav. 2010, 100, 15–21. [Google Scholar] [CrossRef]
- Wittbrodt, M.T.; Millard-Stafford, M. Dehydration Impairs Cognitive Performance. Med. Sci. Sports Exerc. 2018, 50, 2360–2368. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific Opinion on Dietary Reference Values for Water. EFSA J. 2010, 8, 1459. [Google Scholar]
- Poggio, R.; Gutierrez, L.; Matta, M.G.; Elorriaga, N.; Irazola, V.; Rubinstein, A. Daily sodium consumption and CVD mortality in the general population: Systematic review and meta-analysis of prospective studies. Public Health Nutr. 2015, 18, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-J.; Yeh, T.-L.; Shih, M.-C.; Tu, Y.-K.; Chien, K.-L. Dietary Sodium Intake and Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-Analysis. Nutrients 2020, 12, 2934. [Google Scholar] [CrossRef]
- Armstrong, L.E. Rehydration during Endurance Exercise: Challenges, Research, Options, Methods. Nutrients 2021, 13, 887. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Guideline: Sodium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Webb, M.; Fahimi, S.; Singh, G.M.; Khatibzadeh, S.; Micha, R.; Powles, J.; Mozaffarian, D. Cost effectiveness of a government supported policy strategy to decrease sodium intake: Global analysis across 183 nations. BMJ 2017, 356, i6699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, K.; He, Y.; Fang, Y.; Lian, Y. Dietary Sodium Intake and Food Sources among Chinese Adults: Data from the CNNHS 2010–2012. Nutrients 2020, 12, 453. [Google Scholar] [CrossRef] [Green Version]
- Firestone, M.; Beasley, J.; Kwon, S.; Ahn, J.; Trinh-Shevrin, C.; Yi, S.S. Asian American Dietary Sources of Sodium and Salt Behaviors Compared with Other Racial/Ethnic Groups, NHANES, 2011–2012. Ethn. Dis. 2017, 27, 241–248. [Google Scholar] [CrossRef]
- Nowson, C.; Lim, K.; Grimes, C.; O’Halloran, S.; Land, M.A.; Webster, J.; Shaw, J.; Chalmers, J.; Smith, W.; Flood, V.; et al. Dietary Salt Intake and Discretionary Salt Use in Two General Population Samples in Australia: 2011 and 2014. Nutrients 2015, 7, 10501–10512. [Google Scholar] [CrossRef]
- Rakova, N.; Kitada, K.; Lerchl, K.; Dahlmann, A.; Birukov, A.; Daub, S.; Kopp, C.; Pedchenko, T.; Zhang, Y.; Beck, L.; et al. Increased salt consumption induces body water conservation and decreases fluid intake. J. Clin. Investig. 2017, 127, 1932–1943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bankir, L.; Perucca, J.; Norsk, P.; Bouby, N.; Damgaard, M. Relationship between Sodium Intake and Water Intake: The False and the True. Ann. Nutr. Metab. 2017, 70 (Suppl. S1), 51–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spek, J.W.; Bannink, A.; Gort, G.; Hendriks, W.H.; Dijkstra, J. Effect of sodium chloride intake on urine volume, urinary urea excretion, and milk urea concentration in lactating dairy cattle. J. Dairy Sci. 2012, 95, 7288–7298. [Google Scholar] [CrossRef] [Green Version]
- Hawthrone, A.J.; Markwell, P.J. Dietary Sodium Promotes Increased Water Intake and Urine Volume in Cats. J. Nutri. 2004, 134, 2128S–2129S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eriksson, L.; Valtonen, M.; Mäkelä, J. Water and electrolyte balance in male mink (Mustela vison) on varying dietary NaCl intake. Acta Physiol. Scand. Suppl. 1984, 537, 59–64. [Google Scholar]
- Carroll, H.A.; Templeman, I.; Chen, Y.-C.; Edinburgh, R.; Burch, E.K.; Jewitt, J.T.; Povey, G.; Robinson, T.D.; Dooley, W.L.; Buckley, C.; et al. Hydration status affects thirst and salt preference but not energy intake or postprandial ghrelin in healthy adults: A randomised crossover trial. Physiol. Behav. 2019, 212, 112725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexy, U.; Cheng, G.; Libuda, L.; Hilbig, A.; Kersting, M. 24h-Sodium excretion and hydration status in children and adolescents—Results of the DONALD Study. Clin. Nutr. 2012, 31, 78–84. [Google Scholar] [CrossRef]
