The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk—A MARK Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Ethics Approval and Consent to Participate
2.4. Variables and Measurement Instruments
2.4.1. Assessment of Arterial Stiffness with Brachial-Ankle Pulse Wave Velocity (baPWV)
2.4.2. Definition of Individuals with Early Vascular Ageing
2.4.3. Dietary Assessment
2.4.4. Assessment of Regular Physical Activity
2.4.5. Consumption of Alcohol and Tobacco
2.5. Statistical Analysis
3. Results
3.1. Clinical Characteristics and Vascular Ageing
3.2. Relationship of Arterial Stiffness with Diet Quality inDex and Mediterranean Diet Adherence
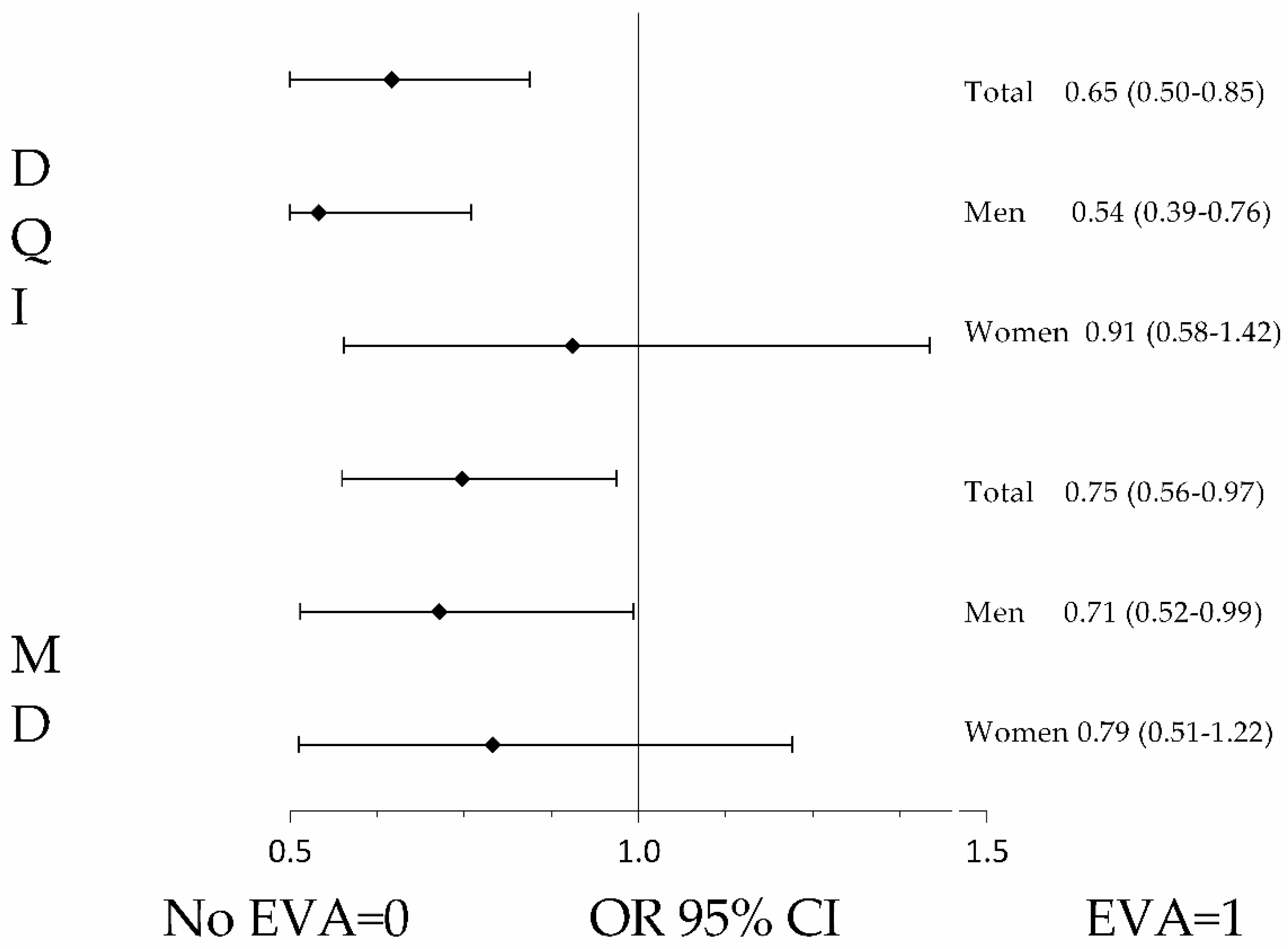
3.3. Association of EVA with Diet Quality Index and Mediterranean Diet Adherence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morze, J.; Danielewicz, A.; Przybyłowicz, K.; Zeng, H.; Hoffmann, G.; Schwingshackl, L. An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer. Eur. J. Nutr. 2021, 60, 1561–1586. [Google Scholar] [CrossRef]
- Papadaki, A.; Nolen-Doerr, E.; Mantzoros, C.S. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients 2020, 12, 3342. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean Diet and Cardiovascular Health. Circ. Res. 2019, 124, 779–798. [Google Scholar] [CrossRef]
- Liu, X.; Guasch-Ferré, M.; Tobias, D.K.; Li, Y. Association of Walnut Consumption with Total and Cause-Specific Mortality and Life Expectancy in U.S. Adults. Nutrients 2021, 13, 2699. [Google Scholar] [CrossRef]
- Ohkuma, T.; Ninomiya, T.; Tomiyama, H.; Kario, K.; Hoshide, S.; Kita, Y.; Inoguchi, T.; Maeda, Y.; Kohara, K.; Tabara, Y.; et al. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension 2017, 69, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Vamvakis, A.; Gkaliagkousi, E.; Lazaridis, A.; Grammatikopoulou, M.G.; Triantafyllou, A.; Nikolaidou, B.; Koletsos, N.; Anyfanti, P.; Tzimos, C.; Zebekakis, P.; et al. Impact of Intensive Lifestyle Treatment (Diet Plus Exercise) on Endothelial and Vascular Function, Arterial Stiffness and Blood Pressure in Stage 1 Hypertension: Results of the HINTreat Randomized Controlled Trial. Nutrients 2020, 12, 1326. [Google Scholar] [CrossRef] [PubMed]
