The Effects of Breastfeeding for Four Months on Thinness, Overweight, and Obesity in Children Aged 3 to 6 Years: A Retrospective Cohort Study from National Physical Fitness Surveillance of Jiangsu Province, China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Data Collection
2.3. Measurements and Definition
2.3.1. Outcomes or Dependent Variables
2.3.2. Feeding Patterns and Covariates
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics and Univariate Analysis on Thinness, Overweight, and Obesity
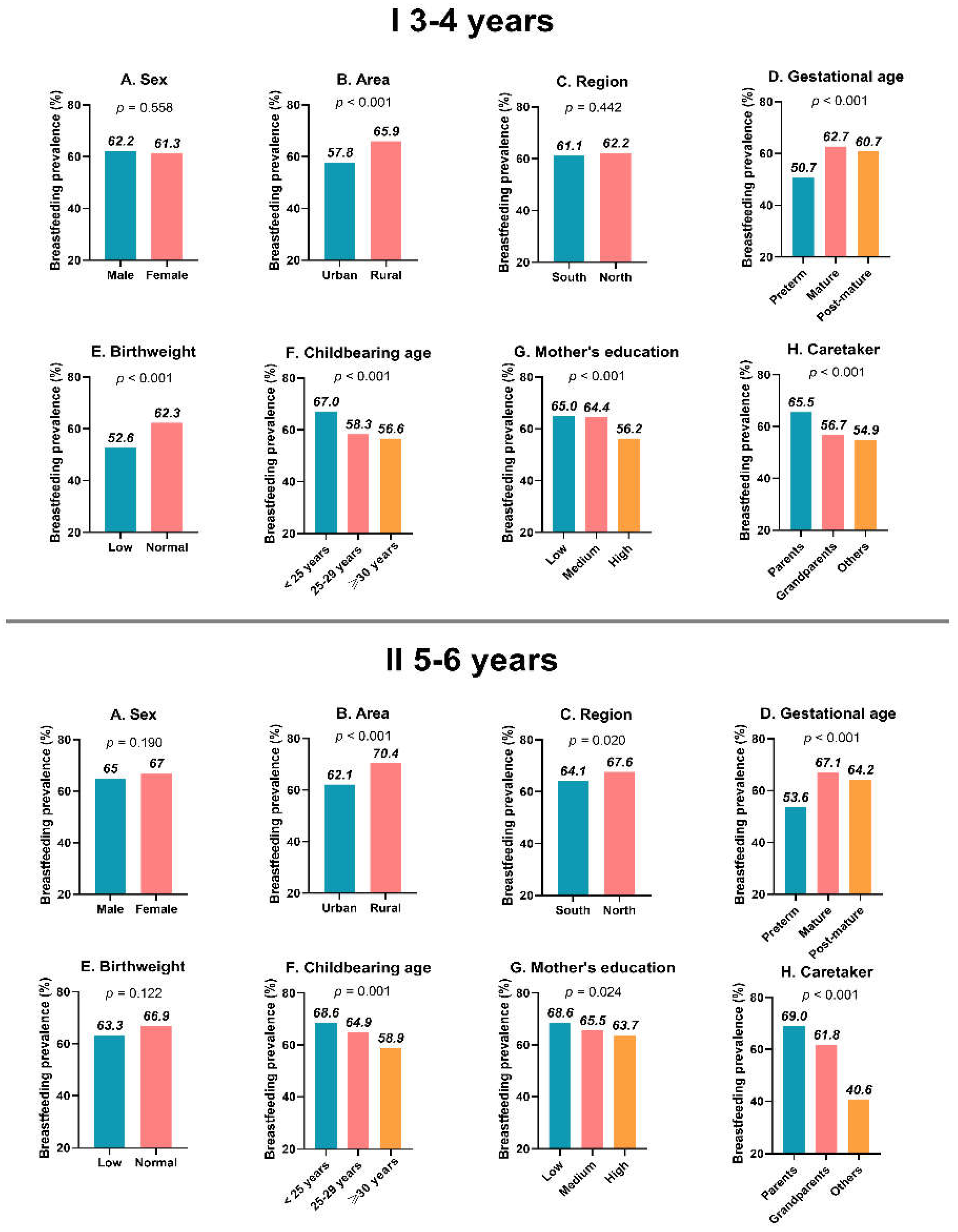
3.2. The Prevalence of Breastfeeding in Subgroups of Covariates
3.3. Mean Distribution of BMI in Subgroups of Covariates
3.4. Association among Breastfeeding, Thinness, Overweight, and Obesity in Multivariate Logistic Regression Models
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Category | Thinness | p | Overweight | p | Obesity | p | Overweight/Obesity | p |
|---|---|---|---|---|---|---|---|---|
| Feeding patterns | ||||||||
| formula feeding | Ref | Ref | Ref | Ref | ||||
| mixed feeding | 1.225 (0.943, 1.593) | 0.129 | 0.855 (0.698, 1.048) | 0.131 | 1.063 (0.826, 1.368) | 0.637 | 0.917 (0.769, 1.094) | 0.335 |
| breastfeeding | 1.307 (1.044, 1.637) | 0.020 | 0.755 (0.635, 0.898) | 0.001 | 0.867 (0.696, 1.081) | 0.205 | 0.758 (0.652, 0.882) | <0.001 |
| Sex | ||||||||
| male | Ref | Ref | Ref | Ref | ||||
| female | 1.150 (0.993, 1.333) | 0.062 | 0.684 (0.603, 0.777) | <0.001 | 0.527 (0.449, 0.618) | <0.001 | 0.562 (0.504, 0.626) | <0.001 |
| Age grade | ||||||||
| 3 years | Ref | Ref | Ref | Ref | ||||
| 4 years | 0.821 (0.671, 1.005) | 0.056 | 1.002 (0.844, 1.190) | 0.982 | 0.940 (0.751, 1.176) | 0.588 | 0.974 (0.839, 1.131) | 0.730 |
| 5 years | 0.829 (0.679, 1.014) | 0.068 | 0.939 (0.790, 1.117) | 0.478 | 1.150 (0.927, 1.426) | 0.203 | 1.020 (0.879, 1.183) | 0.792 |
| 6 years | 0.802 (0.649, 0.992) | 0.042 | 0.875 (1.167, 1.799) | 0.159 | 1.330 (1.066, 1.659) | 0.012 | 1.048 (0.896, 1.225) | 0.557 |
| Area | ||||||||
| urban | Ref | Ref | Ref | Ref | ||||
| rural | 1.389 (1.183, 1.631) | <0.001 | 0.776 (0.676, 0.891) | <0.001 | 0.669 (0.564, 0.795) | <0.001 | 0.688 (0.611, 0.773) | <0.001 |
| Region/economy a | ||||||||
| south/developed | Ref | Ref | Ref | Ref | ||||
| north/less-developed | 0.686 (0.592, 0.796) | <0.001 | 1.421 (1.249, 1.615) | <0.001 | 1.713 (1.457, 2.012) | <0.001 | 1.662 (1.489, 1.854) | <0.001 |
| Gestational age | ||||||||
| preterm | Ref | Ref | Ref | Ref | ||||
| mature | 1.264 (0.920, 1.735) | 0.148 | 0.717 (0.561, 0.918) | 0.008 | 0.876 (0.637, 1.207) | 0.419 | 0.731 (0.588, 0.908) | 0.005 |
| post-mature | 1.114 (0.706, 1758) | 0.642 | 0.813 (0.569, 1.161) | 0.255 | 1.077 (0.695, 1.669) | 0.739 | 0.889 (0.653, 1.209) | 0.453 |
| Birthweight b | ||||||||
| low | Ref | Ref | Ref | Ref | ||||
| normal | 0.635 (0.520, 0.775) | <0.001 | 1.331 (1.087, 1.630) | 0.006 | 1.561 (1.196, 2.039) | 0.001 | 1.507 (1.267, 1.792) | <0.001 |
| Childbearing age | ||||||||
| <25 years | Ref | Ref | Ref | Ref | ||||