- He, F.J.; Marrero, N.M.; MacGregor, G.A. Salt intake is related to soft drink consumption in children and adolescents: A link to obesity? Hypertension 2008, 51, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Grimes, C.A.; Riddell, L.J.; Campbell, K.J.; Nowson, C.A. Dietary salt intake, sugar-sweetened beverage consumption and obesity risk. Pediatrics 2013, 131, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Hardy, L.L.; Bell, J.; Bauman, A.; Mihrshahi, S. Association between adolescents’ consumption of total and different types of sugar-sweetened beverages with oral health impacts and weight status. Aust. N. Z. J. Public Health 2017, 42, 22–26. [Google Scholar] [CrossRef] [Green Version]
- Kwak, J.H.; Jo, G.; Chung, H.-K.; Shin, M.-J. Association between sugar-sweetened beverage consumption and incident hypertension in Korean adults: A prospective study. Eur. J. Nutr. 2018, 58, 1009–1017. [Google Scholar] [CrossRef]
- Luger, M.; Lafontan, M.; Bes-Rastrollo, M.; Winzer, E.; Yumuk, V.; Farpour-Lambert, N. Sugar-Sweetened Beverages and Weight Gain in Children and Adults: A Systematic Review from 2013 to 2015 and a Comparison with Previous Studies. Obes. Facts 2017, 10, 674–693. [Google Scholar] [CrossRef]
- Narain, A.; Kwok, C.S.; Mamas, M.A. Soft drink intake and the risk of metabolic syndrome: A systematic review and meta-analysis. Int. J. Clin. Pract. 2017, 71, e12927. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yatsuya, H.; Tamakoshi, K.; Iso, H.; Tamakoshi, A. Milk Drinking and Mortality: Findings from the Japan Collaborative Cohort Study. J. Epidemiol. 2015, 25, 66–73. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Zhang, N.; Liang, S.; Wang, Y.; Liu, S.; Liu, S.; Du, S.; He, H.; Xu, Y.; Cai, H.; et al. The amounts and contributions of total drinking fluids and water from food to total water intake of young adults in Baoding, China. Eur. J. Nutr. 2019, 58, 2669–2677. [Google Scholar] [CrossRef] [PubMed]
- Guelinckx, I.; Tavoularis, G.; König, J.; Morin, C.; Gharbi, H.; Gandy, J. Contribution of Water from Food and Fluids to Total Water Intake: Analysis of a French and UK Population Surveys. Nutrients 2016, 8, 630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.; Shin, D.; Song, W. Total Water Intake from Beverages and Foods Is Associated with Energy Intake and Eating Behaviors in Korean Adults. Nutrients 2016, 8, 617. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Zhang, N.; Wang, Y.; Liang, S.; Liu, S.; Du, S.; Xu, Y.; He, H.; Cai, H.; Ma, G. Drinking patterns and hydration biomarkers among young adults with different levels of habitual total drinking fluids intake in Baoding, Hebei Province, China: A cross-sectional study. BMC Public Health 2020, 20, 468. [Google Scholar] [CrossRef]
- Dong, W.; Zhang, Q.; Jiang, J.; Chen, H.; Chen, X.; Shao, S.; Liu, J.; Ji, Y. Evaluating the sodium intake of community residents in Shantou city by 24-h urine method. Chin. J. Prev. Control Chronic Dis. 2017, 25, 481–485. (In Chinese) [Google Scholar]
- Pross, N.; Demazières, A.; Girard, N.; Barnouin, R.; Metzger, D.; Klein, A.; Perrier, E.; Guelinckx, I. Effects of Changes in Water Intake on Mood of High and Low Drinkers. PLoS ONE 2014, 9, e94754. [Google Scholar] [CrossRef]
- Ma, G.; Zhang, Q.; Liu, A.; Zuo, J.; Zhang, W.; Zou, S.; Li, X.; Lu, L.; Pan, H.; Hu, X. Fluid intake of adults in four Chinese cities. Nutr. Rev. 2012, 70, S105–S110. [Google Scholar] [CrossRef]
- Du, S.-M.; Pan, H.; Hu, X.-Q.; Zhang, Q.; Wang, X.-J.; Lu, L.-X.; Zou, S.-R.; Fan, J.-W.; Li, X.-H.; Ma, G.-S. Water intake of primary and middle school students in four cities of China. Chin. J. Prev. Med. 2013, 47, 210–213. (In Chinese) [Google Scholar]
- General Administration of Quality Supervision, Inspection and Quarantine of China. General Standard for Beverages GB/T 1–789-2015; Standardization Administration of China: Beijing, China, 2015.
