Abstract
Despite a close relationship between chronic kidney disease (CKD) and uric acid level, few studies have examined the relationship between uric acid level and fat intake by kidney function status. Therefore, we investigated the association between dietary fat intake and hyperuricemia with and without decreased kidney function in males living in Shika Town, Ishikawa Prefecture, Japan. This study included 361 males with a mean age of 60.7 years. Dietary fat and fatty acid intakes were evaluated using the brief-type self-administered diet history questionnaire. Reduced kidney function was defined as an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2, while hyperuricemia was defined as a serum uric acid level >7.0 mg/dL. A two-way analysis of covariance showed that saturated fatty acid (p = 0.026), monounsaturated fatty acid (p = 0.014), and polyunsaturated fatty acid (p = 0.022) were significantly lower in the high uric acid group than in the normal uric acid group. In multiple logistic analysis stratified by renal function, lipid intake was negatively associated with hyperuricemia in the low eGFR group. These findings suggest that higher dietary lipid/fatty acid intake may be effective in the prevention and treatment of hyperuricemia in men with CKD.
1. Introduction
Hyperuricemia is a common biochemical abnormality observed in 20–25% of adult males and only a few females [1,2]. The prevalence of gout induced by hyperuricemia has been reported to be as high as 7% in males aged of ≥65 years [3]. In addition to gout, the pathogenesis of hyperuricemia has been implicated in visceral fat accumulation and insulin resistance, both of which are closely related to organ damage such as atherosclerosis, cardiovascular disease, and chronic kidney disease (CKD) [4].
Dietary factors that contribute to elevated serum uric acid levels and the development of gout include increased intake of sugar [5], alcohol [6,7], and purines [8]. Therefore, lifestyle modification is essential for hyperuricemia with or without drug therapy. To optimize energy intake, measures such as restriction of alcohol consumption and avoidance of excess purine intake have been recommended in addition to dietary therapy [9,10]. Regarding dietary style, the Dietary Approaches to Stop Hypertension (DASH) diet and the Mediterranean diet reduce serum uric acid [11,12,13]. However, only a few studies have investigated the relationship between serum uric acid levels and dietary lipids [14,15,16]. An intervention study in healthy young adults revealed that n-3 polyunsaturated fatty acid intake with 2 g/day of fish oil for 8 weeks reduced serum uric acid levels [14]. Another intervention study in healthy older males reported that a 3-month intake of 700 mg/day of omega-3 lipid supplements reduced serum uric acid levels [15]. Regarding dietary style, a 16-week intervention with a calorie-restricted diet in which saturated fatty acids were substituted for monounsaturated and polyunsaturated fatty acids was shown to induce weight loss and reduce serum uric acid levels in males with gout [16]. However, all of these intervention studies used dietary supplements or diets with adjusted dietary lipid composition, and none examined the direct relationship between dietary lipid intake and serum uric acid levels.
Given the importance of dietary therapy for hyperuricemia according to kidney function from the viewpoint that the kidneys play a key role in regulating serum uric acid levels [17], this study aimed to clarify the relationship between dietary lipids and hyperuricemia stratified by kidney function in males from a community-based cross-sectional study.
2. Materials and Methods
2.1. Study Population
The study participants were residents of Shika Town, Ishikawa, Japan, who underwent a medical checkup between April 2013 and March 2018. This cross-sectional study was conducted as part of the Shika study [18,19,20]. The participants were middle-aged and older adults aged of ≥40 years living in two model districts (Horimatsu and Higashimasuho).
A total of 1184 residents received medical checkups during the study period. Of these, 1175 underwent uric acid measurement, among whom 1161 did not receive treatment for hyperuricemia between 2011 and 2012, the years preceding the start of the medical checkups. Among the 1161 individuals, 808 responded to the brief-type self-administered diet history questionnaire (BDHQ) [21]. Nutrient intake was converted to a percentage of daily energy intake using the density method. Seven hundred and ninety-nine participants had a daily caloric intake of >600 kcal and <4000 kcal. Additionally, uric acid levels were classified into two groups according to reference values. As only 8 of the females were in the high uric acid group, 361 males were included in the final analysis (Figure 1).
