Exploring the Effects of Energy Constraints on Performance, Body Composition, Endocrinological/Hematological Biomarkers, and Immune System among Athletes: An Overview of the Fasting State
Abstract
:1. Introduction
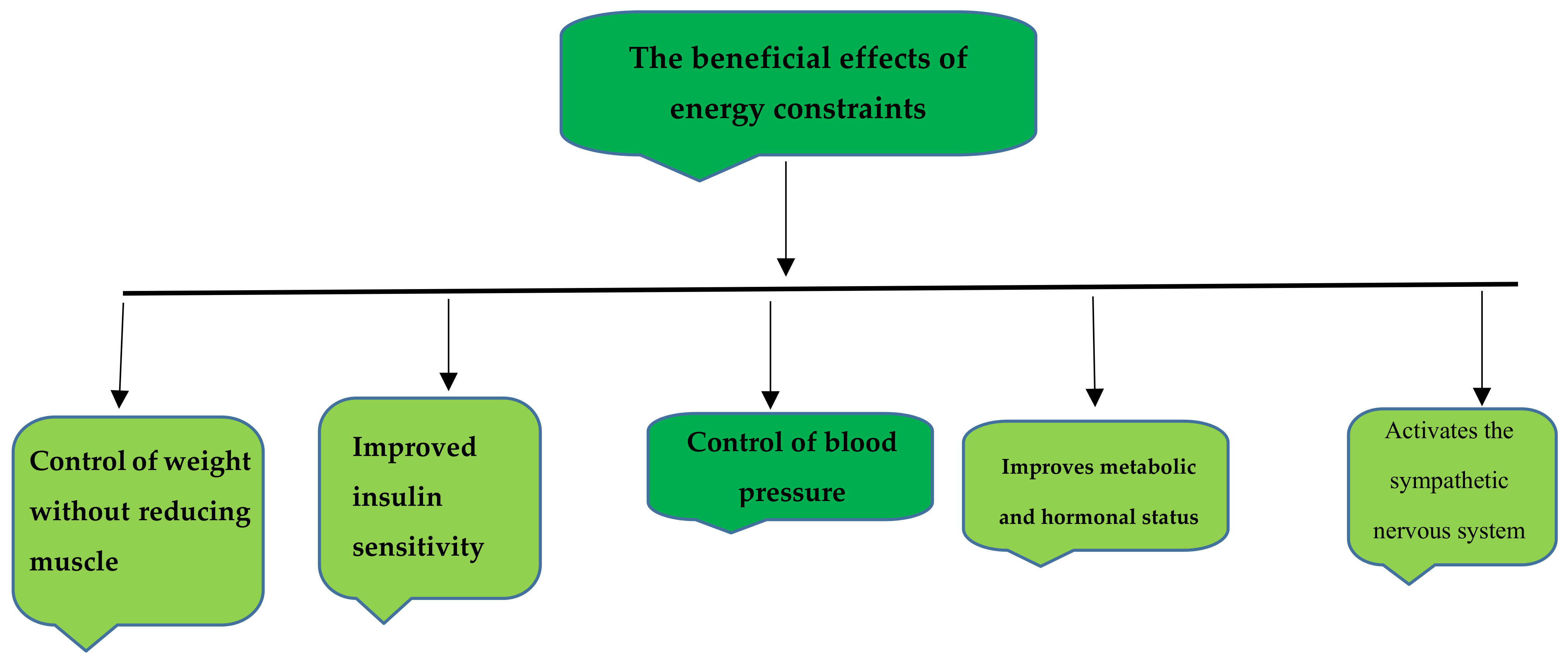
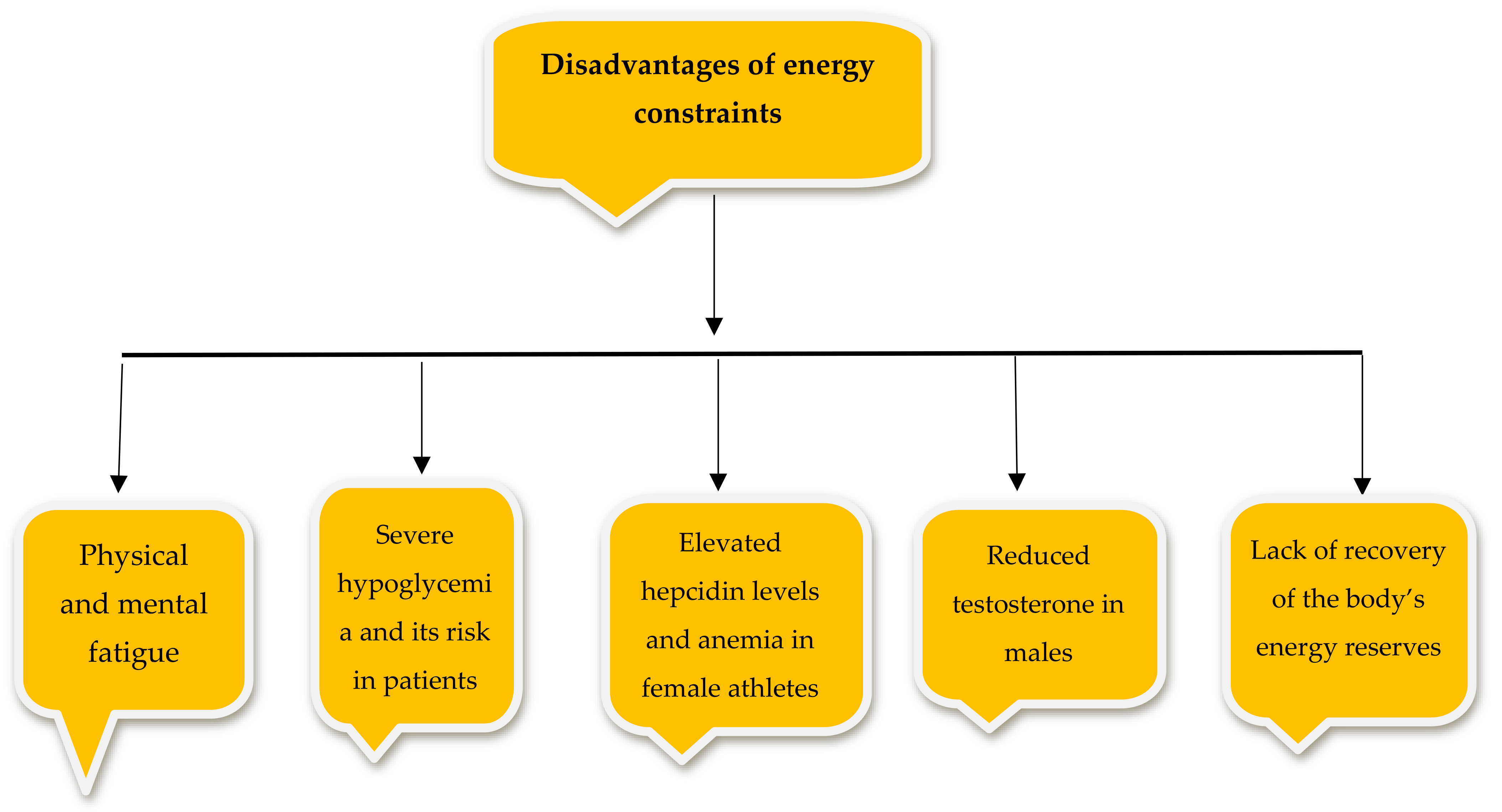
2. Energy Restriction
3. Fasting for All Athletes
4. Muslim Athletes and Fasting
5. Physiological and Metabolic Responses to an RFP and Energy Restrictions
6. Endocrine Adaptations Induced by an RFP
6.1. Hormones Released by the Thyroid and the Effect of an RFP on These Hormones
6.2. Hormones Released by the Adrenal Gland and the Effect of an RFP on These Hormones
6.3. Response of Appetite Hormones to an RFP
7. Nutritional Considerations for Athletes during an RFP
7.1. Protein
7.2. Lipids
7.3. Hydration Strategies
- ⮚
- The RFP prevents athletes from being hydrated during a race, and they become dehydrated.
