Feeding Practices of Infants and Toddlers by Their Mothers in Selected Northern Emirates of the United Arab Emirates
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Maternal Socio-Demographic Characteristics
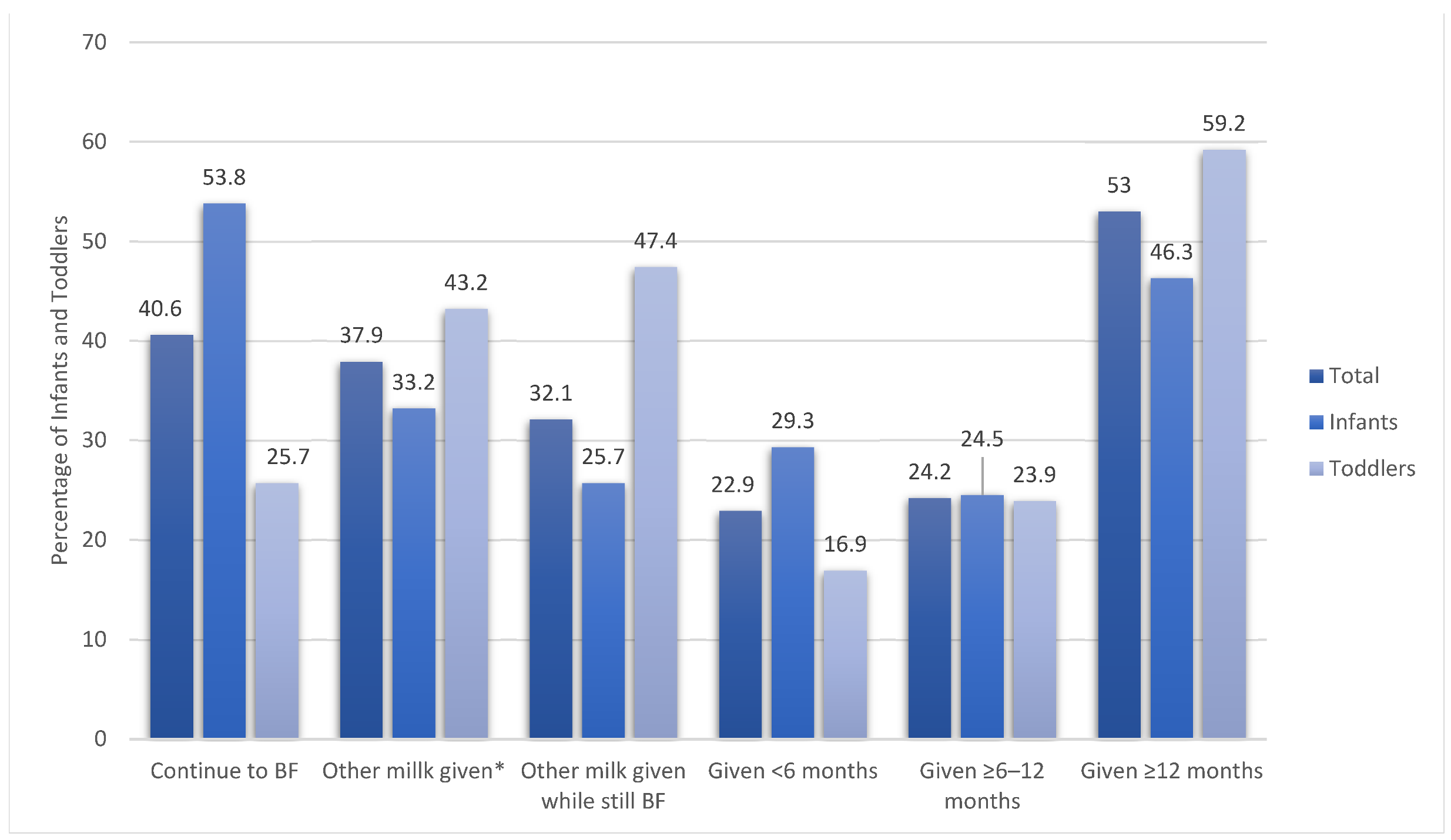
3.2. Types of Milk Given to Infants and Toddlers
3.3. Maternal Socio-Demographic Characteristics and Feeding Practices of Infants and Toddlers
3.4. Infants’ and Toddlers’ Intake of Fluids and Food Groups
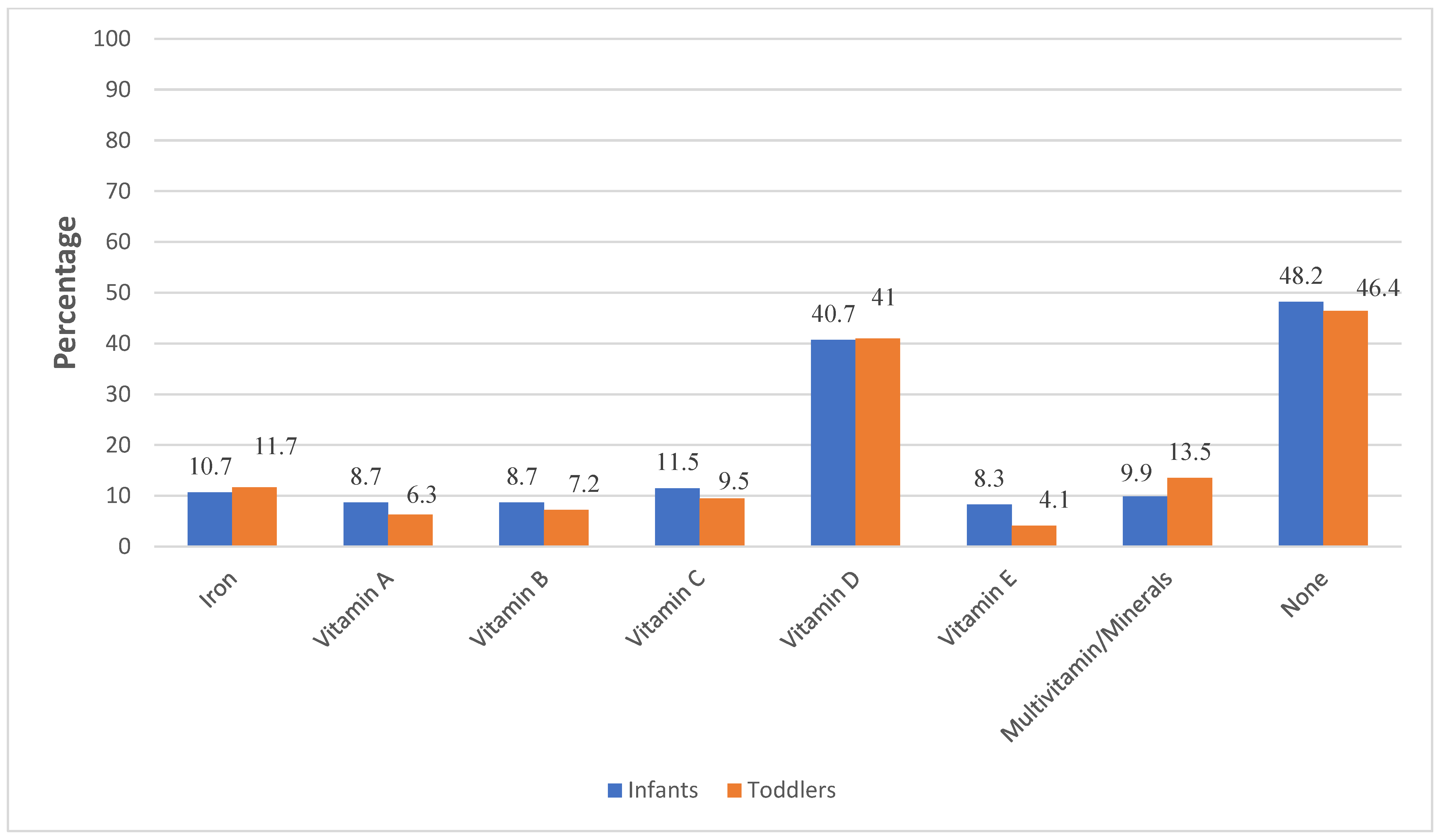
3.5. Introduction of Food Sources of Iron and Use of Vitamin/Mineral Supplements
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization-Infant and Young Child Feeding. Available online: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (accessed on 24 November 2021).
- UNICEF-IRC-The First 1000 Days of Life: The Brain’s Window of Opportunity. Available online: https://www.unicef-irc.org/article/958-the-first-1000-days-of-life-the-brains-window-of-opportunity.html (accessed on 14 February 2021).
- Kelishadi, R.; Farajian, S. The Protective Effects of Breastfeeding on Chronic Non-Communicable Diseases in Adulthood: A Review of Evidence. Adv. Biomed. Res. 2014, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Souza, L.L.; de Moura, E.G.; Lisboa, P.C. Does Early Weaning Shape Future Endocrine and Metabolic Disorders? Lessons from Animal Models. J. Dev. Orig. Health Dis. 2020, 11, 441–451. [Google Scholar] [CrossRef]
- Bagci Bosi, A.T.; Eriksen, K.G.; Sobko, T.; Wijnhoven, T.M.A.; Breda, J. Breastfeeding Practices and Policies in WHO European Region Member States. Public Health Nutr. 2016, 19, 753–764. [Google Scholar] [CrossRef]
- Taha, Z. Trends of Breastfeeding in the United Arab Emirates (UAE). Arab. J. Nutr. Exerc. (AJNE) 2017, 2, 152–159. [Google Scholar] [CrossRef]
- Gardner, H.; Green, K.; Gardner, A. Infant Feeding Practices of Emirati Women in the Rapidly Developing City of Abu Dhabi, United Arab Emirates. Int. J. Environ. Res. Public Health 2015, 12, 10923–10940. [Google Scholar] [CrossRef]
- Radwan, H. Patterns and Determinants of Breastfeeding and Complementary Feeding Practices of Emirati Mothers in the United Arab Emirates. BMC Public Health 2013, 13, 171. [Google Scholar] [CrossRef]
- Taha, Z.; Garemo, M.; Nanda, J. Complementary Feeding Practices among Infants and Young Children in Abu Dhabi, United Arab Emirates. BMC Public Health 2020, 20, 1308. [Google Scholar] [CrossRef]
- Taha, Z.; Hassan, A.; Wikkeling Scott, L.; Papandreou, D. Factors Associated with Delayed Initiation and Cessation of Breastfeeding Among Working Mothers in Abu Dhabi, the United Arab Emirates. Int. J. Women’s Health 2021, 13, 539–548. [Google Scholar] [CrossRef]