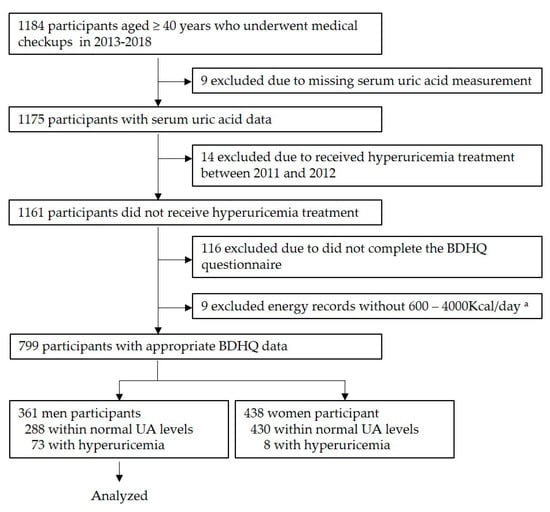
Figure 1.
Participant recruitment chart. a This reference value was chosen for the following reasons: less than 600 kcal/day is equivalent to half the energy intake required for the lowest physical activity category; more than 4000 kcal/day is equivalent to 1.5 times the energy intake required for the medium physical activity category. Abbreviations: BDHQ, brief-type self-administered diet history questionnaire.
2.2. Demographic Data and Medical History
Information on the demographic characteristics of the participants, including age, sex, family composition, job status, educational background, exercise habit, and smoking habit, was collected using a questionnaire [18]. Family composition was classified according to living alone or not. Educational background was classified into the following four levels: 1, elementary and junior high school; 2, high school; 3, junior college or vocational school; and 4, university and higher. Exercise habits were categorized on a 5-point scale based on the weekly frequency of exercise: 1, daily; 2, 5–6 days per week; 3, 3–4 days per week; 4, 1–2 days per week; and 5, none. Smoking habits were classified according to whether the individuals was a current smoker or not. Additionally, participants were asked questions relating to their diabetes and hypertension treatment histories [18].
2.3. Assessment of Kidney Function and Hyperuricemia
To evaluate kidney function, the estimated glomerular filtration rate (eGFR) was calculated using the following formula [22]:
eGFR (mL/min/1.73 m2) = 194 × serum creatinine level−1.094 × age−0.287 (× 0.739 for females)
An eGFR of <60 mL/min/1.73 m2 was defined as reduced kidney function, based on the definition of the Clinical Practice Guideline for Evaluation and Management Chronic Kidney Disease of KDIGO 2012 [23]. Serum creatinine concentrations were measured using an enzymatic method.
The definition of hyperuricemia was based on the “Guidelines for the Treatment of Hyperuricemia and Gout” by the Japanese Society for Gout and Uric & Nucleic Acids [10]. Regardless of sex, participants with uric acid levels of >7.0 mg/dL measured by the enzyme (uricase) method were defined as the high uric acid group, while those with uric acid levels <7.0 mg/dL were defined as the normal uric acid group.
2.4. Evaluation of Nutrient Intake
The BDHQ was used to evaluate nutrient intake [21]. The BDHQ is a brief version of the diet history questionnaire, asking study participants about their consumption frequency of 58 food and beverage items. These food and beverage items were selected from foods commonly consumed in Japan, mainly from a food list used in the National Health and Nutrition Survey of Japan. A previous study in a Japanese population compared the estimated energy and nutrient intake calculated using the BDHQ with data obtained from a 16-day diet record. The energy-adjusted intake of the 42 nutrients were correlated with the diet record, and the Pearson correlation coefficients were 0.45 to 0.61 in females, and 0.41 to 0.63 in males.
The BDHQ has been validated in previous studies as a suitable method for assessing nutrient intake in the Japanese population [24,25]. This study used fat intake adjusted for estimated energy intake. The fat intake consisted of total fat (% energy), animal fat (% energy), plant fat (% energy), saturated fatty acid (SFA) (% energy), monounsaturated fatty acid (MUFA) (% energy), polyunsaturated fatty acid (PUFA) (% energy), n-3 PUFA (% energy), and n-6 PUFA (% energy). Alcohol intake was also assessed from the BDHQ.