- Standardization Administration of China. National Food Safety Standard GB 5009.3–2016: Determination of Moisture in Foods; China Standard Press: Beijing, China, 2016. [Google Scholar]
- Institute for Nutrition and Health, Chinese Center for Disease Control and Prevention. China Food Composition; Peking University Medicine Press: Beijing, China, 2009. [Google Scholar]
- Perrier, E.T.; Buendia-Jimenez, I.; Vecchio, M.; Armstrong, L.E.; Tack, I.; Klein, A. Twenty-Four-Hour Urine Osmolality as a Physiological Index of Adequate Water Intake. Dis. Markers 2015, 2015, 231063. [Google Scholar] [CrossRef] [Green Version]
- Hipgrave, D.B.; Chang, S.; Li, X. Salt and Sodium Intake in China. JAMA 2016, 315, 703. [Google Scholar] [CrossRef] [Green Version]
- Nunez, M.F.; Mollard, R.C.; Luhovyy, B.L.; Wong, C.L.; Anderson, G.H. Acute sodium ingestion has no effect on short-term food and water intake, subjective appetite, thirst, or glycemic response in healthy young men. Appl. Physiol. Nutr. Metab. 2013, 38, 746–752. [Google Scholar] [CrossRef]
- Lucia, K.J.; Curtis, K.S. Behavioral responses and fluid regulation in male rats after combined dietary sodium deficiency and water deprivation. Physiol. Behav. 2018, 184, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J.; Watson, P.; Cordery, P.A.; Walsh, N.P.; Oliver, S.J.; Dolci, A.; Rodriguez-Sanchez, N.; Galloway, S.D. A randomized trial to assess the potential of different beverages to affect hydration status: Development of a beverage hydration index. Am. J. Clin. Nutr. 2016, 103, 717–723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alwis, U.S.; Haddad, R.; Monaghan, T.; Abrams, P.; Dmochowski, R.; Bower, W.; Wein, A.J.; Roggeman, S.; Weiss, J.P.; Mourad, S.; et al. Impact of food and drinks on urine production: A systematic review. Int. J. Clin. Pract. 2020, 74, e13539. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; Markandu, N.D.; Sagnella, G.A.; MacGregor, G.A. Effect of Salt Intake on Renal Excretion of Water in Humans. Hypertension 2001, 38, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, J.M.; Hamilton-Reeves, J.M.; Sullivan, D.K.; Gibson, C.A.; Creed, C.; Carlson, S.E.; Wesson, D.E.; Grantham, J.J. Diet and polycystic kidney disease: A pilot intervention study. Clin. Nutr. 2017, 36, 458–466. [Google Scholar] [CrossRef] [Green Version]