- Hameed, N.; Tatari, H.A. Maternal Factors Hindering Successful Breastfeeding in Al Ain City, United Arab Emirates. J. Women’s Health Care 2015, 4, 2167-0420. [Google Scholar] [CrossRef]
- Abuidhail, J.; Al-Modallal, H.; Yousif, R.; Almresi, N. Exclusive Breast Feeding (EBF) in Jordan: Prevalence, Duration, Practices, and Barriers. Midwifery 2014, 30, 331–337. [Google Scholar] [CrossRef]
- Dashti, M.; Scott, J.A.; Edwards, C.A.; Al-Sughayer, M. Predictors of Breastfeeding Duration among Women in Kuwait: Results of a Prospective Cohort Study. Nutrients 2014, 6, 711–728. [Google Scholar] [CrossRef]
- Shafei, A.M.H.E.; Labib, J.R. Determinants of Exclusive Breastfeeding and Introduction of Complementary Foods in Rural Egyptian Communities. Glob. J. Health Sci. 2014, 6, 236–244. [Google Scholar] [CrossRef]
- Al-Ruzaihan, S.A.; Al-Ghanim, A.A.; Bu-Haimed, B.M.; Al-Rajeh, H.K.; Al-Subaiee, W.R.; Al-Rowished, F.H.; Badger-Emeka, L.I. Effect of Maternal Occupation on Breast Feeding among Females in Al-Hassa, Southeastern Region of KSA. J. Taibah Univ. Med. Sci. 2017, 12, 235–240. [Google Scholar] [CrossRef]
- Veghari, G.; Mansourian, A.; Abdollahi, A. Breastfeeding Status and Some Related Factors in Northern Iran. Oman Med. J. 2011, 26, 342–348. [Google Scholar] [CrossRef]
- Daly, A.; Pollard, C.M.; Phillips, M.; Binns, C.W. Benefits, barriers and enablers of breastfeeding: Factor analysis of population perceptions in Western Australia. PLoS ONE 2014, 9, e88204. [Google Scholar] [CrossRef]
- Mirkovic, K.R.; Perrine, C.G.; Scanlon, K.S.; Grummer-Strawn, L.M. Maternity Leave Duration and Full-Time/Part-Time Work Status Are Associated with US Mothers’ Ability to Meet Breastfeeding Intentions. J. Hum. Lact. 2014, 30, 416–419. [Google Scholar] [CrossRef]
- Rivera-Pasquel, M.; Escobar-Zaragoza, L.; González de Cosío, T. Breastfeeding and maternal employment: Results from three national nutritional surveys in Mexico. Matern. Child Health J. 2015, 19, 1162–1172. [Google Scholar] [CrossRef]
- Dagher, R.K.; McGovern, P.M.; Schold, J.D.; Randall, X.J. Determinants of Breastfeeding Initiation and Cessation among Employed Mothers: A Prospective Cohort Study. BMC Pregnancy Childbirth 2016, 16, 194. [Google Scholar] [CrossRef]
- Scott, J.; Ahwong, E.; Devenish, G.; Ha, D.; Do, L. Determinants of Continued Breastfeeding at 12 and 24 Months: Results of an Australian Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 3980. [Google Scholar] [CrossRef]