2.5. Other Variables
Participants’ body mass index (BMI) was calculated using the following equation:
BMI = weight (kg)/[height (m)]2
2.6. Statistical Analysis
The Student’s t-test was performed to examine the relationships between continuous variables, while the chi-square test was used to investigate the relationships between categorical variables. A two-way analysis of covariance (ANCOVA) was conducted to examine the main effects and interactions between uric acid level and eGFR value on fat and fatty acid intake. The following covariates were used in this study regarding the epidemiological survey by Choi et al. [26]: age, job status, educational background, exercise habit, current smoker, alcohol intake, BMI, diabetes treatment, and hypertension treatment. Furthermore, multiple logistic regression analysis was performed, stratifying the two groups into normal kidney function and reduced kidney function groups, with the two uric acid groups as the dependent variable and fat and fatty acid intake as the independent variable, adjusted for the same covariates as in the two-way ANCOVA.
The p-values shown in all analyses were two-tailed, with a p-value < 0.05 being considered statistically significant. IBM SPSS® Statistics 26.0 (SPSS Inc., Armonk, NY, USA) was used to perform statistical analysis.
3. Results
3.1. Participant Characteristics
Table 1 shows the characteristics of the 361 analyzed participants. The mean age (SD) of the participants was 60.7 (10.0) years. Age (p < 0.001), BMI (p = 0.029), uric acid level (p = 0.004), and the proportion of hypertension treatment (p = 0.015) were significantly higher in the reduced kidney function group than those in the normal kidney function group. However, the proportion of current smokers (p = 0.010) and alcohol intake (p = 0.005) were significantly lower in the reduced kidney function group compared to the normal kidney function group. Among fat intake, SFA intake in the reduced renal function group was significantly higher than that in the normal kidney function group (p = 0.013).

Table 1.
Participant characteristics.
3.2. Comparison between the Two Uric Acid Groups
Table 2 shows a comparison between the normal uric acid group and the high uric acid group. Alcohol intake (p = 0.009) and BMI (p = 0.048) were significantly higher in the high uric acid group than in the normal uric acid group. In contrast, age (p = 0.020), the proportion of diabetes treatment (p < 0.001), and eGFR (p = 0.014) were significantly lower in the high uric acid group than in the normal uric acid group. Among fat intake, plant fat intake (p = 0.025) was significantly lower in the high uric acid group than in the normal uric acid group.

Table 2.
Comparison between the normal uric acid group and the high uric acid group.
3.3. Analysis of Covariance
Table 3 shows the results of the two-way ANCOVA for the two uric acid and two kidney function groups on fat and fatty acid intake. Covariates were adjusted for age, job status, education background, exercise habits, current smoker, alcohol intake, BMI, diabetes treatment, and hypertension treatment. There was an interaction between serum uric acid levels and kidney function on dietary fat intake. Specifically, in the reduced kidney function group, with the exception of animal fat and n-3 fatty acids, all fat and fatty acid intakes in the high uric acid group were significantly lower than those in the normal uric acid group, whereas, in the normal kidney function group, this relationship was not found between the two uric acid groups.

Table 3.
Two-way ANCOVA for the two uric acid and two kidney function groups on fat and fatty acid intake.
3.4. Association between Uric Acid Level and Fat Intake after Stratification into Two eGFR Groups
Table 4 shows the multiple logistic regression analysis of the relationship between fat and fatty acid intake and high uric acid levels, stratified by normal and reduced kidney function groups. Covariates were adjusted for the same variables as in the two-way ANCOVA. With the exception of animal fat, fat and fatty acid intake were inversely related to hyperuricemia in the reduced kidney function group, whereas no such relationship was observed in the normal kidney function group.

Table 4.
Multiple logistic regression analysis of the relationship between fat and fatty acid intake and high uric acid levels.
4. Discussion
This study examined the association between dietary fat and fatty acid intake and hyperuricemia stratified by kidney function in middle-aged and older Japanese males. Our findings revealed that fat and fatty acid intake, including SFA, MUFA, and PUFA, was inversely related to hyperuricemia in males with reduced kidney function. Therefore, higher fat and fatty acid intake is likely to lower serum uric acid levels in males with reduced kidney function.