| 25–29 years | 1.264 (0.920, 1.735) | 0.148 | 0.844 (0.733, 0.971) | 0.018 | 0.974 (0.822, 1.154) | 0.757 | 0.873 (0.775, 0.983) | 0.025 |
| ≥30 years | 1.114 (0.706, 1.758) | 0.642 | 1.057 (0.863, 1.293) | 0.594 | 0.797 (0.608, 1.045) | 0.101 | 0.941 (0.788, 1.125) | 0.506 |
| Mother’s education c | ||||||||
| low | Ref | Ref | Ref | Ref | ||||
| medium | 1.032 (0.856, 1.245) | 0.738 | 1.061 (0.901, 1.250) | 0.476 | 1.131 (0.921, 1.387) | 0.240 | 1.108 (0.963, 1.274) | 0.152 |
| high | 0.960 (0.787, 1.172) | 0.691 | 1.023 (0.862, 1.214) | 0.796 | 1.069 (0.864, 1.323) | 0.540 | 1.048 (0.906, 1.214) | 0.528 |
| Caretaker | ||||||||
| parents | Ref | Ref | Ref | Ref | ||||
| grandparents | 0.862 (0.736, 1.011) | 0.067 | 0.973(0.851, 1.113) | 0.692 | 1.070 (0.908, 1.262) | 0.418 | 1.011 (0.902, 1.133) | 0.855 |
| others | 1.253 (0.787, 1.994) | 0.342 | 0.664 (0.422, 1.046) | 0.077 | 1.301 (0.820, 2.064) | 0.264 | 0.868 (0.608, 1.240) | 0.438 |
References
- Olds, T.; Schranz, N.; Maher, C. Secular trends in the prevalence of childhood overweight and obesity across Australian states: A meta-analysis. J. Sci. Med. Sport 2017, 20, 480–488. [Google Scholar]
- Lobstein, T.; Rugby, N.; Leach, R. Obesity in Europe-3 International Obesity Task Force; European Association for the Study of Obesity: Brussels, Belgium, 2005. [Google Scholar]
- Mazur, A.; Klimek, K.; Telega, G.; Filip, R.; Malecka-Tendera, E. Ten-year secular trend of overweight and obesity in school children in south-eastern Poland. Ann. Agric. Environ. Med. 2014, 21, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Shirasawa, T.; Ochiai, H.; Nanri, H.; Nishimura, R.; Ohtsu, T.; Hoshino, H.; Tajima, N.; Kokaze, A. Trends of underweight and overweight/obesity among Japanese schoolchildren from 2003 to 2012, defined by body mass index and percentage overweight cutoffs. J. Epidemiol. 2015, 25, JE20140144. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, R.C.; Wright, J.A.; Pepe, M.S.; Seidel, K.D.; Dietz, W.H. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 1997, 337, 869–873. [Google Scholar] [CrossRef]
- World Health Organization. Why Does Childhood Overweight and Obesity Matter; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Doak, C.M.; Adair, L.S.; Monteiro, C.; Popkin, B.M. Overweight and underweight coexist within households in Brazil, China and Russia. J. Nutr. 2000, 130, 2965–2971. [Google Scholar] [CrossRef]
- Zhang, Y.-X.; Wang, Z.-X.; Wang, M.; Xie, L. Prevalence of thinness among children and adolescents in Shandong, China. Eur. J. Nutr. 2016, 55, 809–813. [Google Scholar] [CrossRef]
- Kolčić, I. Double burden of malnutrition: A silent driver of double burden of disease in low–and middle–income countries. J. Glob. Health 2012, 2, 020303. [Google Scholar] [CrossRef]
- Pray, L.A. Examining a Developmental Approach to Childhood Obesity: The Fetal and Early Childhood Years: Workshop Summary; National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Zheng, J.-S.; Liu, H.; Li, J.; Chen, Y.; Wei, C.; Shen, G.; Zhu, S.; Chen, H.; Zhao, Y.-M.; Huang, T. Exclusive breastfeeding is inversely associated with risk of childhood overweight in a large Chinese cohort. J. Nutr. 2014, 144, 1454–1459. [Google Scholar] [CrossRef]