- Carter, R.C.; Jacobson, J.L.; Burden, M.J.; Armony-Sivan, R.; Dodge, N.C.; Angelilli, M.L.; Lozoff, B.; Jacobson, S.W. Iron Deficiency Anemia and Cognitive Function in Infancy. Pediatrics 2010, 126, e427–e434. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.; Liu, B.; Gao, R.; Snetselaar, L.G.; Strathearn, L.; Bao, W. Association of Anemia with Neurodevelopmental Disorders in a Nationally Representative Sample of US Children. J. Pediatr. 2021, 228, 183–189.e2. [Google Scholar] [CrossRef]
- Obbagy, J.E.; English, L.K.; Psota, T.L.; Wong, Y.P.; Butte, N.F.; Dewey, K.G.; Fox, M.K.; Greer, F.R.; Krebs, N.F.; Scanlon, K.S.; et al. Complementary Feeding and Micronutrient Status: A Systematic Review. Am. J. Clin. Nutr. 2019, 109, 852S–871S. [Google Scholar] [CrossRef]
- WHO. Anemia. Available online: https://www.who.int/health-topics/anaemia#tab=tab_1 (accessed on 31 July 2022).
- Kumar, D.; Qureshi, Z.N.; Albadwawi, M.S. Iron Deficiency Anemia in Infants of Hatta Suburb-UAE. Int. Arch. Nurs. Health Care 2019, 5, 121. [Google Scholar] [CrossRef]
- Faysal, W.; Zaidi, A.R.Z.; Al-Abdi, S.; Alhumaid, S.; AlShehery, M.Z.; Al Mutair, A. Hospital-Based Prevalence of Iron Deficiency Anemia among Pre-School Children in Dubai. Cureus 2020, 12, e10894. [Google Scholar] [CrossRef]
- Nasreddine, L.M.; Kassis, A.N.; Ayoub, J.J.; Naja, F.A.; Hwalla, N.C. Nutritional status and dietary intakes of children amid the nutrition transition: The case of the Eastern Mediterranean Region. Nutr Res. 2018, 57, 12–27. [Google Scholar] [CrossRef]
- Abdulrazzaq, Y.M.; Nagelkerke, N.; Abdulla, S.; Belhaj, G. Nutrient intake of infants and toddlers in the United Arab Emirates: The Feeding Infants and Toddlers Study. EMHJ-East. Mediterr. Health J. 2016, 22, 293–300. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Al Dhaheri, A.S.; Ibrahim, S.; Ali, H.I.; Chokor, F.A.Z.; O’Neill, L.M.; Mohamad, M.N.; Kassis, A.; Ayesh, W.; Kharroubi, S.; et al. Nutritional Status and Adequacy of Feeding Practices in Infants and Toddlers 0-23.9 Months Living in the United Arab Emirates (UAE): Findings from the Feeding Infants and Toddlers Study (FITS) 2020. BMC Public Health 2022, 22, 319. [Google Scholar] [CrossRef]
- Federal Competitiveness and Statistics Authority-Statistics by Subject. Available online: https://fcsa.gov.ae/en-us/Pages/Statistics/Statistics-by-Subject.aspx#/%3Fyear=&folder=Demography%20and%20Social/Vital%20Statistics/Births%20and%20Deaths&subject=Demography%20and%20Social (accessed on 21 February 2020).