The high uric acid group had higher alcohol intake, higher BMI, and lower eGFR than the normal uric acid group. Alcohol consumption, obesity, and CKD are well-known risk factors for hyperuricemia and gout [4,9,27]. Additionally, plant fat in the high uric acid group was significantly lower than that in the normal uric acid group. Similarly, PUFA intake was lower in the high uric acid group. Previous studies examining the relationship between fatty acid intake and serum uric acid levels include a randomized controlled trial comparing the effects of fish oil intake containing n-3 PUFA [14], an intervention study using n-3 PUFA supplements [15], and an intervention study using a calorie-restricted diet in which SFA was replaced with unsaturated fatty acids [16]. The difference in the fatty acid intake between the two uric acid level groups observed in this study seems to be consistent with these previous studies.
Previous reports on dietary style restricting the consumption of fats and meats include the DASH diet and Mediterranean diets, which are well-known to be effective for achieving appropriate uric acid levels, and have different uric acid-lowering effects, depending on patient characteristics [28,29,30]. A randomized, crossover feeding trial by Juraschek et al. [28] demonstrated that the DASH diet lowered serum uric acid among participants with a higher uric acid level at baseline. Chatzipavlou et al. [29] performed an interventional study using a Mediterranean diet in patients with asymptomatic hyperuricemia, and the findings showed that a higher baseline uric acid level was correlated with a greater reduction in uric acid level after the intervention. Furthermore, a recent cross-sectional study by Gao et al. [30] reported that the DASH diet was effective in lowering uric acid levels in a subgroup with the following characteristics: aged ≥ 50 years, male, and low physical activity. Thus, since the effect of a diet adjusted for fat intake on uric acid levels is inconstant, we speculate that fat intake may be more effective for individuals who are prone to high uric acid levels.
Our notable finding was an inverse relationship between fat and fatty acid intake and a high serum uric acid level in participants with reduced kidney function, whereas these relationships were not observed in the normal kidney function group. Juraschek et al. [28] reported that in African American hypertensive adults, the higher the baseline uric acid level, the greater the uric acid-lowering effect of the DASH diet. It is speculated that the population with high uric acid levels included many adults who were susceptible to hyperuricemia, such as those with gout and CKD. In the Juraschek et al. study [28], the baseline patient characteristics included a mean BMI of 34.7 kg/m2, a prevalence of diabetes of 29.1%, and a mean number of antihypertensive medications of 1.8 on the medication regimen, which suggests a high-risk population for CKD. In this study, the reduced kidney function group had a mean uric acid level of 6.3 mg/dL, which was significantly higher than the 5.8 mg/dL recorded for the normal kidney function group; the higher fat and fatty acid intake is presumed to be more effective in the reduced kidney function group. These findings suggest that higher fat and fatty acid intake for hyperuricemia is effective in individuals with reduced kidney function, suggesting the need for future consideration of individualized dietary therapy.
A mechanism linking fat intake and uric acid metabolism may involve the effects of dietary fats on insulin sensitivity. The effects of dietary fats on insulin sensitivity have been examined in metabolic syndrome with underlying insulin resistance [31,32,33,34]. A systematic review [31] of 14 observational studies and 16 clinical trials demonstrated that many of the observational studies found beneficial associations between MUFA/PUFA intake and metabolic syndrome components. Moreover, previous clinical trials support the benefits of MUFA- or PUFA-enriched diets in reducing metabolic syndrome. In addition to the abovementioned results, both the HOMA-R and blood insulin level, indices of insulin resistance, were shown to be reduced [31]. Another clinical trial [32] in 472 subjects with metabolic syndrome from eight European countries reported that the highest HOMA-R group, one of three groups classified by HOMA-R levels, had the greatest reduction in HOMA-R and insulin levels after consumption of a high MUFA diet or a diet supplemented with n-3 PUFA. These effects with a high MUFA diet or a diet supplemented with n-3 PUFA were also associated with the reduced plasma level of the inflammatory cytokine, IL-6 [32]. Insulin resistance disturbs glycolysis and uric acid clearance by the kidneys, leading to increased production of uric acid and decreased urinary uric acid clearance, respectively [33,34]. A case-control study of nonalcoholic fatty liver disease in Caucasians indicated that dietary patterns high in unsaturated fatty acids [35] were associated with lower serum uric acid levels and improved insulin resistance. A systematic review of insulin resistance in CKD by Spoto et al. [36] explains that the Janus effect of adipokines stimulates fatty acid oxidation by activating AMP-activated protein kinase, thereby improving insulin sensitivity. Therefore, we speculate that the mechanism in which fat and fatty acid intake is negatively associated with hyperuricemia in reduced kidney function partially involves the improvement of insulin resistance.