- Umer, A.; Hamilton, C.; Britton, C.M.; Mullett, M.D.; John, C.; Neal, W.; Lilly, C.L. Association between breastfeeding and childhood obesity: Analysis of a linked longitudinal study of rural Appalachian fifth-grade children. Child. Obes. 2015, 11, 449–455. [Google Scholar] [CrossRef]
- Gibbs, B.G.; Forste, R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr. Obes. 2014, 9, 135–146. [Google Scholar] [CrossRef]
- Jwa, S.C.; Fujiwara, T.; Kondo, N. Latent protective effects of breastfeeding on late childhood overweight and obesity: A nationwide prospective study. Obesity 2014, 22, 1527–1537. [Google Scholar] [CrossRef]
- Horta, B.L.; Bahl, R.; Martinés, J.C.; Victora, C.G.; World Health Organization. Evidence on the Long-Term Effects of Breastfeeding: Systematic Review and Meta-Analyses; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Yan, J.; Liu, L.; Zhu, Y.; Huang, G.; Wang, P.P. The association between breastfeeding and childhood obesity: A meta-analysis. BMC Public Health 2014, 14, 1267. [Google Scholar] [CrossRef]
- Qiao, J.; Dai, L.-J.; Zhang, Q.; Ouyang, Y.-Q. A meta-analysis of the association between breastfeeding and early childhood obesity. J. Pediatr. Nurs. 2020, 53, 57–66. [Google Scholar] [CrossRef]
- Beyerlein, A.; von Kries, R. Breastfeeding and body composition in children: Will there ever be conclusive empirical evidence for a protective effect against overweight? Am. J. Clin. Nutr. 2011, 94 (Suppl. 6), 1772S–1775S. [Google Scholar] [CrossRef]
- Cope, M.B.; Allison, D.B. Critical review of the World Health Organization’s (WHO) 2007 report on ‘evidence of the long-term effects of breastfeeding: Systematic reviews and meta-analysis’ with respect to obesity. Obes. Rev. 2008, 9, 594–605. [Google Scholar] [CrossRef]
- Kwok, M.K.; Schooling, C.M.; Lam, T.H.; Leung, G.M. Does breastfeeding protect against childhood overweight? Hong Kong’s ‘Children of 1997′birth cohort. Int. J. Epidemiol. 2010, 39, 297–305. [Google Scholar] [CrossRef]
- Huus, K.; Ludvigsson, J.F.; Enskär, K.; Ludvigsson, J. Exclusive breastfeeding of Swedish children and its possible influence on the development of obesity: A prospective cohort study. BMC Pediatr. 2008, 8, 42. [Google Scholar] [CrossRef]
- Kramer, M.S.; Matush, L.; Vanilovich, I.; Platt, R.W.; Bogdanovich, N.; Sevkovskaya, Z.; Dzikovich, I.; Shishko, G.; Collet, J.-P.; Martin, R.M. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: Evidence from a large randomized trial. Am. J. Clin. Nutr. 2007, 86, 1717–1721. [Google Scholar] [CrossRef]
- Usheva, N.; Lateva, M.; Galcheva, S.; Koletzko, B.V.; Cardon, G.; De Craemer, M.; Androutsos, O.; Kotowska, A.; Socha, P.; Moreno, L.A. Breastfeeding and overweight in European preschoolers: The ToyBox study. Nutrients 2021, 13, 2880. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- State Physical Culture Administration. National Physical Fitness Evaluation Standard. People’s Physical Culture Publishing House: Beijing, China, 2003; pp. 2–24. (In Chinese) [Google Scholar]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Zhang, R.; Zhang, S.; Shi, W.; Yan, W.; Wang, X.; Lyu, Q.; Liu, L.; Zhou, Q.; Qiu, Q.; et al. Chinese neonatal birth weight curve for different gestational age. Chin. J. Pediatr. 2015, 53, 97–103. [Google Scholar]