- Jennings, A.; Berendsen, A.M.; de Groot, L.; Feskens, E.J.M.; Brzozowska, A.; Sicinska, E.; Pietruszka, B.; Meunier, N.; Caumon, E.; Malpuech-Brugère, C.; et al. Mediterranean-Style Diet Improves Systolic Blood Pressure and Arterial Stiffness in Older Adults. Hypertension 2019, 73, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martín, C.; Garcia-Ortiz, L.; Rodriguez-Sanchez, E.; Maderuelo-Fernandez, C.; Lugones-Sanchez, A.; Martin-Cantera, M.S.; Soriano-Cano, J.F.; Arietaleanizbeaskoa, M.; Magdalena-Belio, J.A.; Menendez-Suarez, C.; et al. The Relationship of the Atlantic Diet with Cardiovascular Risk Factors and Markers of Arterial Stiffness in Adults without Cardiovascular Disease. Nutrients 2019, 11, 742. [Google Scholar] [CrossRef]
- Rodríguez-Martin, C.; Alonso-Domínguez, R.; Patino-Alonso, M.C.; Gómez-Marcos, M.A.; Maderuelo-Fernández, J.A.; Martin-Cantera, C.; García-Ortiz, L.; Recio-Rodríguez, J.I. The EVIDENT diet quality index is associated with cardiovascular risk and arterial stiffness in adults. BMC Public Health 2017, 17, 305. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Couch, S.C.; The, N.S.; Crandell, J.L.; Lawrence, J.M.; Crume, T.L.; Mayer-Davis, E.J.; Zhong, V.W.; Urbina, E.M. Association between diet quality indices and arterial stiffness in youth with type 1 diabetes: SEARCH for Diabetes in Youth Nutrition Ancillary Study. J. Diabetes Complications 2020, 34, 107709. [Google Scholar] [CrossRef]
- Laurent, S.; Boutouyrie, P.; Cunha, P.G.; Lacolley, P.; Nilsson, P.M. Concept of Extremes in Vascular Aging. Hypertension 2019, 74, 218–228. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [PubMed]
- Nowak, K.L.; Rossman, M.J.; Chonchol, M.; Seals, D.R. Strategies for Achieving Healthy Vascular Aging. Hypertension 2018, 71, 389–402. [Google Scholar] [CrossRef]
- Xu, F.; Zhong, J.Y.; Lin, X.; Shan, S.K.; Guo, B.; Zheng, M.H.; Wang, Y.; Li, F.; Cui, R.R.; Wu, F.; et al. Melatonin alleviates vascular calcification and ageing through exosomal miR-204/miR-211 cluster in a paracrine manner. J. Pineal Res. 2020, 68, e12631. [Google Scholar] [CrossRef]
- Serino, A.; Salazar, G. Protective Role of Polyphenols against Vascular Inflammation, Aging and Cardiovascular Disease. Nutrients 2018, 11, 53. [Google Scholar] [CrossRef] [PubMed]
- LaRocca, T.J.; Martens, C.R.; Seals, D.R. Nutrition and other lifestyle influences on arterial aging. Ageing Res. Rev. 2017, 39, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Dhanjal, D.S.; Bhardwaj, S.; Sharma, R.; Bhardwaj, K.; Kumar, D.; Chopra, C.; Nepovimova, E.; Singh, R.; Kuca, K. Plant Fortification of the Diet for Anti-Ageing Effects: A Review. Nutrients 2020, 12, 3008. [Google Scholar] [CrossRef]