This study has several limitations that warrant discussion. First, as this is a cross-sectional study, additional longitudinal studies are needed to elucidate causal relationships. Second, the BDHQ may lack objectivity as it was self-administered. Third, as only males were evaluated, it is unclear whether similar results would be obtained for women.
5. Conclusions
The results of this study demonstrate that fat and fatty acid intake was inversely related to the higher uric acid level in males with reduced eGFR. This finding suggests that a higher intake of dietary fat and fatty acids is effective in the prevention and treatment of hyperuricemia in males with CKD.
Author Contributions
Conceptualization, F.O., A.H. and H.N.; Data curation, T.K. and A.T.; Formal analysis, H.T. and M.N.; Funding acquisition, H.N.; Investigation, F.O., A.H., H.T., K.S. (Keita Suzuki), K.-O.P., F.S., S.M., C.T., K.S.(Kuniko Sato) and T.Y.; Methodology, A.H. and H.N.; Project administration, H.N.; Resources, H.N.; Supervision, H.N.; Validation, H.T. and M.N.; Visualization, F.S.; Writing—original draft preparation, F.O. and A.H.; Writing—review and editing, H.T., K.S. (Keita Suzuki), K.-O.P., F.S., S.M., M.N., C.T., K.S. (Kuniko Sato), T.Y., T.K., A.T. and H.N. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by Grants-in-Acid for Scientific and Technology-Japan (Research project/Area number: 19H03882).
Institutional Review Board Statement
This study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of Kanazawa University (protocol code, 1491; date of approval, 18 December 2013).
Informed Consent Statement
All participants provided written informed consent.
Data Availability Statement
Data in the present study are available upon request from the corresponding author. Data are not publicly available due to privacy and ethical policies.
Acknowledgments
We wish to thank all of the field workers and laboratory personnel of the Shika study for their efforts.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lin, K.C.; Lin, H.Y.; Chou, P. Community based epidemiological study on hyperuricemia and gout in Kin-Hu, Kinmen. J. Rheumatol. 2000, 27, 1045–1050. [Google Scholar] [PubMed]
- Zhu, Y.; Pandya, B.J.; Choi, H.K. Prevalence of gout and hyperuricemia in the US general population: The National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011, 63, 3136–3141. [Google Scholar] [CrossRef]
- Mikuls, T.R.; Farrar, J.T.; Bilker, W.B.; Fernandes, S.; Schumacher, H.R.; Saag, K.G. Gout epidemiology: Results from the UK General Practice Research Database, 1990–1999. Ann. Rheum. Dis. 2005, 64, 267. [Google Scholar] [CrossRef] [PubMed]
- Keenan, R.T. The biology of urate. Semin. Arthritis Rheum. 2020, 50, S2–S10. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Li, L.; Zhang, Y.; Zeng, C. Recent advances in fructose intake and risk of hyperuricemia. Biomed. Pharmacother. 2020, 131, 110795. [Google Scholar] [CrossRef]
- Nakamura, K.; Sakurai, M.; Miura, K.; Morikawa, Y.; Yoshita, K.; Ishizaki, M.; Kido, T.; Naruse, Y.; Suwazono, Y.; Nakagawa, H. Alcohol intake and the risk of hyperuricaemia: A 6-year prospective study in Japanese men. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 989–996. [Google Scholar] [CrossRef]
- Makinouchi, T.; Sakata, K.; Oishi, M.; Tanaka, K.; Nogawa, K.; Watanabe, M.; Suwazono, Y. Benchmark dose of alcohol consumption for development of hyperuricemia in Japanese male workers: An 8-year cohort study. Alcohol 2016, 56, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Choi, H.K.; Atkinson, K.; Karlson, E.W.; Willett, W.; Curhan, G. Purine-rich foods, dairy and protein intake, and the risk of gout in men. N. Engl. J. Med. 2004, 350, 1093–1103. [Google Scholar] [CrossRef] [Green Version]
