Dietitians’ Attitudes and Understanding of the Promotion of Grains, Whole Grains, and Ultra-Processed Foods
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Design
2.2. Participants
2.3. Response Analysis
3. Results
3.1. Demographics
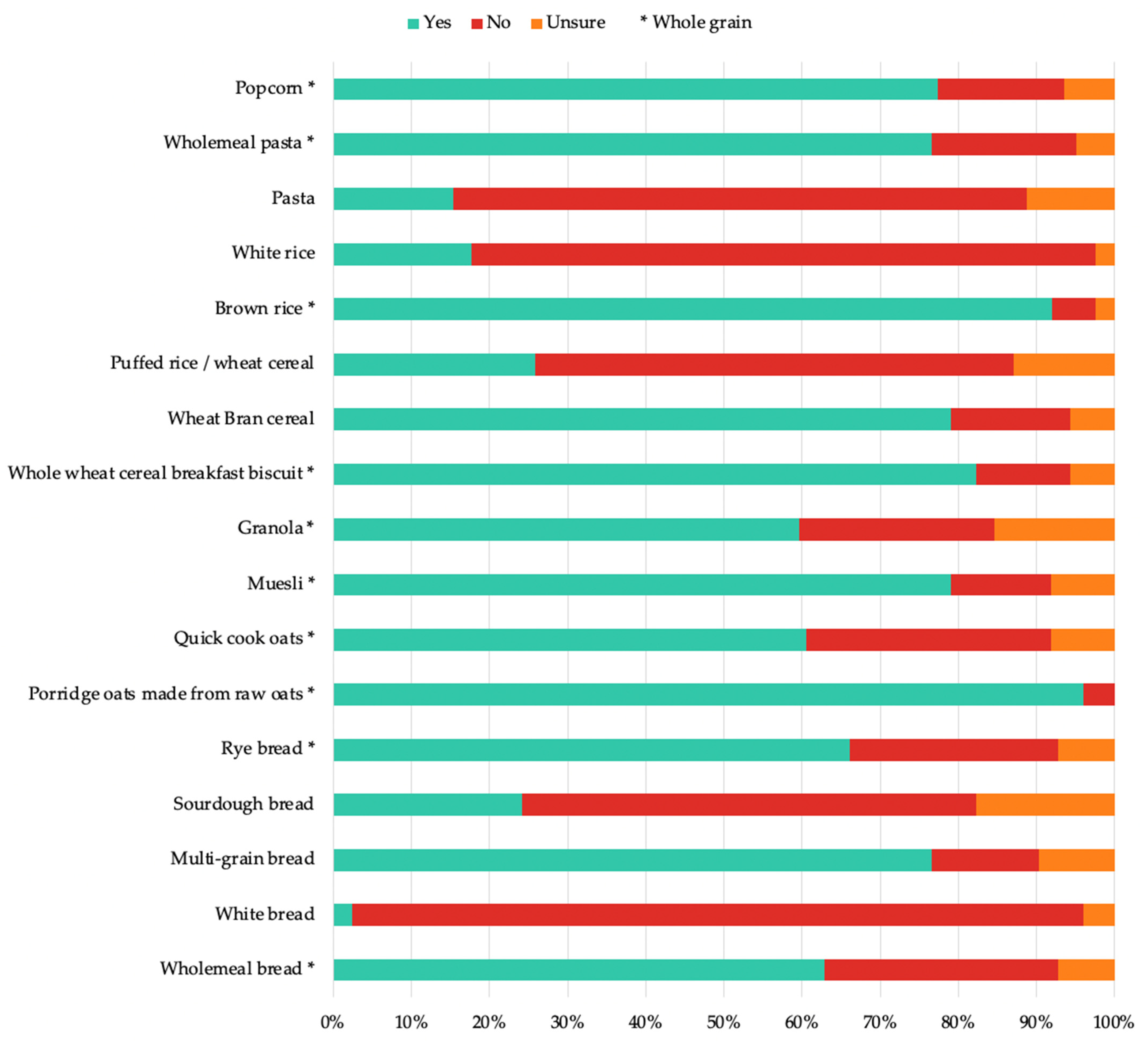
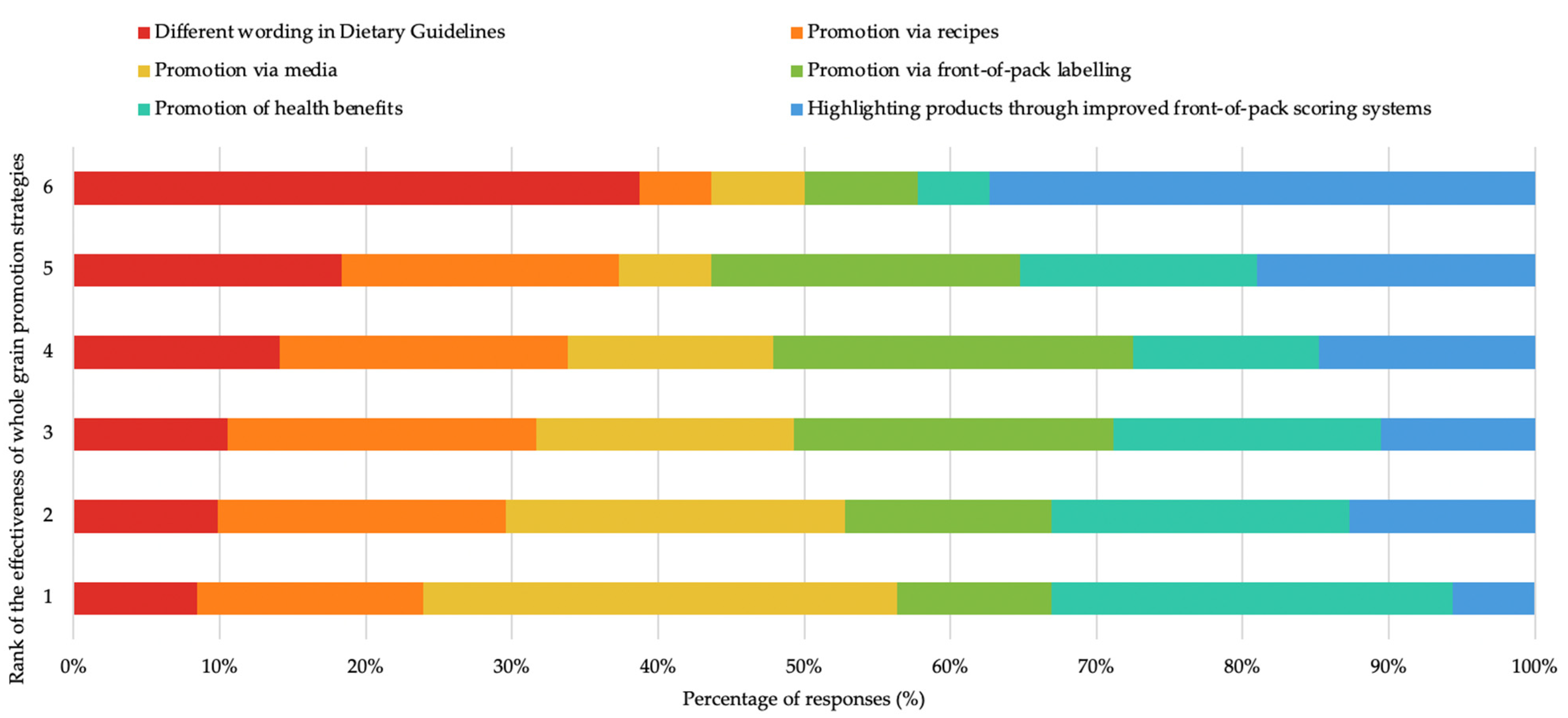
3.2. Perceived Value, Attitudes, and Recommendations of Grains, including Whole Grains
3.3. Perceived Barriers to Whole-Grain Consumption
3.4. Knowledge, Attitudes and Use of the NOVA Classification System
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thurecht, R.L.; Pelly, F.E.; Cooper, S.L. The influence of current food and nutrition trends on dietitians’ perceptions of the healthiness of packaged food. Public Health Nutr. 2020, 23, 2124–2131. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Cannon, G.; Levy, R.; Moubarac, C.; Jaime, P.; Martins, A.P.; Canella, D.; Louzada, M.; Parra, D. NOVA. The star shines bright. World Nutr. 2016, 7, 28–38. [Google Scholar]
- Dietary Guidelines for the Brazilian Population Ministry of Health of Brazil 2015. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/dietary_guidelines_brazilian_population.pdf (accessed on 11 February 2021).