- Schröder, H.; Benitez Arciniega, A.; Soler, C.; Covas, M.I.; Baena-Díez, J.M.; Marrugat, J. Validity of two short screeners for diet quality in time-limited settings. Public Health Nutr. 2012, 15, 618–626. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Fernández-Jarne, E.; Serrano-Martínez, M.; Wright, M.; Gomez-Gracia, E. Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur. J. Clin. Nutr. 2004, 58, 1550–1552. [Google Scholar] [CrossRef]
- Martí, R.; Parramon, D.; García-Ortiz, L.; Rigo, F.; Gómez-Marcos, M.A.; Sempere, I.; García-Regalado, N.; Recio-Rodriguez, J.I.; Agudo-Conde, C.; Feuerbach, N.; et al. Improving interMediAte risk management. MARK study. BMC Cardiovasc. Disord. 2011, 11, 61. [Google Scholar] [CrossRef]
- Marrugat, J.; D’Agostino, R.; Sullivan, L.; Elosua, R.; Wilson, P.; Ordovas, J.; Solanas, P.; Cordón, F.; Ramos, R.; Sala, J.; et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J. Epidemiol. Commun. Health 2003, 57, 634–638. [Google Scholar] [CrossRef]
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redón, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 2013, 31, 1281–1357. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Shirai, K.; Hiruta, N.; Song, M.; Kurosu, T.; Suzuki, J.; Tomaru, T.; Miyashita, Y.; Saiki, A.; Takahashi, M.; Suzuki, K.; et al. Cardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness: Theory, evidence and perspectives. J. Atheroscler Thromb. 2011, 18, 924–938. [Google Scholar] [CrossRef]
- Elosua, R.; Garcia, M.; Aguilar, A.; Molina, L.; Covas, M.I.; Marrugat, J. Validation of the Minnesota Leisure Time Physical Activity Questionnaire In Spanish Women. Investigators of the MARATDON Group. Med. Sci. Sports Exerc. 2000, 32, 1431–1437. [Google Scholar] [CrossRef]
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish men. The MARATHOM Investigators. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Caparello, G.; Galluccio, A.; Giordano, C.; Lofaro, D.; Barone, I.; Morelli, C.; Sisci, D.; Catalano, S.; Ando, S.; Bonofiglio, D. Adherence to the Mediterranean diet pattern among university staff: A cross-sectional web-based epidemiological study in Southern Italy. Int. J. Food Sci. Nutr. 2019, 71, 1–12. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Martinez-Gonzalez, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Angelino, D.; Rosi, A.; Dall’Asta, M.; Bresciani, L.; Ferraris, C.; Guglielmetti, M.; Godos, J.; Del Bo, C.; et al. Effects of Popular Diets on Anthropometric and Cardiometabolic Parameters: An Umbrella Review of Meta-Analyses of Randomized Controlled Trials. Adv. Nutr. 2020, 11, 815–833. [Google Scholar] [CrossRef]
