The Impact of a Web-Based Lifestyle Educational Program (‘Living Better’) Reintervention on Hypertensive Overweight or Obese Patients
Abstract
:1. Introduction
2. Materials and Methods
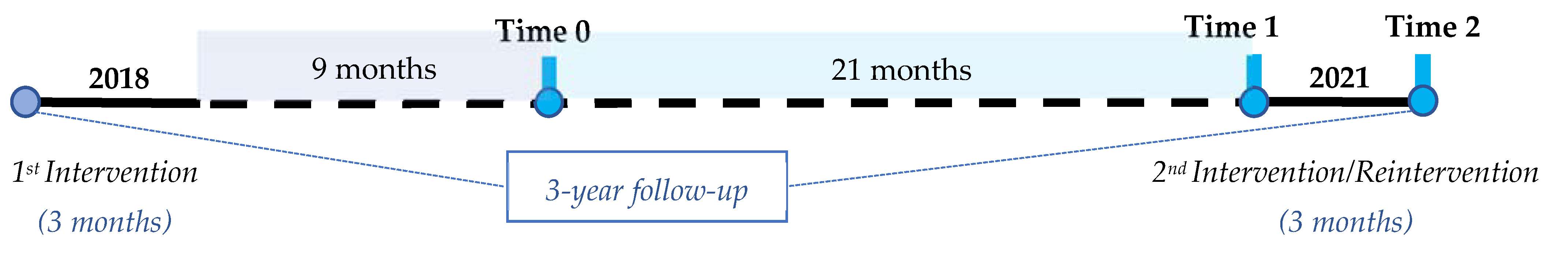
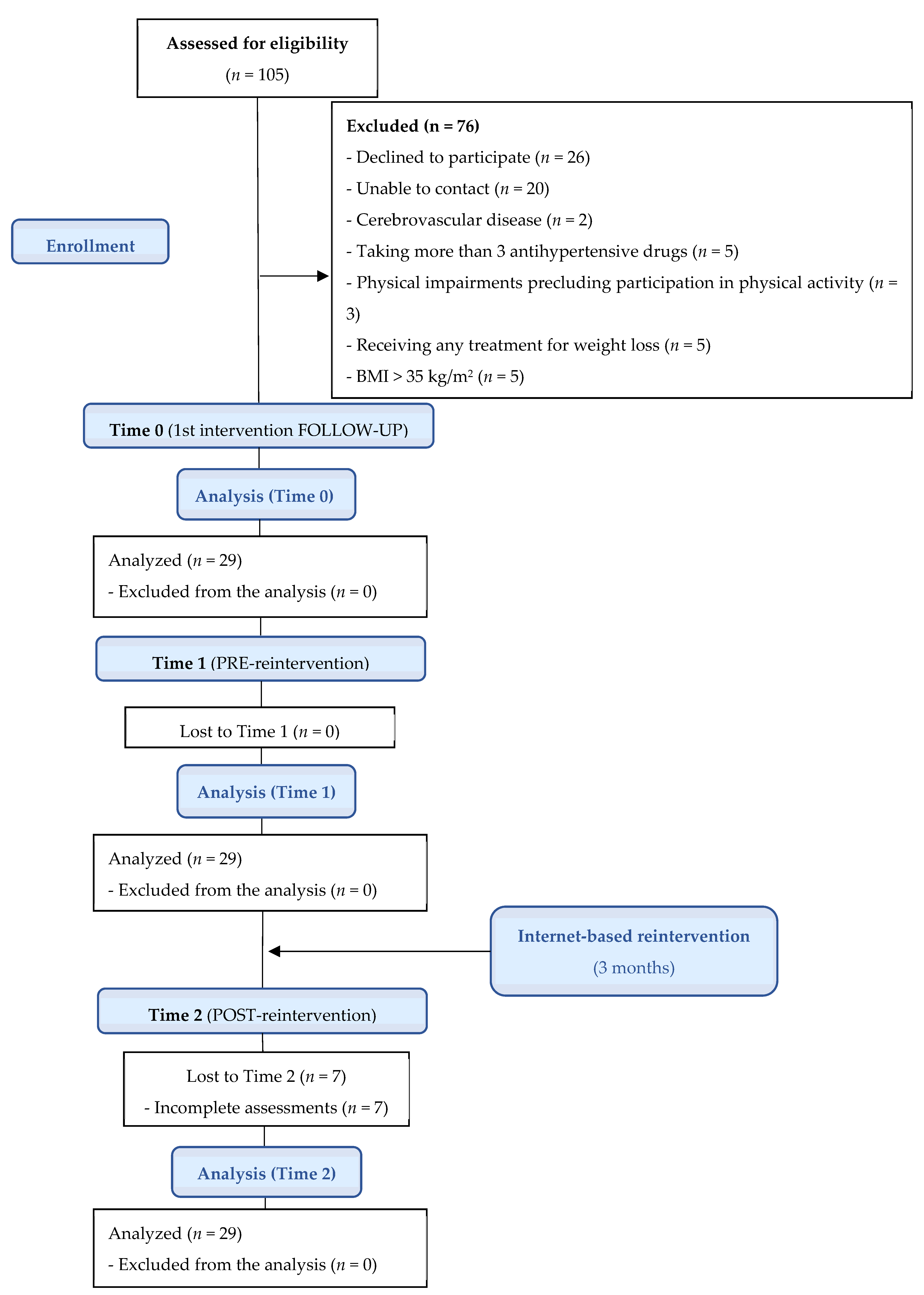
2.1. Study Design
2.2. Eligibility Criteria
2.3. Procedure
2.4. Intervention
2.5. Outcome Measures
2.5.1. Systolic and Diastolic Blood Pressure
2.5.2. Weight, Height, and BMI
2.5.3. Antihypertensive Drugs
2.5.4. Physical Activity Levels
2.5.5. Eating Behavior
2.5.6. Adherence to the Mediterranean Diet
2.5.7. Satisfaction with the Reintervention
2.5.8. Adherence to Reintervention
2.6. Statistical Analysis
3. Results
3.1. Reported Changes in the SBP, DBP, BMI, and Eating Behavior
3.2. Differences Found in Antihypertensive Drugs and PA
3.3. Results Analyses of Adherence to the Mediterranean Diet, Satisfaction, and Adherence to the Reintervention
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keating, S.E.; Coombes, J.S.; Stowasser, M.; Bailey, T.G. The role of exercise in patients with obesity and hypertension. Curr. Hypertens. Rep. 2020, 22, 77. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical P. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). J. Hypertens. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, e177–e232. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [Green Version]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Swift, D.L.; Johannsen, N.M.; Lavie, C.J.; Earnest, C.P.; Church, T.S. The role of exercise and physical activity in weight loss and maintenance. Prog. Cardiovasc. Dis. 2014, 56, 441–447. [Google Scholar] [CrossRef] [Green Version]
- Jakicic, J.M.; Rogers, R.J.; Collins, A.M.; Jackson, R. Strategies for physical activity interventions in the treatment of obesity. Endocrinol. Metab. Clin. N. Am. 2020, 49, 289–301. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef]
- Methnani, J.; Amor, D.; Yousfi, N.; Bouslama, A.; Omezzine, A.; Bouhlel, E. Sedentary behavior, exercise and COVID-19: Immune and metabolic implications in obesity and its comorbidities. J. Sports Med. Phys. Fit. 2020, 61, 1538–1547. [Google Scholar] [CrossRef]
- Browne, R.A.V.; Macêdo, G.A.D.; Cabral, L.L.P.; Oliveira, G.T.A.; Vivas, A.; Fontes, E.B.; Elsangedy, H.M.; Costa, E.C. Initial impact of the COVID-19 pandemic on physical activity and sedentary behavior in hypertensive older adults: An accelerometer-based analysis. Exp. Gerontol. 2020, 142, 111121. [Google Scholar] [CrossRef]
