Health Behaviours among Nursing Students in Poland during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Settings and Design
2.2. Participants
2.3. Research Instruments
2.3.1. Health Behaviour Inventory
- Proper eating habits (PNŻ), mainly taking into account the type of food eaten (e.g., wholemeal bread, fruit and vegetables);
- Prophylactic behaviours (ZP), which involve following health-related recommendations, and acquiring information on health and diseases;
- Health practices (PZ), which include daily habits related to sleep, recreation and physical activity;
- Positive mental attitudes (PNP), which include such psychological factors in the behaviours as avoiding too-strong emotions, stress, tension and depressing situations [20].
2.3.2. Satisfaction with Life Scale (SWLS)
2.4. Statistical Analysis
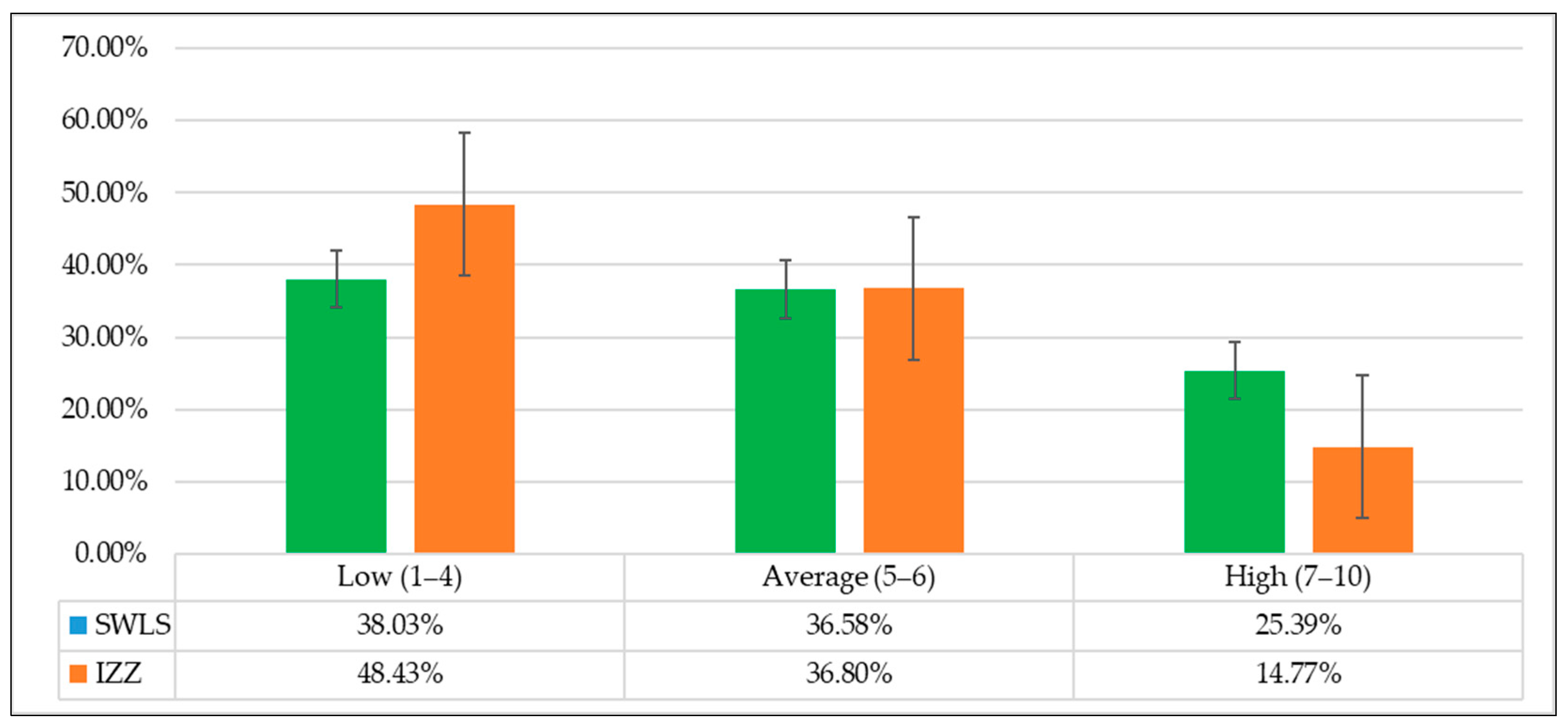
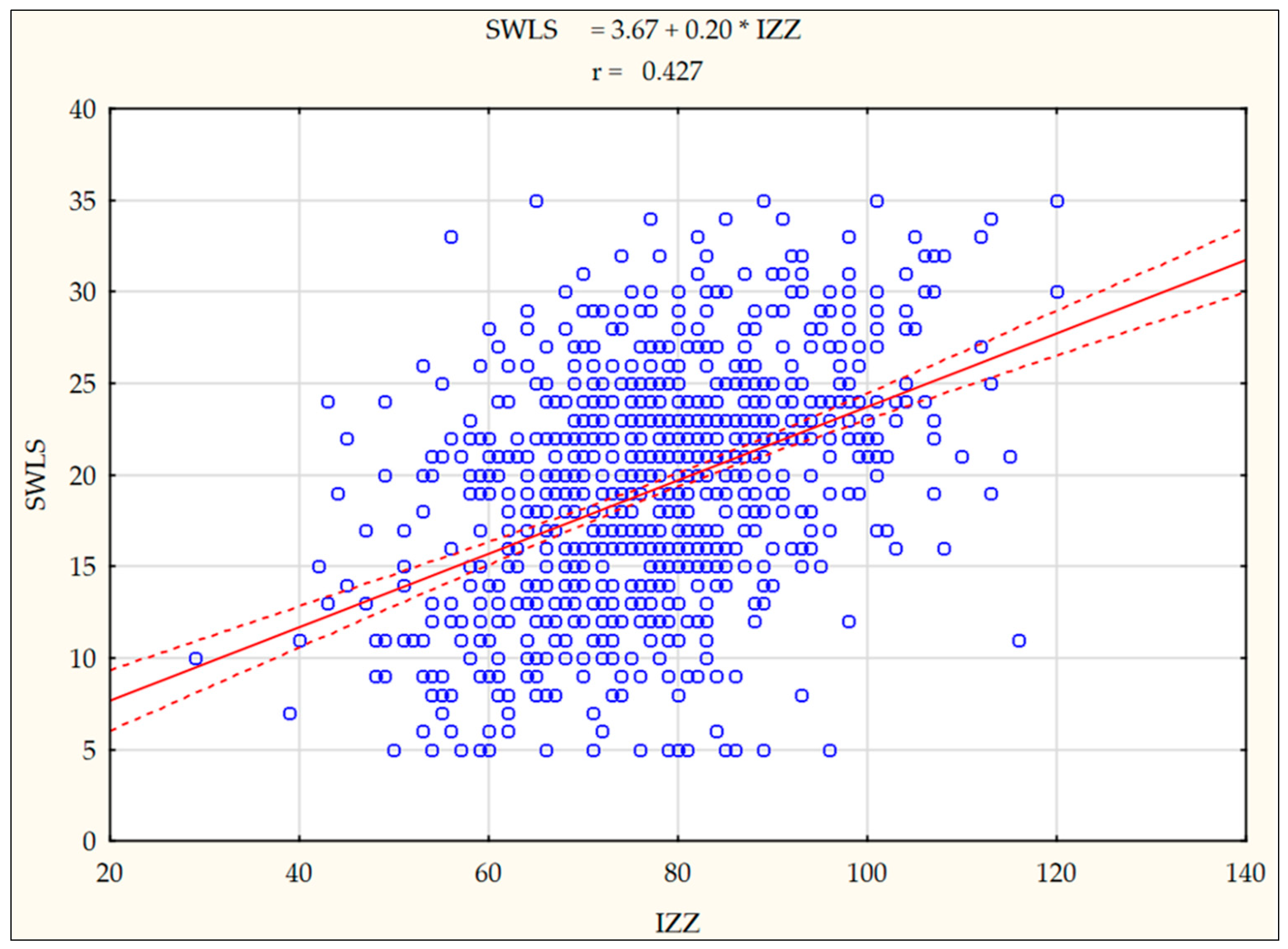
3. Results
4. Discussion
Limitations and Implications Regarding Professional Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables | N = 894 | |||||||
|---|---|---|---|---|---|---|---|---|
| M | SD | 95% CI | Me | Min.–Max. | Skewness | Kurtosis | ||
| SWLS | 19.27 | 6.36 | 18.86–19.69 | 20 | 5–35 | −0.05 | 0.43 | |
| IZZ | 77.75 | 13.52 | 76.87–78.64 | 78 | 29–120 | 0.01 | 0.15 | |
| Behaviour categories health | PNŻ | 3.21 | 0.81 | 3.16–3.27 | 3 | 1–5 | −0.05 | −0.33 |
| ZP | 3.41 | 0.72 | 3.36–3.46 | 4 | 1–5 | −0.28 | 0.01 | |
| PNP | 3.24 | 0.74 | 3.19–3.29 | 3 | 1–5 | −0.26 | −0.15 | |
| PZ | 3.10 | 0.73 | 3.05–3.15 | 3 | 1–5 | −0.03 | −0.43 | |
References
- Usher, K.; Durkin, J.; Bhullar, N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020, 29, 315–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Mata, J.; Wenz, A.; Rettig, T.; Reifenscheid, M.; Möhring, K.; Krieger, U.; Friedel, S.; Fikel, M.; Cornesse, C.; Blom, A.G.; et al. Health behaviors and mental health during the COVID-19 pandemic: A longitudinal population-based survey in Germany. Soc. Sci. Med. 2021, 287, 114333. [Google Scholar] [CrossRef]
- Czerski, W.M. Health behaviours and the intensity of Facebook usage among students. Rozpr. Społeczne [Soc. Diss.] 2021, 15, 30–47. [Google Scholar] [CrossRef]
- Ruiz, M.C.; Devonport, T.J.; Chen-Wilson, C.H.J.; Nicholls, W.; Cagas, J.Y.; Fernandez-Montalvo, J.; Choi, I.; Robazza, C. A cross-cultural exploratory study of health behaviors and wellbeing during COVID-19. Front. Psychol. 2021, 11, 3897. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, W.; Desalegn, H.; Solomon, S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin. Obes. 2021, 11, e12453. [Google Scholar] [CrossRef]