- Eckel, R.H.; Jakicic, J.M.; Ard, J.D.; de Jesus, J.M.; Houston Miller, N.; Hubbard, V.S.; Lee, I.M.; Lichtenstein, A.H.; Loria, C.M.; Millen, B.E.; et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 63, 2960–2984. [Google Scholar] [CrossRef]
- Davis, C.R.; Hodgson, J.M.; Woodman, R.; Bryan, J.; Wilson, C.; Murphy, K.J. A Mediterranean diet lowers blood pressure and improves endothelial function: Results from the MedLey randomized intervention trial. Am. J. Clin. Nutr. 2017, 105, 1305–1313. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef]
- Petersen, K.S.; Clifton, P.M.; Lister, N.; Keogh, J.B. Effect of Improving Dietary Quality on Arterial Stiffness in Subjects with Type 1 and Type 2 Diabetes: A 12 Months Randomised Controlled Trial. Nutrients 2016, 8, 382. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Wang, S.; Wang, D.; Lai, Q.; Chen, X.; Duan, S.; Zhao, M.; Huang, J. Combined moderate and high intensity exercise with dietary restriction improves cardiac autonomic function associated with a reduction in central and systemic arterial stiffness in obese adults: A clinical trial. PeerJ 2017, 5, e3900. [Google Scholar] [CrossRef][Green Version]
- Cunha, P.G.; Boutouyrie, P.; Nilsson, P.M.; Laurent, S. Early Vascular Ageing (EVA): Definitions and Clinical Applicability. Curr. Hypertens. Rev. 2017, 13, 8–15. [Google Scholar] [CrossRef]
- Kane, A.E.; Howlett, S.E. Differences in Cardiovascular Aging in Men and Women. Adv. Exp. Med. Biol. 2018, 1065, 389–411. [Google Scholar] [CrossRef]
- Rossi, P.; Francès, Y.; Kingwell, B.A.; Ahimastos, A.A. Gender differences in artery wall biomechanical properties throughout life. J. Hypertens. 2011, 29, 1023–1033. [Google Scholar] [CrossRef]
- Chester, R.; Sander, G.; Fernandez, C.; Chen, W.; Berenson, G.; Giles, T. Women have significantly greater difference between central and peripheral arterial pressure compared with men: The Bogalusa Heart Study. J. Am. Soc. Hypertens. 2013, 7, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Blanch, N.; Clifton, P.M.; Keogh, J.B. A systematic review of vascular and endothelial function: Effects of fruit, vegetable and potassium intake. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 253–266. [Google Scholar] [CrossRef] [PubMed]