- Ashby, N.J.S. Impact of the COVID-19 pandemic on unhealthy eating in populations with obesity. Obesity 2020, 28, 1802–1805. [Google Scholar] [CrossRef]
- Bullard, T.; Medcalf, A.; Rethorst, C.; Foster, G.D. Impact of the COVID-19 pandemic on initial weight loss in a digital weight management program: A natural experiment. Obesity 2021, 29, 1434–1438. [Google Scholar] [CrossRef]
- Park, M.J.; Kim, H.S.; Kim, K.S. Cellular phone and Internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int. J. Med. Inform. 2009, 78, 704–710. [Google Scholar] [CrossRef]
- Bennett, G.G.; Herring, S.J.; Puleo, E.; Stein, E.K.; Emmons, K.M.; Gillman, M.W. Web-based weight loss in primary care: A randomized controlled trial. Obesity 2010, 18, 308–313. [Google Scholar] [CrossRef]
- Mensorio, M.S.; Cebolla-Martí, A.; Rodilla, E.; Palomar, G.; Lisón, J.F.; Botella, C.; Fernández-Aranda, F.; Jimenez-Murcia, S.; Baños, R.M. Analysis of the efficacy of an internet-based self-administered intervention (“Living Better”) to promote healthy habits in a population with obesity and hypertension: An exploratory randomized controlled trial. Int. J. Med. Inform. 2019, 124, 13–23. [Google Scholar] [CrossRef]
- Lisón, J.F.; Palomar, G.; Mensorio, M.S.; Baños, R.M.; Cebolla-Martí, A.; Botella, C.; Benavent-Caballer, V.; Rodilla, E. Impact of a web-based exercise and nutritional education intervention in patients who are obese with hypertension: Randomized wait-list controlled trial. J. Med. Internet Res. 2020, 22, e14196. [Google Scholar] [CrossRef]
- Hu, E.A.; Pasupuleti, M.; Nguyen, V.; Langheier, J.; Shurney, D. Sustaining weight loss among adults with obesity using a digital meal planning and food purchasing platform for 12, 24, and 36 months: A longitudinal study. Nutr. J. 2021, 20, 8. [Google Scholar] [CrossRef]
- Baños, R.M.; Mensorio, M.S.; Cebolla, A.; Rodilla, E.; Palomar, G.; Lisón, J.F.; Botella, C. An internet-based self-administered intervention for promoting healthy habits and weight loss in hypertensive people who are overweight or obese: A randomized controlled trial. BMC Cardiovasc. Disord. 2015, 15, 83. [Google Scholar] [CrossRef] [Green Version]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam. Fisioter. Kinesiol. 2007, 10, 48–52. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 compendium of physical activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef] [Green Version]