- ⮚
- The lack of water causes a drop in performance.
- ⮚
- The lack of water disrupts the balance of water and electrolytes [71].
- Reduce the time in situations where there is a possibility of dehydration, such as exposure to sunlight.
- Be sure to check the hydration status of the body.
- Before an RFP begins, fluids should be selected according to the conditions and contain minerals and energy that reduce water loss.
- The consumption of fluids when a person is not participating in an RFP should be regular, such as during the night.
- As much as possible, one should train and compete for 2 to 3 h after sunset [78].
8. Response of Hematocrit to an RFP in Athletes
8.1. Erythrocyte States
8.2. Platelet Count
9. Immunosuppression and Related Cells during an RFP
10. Response of the Immune System to an RFP in Athletes
11. Changing the Performance and Record of Athletes during Ramadan
11.1. Endurance Training
11.2. Resistance Training
11.3. Sprint Performance
11.4. Power-Output Measure
11.5. Blood Lactate Concentration
11.6. Practical Applications
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ohta, S.; Nakaji, S.; Suzuki, K.; Totsuka, M.; Umeda, T.; Sugawara, K. Depressed humoral immunity after weight reduction in competitive judoists. Luminescence 2002, 17, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Brownell, K.D.; Steen, S.N.; Wilmore, J.H. Weight regulation practices in athletes: Analysis of metabolic and health effects. Med. Sci. Sports Exerc. 1987, 19, 546–556. [Google Scholar] [CrossRef] [PubMed]
- Lakin, J.A.; Steen, S.N.; Oppliger, R.A. Eating behaviors, weight loss methods, and nutrition practices among high school wrestlers. J. Community Health Nurs. 1990, 7, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K. Recent Progress in Applicability of Exercise Immunology and Inflammation Research to Sports Nutrition. Nutrients 2021, 13, 4299. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Abizari, A.-R. Ramadan fasting alters food patterns, dietary diversity and body weight among Ghanaian adolescents. Nutr. J. 2018, 17, 75. [Google Scholar] [CrossRef]
- Julia, C.; Péneau, S.; Andreeva, V.A.; Méjean, C.; Fezeu, L.; Galan, P.; Hercberg, S. Weight-loss strategies used by the general population: How are they perceived? PLoS ONE 2014, 9, e97834. [Google Scholar] [CrossRef] [Green Version]
- Chaouachi, A.; Leiper, J.B.; Chtourou, H.; Aziz, A.R.; Chamari, K. The effects of Ramadan intermittent fasting on athletic performance: Recommendations for the maintenance of physical fitness. J. Sports Sci. 2012, 30, S53–S73. [Google Scholar] [CrossRef]
- Visioli, F.; Mucignat-Caretta, C.; Anile, F.; Panaite, S.-A. Traditional and Medical Applications of Fasting. Nutrients 2022, 14, 433. [Google Scholar] [CrossRef]
- Zhao, Y.Y.; Qi, Y.; Wang, X.N.; Zhao, W. Resolving the energy restriction at high altitude: Variation in the digestive system of Phrynocephalus vlangalii. Anim. Biol. 2020, 70, 321–331. [Google Scholar] [CrossRef]
- de Cabo, R.; Mattson, M.P. Effects of intermittent fasting on health, aging, and disease. N. Engl. J. Med. 2019, 381, 2541–2551. [Google Scholar] [CrossRef]
- Horne, B.D.; Muhlestein, J.B.; Anderson, J.L. Health effects of intermittent fasting: Hormesis or harm? A systematic review. Am. J. Clin. Nutr. 2015, 102, 464–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patterson, R.E.; Sears, D.D. Metabolic effects of intermittent fasting. Annu. Rev. Nutr. 2017, 37, 371–393. [Google Scholar] [CrossRef] [Green Version]
- Channon, S.; Hayward, A. The effect of short-term fasting on processing of food cues in normal subjects. Int. J. Eat. Disord. 1990, 9, 447–452. [Google Scholar] [CrossRef]
- Miller, W., Jr.; Faust, I.; Goldberger, A.; Hirsch, J. Effects of severe long-term food deprivation and refeeding on adipose tissue cells in the rat. Am. J. Physiol. Endocrinol. Metab. 1983, 245, E74–E80. [Google Scholar] [CrossRef]
- Miller, T. Mapping the Global Muslim Population: A Report on the Size and Distribution of the World’s Muslim Population; Pew Research Center: Washington, DC, USA, 2009. [Google Scholar]
- Chamari, K.; Roussi, M.; Bragazzi, N.L.; Chaouachi, A.; Abdul, R.A. Optimizing training and competition during the month of Ramadan: Recommendations for a holistic and personalized approach for the fasting athletes. Tunis Med. 2019, 97, 1095–1103. [Google Scholar] [PubMed]
- Singh, R.; Hwa, O.C.; Roy, J.; Jin, C.W.; Ismail, S.M.; Lan, M.F.; Hiong, L.L.; Aziz, A.-R. Subjective perception of sports performance, training, sleep and dietary patterns of malaysian junior muslim athletes during ramadan intermittent fasting. Asian J. Sports Med. 2011, 2, 167–176. [Google Scholar] [CrossRef] [Green Version]
- Kirkendall, D.T.; Chaouachi, A.; Aziz, A.R.; Chamari, K. Strategies for maintaining fitness and performance during Ramadan. J. Sports Sci. 2012, 30, S103–S108. [Google Scholar] [CrossRef]
- Burke, L.M.; King, C. Ramadan fasting and the goals of sports nutrition around exercise. J. Sports Sci. 2012, 30, S21–S31. [Google Scholar] [CrossRef]
- Trabelsi, K.; Bragazzi, N.; Zlitni, S.; Khacharem, A.; Boukhris, O.; El-Abed, K.; Ammar, A.; Khanfir, S.; Shephard, R.J.; Hakim, A. Observing Ramadan and sleep-wake patterns in athletes: A systematic review, meta-analysis and meta-regression. Br. J. Sports Med. 2020, 54, 674–680. [Google Scholar] [CrossRef]
- Akter, M. Assessment of Calorie Consumption among Citizen of Coastal Area of Khulna and Barisal. 2019. Available online: https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Akter%2C+M.+Assessment+of+Calorie+Consumption+among+Citizen+of+Coastal+Area+of+Khulna+and+Barisal.+2019.++&btnG= (accessed on 31 December 2019).