- Ehrenthal, D.B.; Wu, P.; Trabulsi, J. Differences in the protective effect of exclusive breastfeeding on child overweight and obesity by mother’s race. Matern. Child Health J. 2016, 20, 1971–1979. [Google Scholar] [CrossRef]
- Li, Q.; Tian, J.; Xu, F.; Binns, C. Breastfeeding in China: A review of changes in the past decade. Int. J. Environ. Res. Public Health 2020, 17, 8234. [Google Scholar] [CrossRef]
- Yang, M.; Liu, N.; Yang, C.; Zheng, X.; Xiong, C.; Yang, S.; Du, Y.; Zhang, J. Analysis on the effect factors of pure breastfeeding among the rural infants in five provinces of Western China. Matern. Child Health Care China 2012, 27, 1035–1037. [Google Scholar]
- Qin, H.; Zhang, L.; Zhang, L.; Zhang, W.; Li, L.; Deng, X.; Tian, D.; Deng, J.; Hu, G. Prevalence of breastfeeding: Findings from the first health service household interview in Hunan Province, China. Int. J. Environ. Res. Public Health 2017, 14, 150. [Google Scholar] [CrossRef]
- Armstrong, J.; Reilly, J.; Child Health Information Team. Breastfeeding and lowering the risk of childhood obesity. Lancet 2002, 359, 2003–2004. [Google Scholar] [CrossRef]
- Pelletier, D.L.; Frongillo, E.A. Changes in child survival are strongly associated with changes in malnutrition in developing countries. J. Nutr. 2003, 133, 107–119. [Google Scholar] [CrossRef]
- El-Ghannam, A.R. The global problems of child malnutrition and mortality in different world regions. J. Health Soc. Policy 2003, 16, 1–26. [Google Scholar] [CrossRef]
- Abarca-Gómez, L.; Abdeen, Z.; Hamid, Z.; Abu-Rmeileh, N.; Acosta-Cazares, B.; Acuin, C.; Adams, R.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C. Non-Communicable Disease Risk Factor Collaboration Worldwide Trends in Body Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128.9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar]
- Torres, A.L.; Estrella, A.; Rivadeneira, M.F.; Astudillo, F.; Buitron, J.; Tello, B.; Moncayo, A.L. Breastfeeding, feeding practices and stunting in indigenous Ecuadorians under 2 years of age. BMC 2022. [Google Scholar]
- Owen, C.G.; Martin, R.M.; Whincup, P.H.; Smith, G.D.; Cook, D.G. Effect of infant feeding on the risk of obesity across the life course: A quantitative review of published evidence. Pediatrics 2005, 115, 1367–1377. [Google Scholar] [CrossRef]
- Grêaux, K.; Schwiebbe, L.; Renders, C.M.; Doak, C.M.; Visser, R.; Holthe, J.K.-V.; HiraSing, R.A. Breastfeeding and food pattern in overweight children in the Caribbean. Paediatr. Int. Child Health 2013, 33, 18–22. [Google Scholar] [CrossRef]