- Villar, J.; Altman, D.G.; Purwar, M.; Noble, J.A.; Knight, H.E.; Ruyan, P.; Cheikh Ismail, L.; Barros, F.C.; Lambert, A.; Papageorghiou, A.T.; et al. The Objectives, Design and Implementation of the INTERGROWTH-21st Project. BJOG 2013, 120 (Suppl. S2), 9–26. [Google Scholar] [CrossRef]
- The International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st)-Study Protocol and Other Project Documents. Available online: https://www.intergrowth21.org.uk/protocol.aspx?lang=1.%20 (accessed on 21 May 2020).
- Cheikh Ismail, L.; Giuliani, F.; Bhat, B.A.; Bishop, D.; Papageorghiou, A.T.; Ochieng, R.; Puglia, F.; Altman, D.G.; Maia-Schlüssel, M.; Noble, J.A.; et al. Preterm Feeding Recommendations Are Achievable in Large-Scale Research Studies. BMC Nutr. 2016, 2, 9. [Google Scholar] [CrossRef]
- Subar, A.F.; Dodd, K.W.; Guenther, P.M.; Kipnis, V.; Midthune, D.; McDowell, M.; Tooze, J.A.; Freedman, L.S.; Krebs-Smith, S.M. The Food Propensity Questionnaire: Concept, Development, and Validation for Use as a Covariate in a Model to Estimate Usual Food Intake. J. Am. Diet Assoc. 2006, 106, 1556–1563. [Google Scholar] [CrossRef]
- Kittisakmontri, K.; Fewtrell, M.; Roekworachai, K.; Phanpong, C.; Lanigan, J. Complementary Feeding: Attitudes, Knowledge and Practices of Urban Families in Northern Thailand. Nutr. Diet 2019, 76, 57–66. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 14; Stata Corp LP: College Station, TX, USA, 2015. [Google Scholar]
- Shaikh, U.; Ahmed, O. Islam and infant feeding. Breastfeed Med. 2006, 1, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Radwan, H.; Fakhry, R.; Metheny, N.; Baniissa, W.; Faris, M.A.I.E.; Obaid, R.S.; Al Marzooqi, S.; Al Ghazal, H.; ElHalik, M.; Dennis, C.-L. Prevalence and Multivariable Predictors of Breastfeeding Outcomes in the United Arab Emirates: A Prospective Cohort Study. Int. Breastfeed. J. 2021, 16, 79. [Google Scholar] [CrossRef] [PubMed]
- Al-Kohji, S.; Said, H.A.; Selim, N.A. Breastfeeding Practice and Determinants among Arab Mothers in Qatar. Saudi Med. J. 2012, 33, 436–443. [Google Scholar] [PubMed]
- Al Ghwass, M.M.E.; Ahmed, D. Prevalence and Predictors of 6-Month Exclusive Breastfeeding in a Rural Area in Egypt. Breastfeed Med. 2011, 6, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Alyousefi, N.A. Determinants of Successful Exclusive Breastfeeding for Saudi Mothers: Social Acceptance Is a Unique Predictor. Int. J. Environ. Res. Public Health 2021, 18, 5172. [Google Scholar] [CrossRef]
- Issa, C.; Hobeika, M.; Salameh, P.; Zeidan, R.K.; Mattar, L. Longer Durations of Both Exclusive and Mixed Breastfeeding Are Associated with Better Health in Infants and Toddlers. Breastfeeding Rev. 2019, 27, 17–27. [Google Scholar] [CrossRef]
- Yılmaz, E.; Doğa Öcal, F.; Vural Yılmaz, Z.; Ceyhan, M.; Kara, O.F.; Küçüközkan, T. Early Initiation and Exclusive Breastfeeding: Factors Influencing the Attitudes of Mothers Who Gave Birth in a Baby-Friendly Hospital. Turk. J. Obstet. Gynecol. 2017, 14, 1–9. [Google Scholar] [CrossRef]
- Inano, H.; Kameya, M.; Sasano, K.; Matsumura, K.; Tsuchida, A.; Hamazaki, K.; Inadera, H.; Hasegawa, T. Factors Influencing Exclusive Breastfeeding Rates until 6 Months Postpartum: The Japan Environment and Children’s Study. Sci. Rep. 2021, 11, 6841. [Google Scholar] [CrossRef]
- Alzaheb, R.A. Factors Influencing Exclusive Breastfeeding in Tabuk, Saudi Arabia. Clin. Med. Insights Pediatr. 2017, 11, 1179556517698136. [Google Scholar] [CrossRef]
- Khasawneh, W.; Khasawneh, A.A. Predictors and Barriers to Breastfeeding in North of Jordan: Could We Do Better? Int. Breastfeed. J. 2017, 12, 49. [Google Scholar] [CrossRef] [PubMed]
- Attanasio, L.; Kozhimannil, K.B.; McGovern, P.; Gjerdingen, D.; Johnson, P.J. The impact of prenatal employment on breastfeeding intentions and breastfeeding status at 1 week postpartum. J. Hum. Lact. 2013, 29, 620–628. [Google Scholar] [CrossRef]
- Oakley, L.L.; Henderson, J.; Redshaw, M.; Quigley, M.A. The Role of Support and Other Factors in Early Breastfeeding Cessation: An Analysis of Data from a Maternity Survey in England. BMC Pregnancy Childbirth 2014, 14, 88. [Google Scholar] [CrossRef]
- Dutheil, F.; Méchin, G.; Vorilhon, P.; Benson, A.C.; Bottet, A.; Clinchamps, M.; Barasinski, C.; Navel, V. Breastfeeding after Returning to Work: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8631. [Google Scholar] [CrossRef] [PubMed]
- The World Bank-Labor Force Participation Rate, Female (% of Female Population Ages 15+) (Modeled ILO Estimate)-United Arab Emirates | Data. Available online: https://data.worldbank.org/indicator/SL.TLF.CACT.FE.ZS?locations=AE (accessed on 30 March 2022).