- Yildiz, C.; Öngel, M.E.; Yilmaz, B.; Özilgen, M. Diet-dependent entropic assessment of athletes’ lifespan. J. Nutr. Sci. 2021, 10, e83. [Google Scholar] [CrossRef]
- Ji, B.; Ernest, B.; Gooding, J.R.; Das, S.; Saxton, A.M.; Simon, J.; Dupont, J.; Métayer-Coustard, S.; Campagna, S.R.; Voy, B.H. Transcriptomic and metabolomic profiling of chicken adipose tissue in response to insulin neutralization and fasting. BMC Genom. 2012, 13, 411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ajibola, A.A.; Azeez, A.O.; Ajibola, A. The Beneficial Effects of Ramadan Fasting from the Medical and Sociocultural Perspectives. J. Fasting Health 2021, 9, 1–13. [Google Scholar]
- Ramadan, J. Does fasting during Ramadan alter body composition, blood constituents and physical performance? Med. Princ. Pract. 2002, 11, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Nobari, H.; Kargarfard, M.; Minasian, V.; Cholewa, J.M.; Pérez-Gómez, J. The effects of 14-week betaine supplementation on endocrine markers, body composition and anthropometrics in professional youth soccer players: A double blind, randomized, placebo-controlled trial. J. Int. Soc. Sports Nutr. 2021, 18, 20. [Google Scholar] [CrossRef]
- Hofer, S.J.; Carmona-Gutierrez, D.; Mueller, M.I.; Madeo, F. The ups and downs of caloric restriction and fasting: From molecular effects to clinical application. EMBO Mol. Med. 2022, 14, e14418. [Google Scholar] [CrossRef]
- Mullur, R.; Liu, Y.-Y.; Brent, G.A. Thyroid hormone regulation of metabolism. Physiol. Rev. 2014, 94, 355–382. [Google Scholar] [CrossRef] [Green Version]
- Rybicka, M.; Krysiak, R.; Okopień, B. The dawn phenomenon and the Somogyi effect—Two phenomena of morning hyperglycaemia. Endokrynol. Pol. 2011, 62, 276–284. [Google Scholar]
- Sajid, K.M.; Akhtar, M.; Malik, G.Q. Ramadan fasting and thyroid hormone profile. J. Pak. Med. Assoc. 1991, 41, 213–216. [Google Scholar]
- Babichuk, N.A.; Volkoff, H. Changes in expression of appetite-regulating hormones in the cunner (Tautogolabrus adspersus) during short-term fasting and winter torpor. Physiol. Behav. 2013, 120, 54–63. [Google Scholar] [CrossRef]
- Breij, L.M.; Mulder, M.T.; van Vark-van der Zee, L.; Hokken-Koelega, A. Appetite-regulating hormones in early life and relationships with type of feeding and body composition in healthy term infants. Eur. J. Nutr. 2017, 56, 1725–1732. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, P.d.F.D.S.; Dos Santos, P.B.; Pazos-Moura, C.C. The role of thyroid hormone in metabolism and metabolic syndrome. Ther. Adv. Endocrinol. Metab. 2020, 11, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Hadjzadeh, M.A.R.; Pakdel, R.; Hayatdavoudi, P.; Nematy, M. Hypothyroidism and Ramadan fasting. J. Nutr. Fasting Health 2014, 2, 80–83. [Google Scholar]
- Al-Rawi, N.; Madkour, M.; Jahrami, H.; Salahat, D.; Alhasan, F.; BaHammam, A.; Al-Islam Faris, M.E. Effect of diurnal intermittent fasting during Ramadan on ghrelin, leptin, melatonin, and cortisol levels among overweight and obese subjects: A prospective observational study. PLoS ONE 2020, 15, e0237922. [Google Scholar] [CrossRef]
- Hernández-Mendoza, H.; Álvarez-Loredo, H.E.; Romero-Guzmán, E.T.; Gaytán-Hernández, D.; Chang-Rueda, C.; Martínez-Navarro, I.; Juárez-Flores, B.I.; Rios-Lugo, M.J. Relationship Between Serum Levels of Arsenic, Cadmium, and Mercury and Body Mass Index and Fasting Plasma Glucose in a Mexican Adult Population. Biol. Trace Elem. Res. 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.H.; Joo, Y.; Kim, M.-S.; Choe, H.K.; Tong, Q.; Kwon, O. Effects of Intermittent Fasting on the Circulating Levels and Circadian Rhythms of Hormones. Endocrinol. Metab. 2021, 36, 745–746. [Google Scholar] [CrossRef]
- Komaki, G.; Kanazawa, F.; Sogawa, H.; Mine, K.; Tamai, H.; Okamura, S.; Kubo, C. Alterations in lymphocyte subsets and pituitary-adrenal gland-related hormones during fasting. Am. J. Clin. Nutr. 1997, 66, 147–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diez, J.J.; Vigo, D.E.; Lloret, S.P.; Rigters, S.; Role, N.; Cardinali, D.P.; Chada, D.P. Sleep habits, alertness, cortisol levels, and cardiac autonomic activity in short-distance bus drivers: Differences between morning and afternoon shifts. J. Occup. Environ. Med. 2011, 53, 806–811. [Google Scholar] [CrossRef] [Green Version]
- Zangeneh, F.; Yazdi, R.S.; Naghizadeh, M.M.; Abedinia, N. Effect of Ramadan fasting on stress neurohormones in women with polycystic ovary syndrome. J. Fam. Reprod. Health 2015, 9, 51–57. [Google Scholar]
- Beasley, J.M.; Ange, B.A.; Anderson, C.A.; Miller Iii, E.R.; Holbrook, J.T.; Appel, L.J. Characteristics associated with fasting appetite hormones (obestatin, ghrelin, and leptin). Obesity 2009, 17, 349–354. [Google Scholar] [CrossRef]
- Wever, M.C.; van Meer, F.; Charbonnier, L.; Crabtree, D.R.; Buosi, W.; Giannopoulou, A.; Androutsos, O.; Johnstone, A.M.; Manios, Y.; Meek, C.L. Associations between ghrelin and leptin and neural food cue reactivity in a fasted and sated state. NeuroImage 2021, 240, 118374. [Google Scholar] [CrossRef]