- Kożybska, M.; Kurpisz, J.; Radlińska, I.; Skwirczyńska, E.; Serwin, N.; Żabielski, P.; Kotwas, A.; Karakiewicz, B.; Lebiecka, Z.; Samochowiec, J.; et al. Problematic Internet Use, health behaviors, depression and eating disorders: A cross-sectional study among Polish medical school students. Ann. Gen. Psychiatry 2022, 21, 5. [Google Scholar] [CrossRef]
- Bener, A.; Bhugra, D. Lifestyle and depressive risk factors associated with problematic internet use in adolescents in an Arabian Gulf culture. J. Addict. Med. 2013, 7, 236–242. [Google Scholar] [CrossRef]
- Secades-Villa, R.; Calafat, A.; Fernández-Hermida, J.R.; Montse, J.; Duch, M.; Skärstrand, E.; Becoña, E.; Talic, S. Duration of Internet use and adverse psychosocial effects among European adolescents. Adicciones 2014, 26, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Villa, T.; Ojeda, J.A.; Gómez, A.A.; Carral, J.; Cancela, M.; Delgado-Rodríguez, M.; Jiménez-Mejías, E.; Llorca, J.; Molina, A.J.; Molanda, R.O.; et al. Problematic Internet Use in University Students: Associated factors and differences of gender. Adicciones 2015, 27, 265–275. [Google Scholar] [CrossRef]
- Marmola, M.; Wańczyk-Welc, A. Zachowania zdrowotne a poczucie satysfakcji z życia u młodych dorosłych. Kwart. Nauk. Fides Ratio 2017, 32, 185–196. [Google Scholar]
- Morton, K.R.; Lee, J.W.; Martin, L.R. Pathways from religion to health: Mediation by psychosocial and lifestyle mechanisms. Psychol. Relig. Spiritual. 2017, 9, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Nowak, G.; Pawlas, K.; Duda, S.; Kulik, A.; Nowak, D. Poczucie własnej skuteczności a zachowania zdrowotne i satysfakcja z życia studentów dietetyki. Psychol. Rozw. 2018, 23, 83–95. [Google Scholar] [CrossRef] [Green Version]
- Noor, A.M.; Priyalatha, G.; Isa, N.J.M. Personal growth initiative in relation to life satisfaction among university students. EDUCATUM J. Soc. Sci. 2020, 6, 42–49. [Google Scholar]
- Rogowska, A.M.; Ochnik, D.; Kuśnierz, C.; Jakubiak, M.; Schütz, A.; Held, M.J.; Arzenšek, A.; Benatov, J.; Berger, R.; Korchagina, E.V.; et al. Satisfaction with life among university students from nine countries: Cross-national study during the first wave of COVID-19 pandemic. BMC Public Health 2021, 21, 2262. [Google Scholar] [CrossRef] [PubMed]