- Weber, M.; Grote, V.; Closa-Monasterolo, R.; Escribano, J.; Langhendries, J.-P.; Dain, E.; Giovannini, M.; Verduci, E.; Gruszfeld, D.; Socha, P. Lower protein content in infant formula reduces BMI and obesity risk at school age: Follow-up of a randomized trial. Am. J. Clin. Nutr. 2014, 99, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.E.; Kim, J.; Mathai, R.A.; Team, S.K.R. Associations of infant feeding practices and picky eating behaviors of preschool children. J. Am. Diet. Assoc. 2011, 111, 1363–1368. [Google Scholar] [CrossRef] [PubMed]
- Procter, S.B.; Holcomb, C.A. Breastfeeding duration and childhood overweight among low-income children in Kansas, 1998–2002. Am. J. Public Health 2008, 98, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Grummer-Strawn, L.M.; Mei, Z. Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics 2004, 113, e81–e86. [Google Scholar] [CrossRef] [PubMed]
- Wallby, T.; Lagerberg, D.; Magnusson, M. Relationship between breastfeeding and early childhood obesity: Results of a prospective longitudinal study from birth to 4 years. Breastfeed. Med. 2017, 12, 48–53. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Total n (%) | Thinness n (%) | p | Overweight n (%) | p | Obesity n (%) | p | Overweight /Obesity n (%) | p |
|---|---|---|---|---|---|---|---|---|---|
| Feeding patterns | 0.066 | <0.001 | 0.042 | <0.001 | |||||
| breastfeeding | 5140 (63.8) | 155 (3.0) | 522 (10.2) | 229 (4.5) | 751 (14.6) | ||||
| mixed feeding | 1638 (20.3) | 33 (2.0) | 203 (12.4) | 97 (5.9) | 300 (18.3) | ||||
| formula feeding | 1275 (15.9) | 30 (2.4) | 174 (13.6) | 56 (4.4) | 230 (18.0) | ||||
| Sex | 0.003 | 0.028 | 0.001 | <0.001 | |||||
| male | 4022 (49.9) | 87 (2.2) | 480 (11.9) | 223 (5.5) | 703 (17.5) | ||||
| female | 4031 (51.1) | 131 (3.2) | 419 (10.4) | 159 (3.9) | 578 (14.3) | ||||
| Age grade | 0.001 | 0.21 | 0.005 | <0.001 | |||||
| 3 years | 2067 (25.7) | 82 (4.0) | 205 (9.9) | 87 (4.2) | 292 (14.1) | ||||
| 4 years | 2040 (25.3) | 48 (2.4) | 214 (10.5) | 76 (3.7) | 290 (14.2) | ||||
| 5 years | 2149 (26.7) | 51 (2.4) | 249 (11.6) | 112 (5.2) | 361 (16.8) | ||||
| 6 years | 1797 (22.3) | 37 (2.1) | 231 (12.9) | 107 (6.0) | 338 (18.8) | ||||
| Area | 0.001 | <0.001 | <0.001 | <0.001 | |||||
| urban | 4219 (52.4) | 89 (2.1) | 545 (12.9) | 241 (5.7) | 786 (18.6) | ||||
| rural | 3843 (47.6) | 129 (3.4) | 354 (9.2) | 141 (3.7) | 495 (12.9) | ||||
| Region/economy a | 0.093 | <0.001 | <0.001 | <0.001 | |||||
| south/developed | 3468 (44.4) | 109 (3.0) | 300 (8.4) | 119 (3.3) | 419 (11.7) | ||||
| north/less-developed | 4476 (55.6) | 109 (2.4) | 599 (13.4) | 263 (5.9) | 862 (19.3) | ||||
| Gestational age | 0.017 | 0.137 | 0.328 | 0.133 | |||||
| preterm | 538 (6.7) | 24 (4.5) | 56 (10.4) | 32 (5.9) | 88 (16.4) | ||||
| mature | 7087 (88.1) | 187 (2.6) | 784 (11.1) | 327 (4.6) | 1111 (15.7) | ||||
| post-mature | 419 (5.2) | 7 (1.7) | 59 (14.1) | 22 (5.3) | 81 (19.3) | ||||
| Birthweight b | <0.001 | <0.001 | 0.153 | <0.001 | |||||
| low | 1045 (13.2) | 44 (4.2) | 73 (7.0) | 40 (3.8) | 113 (10.8) | ||||
| normal | 6871 (86.8) | 165 (2.4) | 811 (11.8) | 337 (4.9) | 1148 (16.7) | ||||
| Childbearing age | 0.036 | 0.774 | 0.771 | 0.785 | |||||