- Bouhlel, E.; Denguezli, M.; Zaouali, M.; Tabka, Z.; Shephard, R.J. Ramadan fasting’s effect on plasma leptin, adiponectin concentrations, and body composition in trained young men. Int. J. Sport Nutr. Exerc. Metab. 2008, 18, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.L.; Heist, K.; DePaoli, A.M.; Veldhuis, J.D.; Mantzoros, C.S. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J. Clin. Investig. 2003, 111, 1409–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moro, T.; Tinsley, G.; Bianco, A.; Marcolin, G.; Pacelli, Q.F.; Battaglia, G.; Palma, A.; Gentil, P.; Neri, M.; Paoli, A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 2016, 14, 290. [Google Scholar] [CrossRef] [PubMed]
- Klok, M.D.; Jakobsdottir, S.; Drent, M. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: A review. Obes. Rev. 2007, 8, 21–34. [Google Scholar] [CrossRef]
- Kumar, S.; Kaur, G. Intermittent fasting dietary restriction regimen negatively influences reproduction in young rats: A study of hypothalamo-hypophysial-gonadal axis. PLoS ONE 2013, 8, e52416. [Google Scholar] [CrossRef]
- Mojo, M.; Greens, M.; Brain, M. The Man Diet: Intermittent Fasting to Boost Testosterone, Burn Fat, and Build Muscle. Available online: https://www.mannutra.com/the-man-diet-intermittent-fasting-to-boost-testosterone-burn-fat-and-build-muscle/ (accessed on 28 June 2022).
- Sinha-Hikim, I.; Roth, S.M.; Lee, M.I.; Bhasin, S. Testosterone-induced muscle hypertrophy is associated with an increase in satellite cell number in healthy, young men. Am. J. Physiol. Endocrinol. Metab. 2003, 285, E197–E205. [Google Scholar] [CrossRef] [Green Version]
- Baik, M.; Harrold, R.L.; Choi, C.B.; Slanger, W.D.; Sung, C.K.; Park, C.S. Energy restriction and testosterone implants alter ornithine decarboxylase gene expression in kidney of female rats. J. Nutr. 1992, 122, 1056–1061. [Google Scholar] [CrossRef]
- Rasmussen, M.H.; Frystyk, J.; Andersen, T.; Breum, L.; Christiansen, J.S.; Hilsted, J. The impact of obesity, fat distribution, and energy restriction on insulin-like growth factor-1 (IGF-1), IGF-binding protein-3, insulin, and growth hormone. Metabolism 1994, 43, 315–319. [Google Scholar] [CrossRef]
- Sonntag, W.E.; Lynch, C.D.; Cefalu, W.T.; Ingram, R.L.; Bennett, S.A.; Thornton, P.L.; Khan, A.S. Pleiotropic effects of growth hormone and insulin-like growth factor (IGF)-1 on biological aging: Inferences from moderate caloric-restricted animals. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 1999, 54, B521–B538. [Google Scholar] [CrossRef] [Green Version]
- Helms, E.R.; Zinn, C.; Rowlands, D.S.; Brown, S.R. A systematic review of dietary protein during caloric restriction in resistance trained lean athletes: A case for higher intakes. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 127–138. [Google Scholar] [CrossRef]
- Campbell, B.I.; Aguilar, D.; Colenso-Semple, L.M.; Hartke, K.; Fleming, A.R.; Fox, C.D.; Longstrom, J.M.; Rogers, G.E.; Mathas, D.B.; Wong, V. Intermittent energy restriction attenuates the loss of fat free mass in resistance trained individuals. A randomized controlled trial. J. Funct. Morphol. Kinesiol. 2020, 5, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips, S.M. A brief review of higher dietary protein diets in weight loss: A focus on athletes. Sports Med. 2014, 44, 149–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westerterp-Plantenga, M.S. Challenging energy balance-during sensitivity to food reward and modulatory factors implying a risk for overweight-during body weight management including dietary restraint and medium-high protein diets. Physiol. Behav. 2020, 221, 112879. [Google Scholar] [CrossRef] [PubMed]
- Santos-Hernández, M.; Miralles, B.; Amigo, L.; Recio, I. Intestinal signaling of proteins and digestion-derived products relevant to satiety. J. Agric. Food Chem. 2018, 66, 10123–10131. [Google Scholar] [CrossRef] [Green Version]
- Mariotti, F.; Gardner, C.D. Dietary protein and amino acids in vegetarian diets—A review. Nutrients 2019, 11, 2661. [Google Scholar] [CrossRef] [Green Version]
- Pesta, D.H.; Samuel, V.T. A high-protein diet for reducing body fat: Mechanisms and possible caveats. Nutr. Metab. 2014, 11, 53. [Google Scholar] [CrossRef] [Green Version]
- Zuo, L.; He, F.; Tinsley, G.M.; Pannell, B.K.; Ward, E.; Arciero, P.J. Comparison of high-protein, intermittent fasting low-calorie diet and heart healthy diet for vascular health of the obese. Front. Physiol. 2016, 7, 350. [Google Scholar] [CrossRef] [Green Version]
- Hager, A.-S.; Wolter, A.; Jacob, F.; Zannini, E.; Arendt, E.K. Nutritional properties and ultra-structure of commercial gluten free flours from different botanical sources compared to wheat flours. J. Cereal Sci. 2012, 56, 239–247. [Google Scholar] [CrossRef]
- Paoli, A.; Tinsley, G.; Bianco, A.; Moro, T. The influence of meal frequency and timing on health in humans: The role of fasting. Nutrients 2019, 11, 719. [Google Scholar] [CrossRef] [Green Version]
- Marques-Lopes, I.; Forga, L.; Martınez, J.A. Thermogenesis induced by a high-carbohydrate meal in fasted lean and overweight young men: Insulin, body fat, and sympathetic nervous system involvement. Nutrition 2003, 19, 25–29. [Google Scholar] [CrossRef]