- Rizun, M.; Strzelecki, A. Students’ acceptance of the COVID-19 impact on shifting higher education to distance learning in Poland. Int. J. Environ. Res. Public Health 2020, 17, 6468. [Google Scholar] [CrossRef]
- Gawrych, M.; Cichoń, E.; Kiejna, A. Strach przed pandemią COVID-19, zadowolenie z życia i zdrowie psychiczne w początkowej fazie pandemii w największych miastach w Polsce. Psychol. Zdr. Med. 2021, 26, 107–113. [Google Scholar]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef] [Green Version]
- Juczyński, Z. Narzędzia Pomiaru w Promocji i Psychologii Zdrowia; Pracownia Testów Psychologicznych: Warszawa, Poland, 2009. [Google Scholar]
- Szymczak, W. Podstawy Statystyki dla Psychologów [Fundamentals of Statistics for Psychologists]; DIFIN: Warszawa, Poland, 2018. [Google Scholar]
- Mun, H.; So, E.S. Changes in Physical Activity, Healthy Diet, and Sleeping Time during the COVID-19 Pandemic in South Korea. Nutrients 2022, 14, 960. [Google Scholar] [CrossRef]
- Knell, G.; Robertson, M.C.; Dooley, E.E.; Burford, K.; Mendez, K.S. Health behavior changes during COVID-19 pandemic and subsequent “stay-at-home” orders. Int. J. Environ. Res. Public Health 2020, 17, 6268. [Google Scholar] [CrossRef] [PubMed]
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: A cross-sectional online survey PLifeCOVID-19 study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Kupcewicz, E.; Mikla, M.; Kadučáková, H.; Schneider-Matyka, D.; Grochans, E. Health Behaviours and the Sense of Optimism in Nursing Students in Poland, Spain and Slovakia during the COVID-19 Pandemic. J. Environ. Res. Public Health 2022, 19, 2388. [Google Scholar] [CrossRef] [PubMed]
- Rasińska, R. Nawyki żywieniowe studentów w zależności od płci. Now. Lek. 2012, 81, 354–359. [Google Scholar]
- Palacz, J. Zachowania zdrowotne studentów w świetle wybranych uwarunkowań. Med. Og. Nauk Zdr. 2014, 20, 301–306. [Google Scholar] [CrossRef]
- Kropornicka, B.; Baczewska, B.; Dragan, W.; Krzyżanowska, E.; Olszak, C.; Szymczuk, E. Zachowania zdrowotne studentów Uniwersytetu Medycznego w Lublinie w zależności od miejsca zamieszkania. Rozpr. Społeczne 2015, 9, 58–64. [Google Scholar]
- Radosz, Z.; Tomaszewska-Kumela, P.; Paplaczyk, M.; Gruszczyńska, M. Zachowania zdrowotne studentów kierunków medycznych. Rozpr. Społeczne [Soc. Diss.] 2020, 14, 151–164. [Google Scholar] [CrossRef]