| <25 years | 3553 (44.4) | 106 (3.0) | 394 (11.1) | 161 (4.5) | 555 (15.6) | ||||
| 25–29 years | 3472 (43.4) | 87 (2.5) | 382 (11.0) | 170 (4.9) | 552 (15.9) | ||||
| ≥30 years | 974 (12.2) | 23 (2.4) | 115 (11.8) | 46 (4.7) | 161 (16.5) | ||||
| Mother’s education c | 0.804 | 66 | 0.027 | 0.285 | 0.025 | ||||
| low | 2748 (34.1) | 79 (2.9) | 278 (10.1) | 119 (4.3) | 397 (14.4) | ||||
| medium | 2627 (32.6) | 69 (2.6) | 326 (12.4) | 123 (4.7) | 449 (17.1) | ||||
| high | 2672 (33.2) | 70 (2.6) | 294 (11.0) | 140 (5.2) | 434 (16.2) | ||||
| Caretaker | 0.215 | 0.180 | 0.058 | 0.680 | |||||
| parents | 5000 (62.1) | 146 (2.9) | 583 (11.7) | 217 (4.3) | 800 (16.0) | ||||
| grandparents | 2838 (35.3) | 65 (2.3) | 292 (10.3) | 151 (5.3) | 443 (15.6) | ||||
| others | 208 (2.6) | 7 (3.4) | 23 (11.1) | 14 (6.7) | 37 (17.8) |
| Category | Thinness | p | Overweight | p | Obesity | p | Overweight/ Obesity | p |
|---|---|---|---|---|---|---|---|---|
| Feeding patterns | ||||||||
| formula feeding | Ref | Ref | Ref | Ref | ||||
| mixed feeding | 0.682 (0.392, 1.186) | 0.175 | 0.842 (0.665, 1.064) | 0.150 | 1.330 (0.918, 1.926) | 0.132 | 0.960 (0.780, 1.181) | 0.698 |
| breastfeeding | 1.179 (0.772, 1.801) | 0.446 | 0.652 (0.533, 0.797) | <0.001 | 1.016 (0.729, 1.415) | 0.926 | 0.721 (0.602, 0.862) | <0.001 |
| Sex | ||||||||
| male | Ref | Ref | Ref | Ref | ||||
| female | 1.566 (1.159, 2.117) | 0.004 | 0.867 (0.747, 1.006) | 0.061 | 0.675 (0.538, 0.846) | 0.001 | 0.786 (0.691, 0.895) | <0.001 |
| Age grade | ||||||||
| 3 years | Ref | Ref | Ref | Ref | ||||
| 4 years | 0.582 (0.396, 0.857) | 0.006 | 1.066 (0.859, 1.324) | 0.562 | 0.807 (0.571, 1.140) | 0.223 | 0.985 (0.815, 1.191) | 0.875 |
| 5 years | 0.497 (0.334, 0.742) | 0.001 | 1.202 (0.972, 1.486) | 0.089 | 1.367 (1.004, 1.861) | 0.047 | 1.277 (1.064, 1.533) | 0.008 |
| 6 years | 0.444 (0.287, 0.687) | <0.001 | 1.449 (1.167, 1.799) | 0.001 | 1.589 (1.159, 2.177) | 0.004 | 1.549 (1.285, 1.866) | <0.001 |
| Area | ||||||||
| urban | Ref | Ref | Ref | Ref | ||||
| rural | 1.507 (1.091, 2.082) | 0.013 | 0.744 (0.631, 0.878) | <0.001 | 0.661 (0.515, 0.849) | 0.001 | 0.698 (0.605, 0.805) | <0.001 |
| Region/economy a | ||||||||
| south/developed | Ref | Ref | Ref | Ref | ||||
| north/less-developed | 0.792 (0.588, 1.067) | 0.125 | 1.620 (1.387, 1.892) | <0.001 | 1.868 (1.474, 2.368) | <0.001 | 1.769 (1.545, 2.024) | <0.001 |
| Gestational age | ||||||||
| preterm | Ref | Ref | Ref | Ref | ||||
| mature | 0.633 (0.384, 1.044) | 0.073 | 0.962 (0.697, 1.327) | 0.812 | 0.651 (0.432, 0.982) | 0.041 | 0.823 (0.630, 1.075) | 0.153 |
| post-mature | 0.409 (0.159, 1.049) | 0.063 | 1.347 (0.879, 2.062) | 0.171 | 0.676 (0.363, 1.257) | 0.216 | 1.085 (0.752, 1.566) | 0.662 |
| Birthweight b | ||||||||
| low | Ref | Ref | Ref | Ref | ||||
| normal | 0.614 (0.418, 0.901) | 0.013 | 1.804 (1.374, 2.368) | <0.001 | 1.324 (0.918, 1.909) | 0.133 | 1.689 (1.348, 2.116) | <0.001 |
| Childbearing age | ||||||||
| <25 years | Ref | Ref | Ref | Ref | ||||
| 25–29 years | 0.810 (0.584, 1.122) | 0.205 | 0.910 (0.771, 1.074) | 0.264 | 0.991 (0.776, 1.267) | 0.994 | 0.929 (0.805, 1.072) | 0.314 |