- van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- Cebolla, A.; Barrada, J.R.; van Strien, T.; Oliver, E.; Baños, R. Validation of the Dutch Eating Behavior Questionnaire (DEBQ) in a sample of Spanish women. Appetite 2014, 73, 58–64. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing mediterranean diet adherence among older spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- Baños, R.M.; Cebolla, A.; Moragrega, I.; van Strien, T.; Fernández-Aranda, F.; Agüera, Z.; de la Torre, R.; Casanueva, F.F.; Fernández-Real, J.M.; Fernández-García, J.C.; et al. Relationship between eating styles and temperament in an anorexia nervosa, healthy control, and morbid obesity female sample. Appetite 2014, 76, 76–83. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Papandreou, C.; Arija, V.; Aretouli, E.; Tsilidis, K.K.; Bulló, M. Comparing eating behaviours, and symptoms of depression and anxiety between Spain and Greece during the COVID-19 outbreak: Cross-sectional analysis of two different confinement strategies. Eur. Eat. Disord. Rev. 2020, 28, 836–846. [Google Scholar] [CrossRef]
- Neter, J.E.; Stam, B.E.; Kok, F.J.; Grobbee, D.E.; Geleijnse, J.M. Influence of weight reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension 2003, 42, 878–884. [Google Scholar] [CrossRef]
- Liu, S.; Dunford, S.D.; Leung, Y.W.; Brooks, D.; Thomas, S.G.; Eysenbach, G.; Nolan, R.P. Reducing blood pressure with internet-based interventions: A meta-analysis. Can. J. Cardiol. 2013, 29, 613–621. [Google Scholar] [CrossRef]
- Müller, A.M.; Alley, S.; Schoeppe, S.; Vandelanotte, C. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 109. [Google Scholar] [PubMed] [Green Version]
- Wijsman, C.A.; Westendorp, R.G.J.; Verhagen, E.A.L.M.; Catt, M.; Slagboom, P.E.; De Craen, A.J.M.; Broekhuizen, K.; Van Mechelen, W.; Van Heemst, D.; Van Der Ouderaa, F.; et al. Effects of a web-based intervention on physical activity and metabolism in older adults: Randomized controlled trial. J. Med. Internet Res. 2013, 15, e233. [Google Scholar] [CrossRef] [PubMed]