- Badura-Brzoza, K.; Bułdak, R.; Dębski, P.; Kasperczyk, S.; Woźniak-Grygiel, E.; Konka, A.; Gawrylak-Dryja, E.; Mond-Paszek, R.; Markiel, M.; Gabryś, D.; et al. Stres okresu pandemii wirusa SARS–CoV–2 a zachowania prozdrowotne wśród personelu medycznego—Doniesienie wstępne. Psychiatr. Pol. 2021, 238, 1–10. [Google Scholar]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, D.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef]
- Okechukwu, E.C.; Tibaldi, L.; La Torre, G. The impact of COVID-19 pandemic on mental health of Nurses. Clin. Ter. 2020, 171, 399–400. [Google Scholar]
- Mahmud, S.; Hossain, S.; Muyeed, A.; Islam, M.M.; Mohsin, M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon 2021, 7, e07393. [Google Scholar] [CrossRef] [PubMed]
- Villadsen, A.; Patalay, P.; Bann, D. Mental health in relation to changes in sleep, exercise, alcohol and diet during the COVID-19 pandemic: Examination of four UK cohort studies. Psychol. Med. 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Cheon, E.Y.; Yoo, J.H. A Study on the Relationship between Knowledge, Risk Perception, Preventive Health Behavior from Coronavirus disease-2019 in Nursing Students. J. Korea Acad.-Ind. Coop. Soc. 2021, 22, 246–254. [Google Scholar]
- Kosiba, G.; Gacek, M.; Bogacz-Walancik, A.; Wojtowicz, A. Zachowania prozdrowotne a satysfakcja z życia studentów kierunków nauczycielskich. Terażniejszość Człowiek Eduk. 2017, 20, 79–93. [Google Scholar]
- Stelcer, B.; Cybulski, M.; Kryvenko, I.; Yurtsenyuk, O.; Kachmarska, M.; Ryshkovska, N.; Katolyk, H.; Lisiński, P. Personal and behavioural health resources in Ukrainian students pursuing healthcare degrees: Preliminary study. Sci. Studios Soc. Political Psychol. 2019, 44, 103–117. [Google Scholar]
- Patsali, M.E.; Mousa, D.P.V.; Papadopoulou, E.V.; Papadopoulou, K.K.; Kaparounaki, C.K.; Diakogiannis, I.; Fountoulakis, K.N. University students’ changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. 2020, 292, 113298. [Google Scholar] [CrossRef]
- Zhang, S.X.; Wang, Y.; Rauch, A.; Wei, F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020, 288, 112958. [Google Scholar] [CrossRef]
- Ammar, A.; Chtourou, H.; Boukhris, O.; Trabelsi, K.; Masmoudi, L.; Brach, M.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. COVID-19 home confinement negatively impacts social participation and life satisfaction: A worldwide multicenter study. Int. J. Environ. Res. Public Health 2020, 17, 6237. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Gultekin, T.; Gultekin, T.; Yenal, S. The effect on life satisfaction of university students’ risky health behavior (abstract). PONTE Int. J. Sci. Res. 2020, 76, 7. [Google Scholar] [CrossRef]