- Rodríguez-Villar, C.; Manzanares, J.M.; Casals, E.; Pérez-Heras, A.; Zambón, D.; Gomis, R.; Ros, E. High-monounsaturated fat, olive oil-rich diet has effects similar to a high-carbohydrate diet on fasting and postprandial state and metabolic profiles of patients with type 2 diabetes. Metab. Clin. Exp. 2000, 49, 1511–1517. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.D.; Haymond, M.W.; Gerich, J.E.; Cryer, P.E.; Miles, J.M. Lipolysis during fasting. Decreased suppression by insulin and increased stimulation by epinephrine. J. Clin. Investig. 1987, 79, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Holland, O.B.; Wolfe, R.R. Importance of blood glucose concentration in regulating lipolysis during fasting in humans. Am. J. Physiol. Endocrinol. Metab. 1990, 258, E32–E39. [Google Scholar] [CrossRef] [PubMed]
- Coppack, S.W.; Jensen, M.D.; Miles, J.M. In Vivo regulation of lipolysis in humans. J. Lipid Res. 1994, 35, 177–193. [Google Scholar] [CrossRef]
- Bai, J.; Farias-Pereira, R.; Zhang, Y.; Jang, M.; Park, Y.; Kim, K.H. C. elegans ACAT regulates lipolysis and its related lifespan in fasting through modulation of the genes in lipolysis and insulin/IGF-1 signaling. BioFactors 2020, 46, 754–765. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Shakhmatova, E.; Iu, V.N. Responses of the rat kidney to the water load test and vasopressin administered during normal feeding and fasting. Ross. Fiziol. Zhurnal Im. IM Sechenova 2004, 90, 202–211. [Google Scholar]
- Finnell, J.S.; Saul, B.C.; Goldhamer, A.C.; Myers, T.R. Is fasting safe? A chart review of adverse events during medically supervised, water-only fasting. BMC Complement. Altern. Med. 2018, 18, 67. [Google Scholar] [CrossRef]
- Trabelsi, K.; Rebai, H.; El-Abed, K.; Stannard, S.R.; Khannous, H.; Masmoudi, L.; Sahnoun, Z.; Hakim, A.; Fellman, N.; Tabka, Z. Effect of ramadan fasting on body water status markers after a rugby sevens match. Asian J. Sports Med. 2011, 2, 186–194. [Google Scholar] [CrossRef] [Green Version]
- Aziz, A.R.; Wahid, M.F.; Png, W.; Jesuvadian, C.V. Effects of Ramadan fasting on 60 min of endurance running performance in moderately trained men. Br. J. Sports Med. 2010, 44, 516–521. [Google Scholar] [CrossRef]
- Solianik, R.; Sujeta, A. Two-day fasting evokes stress, but does not affect mood, brain activity, cognitive, psychomotor, and motor performance in overweight women. Behav. Brain Res. 2018, 338, 166–172. [Google Scholar] [CrossRef]
- Solianik, R.; Žlibinaitė, L.; Drozdova-Statkevičienė, M.; Sujeta, A. Forty-eight-hour fasting declines mental flexibility but improves balance in overweight and obese older women. Physiol. Behav. 2020, 223, 112995. [Google Scholar] [CrossRef] [PubMed]
- Gigou, P.-Y.; Dion, T.; Asselin, A.; Berrigan, F.; Goulet, E.D. Pre-exercise hyperhydration-induced bodyweight gain does not alter prolonged treadmill running time-trial performance in warm ambient conditions. Nutrients 2012, 4, 949–966. [Google Scholar] [CrossRef] [PubMed]
- Zorbas, Y.; Ichinose, M.; Sakagamis, M. Fluid electrolyte changes in physically healthy subjects during prolonged restriction of motor activity and daily hyperhydration. Mater. Med. Polona. Pol. J. Med. Pharm. 1993, 25, 97–107. [Google Scholar]
- Bak, A.; Tsiami, A.; Greene, C. Methods of assessment of hydration status and their usefulness in detecting dehydration in the elderly. Curr. Res. Nutr. Food Sci. 2017, 5, 43–54. [Google Scholar] [CrossRef]
- Trabelsi, K.; Stannard, S.R.; Chtourou, H.; Moalla, W.; Ghozzi, H.; Jamoussi, K.; Hakim, A. Monitoring athletes’ hydration status and sleep patterns during Ramadan observance: Methodological and practical considerations. Biol. Rhythm Res. 2018, 49, 337–365. [Google Scholar] [CrossRef]
- Ramadan, J.; Telahoun, G.; Al-Zaid, N.S.; Barac-Nieto, M. Responses to exercise, fluid, and energy balances during Ramadan in sedentary and active males. Nutrition 1999, 15, 735–739. [Google Scholar] [CrossRef]
- Roky, R.; Chapotot, F.; Hakkou, F.; Benchekroun, M.T.; Buguet, A. Sleep during Ramadan intermittent fasting. J. Sleep Res. 2001, 10, 319–327. [Google Scholar] [CrossRef]
- Bouhlel, E.; Shephard, R.J. Optimizing Physical Performance during Fasting and Dietary Restriction: Implications for Athletes and Sports Medicine; CRC Press: Boca Raton, FL, USA, 2015. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Bouhlel, E.; Salhi, Z.; Bouhlel, H.; Mdella, S.; Amamou, A.; Zaouali, M.; Mercier, J.; Bigard, X.; Tabka, Z.; Zbidi, A. Effect of Ramadan fasting on fuel oxidation during exercise in trained male rugby players. Diabetes Metab. 2006, 32, 617–624. [Google Scholar] [CrossRef]
- Attarzadeh Hosseini, S.R.; Hejazi, K. The Effects of Ramadan Fasting and Physical Activity on Blood Hematological-Biochemical Parameters. Iran. J. Basic Med. Sci. 2013, 16, 845–849. [Google Scholar]
- Hosseini, S.; Motahari Rad, M.; Hejazi, K. The effects of Ramadan fasting and physical activity on body composition and hematological biochemical parameters. J. Fasting Health 2014, 2, 96–103. [Google Scholar]
- Maughan, R.J.; Leiper, J.B.; Bartagi, Z.; Zrifi, R.; Zerguini, Y.; Dvorak, J. Effect of Ramadan fasting on some biochemical and haematological parameters in Tunisian youth soccer players undertaking their usual training and competition schedule. J. Sports Sci. 2008, 26, S39–S46. [Google Scholar] [CrossRef] [PubMed]
- DeLang, M.D.; Salamh, P.A.; Chtourou, H.; Saad, H.B.; Chamari, K. The Effects of Ramadan Intermittent Fasting on Football Players and Implications for Domestic Football Leagues Over the Next Decade: A Systematic Review. Sports Med. 2021, 52, 585–600. [Google Scholar] [CrossRef] [PubMed]