- Nuzzi, G.; Di Cicco, M.E.; Peroni, D.G. Breastfeeding and Allergic Diseases: What’s New? Children 2021, 8, 330. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, H.P.; Krishna, J.; Puri, R.K.; Satyanarayana, L.; Kumar, S. Water Supplementation in Exclusively Breastfed Infants during Summer in the Tropics. Lancet 1991, 337, 929–933. [Google Scholar] [CrossRef]
- Nassreddine, L.M.; Naja, F.A.; Hwalla, N.C.; Ali, H.I.; Mohamad, M.N.; Chokor, F.A.Z.S.; Chehade, L.N.; O’Neill, L.M.; Kharroubi, S.A.; Ayesh, W.H.; et al. Total Usual Nutrient Intakes and Nutritional Status of United Arab Emirates Children (<4 Years): Findings from the Feeding Infants and Toddlers Study (FITS) 2021. Curr. Dev. Nutr. 2022, 6, nzac080. [Google Scholar] [CrossRef]
- Gahche, J.J.; Herrick, K.A.; Potischman, N.; Bailey, R.L.; Ahluwalia, N.; Dwyer, J.T. Dietary Supplement Use among Infants and Toddlers Aged <24 Months in the United States, NHANES 2007–2014. J. Nutr. 2019, 149, 314–322. [Google Scholar] [CrossRef] [Green Version]
| Maternal Characteristic | Total Population (n = 475) |
|---|---|
| Age group, n (%) | |
| 18–25 years | 106 (22.3) |
| 26–33 years | 227 (47.8) |
| 34+ years | 142 (29.9) |
| Educational level, n (%) | |
| Basic/high school | 157 (33.1) |
| University level | 318 (66.9) |
| Professional status, n (%) | |
| Employed (Part-time, full-time, or entrepreneur) | 342 (72.0 |
| Unemployed | 133 (28.0) |
| Nationality, n (%) | |
| UAE national | 262 (55.2) |
| UAE non-national | 213 (44.8) |
| Sources of information used for child feeding | |
| Health professionals | 148 (31.2) |
| Family/friends | 137 (28.8) |
| Social media | 131 (27.6) |
| Other | 59 (12.4) |
| Variable | Total n = 475 | 18–25 Years n = 106, 22.3% | 26–33 Years n = 227, 47.8% | 34+ Years n = 142, 29.9% | p-Value |
|---|---|---|---|---|---|
| Type of feeding for first 6 months | 0.020 | ||||
| Exclusive breastfeeding (EBF) | 222 (46.7) | 62 (58.5) | 102 (44.9) | 58 (40.9) | |
| Breastmilk and formula | 208 (43.8) | 32 (30.2) | 103 (45.4) | 73 (51.4) | |
| Only formula | 45 (9.5) | 12 (11.3) | 22 (9.7) | 11 (7.8) | |
| Age when breastfeeding stopped (n = 339) * | 0.272 | ||||
| <6 months | 181 (53.4) | 42 (61.8) | 88 (52.4) | 51 (49.5) | |
| ≥6 months | 158 (46.6) | 26 (38.2) | 80 (47.6) | 52 (50.5) | |
| Age when child was given milk other than breastmilk or formula | 0.252 | ||||
| <6 months | 89 (22.9) | 20 (22.0) | 37 (20.2) | 32 (27.8) | |
| ≥6 months–11.9 months | 94 (24.2) | 28 (30.8) | 41 (22.4) | 25 (21.7) | |
| ≥1 year | 206 (52.9) | 43 (47.3) | 105 (57.4) | 58 (50.4) | |
| Age when started solid food | 0.964 | ||||
| <6 months | 182 (41.6) | 38 (43.2) | 86 (40.6) | 58 (42.0) | |
| ≥6 months–<1 year | 234 (53.4) | 47 (53.4) | 114 (53.8) | 73 (52.9) | |
| ≥1 year | 22 (5.0) | 3 (3.4) | 12 (5.7) | 7 (5.1) | |
| Age for introducing animal-based protein | 0.156 | ||||
| 6–7 months | 89 (18.7) | 20 (18.9) | 38 (16.7) | 31 (21.8) | |
| 8–9 months | 137 (28.8) | 32 (30.2) | 75 (33.0) | 30 (21.1) | |
| 10–11 months | 79 (16.6) | 23 (21.7) | 34 (15.0) | 22 (15.5) | |
| ≥12 months | 89 (18.7) | 13 (12.3) | 45 (19.8) | 31 (21.8) | |