- Hermassi, S.; Hayes, L.D.; Salman, A.; Sanal, N.E.; Abassi, E.; Al-Kuwari, L.; Aldous, N.; Musa, N.; Alyafei, A.; Bouhafs, E.G.; et al. Physical activity, sedentary behavior, and satisfaction with life of university students in Qatar: Changes during confinement due to the COVID-19 pandemic. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Juczyński, Z. Znaczenie spostrzeganego wsparcia społecznego dla dobrostanu jednostki–na przykładzie badań Kwestionariuszem Wsparcia Społecznego (Soz-U K-14). Czas. Psychol. 2019, 25, 195–202. [Google Scholar]
- Machul, M.; Bieniak, M.; Chałdaś-Majdańska, J.; Bąk, J.; Chrzan-Rodak, A.; Mazurek, P.; Pawłowski, P.; Makuch-Kuśmierz, D.; Obuchowska, A.; Bartoszek, A.; et al. Lifestyle Practices, Satisfaction with Life and the Level of Perceived Stress of Polish and Foreign Medical Students Studying in Poland. Int. J. Environ. Res. Public Health 2020, 17, 4445. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.Y.; Wong, D.F.K.; Joubert, L.; Chan, C.L.W. The protective function of meaning of life on life satisfaction among Chinese students in Australia and Hong Kong: A cross-cultural comparative study. J. Am. Coll. Health 2008, 57, 221–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schnettler, B.; Lobos, G.; Orellana, L.; Grunert, K. Analyzing food-related life satisfaction and other predictors of life satisfaction in central Chile. Span. J. Psychol. 2015, 18, E38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maher, J.P.; Doerksen, S.E.; Elavsky, S.; Conroy, D.E. Daily satisfaction with life is regulated by both physical activity and sedentary behavior. J. Sport Exerc. Psychol. 2014, 36, 166–178. [Google Scholar] [CrossRef]
- Maher, J.P.; Pincus, A.L.; Ram, N.; Conroy, D.E. Daily physical activity and life satisfaction across adulthood. Dev. Psychol. 2015, 51, 1407–1419. [Google Scholar] [CrossRef]
- Eime, R.; Harvey, J.; Payne, W. Dose-response of women’s health-related quality of life (HRQoL) and life satisfaction to physical activity. J. Phys. Act. Health. 2014, 11, 330–338. [Google Scholar] [CrossRef]
- Pedišić, Z.; Rakovac, M.; Titze, S.; Jurakić, D.; Oja, P. Domain-specific physical activity and health-related quality of life in university students. Eur. J. Sport Sci. 2014, 14, 492–499. [Google Scholar] [CrossRef]
| Variables | Total N = 894 | ||
|---|---|---|---|
| Number | % | ||
| University/College name | Pomeranian Medical University in Szczecin | 215 | 24.05 |
| University of Warmia and Mazury in Olsztyn | 175 | 19.57 | |