- Klonizakis, M.; Alkhatib, A.; Middleton, G.; Smith, M.F. Mediterranean diet- and exercise-induced improvement in age-dependent vascular activity. Clin. Sci. (Lond) 2013, 124, 579–587. [Google Scholar] [CrossRef]
- Casado-Diaz, A.; Dorado, G.; Quesada-Gomez, J.M. Influence of olive oil and its components on mesenchymal stem cell biology. World J. Stem. Cells 2019, 11, 1045–1064. [Google Scholar] [CrossRef] [PubMed]
- Cesari, F.; Sofi, F.; Molino Lova, R.; Vannetti, F.; Pasquini, G.; Cecchi, F.; Marcucci, R.; Gori, A.M.; Macchi, C. Aging process, adherence to Mediterranean diet and nutritional status in a large cohort of nonagenarians: Effects on endothelial progenitor cells. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Liu, G.; Ding, M.; Zong, G.; Hu, F.B.; Willett, W.C.; Rimm, E.B.; Manson, J.E.; Sun, Q. Isoflavone Intake and the Risk of Coronary Heart Disease in US Men and Women: Results From 3 Prospective Cohort Studies. Circulation 2020, 141, 1127–1137. [Google Scholar] [CrossRef]
- Bando, M.; Masumoto, S.; Kuroda, M.; Tsutsumi, R.; Sakaue, H. Effect of olive oil consumption on aging in a senescence-accelerated mice-prone 8 (SAMP8) model. J. Med. Investig. 2019, 66, 241–247. [Google Scholar] [CrossRef]
| Global (2475) | Men (1524) | Women (951) | p Value | ||||
|---|---|---|---|---|---|---|---|
| Lifestyles | Mean or N | SD or (%) | Mean or N | SD or (%) | Mean or N | SD or (%) | |
| Years of smoker, (years) | 31.66 | 12.82 | 31.95 | 12.78 | 30.74 | 12.92 | 0.113 |
| Smoker, n (%) | 710 | (28.7) | 486 | (31.9) | 224 | (23.7) | <0.001 |
| Alcohol, (gr/W) | 71.87 | 116.74 | 102.01 | 132.71 | 23.58 | 58.86 | <0.001 |
| Risk consumption, n (%) | 334 | (13.5) | 284 | (18.6) | 50 | (5.3) | <0.001 |
| Total FA, (METs/m/W) | 2462 | 2495 | 2864 | 2815 | 1817 | 1683 | <0.001 |
| Sedentary, n (%) | 2127 | (85.9) | 1269 | (83.3) | 858 | (90.2) | <0.001 |
| MD, (total score) | 5.18 | 1.73 | 5.09 | 1.78 | 5.32 | 1.63 | 0.002 |
| Adherence MD, n (%) | 1295 | (52.4) | 781 | 51.2) | 514 | 54.0) | 0.186 |
| DQI, (total score) | 38.71 | 3.07 | 38.61 | 3.15 | 38.88 | 2.93 | 0.028 |
| Adherence DQI, n (%) | 1358 | (54.9) | 803 | (52.7) | 555 | (58.9) | 0.005 |
| Conventional Risk Factors | |||||||
| Age, (years) | 61.34 | 7.70 | 61.11 | 8.11 | 61.70 | 7.00 | 0.066 |
| SBP, (mmHg) | 137.25 | 17.37 | 139.09 | 17.05 | 134.32 | 17.48 | <0.001 |
| DBP, (mmHg) | 84.58 | 10.23 | 85.67 | 10.44 | 82.84 | 9.63 | <0.001 |