| Don’t give any | 81 (17.1) | 18 (17.0) | 35 (15.4) | 28 (19.7) | |
| Type of first animal protein given | 0.017 | ||||
| Beef | 9 (1.9) | 3 (2.8) | 3 (1.3) | 3 (2.1) | |
| Chicken | 143 (30.1) | 27 (25.5) | 70 (30.8) | 46 (32.4) | |
| Egg yolk | 131 (27.6) | 35 (33.0) | 66 (29.1) | 30 (21.1) | |
| Fish | 31 (6.5) | 13 (12.3) | 13 (5.7) | 5 (3.5) | |
| Liver | 4 (0.8) | 0 (0) | 2 (0.9) | 2 (1.4) | |
| Whole egg | 83 (17.5) | 8 (7.6) | 44 (19.4) | 31 (21.8) | |
| None yet | 74 (15.6) | 20(18.9) | 29(12.8) | 25(17.6) | |
| Infants | 56(22.1) | 14(20.0) | 23(20.2) | 19(27.5) | |
| Toddlers | 18(8.1) | 6 (16.7) | 6 (5.3) | 6 (8.2) | |
| Use of salt or honey in child’s food, % yes | 210 (44.2) | 44 (41.5) | 95 (41.9) | 71 (50.0) | 0.252 |
| Infants | 89 (35.2) | 23 (32.9) | 37 (32.5) | 29 (42.0) | 0.376 |
| Toddlers | 121 (51.5) | 21 (58.3) | 58 (51.3) | 42 (17.8) | 0.624 |
| Child’s food prepared usually, % | 0.406 | ||||
| Home | 467 (98.3) | 105 (99.1) | 225 (99.1) | 137 (96.5) | |
| Family/friends | 4 (0.8) | 1 (0.9) | 0 (0) | 3 (2.1) | |
| Restaurant/take away | 2 (0.4) | 0 (0) | 1 (0.4) | 1 (0.7) | |
| Other | 2 (0.4) | 0 (0) | 1 (0.4) | 1 (0.7) | |
| Who feeds the child | |||||
| Mother | 435 (91.6) | 99 (93.4) | 213 (93.8) | 123 (86.6) | 0.040 |
| Father | 5 (1.1) | 3 (2.8) | 0 (0) | 2 (1.4) | |
| Grandparent | 6 (1.3) | 1 (0.9) | 2 (0.9) | 3 (2.1) | |
| Nanny | 27 (5.7) | 3 (2.8) | 10 (4.4) | 14 (9.9) | |
| Other | 2 (0.4) | 0 (0) | 2 (0.9) | 0 (0) | |
| Use of supplements | 250 (52.6) | 43 (40.6) | 132 (58.2) | 75 (52.8) | 0.011 |
| Infants | 131 (51.8) | 28 (40.0) | 71 (62.3) | 32 (51.8) | 0.008 |
| Toddlers | 119 (53.6) | 15 (41.7) | 61 (54.0) | 43 (58.9) | 0.235 |
| Knowledge of iron-rich foods | 422 (88.8) | 89 (84.0) | 211 (92.9) | 122 (85.9) | 0.022 |
| Variable | Unemployed 342 (72) n (%) | Employed 133 (28) n (%) | p-Value | ≤High School 106 (22.3) n (%) | University 369 (77.7) n (%) | p-Value |
|---|---|---|---|---|---|---|
| Type of food over first 6 months | <0.001 | 0.363 | ||||
| Exclusive breastfeeding (EBF) | 176 (51.5) | 46 (34.6) | 80 (51.0) | 142 (44.7) | ||
| Breastmilk and Formula | 131 (38.3) | 77 (57.9) | 65 (41.4) | 143 (45.0) | ||
| Only formula | 35 (10.2) | 10 (7.5) | 12 (7.6) | 33 (10.4) | ||
| Child’s age when BF stopped | 0.272 | 0.598 | ||||
| <6 months | 119 (50.2) | 62 (60.8) | 61 (55.5) | 120 (52.4) | ||
| ≥6 months | 118 (49.8) | 40 (39.2) | 49 (44.5) | 109 (47.6) | ||
| Continued breastfeeding after 6 months | 150 (43.9) | 43 (32.3) | 0.022 | 75 (47.8) | 118 (37.1) | 0.026 |
| Gave child milk other than breastmilk or formula | 129 (37.7%) | 51 (38.4%) | 0.899 | 70 (44.6) | 110 (34.6) | 0.035 |
| Age when “other milk” was given (does not include breastmilk or formula) | 0.066 | 0.022 | ||||
| <6 months | 57 (20.7) | 32 (28.1) | 28 (21.7) | 61 (23.5) | ||
| ≥6 months–11.9 months | 62 (22.6) | 32 (28.1) | 42 (32.6) | 52 (20.0) | ||
| ≥1 year | 156 (56.7) | 50 (43.9) | 59 (45.7) | 147 (56.5) | ||
| Age when started solid food | 0.271 | 0.791 | ||||
| <6 months | 130 (41.5) | 52 (41.6) | 59 (39.3) | 123 (42.7) | ||
| ≥6 months–<1 year | 164 (52.4) | 70 (56.0) | 83 (55.3) | 151 (52.4) | ||