| Medical University of Gdańsk | 143 | 16.00 | |
| Nicolaus Copernicus University in Toruń, the Collegium Medicum in Bydgoszcz | 171 | 19.24 | |
| Jagiellonian University in Kraków | 132 | 14.77 | |
| Jan Kochanowski University of Kielce | 57 | 6.38 | |
| Gender | female | 822 | 91.95 |
| male | 72 | 8.05 | |
| Study year | first | 397 | 44.41 |
| second | 289 | 32.33 | |
| third | 208 | 23.27 | |
| Age (years) | ≤20 | 481 | 53.80 |
| 21–22 | 319 | 35.68 | |
| ≥23 | 94 | 10.51 | |
| Place and form of residence | with family/someone close | 621 | 69.46 |
| on their own | 273 | 30.54 | |
| Number of hours spent working on a computer | ≤5 | 433 | 48.43 |
| 6–9 | 302 | 33.78 | |
| ≥10 | 159 | 17.79 | |
| Number of consumed meals per day | 1–2 | 104 | 11.63 |
| 3 | 382 | 42.73 | |
| 4 | 280 | 31.32 | |
| ≥5 | 128 | 14.32 | |
| Restriction of physical activity during the pandemic | no | 211 | 23.60 |
| yes, to a small extent | 161 | 18.01 | |
| yes, to a medium extent | 278 | 31.10 | |
| yes, to a considerable extent | 244 | 27.29 | |
| Subjective health status assessment during the pandemic | bad | 24 | 2.68 |
| good/average | 613 | 68.57 | |
| very good | 257 | 28.75 | |
| Restriction of social contacts during the pandemic | very high | 141 | 15.77 |
| considerable | 360 | 40.27 | |
| medium/average | 229 | 25.62 | |
| to a small extent | 164 | 18.34 | |
| Variables | N = 894 (%) | IZZ | SWLS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | F | p-Value | Post Hoc (NIR) | M | SD | F | p-Value | Post Hoc (NIR) | |||
| Gender | female | 822 (91.95) | 77.98 | 13.52 | 2.97 | 0.09 | 19.33 | 6.38 | 0.78 | 0.37 | ||
| male | 72 (8.05) | 75.13 | 13.31 | 18.64 | 6.04 | |||||||
| Study year | first (A) | 397 (44.41) | 76.05 | 13.16 | 5.97 | 0.002 | A < B ** A < C ** | 18.90 | 6.32 | 1.5 | 0.22 | |
| second (B) | 289 (32.33) | 78.80 | 13.49 | 19.39 | 6.49 | |||||||
| third (C) | 208 (23.27) | 79.57 | 13.90 | 19.82 | 6.21 | |||||||
| Age (years) M = 20.73; SD = 1.81 | ≤20 | 481 (53.80) | 77.27 | 13.11 | 1.01 | 0.36 | 19.26 | 6.17 | 0.77 | 0.45 | ||
| 21–22 | 319 (35.68) | 78.02 | 13.97 | 19.08 | 6.61 | |||||||
| ≥23 | 94 (10.51) | 79.33 | 14.03 | 20.01 | 6.43 | |||||||
| Place and form of residence | with family/someone close | 621 (69.46) | 78.02 | 13.30 | 0.76 | 0.38 | 19.38 | 6.40 | 0.6 | 0.43 | ||
| on their own | 273 (30.54) | 77.16 | 14.01 | 19.03 | 6.26 | |||||||