- Tayebi, S.M.; Hanachi, P.; Niaki, A.G.; Ali, P.N.; Ghaziani, F.G.-A. Ramadan fasting and weight-lifting training on vascular volumes and hematological profiles in young male weight-lifters. Glob. J. Health Sci. 2010, 2, 160. [Google Scholar] [CrossRef] [Green Version]
- Alwarawrah, Y.; Kiernan, K.; MacIver, N.J. Changes in nutritional status impact immune cell metabolism and function. Front. Immunol. 2018, 9, 1055. [Google Scholar] [CrossRef] [Green Version]
- Fock, R.A.; Vinolo, M.A.R.; Rocha, V.d.M.S.; de Sá Rocha, L.C.; Borelli, P. Protein-energy malnutrition decreases the expression of TLR-4/MD-2 and CD14 receptors in peritoneal macrophages and reduces the synthesis of TNF-α in response to lipopolysaccharide (LPS) in mice. Cytokine 2007, 40, 105–114. [Google Scholar] [CrossRef]
- Wang, X.; Yang, Q.; Liao, Q.; Li, M.; Zhang, P.; Santos, H.O.; Kord-Varkaneh, H.; Abshirini, M. Effects of intermittent fasting diets on plasma concentrations of inflammatory biomarkers: A systematic review and meta-analysis of randomized controlled trials. Nutrition 2020, 79, 110974. [Google Scholar] [CrossRef]
- Nobari, H.; Cholewa, J.M.; Pérez-Gómez, J.; Castillo-Rodríguez, A. Effects of 14-weeks betaine supplementation on pro-inflammatory cytokines and hematology status in professional youth soccer players during a competition season: A double blind, randomized, placebo-controlled trial. J. Int. Soc. Sports Nutr. 2021, 18, 42. [Google Scholar] [CrossRef]
- Adawi, M.; Watad, A.; Brown, S.; Aazza, K.; Aazza, H.; Zouhir, M.; Sharif, K.; Ghanayem, K.; Farah, R.; Mahagna, H. Ramadan fasting exerts immunomodulatory effects: Insights from a systematic review. Front. Immunol. 2017, 8, 1144. [Google Scholar] [CrossRef] [Green Version]
- Chaouachi, A.; Coutts, A.J.; Wong, D.P.; Roky, R.; Mbazaa, A.; Amri, M.; Chamari, K. Haematological, inflammatory, and immunological responses in elite judo athletes maintaining high training loads during Ramadan. Appl. Physiol. Nutr. Metab. 2009, 34, 907–915. [Google Scholar] [CrossRef] [Green Version]
- Ho, R.C.; Hirshman, M.F.; Li, Y.; Cai, D.; Farmer, J.R.; Aschenbach, W.G.; Witczak, C.A.; Shoelson, S.E.; Goodyear, L.J. Regulation of IκB kinase and NF-κB in contracting adult rat skeletal muscle. Am. J. Physiol. Cell Physiol. 2005, 289, C794–C801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nobari, H.; Nejad, H.A.; Kargarfard, M.; Mohseni, S.; Suzuki, K.; Carmelo Adsuar, J.; Pérez-Gómez, J. The Effect of Acute Intense Exercise on Activity of Antioxidant Enzymes in Smokers and Non-Smokers. Biomolecules 2021, 11, 171. [Google Scholar] [CrossRef]
- Mo’ez, A.-I.E.; Salem, M.L.; Jahrami, H.A.; Madkour, M.I.; BaHammam, A.S. Ramadan intermittent fasting and immunity: An important topic in the era of COVID-19. Ann. Thorac. Med. 2020, 15, 125–133. [Google Scholar]
- Moghadam, M.T.; Taati, B.; Paydar Ardakani, S.M.; Suzuki, K. Ramadan fasting during the COVID-19 pandemic; observance of health, nutrition and exercise criteria for improving the immune system. Front. Nutr. 2021, 7, 570235. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, C.H. A Single Bout of 36 Hours of Fasting in Humans Induces Potent Immunomodulatory Effects on Macrophage and Upregulates the Circulation of Multiple Metabolites That Mimic These Immunomodulatory Effects In Vitro and Extend Lifespan in C. elegans; University of California: Davis, CA, USA, 2020. [Google Scholar]
- Rynders, C.A.; Thomas, E.A.; Zaman, A.; Pan, Z.; Catenacci, V.A.; Melanson, E.L. Effectiveness of intermittent fasting and time-restricted feeding compared to continuous energy restriction for weight loss. Nutrients 2019, 11, 2442. [Google Scholar] [CrossRef] [Green Version]
- Chaouachi, A.; Coutts, A.J.; Chamari, K.; Wong, d.P.; Chaouachi, M.; Chtara, M.; Roky, R.; Amri, M. Effect of Ramadan intermittent fasting on aerobic and anaerobic performance and perception of fatigue in male elite judo athletes. J. Strength Cond. Res. 2009, 23, 2702–2709. [Google Scholar] [CrossRef] [Green Version]
- Abaidia, A.-E.; Daab, W.; Bouzid, M.A. Effects of Ramadan fasting on physical performance: A systematic review with meta-analysis. Sports Med. 2020, 50, 1009–1026. [Google Scholar] [CrossRef]
- Bouzid, M.A.; Abaïdia, A.-E.; Bouchiba, M.; Ghattassi, K.; Daab, W.; Engel, F.A.; Chtourou, H. Effects of Ramadan fasting on recovery following a simulated soccer match in professional soccer players: A pilot study. Front. Physiol. 2019, 10, 1480. [Google Scholar] [CrossRef] [Green Version]
- Fashi, M.; Ahmadizad, S.; Nobari, H.; Pérez-Gómez, J.; Oliveira, R.; Carlos-Vivas, J.; Ardigò, L.P. Effect of acute ramadan fasting on muscle function and buffering system of male athletes. Healthcare 2021, 9, 397. [Google Scholar] [CrossRef]
- Zouhal, H.; Saeidi, A.; Salhi, A.; Li, H.; Essop, M.F.; Laher, I.; Rhibi, F.; Amani-Shalamzari, S.; Abderrahman, A.B. Exercise training and fasting: Current insights. Open Access J. Sports Med. 2020, 11, 1–28. [Google Scholar] [CrossRef] [Green Version]
- Small, S.D.; Margolis, L.M. Impact of Dietary Carbohydrate Restriction versus Energy Restriction on Exogenous Carbohydrate Oxidation during Aerobic Exercise. Adv. Nutr. 2021, 13, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Levy, E.; Chu, T. Intermittent fasting and its effects on athletic performance: A review. Curr. Sports Med. Rep. 2019, 18, 266–269. [Google Scholar] [CrossRef] [PubMed]