| ≥1 year | 19 (6.1) | 3 (2.4) | 8 (5.3) | 14 (4.9) | ||
| Age when animal-based protein was given | 0.064 | 0.312 | ||||
| 6–7 months | 57 (16.7) | 32 (24.1) | 34 (21.7) | 55 (17.3) | ||
| 8–9 months | 92 (26.9) | 45 (33.8) | 37 (23.6) | 100 (31.5) | ||
| 10–11 months | 62 (18.1) | 17 (12.8) | 30 (19.1) | 49 (15.4) | ||
| ≥12 months | 71 (20.8) | 18 (13.5) | 27 (17.2) | 62 (19.5) | ||
| Do not give any | 60 (17.5) | 21 (15.8) | 29 (18.5) | 52 (16.4%) | ||
| Infants | 47 (24.6) | 15 (24.2) | 0.012 | 23 (23.5) | 39 (25.2) | 0.533 |
| Toddlers | 13 (8.6) | 6 (8.5) | 0.793 | 6 (10.2) | 13 (8.0) | 0.588 |
| First animal protein given | 0.183 | 0.166 | ||||
| Beef | 9 (2.6) | 0 (0) | 2 (1.3) | 7 (2.2) | ||
| Chicken | 102 (29.8) | 41 (30.8) | 49 (31.2) | 94 (29.6) | ||
| Egg yolk | 86 (25.2) | 45 (33.8) | 36 (22.9) | 95 (29.9) | ||
| Fish | 24 (7.0) | 7 (5.3) | 15 (9.5) | 16 (5.0) | ||
| Liver | 2 (0.6) | 2 (1.5) | 3 (1.9) | 1 (0.3) | ||
| Whole egg | 64 (18.7) | 19 (14.3) | 26 (16.6) | 57 (17.9) | ||
| None yet | 55 (16.1) | 19 (14.3) | 26 (16.6) | 48 (15.1) | ||
| Use of salt or honey in child’s food, n = 210 (%) | 149 (43.6) | 61 (45.9) | 0.651 | 77 (49.0) | 133 (41.8) | 0.136 |
| Infants | 64 (33.5) | 25 (40.3) | 0.329 | 40 (40.8) | 49 (31.6) | 0.135 |
| Toddlers | 85 (56.3) | 36 (50.7) | 0.436 | 37 (62.7) | 84 (51.5) | 0.140 |
| Who feeds the child? | <0.001 | 0.066 | ||||
| Mother | 333 (97.4) | 102 (76.7) | 151 (96.2) | 284 (89.3) | ||
| Father | 3 (0.9) | 2 (1.5) | 0 (0) | 5 (1.6) | ||
| Grandparent | 1 (0.3) | 5 (3.8) | 0 (0) | 6 (1.9) | ||
| Nanny | 5 (1.5) | 22 (16.5) | 5 (3.2) | 22 (6.9) | ||
| Other | 0 (0) | 2 (1.5) | 1 (0.6) | 1 (0.3) | ||
| Use of supplements, Yes (%) | 163 (47.7) | 87 (65.4) | 0.001 | 61 (57.6) | 189 (51.2) | 0.250 |
| Infants | 88 (46.1) | 43 (69.4) | 0.001 | 58 (59.2) | 73 (47.1) | 0.061 |
| Toddlers | 75 (49.7) | 44 (62.0) | 0.086 | 3 (37.5) | 116 (54.2) | 0.477 |
| Knowledge of iron-rich foods, Yes (%) | 304 (88.9) | 118 (88.7) | 0.959 | 138 (87.9) | 284 (89.3) | 0.646 |
| Variables | Odds Ratio | 95% Confidence Interval | p Value * | |
|---|---|---|---|---|
| Exclusive breastfeeding | (base outcome) | |||
| Breastmilk and formula | ||||
| Age category 1 | ||||
| 25–33 years old | 1.7 | 1.014–2.958 | 0.044 | |
| 33+ years old | 2.2 | 1.262–3.993 | 0.006 | |
| Educational level 2 | 1.1 | 0.698–1.672 | 0.729 | |
| Employed vs. unemployed | 2.0 | 1.298–3.220 | 0.002 | |
| Nationality 3 | ||||
| Arab | 0.9 | 0.607–1.445 | 0.768 | |
| Non-Arab | 0.7 | 0.222–2.003 | 0.470 | |
| Method of delivery | 1.2 | 0.728–1.863 | 0.526 | |
| Weeks of gestation | 0.9 | 0.583–1.467 | 0.739 | |
| Only formula | ||||
| Age category 1 | ||||
| 25–33 | 0.8 | 0.367–1.913 | 0.674 | |
| 33+ | 0.8 | 0.307–1.994 | 0.607 | |
| Educational level 2 | 1.3 | 0.627–2.875 | 0.449 | |
| Employed vs. unemployed | 1.0 | 0.437–2.170 | 0.949 | |
| Nationality 3 | ||||
| Arab | 1.7 | 0.819–3.517 | 0.155 | |
| Non-Arab | 0.7 | 0.079–6.375 | 0.761 | |
| Method of delivery | 1.9 | 0.901–3.821 | 0.094 | |
| Weeks of gestation | 1.2 | 0.548–2.584 | 0.660 | |
| Variable | Total Children | Infants (n = 253) | Toddlers (n = 222) | p-Value |
|---|---|---|---|---|