- Kreutz, R.; Dobrowolski, P.; Prejbisz, A.; Algharably, E.A.-H.; Bilo, G.; Creutzig, F.; Grassi, G.; Kotsis, V.; Lovic, D.; Lurbe, E.; et al. Lifestyle, psychological, socioeconomic and environmental factors and their impact on hypertension during the coronavirus disease 2019 pandemic. J. Hypertens. 2021, 39, 1077–1089. [Google Scholar] [CrossRef] [PubMed]
- Marashi, M.Y.; Nicholson, E.; Ogrodnik, M.; Fenesi, B.; Heisz, J.J. A mental health paradox: Mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PLoS ONE 2021, 16, e0239244. [Google Scholar] [CrossRef]
- Khan, N.; Marvel, F.A.; Wang, J.; Martin, S.S. Digital health technologies to promote lifestyle change and adherence. Curr. Treat. Options Cardiovasc. Med. 2017, 19, 60. [Google Scholar] [CrossRef]
- Alkhaldi, G.; Hamilton, F.L.; Lau, R.; Webster, R.; Michie, S.; Murray, E. The effectiveness of technology-based strategies to promote engagement with digital interventions: A systematic review protocol. JMIR Res. Protoc. 2015, 4, e47. [Google Scholar] [CrossRef] [Green Version]
- Richard, E.; Jongstra, S.; Soininen, H.; Brayne, C.; Moll Van Charante, E.P.; Meiller, Y.; Van Der Groep, B.; Beishuizen, C.R.L.; Mangialasche, F.; Barbera, M.; et al. Healthy ageing through Internet counselling in the elderly: The HATICE randomised controlled trial for the prevention of cardiovascular disease and cognitive impairment. BMJ Open 2016, 6, e010806. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Manzoni, G.M.; Cuzziol, P.; Cesa, G.L.; Tuzzi, C.; Villa, V.; Liuzzi, A.; Petroni, M.L.; Molinari, E. TECNOB: Study design of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes. BMC Public Health 2010, 10, 204. [Google Scholar] [CrossRef] [Green Version]
| VARIABLES | Time 1; Mean (SD) a | |
|---|---|---|
| Sex (n) | Women | 8 |
| Men | 21 | |
| Age (years) | 57.3 (10.0) | |
| Systolic blood pressure (mmHg) | 129.6 (12.2) | |
| Diastolic blood pressure (mmHg) | 78.6 (8.1) | |
| Weight (kg) | 84.1 (11.0) | |
| BMI (kg/m2) | 29.2 (2.4) | |
| Antihypertensive drugs (n) | 1.6 (1.4) | |
| Physical activity level (METs-min/week) | 2308 (2266) | |
| Eating behavior (points) | Emotional eating | 27.1 (10.7) |
| External eating | 28.4 (6.6) | |
| Restrained eating | 27.0 (6.0) | |
| Adherence to the Mediterranean diet (points) | 8.2 (2.1) | |
| Time 0 vs. Time 1 | Time 1 vs. Time 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| VARIABLES | Baseline a | Time 0 b | Time 1 c | Time 2 d | Difference e (95% CI) | p | Difference f (95% CI) | p | |