- Ogna, A.; Ogna, V.F.; Bochud, M.; Guessous, I.; Paccaud, F.; Burnier, M.; Wuerzner, G. Association between obesity and glomerular hyperfiltration: The confounding effect of smoking and sodium and protein intakes. Eur. J. Nutr. 2016, 55, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Kanbay, M.; Aslan, G.; Afsar, B.; Dagel, T.; Siriopol, D.; Kuwabara, M.; Incir, S.; Camkiran, V.; Rodriguez-Iturbe, B.; Lanaspa, M.A.; et al. Acute effects of salt on blood pressure are mediated by serum osmolality. J. Clin. Hypertens. 2018, 20, 1447–1454. [Google Scholar] [CrossRef] [PubMed]
- Twerenbold, R.; Knechtle, B.; Kakebeeke, T.H.; Eser, P.; Müller, G.; Von Arx, P.; Knecht, H. Effects of different sodium concentrations in replacement fluids during prolonged exercise in women. Br. J. Sports Med. 2003, 37, 300–303. [Google Scholar] [CrossRef] [Green Version]
- Kitada, K.; Daub, S.; Zhang, Y.; Klein, J.D.; Nakano, D.; Pedchenko, T.; Lantier, L.; Larocque, L.M.; Marton, A.; Neubert, P.; et al. High salt intake reprioritizes osmolyte and energy metabolism for body fluid conservation. J. Clin. Investig. 2017, 127, 1944–1959. [Google Scholar] [CrossRef] [Green Version]
- Barić, L.; Drenjančević, I.; Matić, A.; Stupin, M.; Kolar, L.; Mihaljević, Z.; Lenasi, H.; Šerić, V.; Stupin, A. Seven-Day Salt Loading Impairs Microvascular Endothelium-Dependent Vasodilation without Changes in Blood Pressure, Body Composition and Fluid Status in Healthy Young Humans. Kidney Blood Press. Res. 2019, 44, 835–847. [Google Scholar] [CrossRef] [Green Version]
- He, F.J.; Macgregor, G.A. Salt intake, plasma sodium, and worldwide salt reduction. Ann. Med. 2012, 44, S127–S137. [Google Scholar] [CrossRef]
- Bingham, S.A. Biomarkers in nutritional epidemiology. Public Health Nutr. 2002, 5, 821–827. [Google Scholar] [CrossRef] [Green Version]
- Swanepoel, B.; Schutte, A.E.; Cockeran, M.; Steyn, K.; Wentzel-Viljoen, E. Monitoring the South African population’s salt intake: Spot urine v. 24 h urine. Public Health Nutr. 2018, 21, 480–488. [Google Scholar] [CrossRef] [Green Version]

| LS1 (n = 39) | LS2 (n = 39) | HS1 (n = 39) | HS2 (n = 39) | Total (n = 156) | p | |
|---|---|---|---|---|---|---|
| Age (y) | 19.7 ± 1.0 | 20.0 ± 1.1 | 19.8 ± 1.0 | 19.7 ± 1.2 | 19.8 ± 1.1 | 0.792 |
| Height (cm) | 163.6 ± 8.3 a | 163.2 ± 8.0 a | 167.4 ± 8.2 b | 170.7 ± 6.6 b | 166.2 ± 8.3 | <0.001 |
| Weight (kg) | 59.2 ± 11.4 a | 57.2 ± 8.2 a | 61.8 ± 8.5 a | 67.1 ± 14.7 b | 61.3 ± 11.5 | 0.001 |
| BMI (Kg/m2) | 22.0 ± 3.1 | 21.4 ± 2.3 | 22.1 ± 2.6 | 23.0 ± 4.4 | 22.1 ± 3.3 | 0.219 |
| Systolic pressure | 115 ± 14 | 111 ± 15 | 114 ± 15 | 118 ± 20 | 115 ± 16 | 0.368 |
| Diastolic pressure | 69 ± 7 | 74 ± 10 | 72 ± 7 | 73 ± 9 | 72 ± 9 | 0.083 |