| ≥30 years | 0.664 (0.388, 1.136) | 0.135 | 1.008 (0.789, 1.288) | 0.950 | 0.873 (0.591, 1.289) | 0.494 | 0.963 (0.775, 1.195) | 0.730 |
| Mother’s education c | ||||||||
| low | Ref | Ref | Ref | Ref | ||||
| medium | 1.068 (0.732, 1.557) | 0.733 | 1.217 (1.002, 1.478) | 0.048 | 0.882 (0.655, 1.187) | 0.407 | 1.115 (0.941, 1.321) | 0.209 |
| high | 1.180 (0.794, 1.755) | 0.413 | 1.024 (0.833, 1.260) | 0.820 | 0.968 (0.716, 1.309) | 0.834 | 1.010 (0.845, 1.207) | 0.961 |
| Caretaker | ||||||||
| parents | Ref | Ref | Ref | Ref | ||||
| grandparents | 0.713 (0.514, 0.990) | 0.044 | 0.870 (0.739, 1.023) | 0.092 | 1.354 (1.072, 1.710) | 0.011 | 1.001 (0.871, 1.150) | 0.994 |
| others | 1.751 (0.793, 3.863) | 0.166 | 0.834 (0.509, 1.368) | 0.473 | 1.487 (0.783, 2.824) | 0.225 | 1.008 (0.996, 1.524) | 0.971 |
| Category | Thinness | p | Overweight | p | Obesity | p | Overweight/Obesity | p |
|---|---|---|---|---|---|---|---|---|
| Total | 1.179 (0.772, 1.801) | 0.446 | 0.652 (0.533, 0.797) | <0.001 | 1.016 (0.729, 1.415) | 0.926 | 0.721 (0.602, 0.862) | <0.001 |
| Sex | ||||||||
| male | 0.966 (0.505, 1.848) | 0.918 | 0.621 (0.471, 0.820) | 0.001 | 0.946 (0.614, 1.457) | 0.801 | 0.681 (0.532, 0.871) | 0.002 |
| female | 1.362 (0.777, 2.390) | 0.281 | 0.697 (0.519, 0.937) | 0.017 | 1.170 (0.694, 1.970) | 0.556 | 0.773 (0.595, 1.005) | 0.054 |
| Age grade | ||||||||
| 3 years | 2.373 (0.991, 5.682) | 0.052 | 0.531 (0.350, 0.804) | 0.003 | 1.290 (0.612, 2.718) | 0.503 | 0.655 (0.452, 0.950) | 0.026 |
| 4 years | 0.685 (0.338, 1.387) | 0.293 | 0.466 (0.320, 0.680) | <0.001 | 0.618 (0.299, 1.281) | 0.196 | 0.478 (0.338, 0.675) | <0.001 |
| 5 years | 0.740 (0.310, 1.766) | 0.497 | 0.832 (0.551, 1.256) | 0.382 | 1.763 (0.875, 3.555) | 0.113 | 1.045 (0.723, 1.511) | 0.814 |
| 6 years | 1.687 (0.488, 5.833) | 0.408 | 0.996 (0.641, 1.548) | 0.986 | 0.758 (0.425, 1.354) | 0.350 | 0.892 (0.613, 1.297) | 0.550 |
| Area | ||||||||
| urban | 1.159 (0.615, 2.181) | 0.648 | 0.761 (0.585, 0.990) | 0.042 | 1.095 (0.721, 1.664) | 0.669 | 0.834 (0.660, 1.054) | 0.129 |
| rural | 1.130 (0.638, 2.000) | 0.675 | 0.534 (0.391, 0.728) | <0.001 | 0.959 (0.557, 1.651) | 0.881 | 0.607 (0.460, 0.801) | <0.001 |
| Region/economy a | ||||||||
| south/developed | 1.212 (0.668, 2.200) | 0.526 | 0.783 (0.558, 1.097) | 0.155 | 0.888 (0.513, 1.538) | 0.672 | 0.804 (0.598, 1.082) | 0.149 |
| north/less-developed | 1.096 (0.598, 2.008) | 0.768 | 0.587 (0.457, 0.755) | <0.001 | 1.098 (0.722, 1.669) | 0.662 | 0.680 (0.542, 0.853) | 0.001 |
| Gestational age | ||||||||
| preterm | 8.854 (1.096, 71.527) | 0.041 | 0.505 (0.244, 1.047) | 0.066 | 0.564 (0.226, 1.406) | 0.219 | 0.478 (0.259, 0.880) | 0.018 |
| mature | 0.932 (0.603, 1.440) | 0.750 | 0.645 (0.520, 0.801) | <0.001 | 1.099 (0.758, 1.593) | 0.618 | 0.730 (0.601, 0.886) | 0.001 |
| post-mature d | NA | - | 1.058 (0.405, 2.764) | 0.909 | 2.418 (0.277, 21.13) | 0.425 | 1.240 (0.502, 3.062) | 0.641 |
| Birthweight b | ||||||||