| Systolic blood pressure (mmHg) | 128.8 (11.5) | 127.3 (12.7) | 129.6 (12.2) | 124.9 (11.1) | 2.3 (−4.0 to 8.5) | 1.000 | −4.7 (−8.7 to −0.7) | 0.017 * | |
| Diastolic blood pressure (mmHg) | 77.0 (6.6) | 76.4 (6.7) | 78.6 (8.1) | 75.1 (8.9) | 2.2 (−2.0 to 6.4) | 0.600 | −3.5 (−6.2 to −0.8) | 0.009 ** | |
| BMI (kg/m2) | 29.3 (2.6) | 28.9 (2.5) | 29.2 (2.4) | 28.6 (2.3) | 0.3 (−0.4 to 1.0) | 0.895 | −0.7 (−1.0 to −0.4) | <0.001 ** | |
| Eating behavior (points) | Emotional eating | 28.8 (10.6) | 27.8 (8.6) | 27.1 (10.7) | 24.3 (9.0) | −0.8 (−3.7 to 2.2) | 1.000 | −2.8 (−5.1 to −0.5) | 0.012 * |
| External eating | 30.6 (6.1) | 29.5 (6.4) | 28.4 (6.6) | 27.3 (7.0) | −1.1 (−3.3 to 1.1) | 0.640 | −1.1 (−2.1 to −0.1) | 0.039 * | |
| Restrained eating | 27.9 (6.6) | 28.6 (6.6) | 27.0 (6.0) | 26.9 (6.0) | −1.6 (−3.9 to 0.7) | 0.248 | −0.2 (−1.6 to 1.2) | 1.000 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Múzquiz-Barberá, P.; Ruiz-Cortés, M.; Herrero, R.; Vara, M.D.; Escrivá-Martínez, T.; Carcelén, R.; Baños, R.M.; Rodilla, E.; Lisón, J.F. The Impact of a Web-Based Lifestyle Educational Program (‘Living Better’) Reintervention on Hypertensive Overweight or Obese Patients. Nutrients 2022, 14, 2235. https://doi.org/10.3390/nu14112235
Múzquiz-Barberá P, Ruiz-Cortés M, Herrero R, Vara MD, Escrivá-Martínez T, Carcelén R, Baños RM, Rodilla E, Lisón JF. The Impact of a Web-Based Lifestyle Educational Program (‘Living Better’) Reintervention on Hypertensive Overweight or Obese Patients. Nutrients. 2022; 14(11):2235. https://doi.org/10.3390/nu14112235
Chicago/Turabian StyleMúzquiz-Barberá, Pedro, Marta Ruiz-Cortés, Rocío Herrero, María Dolores Vara, Tamara Escrivá-Martínez, Raquel Carcelén, Rosa María Baños, Enrique Rodilla, and Juan Francisco Lisón. 2022. "The Impact of a Web-Based Lifestyle Educational Program (‘Living Better’) Reintervention on Hypertensive Overweight or Obese Patients" Nutrients 14, no. 11: 2235. https://doi.org/10.3390/nu14112235
APA StyleMúzquiz-Barberá, P., Ruiz-Cortés, M., Herrero, R., Vara, M. D., Escrivá-Martínez, T., Carcelén, R., Baños, R. M., Rodilla, E., & Lisón, J. F. (2022). The Impact of a Web-Based Lifestyle Educational Program (‘Living Better’) Reintervention on Hypertensive Overweight or Obese Patients. Nutrients, 14(11), 2235. https://doi.org/10.3390/nu14112235