| LS1 (n = 39) | LS2 (n = 39) | HS1 (n = 39) | HS2 (n = 39) | Total (n = 156) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | Q | % | M | Q | % | M | Q | % | M | Q | % | M | Q | % | |
| Total drinking fluids | 962 a | 411 | 49.3% | 1033 ab | 723 | 49.3% | 1186 bc | 709 | 48.5% | 1343 c | 648 | 49.2% | 1135 | 620 | 50.6% |
| Meets the adequate fluid intake of China | 36 (92.3%) | 31 (79.5%) | 30 (76.9%) | 30 (76.9%) | 127 (81.4%) | ||||||||||
| Meets the recommendation of TWI of China | 35 (89.7%) | 32 (82.1%) | 30 (76.9%) | 28 (71.8%) | 125 (80.1%) | ||||||||||
| Water | 726 a | 497 | 77.8% | 745 ab | 684 | 84.0% | 978 bc | 664 | 88.0% | 1129 c | 646 | 86.1% | 866 | 642 | 81.0% |
| Tea | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 1.0% |
| Milk and milk products | 43 | 107 | 5.0% | 54 | 162 | 5.6% | 51 | 131 | 4.1% | 36 | 114 | 3.0% | 43 | 131 | 6.6% |
| SSBs | 75 a | 176 | 8.1% a | 24 b | 64 | 2.5% ab | 0 b | 63 | 0.0% ab | 52 a | 188 | 4.3% ac | 43 | 112 | 8.0% |
| Alcohol | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.7% |
| Others | 4 | 39 | 0.3% | 0 | 45 | 0.0% | 0 | 36 | 0.0% | 9 | 30 | 0.7% | 0 | 17 | 2.7% |
| Water from food | 962 a | 284 | 50.7% | 1070 ab | 318 | 50.7% | 1281 c | 336 | 51.5% | 1320 c | 318 | 50.8% | 1174 | 373 | 49.4% |
| Staple food | 252 a | 86 | 27.5% | 285 ab | 161 | 28.2% | 321 c | 151 | 25.9% | 366 c | 125 | 28.2% | 301 | 141 | 26.3% |
| Dishes | 474 a | 185 | 50.8% | 573 b | 190 | 52.6% | 668 c | 189 | 53.5% | 702 c | 267 | 54.5% | 620 | 217 | 52.2% |
| Soup | 15 a | 194 | 2.1% a | 75 a | 157 | 6.0% ab | 93 a | 186 | 7.5% ab | 186 b | 194 | 13.5% bc | 93 | 195 | 10.1% |
| Porridge | 127 a | 176 | 13.3% a | 115 a | 123 | 10.3% a | 111 a | 259 | 11.3% a | 57 b | 100 | 4.1% b | 97 | 182 | 10.4% |
| Snacks | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.0% | 0 | 0 | 0.9% |
| Total water intake | 1948 a | 648 | _ | 2221 ab | 780 | _ | 2529 bc | 740 | _ | 2603 c | 376 | _ | _ | ||
| LS1 (n = 39) | LS2 (n = 39) | HS1 (n = 39) | HS2 (n = 39) | p | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | Q | X | SD | M | Q | X | SD | M | Q | X | SD | M | Q | X | SD | ||
| 24 h volume (mL) | 1049 a | 479 | 1317 b | 468 | 1467 bc | 447 | 1522 c | 460 | <0.001 | ||||||||
| 24 h urine osmolality (mOsm/kg) | 625 | 390 | 582 | 315 | 541 | 316 | 636 | 268 | 0.463 | ||||||||
| (≤500 mOsm/kg, n, %) | 16 (41.0%) a | 16 (41.0%) a | 16 (41.0%) a | 10 (25.6%) b | 0.032 | ||||||||||||
| Na (mmol/L) | 133 a | 62 | 151 ab | 78 | 192 b | 91 | 245 c | 105 | <0.001 | ||||||||
| K (mmol/L) | 33.3 a | 12.6 | 33.4 a | 14.8 | 32.6 a | 10.6 | 42.6 b | 14.2 | 0.002 | ||||||||