- Elizabeth, L.; Machado, P.; Zinöcker, M.; Baker, P.; Lawrence, M. Ultra-processed foods and health outcomes: A narrative review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.-C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, C.A. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009, 12, 729–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mackerras, D. Mis-match between the healthy food and the ultra-processed food classifications in Australia (OR14-03-19). Curr. Dev. Nutr. 2019, 3 (Suppl. 1), nzz038.OR14-03-19. [Google Scholar] [CrossRef] [Green Version]
- National Health and Medical Research Council. Eat For Health Educator Guide; National Health and Medical Research Council: Canberra, Australia, 2013. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Costa Louzada, M.L.; Pereira Machado, P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; FAO: Rome, Italy, 2019. [Google Scholar]
- Galea, L.M.; Beck, E.J.; Probst, Y.C.; Cashman, C.J. Whole grain intake of Australians estimated from a cross-sectional analysis of dietary intake data from the 2011–13 Australian Health Survey. Public Health Nutr. 2017, 20, 2166–2172. [Google Scholar] [CrossRef] [Green Version]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Sandvik, P.; Nydahl, M.; Kihlberg, I.; Marklinder, I. Consumers’ health-related perceptions of bread—Implications for labeling and health communication. Appetite 2018, 121, 285–293. [Google Scholar] [CrossRef]
- Chase, K.; Reicks, M.; Jones, J.M. Applying the theory of planned behavior to promotion of whole-grain foods by dietitians. J. Am. Diet. Assoc. 2003, 103, 1639–1642. [Google Scholar] [CrossRef]
- Manning, M. The effects of subjective norms on behaviour in the theory of planned behaviour: A meta-analysis. Br. J. Soc. Psychol. 2009, 48, 649–705. [Google Scholar] [CrossRef] [PubMed]
- Qualtrics. Provo, Utah, USA. 2021. Available online: https://www.qualtrics.com (accessed on 30 February 2022).
- Ajzen, I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J. Appl. Soc. Psychol. 2002, 32, 665–683. [Google Scholar] [CrossRef]
- Phillips, F.; Ruxton, C.H.S. Scientific evidence and daily food for a better life: Milan, 19 June 2015. Public Health 2016, 140, 73–79. [Google Scholar] [CrossRef]
- The Eatwell Guide: Public Health England. 2016. Available online: https://www.gov.uk/government/publications/the-eatwell-guide (accessed on 20 July 2021).
- Dietary Guidelines for Americans 2020–2025: U.S. Department of Agriculture and U.S. Department of Health and Human Services. 2020. Available online: https://www.dietaryguidelines.gov/ (accessed on 20 July 2022).
- Botelho, R.; Araújo, W.; Pineli, L. Food formulation and not processing level: Conceptual divergences between public health and food science and technology sectors. Crit. Rev. Food Sci. Nutr. 2018, 58, 639–650. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.M.; Batterham, M.J.; Ray, S.; Beck, E.J. Whole grain, bran and cereal fibre consumption and CVD: A systematic review. Br. J. Nutr. 2019, 121, 914–937. [Google Scholar] [CrossRef] [PubMed]
- Sadler, C.R.; Grassby, T.; Hart, K.; Raats, M.M.; Sokolović, M.; Timotijevic, L. “Even We Are Confused”: A thematic analysis of professionals’ perceptions of processed foods and challenges for communication. Front. Nutr. 2022, 9, 826162. [Google Scholar] [CrossRef] [PubMed]
- Marchese, L.; Livingstone, K.M.; Woods, J.L.; Wingrove, K.; Machado, P. Ultra-processed food consumption, socio-demographics and diet quality in Australian adults. Public Health Nutr. 2021, 25, 94–104. [Google Scholar] [CrossRef]
- Sawicki, C.M.; Jacques, P.F.; Lichtenstein, A.H.; Rogers, G.T.; Ma, J.; Saltzman, E.; McKeown, N.M. Whole- and refined-grain consumption and longitudinal changes in cardiometabolic risk factors in the Framingham Offspring Cohort. J. Nutr. 2021, 151, 2790–2799. [Google Scholar] [CrossRef]