- Stannard, S.R.; Buckley, A.J.; Edge, J.A.; Thompson, M.W. Adaptations to skeletal muscle with endurance exercise training in the acutely fed versus overnight-fasted state. J. Sci. Med. Sport 2010, 13, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Weinsier, R.L. Fasting—A review with emphasis on the electrolytes. Am. J. Med. 1971, 50, 233–240. [Google Scholar] [CrossRef]
- Darzabi, T.; Hejazi, K. The Effects of Ramadan Fasting on Electrolytes Index, Serum Osmolarity and Body Composition in Fasting and Non-Fasting Students: A Quasi-Experimental Study. Jundishapur J. Chronic Dis. Care 2020, 9, e100079. [Google Scholar] [CrossRef]
- Aragón-Vargas, L.F. Effects of fasting on endurance exercise. Sports Med. 1993, 16, 255–265. [Google Scholar] [CrossRef]
- Muñoz-Hernández, L.; Márquez-López, Z.; Mehta, R.; Aguilar-Salinas, C.A. Intermittent fasting as part of the management for T2DM: From animal models to human clinical studies. Curr. Diabetes Rep. 2020, 20, 13. [Google Scholar] [CrossRef]
- Lv, M.; Zhu, X.; Wang, H.; Wang, F.; Guan, W. Roles of caloric restriction, ketogenic diet and intermittent fasting during initiation, progression and metastasis of cancer in animal models: A systematic review and meta-analysis. PLoS ONE 2014, 9, e115147. [Google Scholar] [CrossRef]
- Zerguini, Y.; Kirkendall, D.; Junge, A.; Dvorak, J. Impact of Ramadan on physical performance in professional soccer players. Br. J. Sports Med. 2007, 41, 398–400. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Cotillard, A.; Vatier, C.; Bastard, J.-P.; Fellahi, S.; Stevant, M.; Allatif, O.; Langlois, C.; Bieuvelet, S.; Brochot, A. A dietary supplement containing cinnamon, chromium and carnosine decreases fasting plasma glucose and increases lean mass in overweight or obese pre-diabetic subjects: A randomized, placebo-controlled trial. PLoS ONE 2015, 10, e0138646. [Google Scholar] [CrossRef]
- Real-Hohn, A.; Navegantes, C.; Ramos, K.; Ramos-Filho, D.; Cahuê, F.; Galina, A.; Salerno, V.P. The synergism of high-intensity intermittent exercise and every-other-day intermittent fasting regimen on energy metabolism adaptations includes hexokinase activity and mitochondrial efficiency. PLoS ONE 2018, 13, e0202784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trabelsi, K.; Stannard, S.R.; Ghlissi, Z.; Maughan, R.J.; Kallel, C.; Jamoussi, K.; Zeghal, K.M.; Hakim, A. Effect of fed-versus fasted state resistance training during Ramadan on body composition and selected metabolic parameters in bodybuilders. J. Int. Soc. Sports Nutr. 2013, 10, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salama, B.; Hsairi, M.; Belaid, J.; Achour, N.; Achour, A.; Nacef, T. Food intake and energy expenditure in high school athletes before, during and after the month of Ramadan: Effect of fasting on performance. La Tunis. Méd. 1993, 71, 85–89. [Google Scholar]
- Mhenni, T.; Souissi, A.; Tayech, A.; Yousfi, N.; Mejri, M.A.; Chamari, K.; Souissi, N.; Khlifa, R.; Haddad, M. The effect of Ramadan fasting on the morning–evening difference in team-handball-related short-term maximal physical performances in elite female team-handball players. Chronobiol. Int. 2021, 38, 1488–1499. [Google Scholar] [CrossRef] [PubMed]
- Killen, S.S.; Marras, S.; McKenzie, D.J. Fast growers sprint slower: Effects of food deprivation and re-feeding on sprint swimming performance in individual juvenile European sea bass. J. Exp. Biol. 2014, 217, 859–865. [Google Scholar] [CrossRef] [Green Version]
- Chtourou, H.; Hammouda, O.; Souissi, H.; Chamari, K.; Chaouachi, A.; Souissi, N. The effect of Ramadan fasting on physical performances, mood state and perceived exertion in young footballers. Asian J. Sports Med. 2011, 2, 177–185. [Google Scholar] [CrossRef] [Green Version]
- Chtourou, H.; Hammouda, O.; Chaouachi, A.; Chamari, K.; Souissi, N. The effect of time-of-day and Ramadan fasting on anaerobic performances. Int. J. Sports Med. 2012, 33, 142–147. [Google Scholar] [CrossRef]
- Champagne, C.D.; Crocker, D.E.; Fowler, M.A.; Houser, D.S. Fasting physiology of the pinnipeds: The challenges of fasting while maintaining high energy expenditure and nutrient delivery for lactation. In Comparative Physiology of Fasting, Starvation, and Food Limitation; Springer: Berlin/Heidelberg, Germany, 2012; pp. 309–336. [Google Scholar]
- Güvenç, A. Effects of Ramadan fasting on body composition, aerobic performance and lactate, heart rate and perceptual responses in young soccer players. J. Hum. Kinet. 2011, 29, 79–91. [Google Scholar] [CrossRef]
- Dewanti, L.; Watanabe, C.; Ohtsuka, R. Unexpected changes in blood pressure and hematological parameters among fasting and nonfasting workers during Ramadan in Indonesia. Eur. J. Clin. Nutr. 2006, 60, 877–881. [Google Scholar] [CrossRef] [Green Version]
- Basilio, P.G.; Oliveira, A.P.C.d.; Castro, A.C.F.d.; Carvalho, M.R.d.; Zagatto, A.M.; Martinez, P.F.; Okoshi, M.P.; Okoshi, K.; Ota, G.E.; Reis, F.A.d. Intermittent fasting attenuates exercise training-induced cardiac remodeling. Arq. Bras. Cardiol. 2020, 115, 184–193. [Google Scholar] [CrossRef]