| Cl (mmol/L) | 132 a | 64 | 143 ab | 79 | 189 b | 99 | 244 c | 95 | <0.001 | ||||||||
| Mg (mmol/L) | 2.83 | 1.21 | 2.64 | 1.16 | 2.40 | 0.92 | 2.66 | 0.89 | 0.340 | ||||||||
| Ca (mmol/L) | 2.04 | 1.57 | 1.98 | 1.40 | 2.05 | 1.26 | 2.55 | 1.86 | 0.081 | ||||||||
| Phosphate (mmol/L) | 14.93 | 13.21 | 15.22 | 10.83 | 14.21 | 6.89 | 16.18 | 10.45 | 0.254 | ||||||||
| Creatinine (mmol/L) | 106.8 | 51.8 | 91.2 | 38.4 | 87.7 | 33.7 | 100.5 | 35.7 | 0.274 | ||||||||
| Uric acid (mmol/L) | 26.4 | 9.5 | 24.3 | 11.1 | 23.1 | 9.2 | 26.4 | 9.1 | 0.354 | ||||||||
| Urea (mmol/L) | 225.3 | 94.0 | 211.5 | 92.3 | 192.4 | 67.9 | 232.1 | 80.0 | 0.173 | ||||||||
| USG | 6.6 | 0.3 | 6.7 | 0.3 | 6.8 | 0.2 | 6.7 | 0.3 | 0.295 | ||||||||
| pH | 1.016 a | 0.004 | 1.016 ab | 0.004 | 1.015 ab | 0.004 | 1.017 b | 0.004 | 0.011 | ||||||||
| LS1 (n = 39) | LS2 (n = 39) | HS1 (n = 39) | HS2 (n = 39) | ||
|---|---|---|---|---|---|
| X (95% CI) | X (95% CI) | X (95% CI) | X (95% CI) | p | |
| Osmolality (mOsm/kg) | 299 [297, 301] | 299 [297, 301] | 299 [297, 301] | 299 [298, 301] | 0.935 |
| Na (mmol/L) | 141 [141, 141] | 141 [141, 142] | 141 [140, 141] | 141 [140, 141] | 0.241 |
| K (mmol/L) | 4.6 [4.5, 4.7] | 4.5 [4.4, 4.7] | 4.5 [4.4, 4.6] | 4.5 [4.4, 4.7] | 0.953 |
| Cl (mmol/L) | 103 [102, 103] a | 104 [103, 104] ab | 104 [104, 105] b | 104 [104, 105] b | 0.025 |
| Ca (mmol/L) | 2.52 [2.49, 2.52] | 2.53 [2.50, 2.54] | 2.51 [2.48, 2.54] | 2.51 [2.49, 2.53] | 0.781 |
| Phosphate (mmol/L) | 1.35 [1.31, 1.39] a | 1.33 [1.27, 1.38] a | 1.30 [1.25, 1.36] a | 1.22 [1.18, 1.27] b | 0.002 |
| Mg (mmol/L) | 0.92 [0.90, 0.94] | 0.91 [0.89, 0.93] | 0.92 [0.90, 0.94] | 0.92 [0.90, 0.94] | 0.770 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Zhang, N.; Liu, S.; Du, S.; Ma, G. Young Adults with Higher Salt Intake Have Inferior Hydration Status: A Cross-Sectional Study. Nutrients 2022, 14, 287. https://doi.org/10.3390/nu14020287
Zhang J, Zhang N, Liu S, Du S, Ma G. Young Adults with Higher Salt Intake Have Inferior Hydration Status: A Cross-Sectional Study. Nutrients. 2022; 14(2):287. https://doi.org/10.3390/nu14020287
Chicago/Turabian StyleZhang, Jianfen, Na Zhang, Shufang Liu, Songming Du, and Guansheng Ma. 2022. "Young Adults with Higher Salt Intake Have Inferior Hydration Status: A Cross-Sectional Study" Nutrients 14, no. 2: 287. https://doi.org/10.3390/nu14020287
APA StyleZhang, J., Zhang, N., Liu, S., Du, S., & Ma, G. (2022). Young Adults with Higher Salt Intake Have Inferior Hydration Status: A Cross-Sectional Study. Nutrients, 14(2), 287. https://doi.org/10.3390/nu14020287