| low | 0.943 (0.396, 2.244) | 0.894 | 0.496 (0.263, 0.934) | 0.030 | 1.070 (0.400, 2.860) | 0.893 | 0.616 (0.356, 1.065) | 0.083 |
| normal | 1.241 (0.759, 2.027) | 0.390 | 0.670 (0.542, 0.829) | <0.001 | 1.012 (0.710, 1.441) | 0.949 | 0.734 (0.607, 0.888) | 0.001 |
| Childbearing age | ||||||||
| <25 years | 0.977 (0.537, 1.779) | 0.941 | 0.548 (0.402, 0.747) | <0.001 | 1.009 (0.608, 1.673) | 0.973 | 0.630 (0.478, 0.831) | 0.001 |
| 25–29 years | 2.334 (1.043, 5.223) | 0.039 | 0.759 (0.555, 1.038) | 0.084 | 1.013 (0.612, 1.676) | 0.959 | 0.814 (0.617, 1.074) | 0.145 |
| ≥30 years | 0.344 (0.144, 1.036) | 0.058 | 0.700 (0.418, 1.171) | 0.174 | 0.850 (0.331, 2.181) | 0.735 | 0.712 (0.446, 1.138) | 0.155 |
| Mother’s education c | ||||||||
| low | 1.026 (0.510, 2.062) | 0.943 | 0.641 (0.450, 0.915) | 0.014 | 1.112 (0.624, 1.983) | 0.719 | 0.739 (0.540, 1.013) | 0.060 |
| medium | 1.454 (0.640, 3.303) | 0.371 | 0.774 (0.550, 1.090) | 0.143 | 0.918 (0.526, 1.604) | 0.765 | 0.795 (0.585, 1.079) | 0.141 |
| high | 1.090 (0.529, 2.247) | 0.815 | 0.558 (0.392, 0.794) | 0.001 | 1.053 (0.580, 1.913) | 0.865 | 0.646 (0.470, 0.887) | 0.007 |
| Caretaker | ||||||||
| parents | 0.999 (0.599, 1.668) | 0.998 | 0.645 (0.502, 0.828) | 0.001 | 1.037 (0.667, 1.611) | 0.873 | 0.709 (0.565, 0.890) | 0.003 |
| grandparents | 1.275 (0.579, 2.808) | 0.546 | 0.588 (0.415, 0.834) | 0.003 | 0.946 (0.553, 1.619) | 0.840 | 0.658 (0.485, 0.893) | 0.007 |
| others | 2.004 (0.602, 6.674) | 0.258 | 3.235 (0.671, 15.60) | 0.144 | 2.353 (0.352,15.73) | 0.377 | 2.741 (0.809, 9.288) | 0.105 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, H.; Gao, Y.; Zhu, N.; Yuan, G.; Li, X.; Feng, Y.; Gao, L.; Yu, J. The Effects of Breastfeeding for Four Months on Thinness, Overweight, and Obesity in Children Aged 3 to 6 Years: A Retrospective Cohort Study from National Physical Fitness Surveillance of Jiangsu Province, China. Nutrients 2022, 14, 4154. https://doi.org/10.3390/nu14194154
Huang H, Gao Y, Zhu N, Yuan G, Li X, Feng Y, Gao L, Yu J. The Effects of Breastfeeding for Four Months on Thinness, Overweight, and Obesity in Children Aged 3 to 6 Years: A Retrospective Cohort Study from National Physical Fitness Surveillance of Jiangsu Province, China. Nutrients. 2022; 14(19):4154. https://doi.org/10.3390/nu14194154
Chicago/Turabian StyleHuang, Huiming, Yanan Gao, Na Zhu, Guoqing Yuan, Xiaohan Li, Yong Feng, Linna Gao, and Junwu Yu. 2022. "The Effects of Breastfeeding for Four Months on Thinness, Overweight, and Obesity in Children Aged 3 to 6 Years: A Retrospective Cohort Study from National Physical Fitness Surveillance of Jiangsu Province, China" Nutrients 14, no. 19: 4154. https://doi.org/10.3390/nu14194154
APA StyleHuang, H., Gao, Y., Zhu, N., Yuan, G., Li, X., Feng, Y., Gao, L., & Yu, J. (2022). The Effects of Breastfeeding for Four Months on Thinness, Overweight, and Obesity in Children Aged 3 to 6 Years: A Retrospective Cohort Study from National Physical Fitness Surveillance of Jiangsu Province, China. Nutrients, 14(19), 4154. https://doi.org/10.3390/nu14194154