| BP, (mmHg) | 52.66 | 14.16 | 53.40 | 14.19 | 51.47 | 14.04 | 0.001 |
| MBP, (mmHg) | 101.89 | 11.21 | 103.23 | 11.17 | 99.74 | 10.95 | <0.001 |
| Hypertension, n (%) | 1795 | (72.5) | 1172 | (76.9) | 623 | (65.5) | <0.001 |
| Antihypertensive drugs, n (%) | 1272 | (51.4) | 786 | (50.4) | 504 | (53.0) | 0.215 |
| Total cholesterol, (mg/dL) | 225.53 | 41.07 | 220.39 | 38.92 | 233.77 | 43.05 | <0.001 |
| LDL cholesterol, (mg/dL) | 139.88 | 34.97 | 138.34 | 34.26 | 142.32 | 35.96 | 0.006 |
| HDL cholesterol, (mg/dL) | 49.81 | 13.03 | 47.89 | 11.96 | 52.90 | 14.04 | <0.001 |
| Triglycerides, (mg/dl) | 146.21 | 96.48 | 150.99 | 105.90 | 138.59 | 78.63 | 0.001 |
| No-HDL cholesterol, (mg/dL) | 175.74 | 40.74 | 172.54 | 38.34 | 180.86 | 43.84 | <0.001 |
| Atherogenic index, (mg/dL) | 4.76 | 1.31 | 4.82 | 1.30 | 4.67 | 1.34 | 0.004 |
| Dyslipidemia, n (%) | 1664 | (67.2) | 969 | (63.6) | 695 | (73.2) | <0.001 |
| Lipid–lowering drugs, n (%) | 717 | (29.0) | 419 | (27.5) | 298 | (31.3) | 0.045 |
| FPG, (mg/dL) | 107.98 | 34.83 | 107.76 | 33.90 | 108.35 | 36.29 | 0.683 |
| HbA1c, (%) | 6.12 | 1.18 | 6.06 | 1.12 | 6.21 | 1.26 | 0.002 |
| Diabetes mellitus, n (%) | 842 | (34.0) | 493 | (32.3) | 349 | (36.7) | 0.029 |
| Hypoglycaemic drugs, n (%) | 511 | (20.6) | 289 | (19.0) | 222 | (23.3) | 0.009 |
| Height, (cm) | 164.56 | 9.27 | 169.69 | 6.78 | 156.34 | 6.36 | <0.001 |
| Weight, (kg) | 79.41 | 14.67 | 83.81 | 13.52 | 72.36 | 13.67 | <0.001 |
| WC, (cm) | 100.95 | 11.68 | 102.94 | 10.52 | 97.76 | 12.69 | <0.001 |
| BMI, (kg/m2) | 29.26 | 4.52 | 29.06 | 3.95 | 29.59 | 5.28 | 0.004 |
| Obesity, n (%) | 897 | (26.2) | 510 | (33.5) | 387 | (40.7) | <0.001 |
| Abdominal obesity, n (%) | 1546 | (62.8) | 797 | (52.6) | 749 | (79.3) | <0.001 |
| Plasma creatine, (mg/dL) | 0.85 | 0.23 | 0.94 | 0.24 | 0.71 | 0.13 | <0.001 |
| GFR, (mL/min/1,73 m2) | 87.47 | 14.21 | 86.79 | 14.87 | 88.56 | 13.02 | 0.003 |
| CVR SCORE scale, (%) | 3.55 | 2.73 | 4.48 | 2.93 | 2.05 | 1.40 | <0.001 |
| Cardiovascular diseases | |||||||
| Renal disease, n (%) | 2 | (0.1) | 2 | (0.1) | 0 | 0.00 | 0.526 |
| Peripheral arteriopathy, n (%) | 13 | (0.5) | 11 | (0.7) | 2 | (0.2) | 0.150 |
| Heart failure, n (%) | 12 | (0.5) | 11 | (0.7) | 1 | (0.1) | 0.036 |
| Vascular function | |||||||
| baPWV, (m/s) | 14.87 | 2.63 | 14.82 | 2.65 | 14.93 | 2.60 | 0.313 |
| baPWV yes Adherence MD, (m/s) | 14.80 | 2.49 | 14.70 | 2.48 | 14.95 | 2.52 | 0.068 |