- Schübel, R.; Nattenmüller, J.; Schlett, C.L.; Stackelberg, O.V.; Johnson, T.S.; Kirsten, R.; Kauczor, H.-U.; Ulrich, C.; Kaaks, R.; Kühn, T. Effects of intermittent and continuous calorie restriction on body weight and metabolism over 50 wk. Am. J. Clin. Nutr. 2018, 108, 933–945. [Google Scholar] [CrossRef] [PubMed]


| Authors | Sample | Protocol | Results |
|---|---|---|---|
| Attarzadeh Hosseini et al. [84] | 26 healthy males (two experimental groups were compared before and after the training period). | Participants were divided into non-active fasting (n = 13) and active fasting (n = 13) groups. | Positive alterations in hematological–biochemical Indices (Hb and Hct decreased; plasma glucose reduced significantly). |
| Dewanti et al. [125] | 100 male outdoor workers. | Before the start of Ramadan and during the third week of the month of Ramadan. | Blood pressure was reduced in the partial-fasting and non-fasting groups, which was an unexpected result. While red blood cell production was suppressed, as evidenced by lower levels of Hb, red blood cells (RBC), and packed cell volume (PCV), the subjects were normocytic and normochromic based on normal mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) levels. |
| Chaouachi et al. [94] | 15 elite male judo athletes. | Before, during, and after Ramadan (maintaining their usual high training loads). | The RFP produced small but significant changes in the inflammatory, hormonal, and immunological profiles of the judo athletes. Serum C-reactive protein increased from 2.93 ± 0.26 mg·L−1 pre-Ramadan to 4.60 ± 0.51 mg·L−1 at the end of Ramadan. Haptoglobin and antitrypsin significantly increased during different phases of Ramadan, whereas homocysteine and prealbumin levels remained relatively unchanged. Albumin decreased slightly by mid-Ramadan, then recovered. Immunoglobulin A increased from 1.87 ± 0.56 g·L−1 before Ramadan to 2.49 ± 0.75 g·L−1 at the end and remained high for 3 weeks after it ended. There were no changes in leucocyte cell counts throughout the study. The mean blood levels of thyroid-stimulating hormone and free thyroxine increased significantly during the RFP. |
| Basilio et al. [126] | Wistar rats (n = 60) were randomly divided into 4 groups: control, exercise training (ET), intermittent fasting (IF), and exercise training plus intermittent fasting (ETI). | Over 12 weeks, control and ET animals were fed a standard, commercial diet ad libitum daily, while IF and ETI animals were fed every other day. In addition, the ET and ETI groups were submitted to a running protocol on a treadmill. | Exercise training increased the functional fitness of the ET and ETI groups and promoted cardiac fibrosis. The combination of IF and exercise training resulted in a smaller area under the blood-glucose curve and reduced the cardiomyocyte cross-sectional area and the interstitial collagen fraction in the ETI group as compared to the ET group. ERK and JNK expression levels were similar among groups (p > 0.05). |
| Schübel et al. [127] | 150 overweight and obese participants (50% males, 50% females), age 35–65, with BMIs between 25–40 kg/m2 were divided into three groups (CCR: n = 49, ICR: n = 49, CG: n = 52). | →ICR: 5 days without energy restriction and 2 days with 75% ↓ in energy needs. → CCR: 20% daily ↓ in energy needs. →CG: NC in calorie intake. Over a 12-week intervention phase, a 12-week maintenance phase, and a 26-week follow-up phase. | Body weight during the intervention phase decreased by 7.1% ± 0.7% (p < 0.001) in the ICR group, by 5.2% ± 0.6% (p = 0.053) in the CCR group, and by 3.3% ± 0.6% (NS) in the CG group. At the final follow-up assessment (week 50), weight loss was 5.2% ± 1.2 (p = 0.01) in the ICR group, 4.9% ± 1.1% (p = 0.89) in the CCR group, and 1.7% ± 0.8% in the CG group. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nobari, H.; Saedmocheshi, S.; Murawska-Ciałowicz, E.; Clemente, F.M.; Suzuki, K.; Silva, A.F. Exploring the Effects of Energy Constraints on Performance, Body Composition, Endocrinological/Hematological Biomarkers, and Immune System among Athletes: An Overview of the Fasting State. Nutrients 2022, 14, 3197. https://doi.org/10.3390/nu14153197
Nobari H, Saedmocheshi S, Murawska-Ciałowicz E, Clemente FM, Suzuki K, Silva AF. Exploring the Effects of Energy Constraints on Performance, Body Composition, Endocrinological/Hematological Biomarkers, and Immune System among Athletes: An Overview of the Fasting State. Nutrients. 2022; 14(15):3197. https://doi.org/10.3390/nu14153197
Chicago/Turabian StyleNobari, Hadi, Saber Saedmocheshi, Eugenia Murawska-Ciałowicz, Filipe Manuel Clemente, Katsuhiko Suzuki, and Ana Filipa Silva. 2022. "Exploring the Effects of Energy Constraints on Performance, Body Composition, Endocrinological/Hematological Biomarkers, and Immune System among Athletes: An Overview of the Fasting State" Nutrients 14, no. 15: 3197. https://doi.org/10.3390/nu14153197
APA StyleNobari, H., Saedmocheshi, S., Murawska-Ciałowicz, E., Clemente, F. M., Suzuki, K., & Silva, A. F. (2022). Exploring the Effects of Energy Constraints on Performance, Body Composition, Endocrinological/Hematological Biomarkers, and Immune System among Athletes: An Overview of the Fasting State. Nutrients, 14(15), 3197. https://doi.org/10.3390/nu14153197