- Khanna, D.; Fitzgerald, J.D.; Khanna, P.P.; Bae, S.; Singh, M.K.; Neogi, T.; Pillinger, M.H.; Merill, J.; Lee, S.; Prakash, S.; et al. 2012 American college of rheumatology guidelines for management of gout part I: Systematic non-pharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res. 2012, 64, 1431. [Google Scholar] [CrossRef] [Green Version]
- Hisatome, I.; Ichida, K.; Mineo, I.; Ohtahara, A.; Ogino, K.; Kuwabara, M.; Ishizaka, N.; Uchida, S.; Kurajoh, M.; Kohagura, K.; et al. Japanese Society of Gout and Uric & Nucleic Acids 2019 guidelines for management of hyperuricemia and gout 3rd edition. Gout Uric Nucleic Acids 2020, 44, sp-1. [Google Scholar] [CrossRef]
- Juraschek, S.P.; Gelber, A.C.; Choi, H.K.; Appel, L.J.; Miller, E.R. Effects of the Dietary Approaches To Stop Hypertension (DASH) diet and sodium Intake on serum uric acid. Arthritis Rheumatol. 2016, 68, 3002. [Google Scholar] [CrossRef] [Green Version]
- Chrysohoou, C.; Skoumas, J.; Pitsavos, C.; Masoura, C.; Siasos, G.; Galiatsatos, N.; Psaltopoulou, T.; Mylonakis, C.; Margazas, A.; Kyvelou, S.; et al. Long-term adherence to the Mediterranean diet reduces the prevalence of hyperuricaemia in elderly individuals, without known cardiovascular disease: The Ikaria study. Maturitas 2011, 70, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Vernier, C.; Crichton, G.E.; Sauvageot, N.; Shivappa, N.; Hébert, J.R. Cross-comparison of diet quality indices for predicting chronic disease risk: Findings from the Observation of Cardiovascular Risk Factors in Luxembourg (ORISCAV-LUX) study. Br. J. Nutr. 2015, 113, 259. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Li, K.; Asimi, S.; Chen, Q.; Li, D. Effect of vitamin B-12 and n-3 polyunsaturated fatty acids on plasma homocysteine, ferritin, C-reaction protein, and other cardiovascular risk factors: A randomized controlled trial. Asia Pac. J. Clin. Nutr. 2015, 24, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Stea, T.H.; Stølevik, S.B.; Berntsen, S.; Ezzathkah Bastani, N.; Paulsen, G.; Lohne Seiler, H.; Hetlelid, K.J.; Blomhoff, R.; Mansoor, M.A. Effect of omega-3 and vitamins E + C supplements on the concentration of serum B-vitamins and plasma redox aminothiol antioxidant status in elderly men after strength training for three months. Ann. Nutr. Metab. 2016, 68, 145–155. [Google Scholar] [CrossRef]
- Dessein, P.H.; Shipton, E.A.; Stanwix, A.E.; Joffe, B.I.; Ramokgadi, J. Beneficial effects of weight loss associated with moderate calorie/carbohydrate restriction, and increased proportional intake of protein and unsaturated fat on serum urate and lipoprotein levels in gout: A pilot study. Ann. Rheum. Dis. 2000, 59, 539. [Google Scholar] [CrossRef] [Green Version]
- Li, R.; Yu, K.; Li, C. Dietary factors and risk of gout and hyperuricemia: A meta-analysis and systematic review. Asia Pac. J. Clin. Nutr. 2018, 27, 1344–1356. [Google Scholar] [CrossRef]
- Kitaoka, M.; Mitoma, J.; Asakura, H.; Anyenda, O.E.; Nguyen, T.T.T.; Hamagishi, T.; Hori, D.; Suzuki, F.; Shibata, A.; Horii, M.; et al. The relationship between hypertension and health-related quality of life: Adjusted by chronic pain, chronic diseases, and life habits in the general middle-aged population in Japan. Environ. Health Prev. Med. 2016, 21, 193. [Google Scholar] [CrossRef]