| baPWV non-Adherence MD, (m/s) | 14.93 | 2.78 | 14.96 | 2.83 | 14.90 | 2.69 | 0.760 |
| baPWV yes Adherence DQI (m/s) | 14.77 | 2.71 | 14.74 | 2.70 | 14.85 | 2.72 | 0.752 |
| baPWV non-Adherence DQI, (m/s) | 14.94 | 2.57 | 15.08 | 2.52 | 14.78 | 2.71 | 0.114 |
| Without EVA | (2210) | With EVA | (265) | p Value | |
|---|---|---|---|---|---|
| Lifestyles | Mean or N | SD or (%) | Mean or N | SD or (%) | |
| Years of smoker, (years) | 31.60 | 12.70 | 32.27 | 14.02 | 0.555 |
| Smoker, n (%) | 652 | (29.5) | 58 | (21.9) | 0.010 |
| Alcohol, (gr/W) | 70.75 | 111.72 | 81.28 | 152.23 | 0.276 |
| Risk consumption, n (%) | 296 | (13.4) | 38 | (14.3) | 0.636 |
| Total FA, (METs/m/W) | 2461 | 2449 | 2464 | 2861 | 0.986 |
| Sedentary, n (%) | 1893 | (85.7) | 234 | (88.9) | 0.263 |
| MD, (total score) | 5.20 | 1.721 | 4.98 | 1.771 | 0.056 |
| Adherence MD, n (%) | 1172 | (53.0) | 123 | (46.4) | 0.044 |
| DQI, (total score) | 38.78 | 3.04 | 38.11 | 3.21 | 0.001 |
| Adherence DQI, n (%) | 1233 | (55.8) | 125 | (47.2) | 0.009 |
| Conventional Risk Factors | |||||
| Age, (years) | 61.24 | 7.737 | 62.13 | 7.397 | 0.076 |
| SBP, (mmHg) | 135.57 | 16.15 | 151.27 | 20.57 | <0.001 |
| DBP, (mmHg) | 84.00 | 9.92 | 89.40 | 11.42 | <0.001 |
| BP, (mmHg) | 51.56 | 13.38 | 61.88 | 16.86 | <0.001 |
| MBP, (mmHg) | 100.94 | 10.62 | 109.77 | 12.83 | <0.001 |
| Hypertension, n (%) | 1554 | (70.3) | 241 | (90.9) | <0.001 |
| Antihypertensive drugs, n (%) | 1113 | (50.4) | 159 | (60.0) | 0.003 |
| Total cholesterol, (mg/dL) | 226.20 | 41.03 | 219.96 | 40.99 | 0.019 |
| LDL cholesterol, (mg/dL) | 140.78 | 34.92 | 132.35 | 34.61 | <0.001 |
| HDL cholesterol, (mg/dL) | 49.80 | 12.93 | 49.88 | 13.80 | 0.928 |
| Triglycerides, (mg/dL) | 144.43 | 91.44 | 161.23 | 130.80 | 0.008 |
| No-HDL cholesterol, (mg/dL) | 176.42 | 40.68 | 170.08 | 40.84 | 0.017 |
| Atherogenic index, (mg/dL) | 4.78 | 1.32 | 4.63 | 1.27 | 0.090 |
| Dyslipidemia, n (%) | 1496 | (67.7) | 168 | (63.4) | 0.166 |
| Lipid–lowering drugs, n (%) | 635 | (28.7) | 82 | (30.9) | 0.474 |
| FPG, (mg/dL) | 121.04 | 42.47 | 106.42 | 33.474 | <0.001 |
| HbA1c, (%) | 6.06 | 1.14 | 6.59 | 1.36961 | <0.001 |
| Diabetes mellitus, n (%) | 710 | (32.1) | 132 | (49.8) | <0.001 |
| Hypoglycaemic drugs, n (%) | 413 | (18.7) | 98 | (37.0) | <0.001 |
| Height, (cm) | 164.64 | 9.240 | 163.86 | 9.545 | 0.0198 |
| Weight, (kg) | 79.50 | 14.72 | 78.61 | 14.29 | 0.349 |
| WC, (cm) | 100.87 | 11.78 | 101.60 | 10.80 | 0.340 |