- Blumfield, M.; Starck, C.; Keighley, T.; Petocz, P.; Roesler, A.; Abbott, K.; Cassettari, T.; Marshall, S.; Fayet-Moore, S. Diet and economic modelling to improve the quality and affordability of the Australian diet for low and medium socioeconomic households. Int. J. Environ. Res. Public Health 2021, 18, 5771. [Google Scholar] [CrossRef]
- Cole, M.B.; Augustin, M.A.; Robertson, M.J.; Manners, J.M. The science of food security. NPJ Sci. Food 2018, 2, 1–8. [Google Scholar] [CrossRef]
- Bisogni, C.A.; Jastran, M.; Seligson, M.; Thompson, A. How people interpret healthy eating: Contributions of qualitative research. J. Nutr. Educ. Behav. 2012, 44, 282–301. [Google Scholar] [CrossRef] [PubMed]

| Demographic Characteristics | Count (%) |
|---|---|
| Gender | |
| Female | 142 (94.7) |
| Male | 6 (4.0) |
| Prefer not to answer | 2 (1.3) |
| Prefer to self-describe | 0 (0) |
| Age | |
| 18–24 | 19 (12.7) |
| 25–34 | 51 (34.0) |
| 35–44 | 31 (20.7) |
| 45–54 | 25 (16.7) |
| 55–64 | 16 (10.7) |
| 65+ | 8 (5.3) |
| Level of Education | |
| Certificate/diploma | 3 (2.0) |
| Bachelor degree | 64 (42.7) |
| Masters degree | 77 (51.3) |
| Ph.D. | 6 (4.0) |
| Dietetic credential | |
| Accredited practicing dietitian | 110 (73.3) |
| Registered dietitian | 35 (23.3) |
| Qualified dietitian but not registered | 3 (2.0) |
| Other | 2 (1.3) |
| Country dietetics education was completed | |
| Australia | 102 (68.0) |
| New Zealand | 5 (3.3) |
| Canada | 3 (2.0) |
| United States | 33 (22.0) |
| United Kingdom | 1 (0.7) |
| South Africa | 4 (2.7) |
| Other | 2 (1.3) |
| Country currently practising as a dietitian | |
| Australia | 110 (73.3) |
| New Zealand | 2 (1.3) |
| Canada | 0 (0.0) |
| United States | 30 (20.0) |
| United Kingdom | 2 (1.3) |
| South Africa | 2 (1.3) |
| Other | 4 (2.7) |
| Years practised as a dietitian | |
| ≤5 years | 50 (33.3) |
| 6–10 years | 38 (25.3) |
| 11–20 years | 24 (16.0) |
| >20 years | 38 (25.3) |
| Main area of work | |
| Community/public health | 31 (20.7) |
| Food service | 3 (2.0) |
| Academia/education | 8 (5.3) |
| Research | 4 (2.7) |
| Clinical (hospital) | 32 (21.3) |
| Clinical (primary care) | 13 (8.7) |
| Private practice | 38 (25.3) |
| Corporate nutrition | 4 (2.7) |
| Food industry | 3 (2.0) |
| Retail | 3 (2.0) |
| Other | 11 (7.3) |
| Question | Response | Count (%) |
|---|---|---|
| Do you recommend or discuss grain foods in consultation, groups sessions or via media messages? | Yes No | 149 (99.3) 1 (0.7) |
| Are grain foods prioritised in your advice for general healthy eating? | Yes No Other | 116 (77.3) 19 (12.7) 15 (10.0) |
| Do you promote amounts of grain foods based on National Dietary Guidelines? | Yes No | 121 (80.7) 29 (19.3) |
| Do you recommend whole grain foods? | Yes No | 148 (99.3) 1 (0.7) |
| Considering your advice on general healthy eating, how often do you recommend whole grain foods in dietetic practice? | Always Most of the time About half of the time Sometimes Never | 74 (49.7) 63 (42.3) 6 (4.0) 6 (4.0) 0 (0.0) |
| What sources of information do you most often use for your advice relating to whole grain food intake? * | National Dietary Guidelines Government Resources Resources from professional organisations Resources from non-government organisations Other | 102 (68.5) 26 (17.5) 82 (55.0) 44 (29.5) 11 (7.4) |
| Question | Response | Count (%) |
|---|---|---|
| In your opinion, what are the nutrition and health benefits of whole grain foods? * | High fibre | 144 (96.6) |
| Low GI | 120 (80.5) | |
| Improves weight control | 104 (69.8) | |
| Improves blood glucose control | 133 (89.3) | |
| Reduces insulin resistance | 78 (52.4) | |
| Increases HDL-cholesterol | 40 (26.9) | |
| Decreases LDL-cholesterol | 95 (63.8) | |
| Lowers blood pressure | 51 (34.2) | |
| Reduces inflammation | 62 (41.6) | |
| Reduces risk of heart disease | 102 (68.5) | |
| Management and reduced risk of type 2 diabetes | 112 (75.2) | |