- Tsujiguchi, H.; Nguyen, T.T.T.; Goto, D.; Miyagi, S.; Kambayashi, Y.; Hara, A.; Yamada, Y.; Nakamura, H.; Shimizu, Y.; Hori, D.; et al. Relationship between the intake of n-3 polyunsaturated fatty acids and depressive symptoms in elderly Japanese people: Differences according to sex and weight status. Nutrients 2019, 11, 775. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, H.; Tsujiguchi, H.; Kambayashi, Y.; Hara, A.; Miyagi, S.; Yamada, Y.; Nguyen, T.T.T.; Shimizu, Y.; Hori, D.; Nakamura, H. Relationship between saturated fatty acid intake and hypertension and oxidative stress. Nutrition 2019, 61, 8–15. [Google Scholar] [CrossRef]
- Sasaki, S.; Yanagibori, R.; Amano, K. Self-administered diet history questionnaire developed for health education: A relative validation of the test-version by comparison with 3-day diet record in women. J. Epidemiol. 1998, 8, 203–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A.; et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.S.; Bilous, R.W.; Coresh, J. Chapter 1: Definition and classification of CKD. Kidney Int. Suppl. 2013, 3, 19–62. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, S.; Honda, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J. Epidemiol. 2012, 22, 151–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef]
- Choi, J.W.J.; Ford, E.S.; Gao, X.; Choi, H.K. Sugar-sweetened soft drinks, diet soft drinks, and serum uric acid level: The Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2008, 59, 109–116. [Google Scholar] [CrossRef]
- David B Mount Asymptomatic Hyperuricemia. Available online: https://www.uptodate.com/contents/asymptomatic-hyperuricemia (accessed on 16 March 2022).
- Juraschek, S.P.; White, K.; Tang, O.; Yeh, H.C.; Cooper, L.A.; Miller, E.R. Effects of a Dietary Approach to Stop Hypertension (DASH) diet intervention on serum uric acid in African Americans With hypertension. Arthritis Care Res. 2018, 70, 1509–1516. [Google Scholar] [CrossRef] [Green Version]
- Chatzipavlou, M.; Magiorkinis, G.; Koutsogeorgopoulou, L.; Kassimos, D. Mediterranean diet intervention for patients with hyperuricemia: A pilot study. Rheumatol. Int. 2014, 34, 759–762. [Google Scholar] [CrossRef]
- Gao, Y.; Cui, L.F.; Sun, Y.Y.; Yang, W.H.; Wang, J.R.; Wu, S.L.; Gao, X. Adherence to the dietary approaches to stop hypertension diet and hyperuricemia: A cross-sectional study. Arthritis Care Res. 2021, 73, 603–611. [Google Scholar] [CrossRef]
- Julibert, A.; del Mar Bibiloni, M.; Tur, J.A. Dietary fat intake and metabolic syndrome in adults: A systematic review. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 887–905. [Google Scholar] [CrossRef]
- Yubero-Serrano, E.M.; Delgado-Lista, J.; Tierney, A.C.; Perez-Martinez, P.; Garcia-Rios, A.; Alcala-Diaz, J.F.; Castaño, J.P.; Tinahones, F.J.; Drevon, C.A.; Defoort, C.; et al. Insulin resistance determines a differential response to changes in dietary fat modification on metabolic syndrome risk factors: The LIPGENE study. Am. J. Clin. Nutr. 2015, 102, 1509–1517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leyva, F.; Wingrove, C.S.; Godsland, I.F.; Stevenson, J.C. The glycolytic pathway to coronary heart disease: A hypothesis. Metabolism 1998, 47, 657–662. [Google Scholar] [CrossRef]
- Facchini, F.; Ida Chen, Y.D.; Hollenbeck, C.B.; Reaven, G.M. Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration. JAMA 1991, 266, 3008–3011. [Google Scholar] [CrossRef] [PubMed]
- Kalafati, I.-P.; Borsa, D.; Dimitriou, M.; Revenas, K.; Kokkinos, A.; Dedoussis, G.V. Dietary patterns and non-alcoholic fatty liver disease in a Greek case-control study. Nutrition 2019, 61, 105–110. [Google Scholar] [CrossRef]
- Spoto, B.; Pisano, A.; Zoccali, C. Insulin resistance in chronic kidney disease: A systematic review. Am. J. Physiol. Renal Physiol. 2016, 311, F1087–F1108. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).