| Number of hours spent working on a computer M = 6.08; SD = 3.19 | ≤5 (A) | 433 (48.43) | 78.59 | 13.77 | 1.84 | 0.15 | 19.96 | 6.14 | 5.4 | 0.004 | A < B ** | |
| 6–9 (B) | 302 (33.78) | 77.27 | 13.19 | 18.43 | 6.47 | |||||||
| ≥10 (C) | 159 (17.79) | 76.38 | 13.36 | 19.00 | 6.54 | |||||||
| Number of meals M = 3.48; SD = 0.87 | 1–2 (A) | 104 (11.63) | 69.03 | 14.19 | 27.76 | 0.0001 | A < B,C,D *** B < C,D *** C < D *** | 16.22 | 6.81 | 12.17 | 0.0001 | A < B,C,D *** B < C ** B < D * |
| 3 (B) | 382 (42.73) | 76.55 | 13.35 | 19.01 | 6.37 | |||||||
| 4 (C) | 280 (31.32) | 80.13 | 12.32 | 20.31 | 5.86 | |||||||
| ≥5 (D) | 128 (14.32) | 83.25 | 12.00 | 20.27 | 6.17 | |||||||
| Restriction of physical activity during the pandemic | no | 211 (23.60) | 78.51 | 13.65 | 3.46 | 0.02 | 19.70 | 6.29 | 1.79 | 0.14 | ||
| yes, to a small extent | 161 (18.01) | 79.11 | 13.64 | 19.55 | 6.25 | |||||||
| yes, to a medium extent | 278 (31.10) | 78.45 | 12.69 | 19.49 | 6.53 | |||||||
| yes, to a considerable extent | 244 (27.29) | 75.41 | 14.03 | 18.48 | 6.25 | |||||||
| Subjective health status assessment during the pandemic | bad (A) | 24 (2.68) | 66.08 | 11.45 | 44.02 | 0.0001 | A < B ** A < C *** B < C *** | 14.71 | 5.99 | 33.03 | 0.0001 | A < B ** A < C *** B < C *** |
| good/average (B) | 613 (68.57) | 75.74 | 13.03 | 18.42 | 6.14 | |||||||
| very good (C) | 257 (28.75) | 83.65 | 12.74 | 21.73 | 6.15 | |||||||
| Restriction of social contacts during the pandemic | very high (A) | 141 (15.77) | 77.38 | 14.35 | 0.88 | 0.44 | 18.21 | 5.98 | 4.24 | 0.005 | A < C * A < D ** | |
| considerable (B) | 360 (40.27) | 77.80 | 13.64 | 18.89 | 6.42 | |||||||
| medium/average (C) | 229 (25.62) | 78.76 | 13.01 | 19.62 | 6.26 | |||||||
| to a small extent (D) | 164 (18.34) | 76.57 | 13.22 | 20.55 | 6.47 | |||||||
| Variables | R2 | ßeta | ß | t | p-Value | |
|---|---|---|---|---|---|---|
| IZZ | Constant value | 44.80 | 15.24 | 0.001 | ||
| SWLS | 0.18 | 0.34 | 0.73 | 11.38 | 0.001 | |
| Number of meals | 0.23 | 0.19 | 2.94 | 6.49 | 0.001 | |
| Subjective health status assessment during the pandemic | 0.26 | 0.19 | 5.09 | 6.24 | 0.001 | |
| Study year | 0.26 | 0.12 | 2.05 | 2.65 | 0.008 | |
| Restriction of social contacts during the pandemic | 0.27 | −0.08 | −1.06 | −2.53 | 0.01 | |
| R = 0.52; R2 = 0.27; corrected R2 = 0.27 | ||||||
| PNŻ | Constant value | 13.10 | 9.30 | 0.001 | ||
| SWLS | 0.04 | 0.15 | 0.12 | 4.57 | 0.001 | |
| Number of meals | 0.06 | 0.14 | 0.76 | 4.17 | 0.001 | |
| Subjective health status assessment during the pandemic | 0.08 | 0.14 | 1.35 | 4.15 | 0.001 | |