| Protective factor against colorectal cancer | 119 (79.9) | |
| Other | 18 (12.1) | |
| Typically, in what situations might you prioritise whole grain foods in dietetic practice? * | I do not prioritise whole-grain foods in practice | 1 (0.7) |
| In general dietary advice | 112 (75.2) | |
| To increase dietary fibre intake | 130 (87.3) | |
| For weight control | 81 (54.4) | |
| For diabetes management | 106 (71.1) | |
| For blood-glucose control | 105 (70.5) | |
| For cholesterol management | 99 (66.4) | |
| For blood-pressure management | 43 (29.9) | |
| Other | 8 (5.4) | |
| Are there any reasons why you would not recommend whole grain foods to a patient/client/group? | Contraindicated | 87 (56.9) |
| No reasons | 46 (30.1) | |
| Individual taste preferences | 10 (6.5) | |
| Low-carbohydrate diet | 5 (3.3) | |
| Other client priorities | 2 (1.3) | |
| Weight loss | 2 (1.3) |
| Question | Response | Count (%) |
|---|---|---|
| In your opinion, what are the barriers to whole grain food consumption? * | Taste | 83 (71.6) |
| Concerns about carbohydrate intake | 66 (56.9) | |
| Culinary skills (e.g., easy recipes) | 65 (56.0) | |
| Time taken to prepare | 52 (44.8) | |
| Price | 46 (39.7) | |
| Other (please specify) | 37 (31.9) | |
| Availability | 26 (22.4) | |
| There are no barriers | 2 (1.7) | |
| What strategies could help overcome the barriers to whole grain consumption? | Education | 86 (51.5) |
| Public-health-promotion messages | 31 (18.6) | |
| Food-industry action | 24 (14.4) | |
| Improving individual acceptability | 22 (13.2) | |
| Using evidence-based practice | 2 (1.2) | |
| Not sure | 2 (1.2) |
| Statement | Count (%) | |||
|---|---|---|---|---|
| Disagree | Neither Agree-Nor Disagree | Agree | Not Sure | |
| I agree with the classification in NOVA for breads as “ultra-processed foods” if they are packaged and fortified. | 75 (61.0) | 16 (13.0) | 29 (23.6) | 3 (2.4) |
| I agree with the classification in NOVA for ready-to-eat breakfast cereals as “ultra-processed foods” even if they are fortified. | 62 (50.4) | 23 (18.7) | 34 (27.6) | 4 (3.3) |
| Knowing that some whole grain breads and ready-to-eat cereals are classified as “ultra-processed foods” has negatively impacted my perception of these sources of whole grains. | 63 (51.2) | 28 (22.8) | 30 (24.4) | 2 (1.6) |
| I am less inclined to recommend whole grain breads and ready-to-eat cereals in dietetic practice knowing that they are classified as “ultra-processed foods”. | 83 (67.5) | 21 (17.1) | 16 (13.0) | 3 (2.4) |
| I am less inclined to recommend avoidance of ultra-processed foods knowing that they may include some whole grain foods (such as some ready-to-eat cereals and breads). | 43 (35.0) | 29 (23.6) | 47 (38.2) | 4 (3.3) |
| I generally agree to avoid ultra-processed foods but do not agree that whole grain breads and cereals should be included in this classification. | 10 (8.1) | 16 (13.0) | 92 (74.8) | 5 (4.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krois, N.; Hughes, J.; Grafenauer, S. Dietitians’ Attitudes and Understanding of the Promotion of Grains, Whole Grains, and Ultra-Processed Foods. Nutrients 2022, 14, 3026. https://doi.org/10.3390/nu14153026
Krois N, Hughes J, Grafenauer S. Dietitians’ Attitudes and Understanding of the Promotion of Grains, Whole Grains, and Ultra-Processed Foods. Nutrients. 2022; 14(15):3026. https://doi.org/10.3390/nu14153026
Chicago/Turabian StyleKrois, Natasha, Jaimee Hughes, and Sara Grafenauer. 2022. "Dietitians’ Attitudes and Understanding of the Promotion of Grains, Whole Grains, and Ultra-Processed Foods" Nutrients 14, no. 15: 3026. https://doi.org/10.3390/nu14153026
APA StyleKrois, N., Hughes, J., & Grafenauer, S. (2022). Dietitians’ Attitudes and Understanding of the Promotion of Grains, Whole Grains, and Ultra-Processed Foods. Nutrients, 14(15), 3026. https://doi.org/10.3390/nu14153026