| BMI, (kg/m2) | 29.27 | 4.53 | 29.21 | 4.37 | 0.848 |
| Obesity, n (%) | 800 | (36.2) | 97 | (36.6) | 0.893 |
| Abdominal obesity, n (%) | 1371 | (62.5) | 175 | (66.0) | 0.256 |
| Plasma creatine, (mg/dL) | 0.85 | 0.19 | 0.89 | 0.4168872 | 0.004 |
| GFR, (mL/min/1,73 m2) | 87.63 | 13.85 | 86.13 | 16.86132 | 0.104 |
| CVR SCORE scale, (%) | 3.41 | 2.59 | 4.66 | 3.48391 | <0.001 |
| Cardiovascular diseases | |||||
| Renal disease, n (%) | 0 | (0.0) | 2 | (0.8) | <0.001 |
| Peripheral arteriopathy | 0 | (0.0) | 13 | (4.9) | <0.001 |
| Heart failure | 0 | (0.0) | 12 | (4.5) | <0.001 |
| Vascular function | |||||
| baPWV, (m/s) | 14.32 | 1.93 | 19.46 | 3.21 | <0.001 |
| β | 95% CI | p Value | |
|---|---|---|---|
| DQI | |||
| Total | −0.081 | (−0.105 to −0.028) | 0.001 |
| Men | −0.118 | (−0.145 to −0.054) | <0.001 |
| Women | 0.067 | (−0.020 to 0.118) | 0.162 |
| MD | |||
| Total | −0.052 | (−0.141 to −0.008) | 0.027 |
| Men | −0.081 | (−0.198 to −0.040) | 0.003 |
| Women | 0.066 | (−0.036 to 0.204) | 0.168 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Sánchez, L.; Rodríguez-Sánchez, E.; Ramos, R.; Marti-Lluch, R.; Gómez-Sánchez, M.; Lugones-Sánchez, C.; Tamayo-Morales, O.; Llamas-Ramos, I.; Rigo, F.; García-Ortiz, L.; et al. The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk—A MARK Study. Nutrients 2022, 14, 244. https://doi.org/10.3390/nu14020244
Gómez-Sánchez L, Rodríguez-Sánchez E, Ramos R, Marti-Lluch R, Gómez-Sánchez M, Lugones-Sánchez C, Tamayo-Morales O, Llamas-Ramos I, Rigo F, García-Ortiz L, et al. The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk—A MARK Study. Nutrients. 2022; 14(2):244. https://doi.org/10.3390/nu14020244
Chicago/Turabian StyleGómez-Sánchez, Leticia, Emiliano Rodríguez-Sánchez, Rafel Ramos, Ruth Marti-Lluch, Marta Gómez-Sánchez, Cristina Lugones-Sánchez, Olaya Tamayo-Morales, Ines Llamas-Ramos, Fernando Rigo, Luis García-Ortiz, and et al. 2022. "The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk—A MARK Study" Nutrients 14, no. 2: 244. https://doi.org/10.3390/nu14020244
APA StyleGómez-Sánchez, L., Rodríguez-Sánchez, E., Ramos, R., Marti-Lluch, R., Gómez-Sánchez, M., Lugones-Sánchez, C., Tamayo-Morales, O., Llamas-Ramos, I., Rigo, F., García-Ortiz, L., & Gómez-Marcos, M. A. (2022). The Association of Dietary Intake with Arterial Stiffness and Vascular Ageing in a Population with Intermediate Cardiovascular Risk—A MARK Study. Nutrients, 14(2), 244. https://doi.org/10.3390/nu14020244