| Restriction of social contacts during the pandemic | 0.08 | −0.09 | −0.45 | −2.69 | 0.007 | |
| Restriction of physical activity during the pandemic | 0.10 | −0.09 | −0.37 | −2.58 | 0.01 | |
| R = 0.33; R2 = 0.10; corrected R2 = 0.10 | ||||||
| ZP | Constant value | 3.04 | 8.57 | 0.001 | ||
| SWLS | 0.06 | 0.21 | 0.02 | 6.10 | 0.001 | |
| Number of meals | 0.08 | 0.12 | 0.10 | 3.80 | 0.001 | |
| Subjective health status assessment during the pandemic | 0.09 | 0.11 | 0.16 | 3.26 | 0.001 | |
| Study year | 0.10 | 0.12 | 0.11 | 2.69 | 0.007 | |
| Age | 0.10 | −0.10 | −0.04 | −2.22 | 0.03 | |
| R = 0.32; R2 = 0.11; corrected R2 = 0.10 | ||||||
| PNP | Constant value | 6.90 | 8.57 | 0.001 | ||
| SWLS | 0.26 | 0.44 | 0.31 | 15.07 | 0.001 | |
| Subjective health status assessment during the pandemic | 0.29 | 0.18 | 1.58 | 6.18 | 0.001 | |
| Number of meals | 0.32 | 0.15 | 0.76 | 5.30 | 0.001 | |
| Study year | 0.32 | 0.08 | 0.43 | 2.78 | 0.005 | |
| R = 0.57; R2 = 0.33; corrected R2 = 0.32 | ||||||
| PZ | Constant value | 11.42 | 10.13 | 0.001 | ||
| SWLS | 0.10 | 0.25 | 0.17 | 7.64 | 0.001 | |
| Number of meals | 0.13 | 0.17 | 0.85 | 5.40 | 0.001 | |
| Subjective health status assessment during the pandemic | 0.15 | 0.13 | 1.18 | 4.11 | 0.001 | |
| R = 0.39; R2 = 0.153; corrected R2 = 0.15 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kupcewicz, E.; Rachubińska, K.; Gaworska-Krzemińska, A.; Andruszkiewicz, A.; Kuźmicz, I.; Kozieł, D.; Grochans, E. Health Behaviours among Nursing Students in Poland during the COVID-19 Pandemic. Nutrients 2022, 14, 2638. https://doi.org/10.3390/nu14132638
Kupcewicz E, Rachubińska K, Gaworska-Krzemińska A, Andruszkiewicz A, Kuźmicz I, Kozieł D, Grochans E. Health Behaviours among Nursing Students in Poland during the COVID-19 Pandemic. Nutrients. 2022; 14(13):2638. https://doi.org/10.3390/nu14132638
Chicago/Turabian StyleKupcewicz, Ewa, Kamila Rachubińska, Aleksandra Gaworska-Krzemińska, Anna Andruszkiewicz, Ilona Kuźmicz, Dorota Kozieł, and Elżbieta Grochans. 2022. "Health Behaviours among Nursing Students in Poland during the COVID-19 Pandemic" Nutrients 14, no. 13: 2638. https://doi.org/10.3390/nu14132638
APA StyleKupcewicz, E., Rachubińska, K., Gaworska-Krzemińska, A., Andruszkiewicz, A., Kuźmicz, I., Kozieł, D., & Grochans, E. (2022). Health Behaviours among Nursing Students in Poland during the COVID-19 Pandemic. Nutrients, 14(13), 2638. https://doi.org/10.3390/nu14132638