| Daily intake, median (25–75% range) | ||||
| Breastmilk | 0.64 (0, 2.0) | 0.64 (0.1, 2.0) | 0.64 (0, 2.0) | 0.732 |
| Formula/soya milk | 0.29 (0, 2.0) | 0.29 (0, 2.0) | 0.64 (0, 2.0) | 0.404 |
| Animal milk | 0.1 (0, 0.64) | 0 (0, 0.29) | 0.29 (0. 2.0) | <0.001 |
| Water | 2.0 (0.3, 4.0) | 0.64 (0.1, 2.0) | 2.0 (0.64, 4.0) | <0.001 |
| Weekly intake, median (25–75% range) | ||||
| 100% fruit or vegetable juice | 2.0 (0, 14) | 0.5 (0, 4.5) | 2.0 (0.5, 14) | <0.001 |
| Ready to drink (packaged) fruit or vegetable juice | 2.0 (0.5, 14) | 2.0 (0.5, 14) | 2.0 (0.5, 14) | 0.249 |
| Soft drinks | 0 (0, 4.5) | 0 (0, 4.5) | 0 (0, 14) | 0.477 |
| Food groups, daily 1 intake, median (25–75% range) | ||||
| Grains and cereal | 2.9 (1.3, 6.1) | 2.6 (1.2, 5.3) | 3.4 (1.3, 8.0) | 0.002 |
| Dairy | 0.3 (0.07, 2.0) | 0.07 (0, 0.64) | 0.64 (0.29, 2.0) | <0.001 |
| Tubers | 0.3 (0.07, 2.0) | 0.3 (0.07, 2.0) | 0.3 (0.29, 2.0) | 0.027 |
| Vitamin-A-rich fruit & vegetables | 0.64 (0.29, 2.0) | 0.64 (0.1, 2.0) | 0.64 (0.29, 2.0) | 0.003 |
| Vegetables (other) | 0.64 (0.07, 2.0) | 0.29 (0.07, 0.64) | 0.64 (0.29, 2.0) | |
| Fruit (other) | 0.29 (0.07, 0.64) | 0.29 (0.07, 0.64) | 0.29 (0.64, 2.0) | <0.001 |
| Total fruits and vegetables | 1.92 (0.87, 5.28) | 1.57 (0.43, 3.28) | 3.28 (0.87, 6.0) | <0.001 |
| Weekly 2 intake, median (25–75% range) | ||||
| Eggs | 2.0 (0.5, 4.5) | 2.0 (0, 4.5) | 2.0 (2.0, 14.0) | <0.001 |
| Pulses/legumes | 2.0 (0.5, 14.0) | 2.0 (0.5, 4.5) | 2.0 (2.0, 14.0) | 0.054 |
| Red meat, organ meats | 2.0 (0, 4.5) | 0.5 (0, 4.5) | 0.5 (2.0, 4.5) | <0.001 |
| Poultry | 2.0 (0.5, 4.5) | 2.0 (0, 4.5) | 2.0 (2.0, 14.0) | <0.001 |
| Fish | 2.0 (0.5, 4.5) | 0.5 (0, 4.5) | 2.0 (0.5, 4.5) | <0.001 |
| Sweets (all baked goods and desserts) | 2.0 (0.6, 4.4) | 1.5 (0.5, 3.2) | 2.6 (0.9, 4.9) | <0.001 |
| Chips and savory snacks | 2.0 (0, 4.5) | 0.5 (0, 4.5) | 2.0 (0.5, 14) | <0.001 |
| Take away food | 0.5 (0, 2.0) | 0.5 (0, 2.0) | 2.0 (0, 4.5) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, H.I.; Magriplis, E.; Attlee, A.; Al Dhaheri, A.S.; Cheikh Ismail, L.; Stojanovska, L. Feeding Practices of Infants and Toddlers by Their Mothers in Selected Northern Emirates of the United Arab Emirates. Nutrients 2022, 14, 3719. https://doi.org/10.3390/nu14183719
Ali HI, Magriplis E, Attlee A, Al Dhaheri AS, Cheikh Ismail L, Stojanovska L. Feeding Practices of Infants and Toddlers by Their Mothers in Selected Northern Emirates of the United Arab Emirates. Nutrients. 2022; 14(18):3719. https://doi.org/10.3390/nu14183719
Chicago/Turabian StyleAli, Habiba I., Emmanuella Magriplis, Amita Attlee, Ayesha S. Al Dhaheri, Leila Cheikh Ismail, and Lily Stojanovska. 2022. "Feeding Practices of Infants and Toddlers by Their Mothers in Selected Northern Emirates of the United Arab Emirates" Nutrients 14, no. 18: 3719. https://doi.org/10.3390/nu14183719
APA StyleAli, H. I., Magriplis, E., Attlee, A., Al Dhaheri, A. S., Cheikh Ismail, L., & Stojanovska, L. (2022). Feeding Practices of Infants and Toddlers by Their Mothers in Selected Northern Emirates of the United Arab Emirates. Nutrients, 14(18), 3719. https://doi.org/10.3390/nu14183719











